Abstract
We evaluated the impact of FLT3-ITD, NPM1 mutations, and double mutant CEBPa (dmCEBPa) on overall survival (OS) after relapse in patients with cytogenetically intermediate-risk acute myeloid leukemia (AML) who were treated with chemotherapy alone in the first remission (CR1). Patients aged 16–65 years diagnosed with cytogenetically intermediate-risk AML, and who achieved CR1 were included. We retrospectively analyzed FLT3-ITD, NPM1 mutations and CEBPa using samples obtained at diagnosis, which therefore did not affect the therapeutic decisions. Among 235 patients who had achieved CR1, 152 relapsed, and 52% of them achieved second CR. The rate of achieving second CR was significantly higher (85%) in those with dmCEBPa. Patients with FLT3-ITD had significantly worse OS after relapse than those without (19% vs 41%, p = 0.002), while OS was comparable between patients with and without NPM1 mutations (37% vs 34%, p = 0.309). Patients with dmCEBPa had improved OS than those without (61% vs 32%, p = 0.006). By multivariate analysis, FLT3-ITD was independently associated with worse OS after relapse [hazard ratio (HR) 1.99, 95% CI 1.27–3.12, p = 0.003], and dmCEBPa with improved OS (HR 0.40, 95% CI 0.17–0.93, p = 0.033). Our data show that screening for these mutations at diagnosis is useful for facilitating effective therapeutic decision-making even after relapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a molecularly heterogeneous hematological malignancy [1,2,3,4]. Although pretreatment cytogenetic classification has traditionally been the most potent prognostic factor [5,6,7,8], the importance of considering genetic profiles when formulating post-remission treatment strategies has been recognized [9]. Regarding the role of allogeneic hematopoietic cell transplantation (allo-HCT), genetic profiles may be particularly useful in cytogenetically intermediate-risk AML, which accounts for 46–67% of AML cases.
The National Comprehensive Cancer Network (NCCN) [10] and European LeukemiaNet (ELN) [11] have included three major mutations, namely Fms-like tyrosine kinase 3-internal tandem duplication (FLT3-ITD), mutant nucleophosmin (NPM1), and double mutant CCAAT/enhancer binding protein alpha (dmCEBPa), in the risk stratification of AML. Exploration of these molecular markers in the initial work-up is strongly encouraged, especially in cytogenetically intermediate-risk AML. FLT3-ITD is associated with poor prognosis [12,13,14,15], and we previously showed that allo-HCT during first complete remission (CR1) improved the outcomes of patients with FLT3-ITD [16]. On the other hand, dmCEBPa has been shown to carry a favorable prognosis [17, 18], and we showed in the same analysis that allo-HCT in CR1 was not recommended in patients with dmCEBPa. Regarding NPM1, Schlenk et al. indicated that patients with mutant NPM1 without FLT3-ITD had a favorable prognosis and did not benefit from allo-HCT [19]. However, an Eastern Cooperative Oncology Group trial indicated that the favorable effect of NPM1 mutations was restricted to patients who had co-occurring mutations in isocitrate dehydrogenase (IDH) [2], suggesting that possible heterogeneities in NPM1-positive patients may require the examination of background co-mutations [20,21,22]. NCCN and ELN both regard NPM1 and the allelic ratio of FLT3-ITD [23,24,25] as potent prognostic factors, and include them in risk stratification: mutated NPM1 without FLT3-ITD or with FLT3-ITD of low allelic ratio indicates low risk; mutated NPM1 and FLT3-ITD of high allelic ratio, and wild-type NPM1 without FLT3-ITD or with FLT3-ITD of low allelic ratio indicates intermediate risk; and wild-type NPM1 with FLT3-ITD of high allelic ratio indicates poor risk.
We previously showed that achieving second complete remission (CR2) and performing allo-HCT in CR2 were crucial for improving the prognosis after relapse [26]. Considering the risks of not only acute but late side effects [27], and possible changes in quality of life [28], the decision to perform allo-HCT in CR1 should be made by carefully evaluating the risk of relapse and the probability of being rescued after relapse [9]. In the abovementioned study [26], we only evaluated the cytogenetic risk and did not consider genetic heterogeneities. The aim of the present study was to evaluate the impact of FLT3-ITD, mutated NPM1, and dmCEBPa on outcomes of patients with cytogenetically intermediate-risk AML who were treated with chemotherapy alone in CR1, as well as the impact of genetic profiles on outcomes after the first relapse.
Patients and methods
Patients and mutational analysis
Adult patients with AML who had achieved CR1 were retrospectively registered in a nation-wide database that formed the basis of this study. We included patients aged 18–65 years who were diagnosed between 1999 and 2010 with intermediate- or unknown-risk AML according to the Southwest Oncology Group (SWOG) cytogenetic classification, and who had achieved CR1 with one or two courses of chemotherapy. We excluded patients with AML with myelodysplasia-related changes.
For eligible patients registered in the database, we retrospectively collected clinical information as well as bone marrow or peripheral blood samples obtained at diagnosis. Genomic DNA extraction and mutational analyses of FLT3-ITD, NPM1, and CEBPA were conducted as previously reported [22, 29]. Chemotherapy regimens were chosen at the discretion of physicians. Mutational status was examined retrospectively, so the mutational profile was not available when treatment strategy was determined. This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by institutional review boards of the National Cancer Center Hospital and all the participating institutions.
Statistical analyses
Distributions of patient characteristics between groups were compared using the chi-square test for categorical variables and the Wilcoxon rank-sum test for continuous variables. The unadjusted probabilities of overall survival (OS) and relapse-free survival (RFS) were estimated using Kaplan–Meier survival analysis. The log-rank test was used to compare OS and RFS among groups, and Gray's test was used to compare the cumulative incidence of relapse (CIR). To compare the OS of patients who received allo-HCT and those who did not, we performed landmark analyses by excluding patients who died within 150 days after relapse; 150 days was the median day for receiving allo-HCT from an unrelated donor registered in the Japan Marrow Donor Program [30]. A Cox proportional hazard regression model was used to estimate relative hazard ratios (HRs) for OS. The analyses were performed using SPSS software (IBM, SPSS Statistics 22) and EZR version 1.36 (Saitama Medical Center, Jichi Medical University), the latter of which is a graphical user interface for R (the R Foundation for Statistical Computing, version 3.3.2) [31]. For original data, please contact skurosaw@inahp.jp.
Results
Patients
A total of 480 patients with cytogenetically intermediate-risk AML who had achieved CR1 were retrospectively registered in the database. DNA extraction and analysis of FLT3-ITD status were successfully conducted in 296 patients (62%, Fig. 1). Most of the patients had received conventional anthracycline-AraC-based induction therapy (94% in 480 patients originally registered, and 95% in 296 with successful genetic data). Patients with available mutational data had a shorter follow-up period and a higher WBC count at diagnosis compared to those without available mutational data, but the two groups were similar in other characteristics including probabilities of OS [16]. In the 296 patients with cytogenetically intermediate-risk AML, 61 received allo-HCT in CR1. In further analyses, we included the 235 patients who were treated with chemotherapy alone during CR1 (Table 1); their median age at diagnosis was 51 years, the median follow-up was 3.2 years among survivors, and 152 of the 235 patients relapsed. After relapse, 77 patients (51%) received allo-HCT.
Mutational analysis
The distributions of FLT3-ITD, NPM1 mutations, and CEBPa in the 235 patients treated with chemotherapy alone and in the 152 who relapsed afterward are shown in Fig. 2. Forty-five patients (19%) had dmCEBPA. Of the 46 patients with FLT3-ITD (20%), 26 also had NPM1 mutations but did not have dmCEBPa (11%, NPM1 + /FLT3 +). In the other 20 patients with FLT3-ITD, 2 had dmCEBPa, while the remaining 18 were categorized as NPM1-/FLT3 + (8%). Of the 189 patients without FLT3-ITD, 60 had NPM1 mutations, and the 59 who did not also have dmCEBPa were categorized as NPM1 + /FLT3- (25%). The remaining 87 patients did not have FLT3-ITD, NPM1 mutations, or dmCEBPa, and were categorized as triple negative (37%). The characteristics of patients based on the presence and absence of FLT3-ITD, NPM1 mutations, and dmCEBPa are shown in Supplementary Table 1.
Similarly, the 152 patients who relapsed were categorized based on mutational profile (dmCEBPa, n = 20, 13%; NPM1 + /FLT3-, n = 32, 21%; triple negative, n = 64, 42%; NPM1 + /FLT3 + , n = 22, 14%; NPM1-/FLT3 + , n = 14, 9%) (Supplementary Table 2).
Outcomes after treatment with chemotherapy alone
As shown in Supplementary Fig. 1A, OS, RFS, and CIR in the 235 patients who were treated with chemotherapy alone during CR1 were 63%, 36%, and 61%, respectively, at 2 years after CR1. When stratified by the five groups of genetic profile groups, namely dmCEBPa, NPM1 + /FLT3-, triple negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + , OS, RFS, and CIR at 2 years after CR1 were 88%/74%/57%/46%/29%, 54%/48%/26%/31%/6%, and 44%/49%/71%/69%/87%, respectively (Fig. 3). Statistically significant differences in OS and RFS after CR1 were seen versus dmCEBPa in the triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups, but there were no significant differences between the dmCEBPa and NPM1 + /FLT3- groups (Supplementary Table 3). Similarly, the NPM1 + /FLT3- group had significantly better OS and RFS than the triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups. OS and RFS in the triple-negative group were significantly better than in the NPM1-/FLT3 + group, and were significantly worse than in the dmCEBPa and NPM1 + FLT3- groups. The NPM1-/FLT3 + group had significantly worse OS and RFS compared to the dmCEBPa, NPM1 + /FLT3-, and triple-negative groups; however, there was no significant difference in OS or RFS between the NPM1-/FLT3 + and NPM1 + /FLT3 + groups. OS values based on the presence or absence of FLT3-ITD, NPM1 mutations, and dmCEBPa are shown in Supplementary Fig. 1B.
Overall survival, relapse-free survival, and cumulative incidence of relapse after chemotherapy. Overall survival, relapse-free survival, and cumulative incidence of relapse in 235 patients treated with chemotherapy alone during CR1 are shown, stratified by five genetic profile groups: dmCEBPa, NPM1 + /FLT3-, triple negative, NPM1 + /FLT3 + , and NPM1-/FLT3 +
Outcomes after relapse based on genetic profiles at diagnosis
In 152 patients who relapsed, the median duration of CR1 was 247 days. Information on CR2 status was available for 133 of the 152 patients who relapsed after being treated with chemotherapy alone, and showed that 69 patients had achieved CR2 (52%). The rates of CR2 achievement were 85%, 48%, 52%, 41%, and 23%, respectively, in the dmCEBPa, NPM1 + /FLT3-, triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups. Patients with dmCEBPa showed a significantly higher rate of CR2 achievement compared to those without dmCEBPa. The CR2 rates based on the presence or absence of FLT3-ITD, NPM1 mutations, and dmCEBPa are shown in Supplementary Table 4.
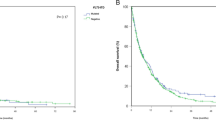
OS after the first relapse was 35% at 2 years (Supplementary Fig. 2A). OS after relapse in patients without FLT3-ITD was significantly better than in those with FLT3-ITD (41% vs 19% at 2 years after relapse, respectively, p = 0.002, Fig. 4A). On the other hand, OS after relapse was similar in patients without and with NPM1 mutations (34% vs 37%, p = 0.309). OS was significantly better in patients with dmCEBPa than in those without dmCEBPa, and in those without dmCEBPa, there was no significant difference in OS between patients with monoallelic CEBPa and wild type (61%, 40%, and 30%, p = 0.022). Among the five genetic profile groups (Fig. 4b), a significant difference in OS was seen between the dmCEBPa group and each of the triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups (dmCEBPa vs NPM1 + /FLT3-, p = 0.079). The NPM1-/FLT3 + group showed significantly inferior OS compared to the triple-negative and dmCEBPa groups (NPM1-/FLT3 + vs NPM1 + /FLT3-, p = 0.057), and there was no significant difference between the NPM1 + /FLT3 + and NPM1-/FLT3 + groups.
Mutational status at the time of relapse was obtained for 44 patients, and different profile was observed in 6 patients. Five of them showed triple-negative at the time of relapse (mutational status at diagnosis: two patients had dmCEBPa and one patient for each of NPM1 + /FLT3-, NPM1 + /FLT3 + , and NPM1-/FLT3 +), and one patient who had triple-negative at diagnosis showed dmCEBPa at the time of relapse. All of the six patients achieved CR2, and significant difference in OS was not seen between those with and without different mutational profile.
Role of allo-HCT after relapse and outcomes based on genetic profile at diagnosis
After relapse, 77 patients received allo-HCT; 24 patients received allo-HCT in the first relapse, 38 in CR2, and the other 15 were in other statuses. We compared OS after relapse in patients who received allo-HCT and those who did not using a landmark analysis at 150 days after relapse, which excluded 40 patients (6 of them had received allo-HCT). Patients who received allo-HCT after relapse had a significantly better OS compared to those who did not (55% and 24%, respectively, p < 0.001, Supplementary Fig. 2B). The advantage of allo-HCT after relapse was observed in most of the genetic profiles (Supplementary Fig. 2C). Patients with FLT3-ITD who received allo-HCT had a better OS than those who did not, but the difference was not statistically significant (53% vs 0%, p = 0.112); 11 out of 13 patients received HCT in the second relapse or later. In patients with dmCEBPa, OS after allo-HCT was 67%; however, the no-HCT group consisted of only two patients, and therefore there was insufficient statistical power to form a definitive conclusion.
Factors associated with OS after relapse
Table 2 shows the results of univariate and multivariate analyses for overall survival after relapse. In univariate analysis, older age (HR 1.03, 95% CI 1.01–1.04, p < 0.001), achievement of CR1 after two or more courses of remission induction (HR 1.97, 95% CI 1.17–3.29, p = 0.010), a shorter CR1 duration (< 8 months, HR 2.23, 95% CI 1.46–3.41, p < 0.001), and FLT3-ITD at diagnosis (HR 1.98, 95% CI 1.27–3.06, p < 0.001) were associated with a lower OS after relapse, while dmCEBPa at diagnosis was associated with better OS after relapse (HR 0.33, 95% CI 0.14–0.75, p < 0.001). In multivariate analysis, age, CR1 duration, FLT3-ITD, and dmCEBPA were independently associated with OS after relapse. When the administration of allo-HCT after relapse was added to the model, allo-HCT was independently associated with better OS after relapse, while FLT3-ITD as well as a shorter CR1 duration remained independently associated with worse OS. We also conducted a multivariate analysis that included five subgroups of genetic profile at diagnosis (Supplementary Table 5). Compared to dmCEBPA, the NPM1 + /FLT3 + and NPM1-/FLT3 + groups were independently associated with a lower OS after relapse, with or without performance of allo-HCT after relapse.
Discussion
The focus of this study was to assess the prognostic impact of FLT3-ITD, NPM1 mutations, and dmCEBPa on outcomes of patients with cytogenetically intermediate-risk AML after being treated with chemotherapy alone during CR1, as well as the impact of genetic profiles on outcomes after first relapse. Although we did not evaluate the allelic ratio of FLT3-ITD in this cohort, we presented survival probabilities and incidences of relapse after achieving CR1 based on the risk classification recommended by ELN [11] and NCCN [10], and we also demonstrated the relation between genetic profiles and the probabilities of achieving CR2 and survival after relapse.
Patients with dmCEBPa treated with chemotherapy alone showed significantly better OS and RFS compared to the triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups. The risk of relapse in the dmCEBPa group was higher than 35%, which according to ELN, is the value at which allo-HCT in CR1 should be considered [9]; however, patients with AML harboring dmCEBPa had a high rate of achieving CR2, and consequently had significantly better OS after relapse compared to the other genetic groups. Our sample size was too small to assess the role of allo-HCT after relapse in patients with dmCEBPa, but the favorable OS of 67% in patients who received allo-HCT after relapse may have contributed to the improved prognosis.
The favorable prognosis of the NPM1 + /FLT3- genetic profile group was previously shown [19], and this profile was categorized as favorable risk both by ELN and NCCN. The patients with NPM1 + /FLT3- in our cohort showed better OS and RFS than the triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups, and the NPM1 + /FLT3- group did not differ significantly from the dmCEBPa group. However, regarding the prognosis after the first relapse, the NPM1 + /FLT3- group demonstrated a significantly lower rate of achieving CR2 than the dmCEBPa group, and no significant difference in OS after relapse compared to the triple-negative, NPM1 + /FLT3 + , and NPM1-/FLT3 + groups. We also found that allo-HCT after relapse improved the outcomes in patients with mutated NPM1. Therefore, NPM1 + /FLT3- patients are categorized as favorable risk, but given their modest chance of achieving CR2 and the beneficial effect of allo-HCT after relapse, there may be an increased need to proactively consider the treatment strategy after the first relapse in this group, compared to the dmCEBPa group, including administration of allo-HCT in CR2.
In patients who were triple negative for FLT3-ITD, NPM1, and dmCEBPa, OS and RFS after achieving CR1 were significantly worse than patients with dmCEBPa and NPM1 + /FLT3-, and better than those with NPM1-/FLT3 + , which may reflect the intermediate risk of this group. In the NPM1 + /FLT3 + group, which is also categorized as intermediate risk both by ELN and NCCN, OS and RFS were not significantly different from those of the triple-negative group; at the same time, however, the survival rates in the NPM1 + /FLT3 + group were not different from those in the NPM1-/FLT3 + group. As for NPM1, the presence of minimal residual disease has been reported to be a powerful prognostic factor [32, 33], so we may be able to explore its use when choosing post-remission strategies in patients with mutated NPM1.
We confirmed that even after achieving CR1, patients with NPM1-/FLT3 + had a dismal prognosis when they were treated with chemotherapy alone, with a relapse risk of as high as 87%. As described in the Methods section, the presence or absence of FLT3-ITD was analyzed retrospectively, and therefore it did not affect the treatment decisions. After relapse, the rate of achieving CR2 in patients with FLT3-ITD was lower than in the other genetic profile groups, and there was a lower likelihood of performing allo-HCT in CR2. Thus FLT3-ITD was an independent factor associated with worse prognosis after relapse, and allo-HCT performed after relapse did not seem to adequately improve outcomes. As multiple studies have shown [34, 35], there is a need to consider more proactive and innovative strategies after diagnosis, including FLT3-inhibitors [36,37,38,39] in addition to allo-HCT in CR1 [16].
We believe that our analysis is informative, but it also has limitations that must be acknowledged. First, our study used a retrospective design and may therefore be susceptible to disadvantages such as patient selection bias. However, participating centers consecutively registered eligible patients. Furthermore, as mutational status was examined retrospectively, physicians did not have molecular results when treatment strategy was chosen. However, a concern about the heterogeneity in the post-remission treatment strategy including re-induction therapy after the first relapse that depended on physicians or institutions must be acknowledged. Second, the relatively small number of patients included in each molecular risk subgroup might have led to failures in distinguishing the prognostic difference of each genetic profile group. Third, we did not assess the allelic ratio of FLT3-ITD in this cohort, though it is presently included in risk stratification recommended from ELN and NCCN. We previously reported that mutated NPM1 with FLT3-ITD of low allelic ratio was not associated with favorable outcomes, and patients with this genetic profile benefited from allo-HCT in CR1 [40]. The impact of allele ratio of FLT3-ITD may need to be further clarified, and therefore we believe that the findings of our analysis will help guide post-remission therapeutic decisions. Lastly, this analysis was conducted using a nation-wide database from pre-FLT3 inhibitor era, therefore, its role in FLT3-positive AML need to be evaluated.
In conclusion, this study analyzed the mutation data of 235 patients who achieved CR1, and showed the survival probability and incidence of relapse using the five genetic profile groups defined by ELN and NCCN recommendations. After the first relapse, patients with dmCEBPa had a significantly higher rate of achieving CR2 and a remarkably better prognosis even after relapse. For patients with FLT3-ITD, we confirmed that the prognosis after treatment with chemotherapy alone was dismal, indicating that more proactive and novel treatment strategies, including FLT3 inhibitors, are needed. Our data, including the risk of relapse and rate of achieving CR2, show that screening for these risk-related mutations at diagnosis helps to better inform patients of their predicted clinical course after CR1, and is useful in facilitating effective therapeutic decision-making even after relapse.
References
Grimwade D, Ivey A, Huntly BJ. Molecular landscape of acute myeloid leukemia in younger adults and its clinical relevance. Blood. 2016;127(1):29–41.
Patel JP, Gonen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366(12):1079–89.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374(23):2209–21.
Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368(22):2059–74.
Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100(13):4325–36.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116(3):354–65.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998;92(7):2322–33.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96(13):4075–83.
Cornelissen JJ, Gratwohl A, Schlenk RF, Sierra J, Bornhauser M, Juliusson G, et al. The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat Rev Clin Oncol. 2012;9(10):579–90.
O’Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA, et al. Acute myeloid leukemia, Version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Comprehen Cancer Netw. 2017;15(7):926–57.
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S, et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood. 1999;93(9):3074–80.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98(6):1752–9.
Frohling S, Schlenk RF, Breitruck J, Benner A, Kreitmeier S, Tobis K, et al. Prognostic significance of activating FLT3 mutations in younger adults (16 to 60 years) with acute myeloid leukemia and normal cytogenetics: a study of the AML Study Group Ulm. Blood. 2002;100(13):4372–80.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99(12):4326–35.
Kurosawa S, Yamaguchi H, Yamaguchi T, Fukunaga K, Yui S, Wakita S, et al. Decision Analysis Of Postremission Therapy In Cytogenetically Intermediate-Risk Acute Myeloid Leukemia: The impact of FLT3 internal tandem duplication, nucleophosmin, and CCAAT/enhancer binding protein alpha. Biol Blood Marrow Transpl. 2016;22(6):1125–32.
Ahn JS, Kim JY, Kim HJ, Kim YK, Lee SS, Jung SH, et al. Normal karyotype acute myeloid leukemia patients with CEBPA double mutation have a favorable prognosis but no survival benefit from allogeneic stem cell transplant. Ann Hematol. 2016;95(2):301–10.
Pastore F, Kling D, Hoster E, Dufour A, Konstandin NP, Schneider S, et al. Long-term follow-up of cytogenetically normal CEBPA-mutated AML. J Hematol Oncol. 2014;7:55.
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358(18):1909–18.
Ley TJ, Ding L, Walter MJ, McLellan MD, Lamprecht T, Larson DE, et al. DNMT3A mutations in acute myeloid leukemia. N Engl J Med. 2010;363(25):2424–33.
Peterlin P, Renneville A, Ben Abdelali R, Nibourel O, Thomas X, Pautas C, et al. Impact of additional genetic alterations on the outcome of patients with NPM1-mutated cytogenetically normal acute myeloid leukemia. Haematologica. 2015;100(5):e196–e199199.
Wakita S, Yamaguchi H, Ueki T, Usuki K, Kurosawa S, Kobayashi Y, et al. Complex molecular genetic abnormalities involving three or more genetic mutations are important prognostic factors for acute myeloid leukemia. Leukemia. 2016;30(3):545–54.
Pratcorona M, Brunet S, Nomdedeu J, Ribera JM, Tormo M, Duarte R, et al. Favorable outcome of patients with acute myeloid leukemia harboring a low-allelic burden FLT3-ITD mutation and concomitant NPM1 mutation: relevance to post-remission therapy. Blood. 2013;121(14):2734–8.
Schlenk RF, Kayser S, Bullinger L, Kobbe G, Casper J, Ringhoffer M, et al. Differential impact of allelic ratio and insertion site in FLT3-ITD-positive AML with respect to allogeneic transplantation. Blood. 2014;124(23):3441–9.
Kim Y, Lee GD, Park J, Yoon JH, Kim HJ, Min WS, et al. Quantitative fragment analysis of FLT3-ITD efficiently identifying poor prognostic group with high mutant allele burden or long ITD length. Blood Cancer J. 2015;5:e336.
Kurosawa S, Yamaguchi T, Miyawaki S, Uchida N, Sakura T, Kanamori H, et al. Prognostic factors and outcomes of adult patients with acute myeloid leukemia after first relapse. Haematologica. 2010;95(11):1857–64.
Atsuta Y, Suzuki R, Yamashita T, Fukuda T, Miyamura K, Taniguchi S, et al. Continuing increased risk of oral/esophageal cancer after allogeneic hematopoietic stem cell transplantation in adults in association with chronic graft-versus-host disease. Ann Oncol. 2014;25(2):435–41.
Kurosawa S, Oshima K, Yamaguchi T, Yanagisawa A, Fukuda T, Kanamori H, et al. Quality of life after allogeneic hematopoietic cell transplantation according to affected organ and severity of chronic graft-versus-host disease. Biol Blood Marrow Transpl. 2017.
Wakita S, Yamaguchi H, Omori I, Terada K, Ueda T, Manabe E, et al. Mutations of the epigenetics-modifying gene (DNMT3a, TET2, IDH1/2) at diagnosis may induce FLT3-ITD at relapse in de novo acute myeloid leukemia. Leukemia. 2013;27(5):1044–52.
Hirakawa T, Kurosawa S, Tajima K, Yamazaki Y, Ikeda N, Kojima H, et al. Japan marrow donor program and its coordinating process: current situations. Jpn J Clin Hematol. 2018;59(2):153–60.
Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Ivey A, Hills RK, Simpson MA, Jovanovic JV, Gilkes A, Grech A, et al. Assessment of minimal residual disease in standard-risk AML. N Engl J Med. 2016;374(5):422–33.
Kayser S, Benner A, Thiede C, Martens U, Huber J, Stadtherr P, et al. Pretransplant NPM1 MRD levels predict outcome after allogeneic hematopoietic stem cell transplantation in patients with acute myeloid leukemia. Blood Cancer J. 2016;6(7):e449.
Badar T, Kantarjian HM, Nogueras-Gonzalez GM, Borthakur G, Garcia Manero G, Andreeff M, et al. Improvement in clinical outcome of FLT3 ITD mutated acute myeloid leukemia patients over the last one and a half decade. Am J Hematol. 2015;90(11):1065–70.
Schmid C, Labopin M, Socie G, Daguindau E, Volin L, Huynh A, et al. Outcome of patients with distinct molecular genotypes and cytogenetically normal AML after allogeneic transplantation. Blood. 2015;126(17):2062–9.
Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med. 2017;377(5):454–64.
Yamaura T, Nakatani T, Uda K, Ogura H, Shin W, Kurokawa N, et al. A novel irreversible FLT3 inhibitor, FF-10101, shows excellent efficacy against AML cells with FLT3 mutations. Blood. 2018;131(4):426–38.
Perl AE, Altman JK, Cortes J, Smith C, Litzow M, Baer MR, et al. Selective inhibition of FLT3 by gilteritinib in relapsed or refractory acute myeloid leukaemia: a multicentre, first-in-human, open-label, phase 1–2 study. Lancet Oncol. 2017;18(8):1061–75.
Usuki K, Sakura T, Kobayashi Y. Clinical profile of gilteritinib in Japanese patients with relapsed/refractory acute myeloid leukemia: an open-label phase 1 study. Cancer Sci. 2018;109(10):3235–44.
Sakaguchi M, Yamaguchi H, Najima Y, Usuki K, Ueki T, Oh I, et al. Prognostic impact of low allelic ratio FLT3-ITD and NPM1 mutation in acute myeloid leukemia. Blood Adv. 2018;2(20):2744–54.
Acknowledgements
The authors thank all the physicians who provided leukemia samples and clinical data. This work was supported by Grants from the National Cancer Research and Development Fund (29-A-14) and the Advanced Clinical Research Organization.
Author information
Authors and Affiliations
Contributions
SK designed the study, manipulated the data file, performed data analysis and wrote the manuscript; HY was primarily responsible for the laboratory work in this study and interpreted data; TY was primarily responsible for the study design, data analysis and interpretation of the data; KF and SY performed laboratory work; HK, KU, NU, MY, JT, IM, JK, HO, SY, HT, TS, SC, and JT provided leukemia samples and clinical data and also interpreted data; and KI and TF interpreted data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kurosawa, S., Yamaguchi, H., Yamaguchi, T. et al. The prognostic impact of FLT3-ITD, NPM1 and CEBPa in cytogenetically intermediate-risk AML after first relapse. Int J Hematol 112, 200–209 (2020). https://doi.org/10.1007/s12185-020-02894-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-020-02894-x