Abstract
Hemophagocytic lymphohistiocytosis (HLH) is a rare hyperinflammatory syndrome, which can manifest either secondary to a variety of underlying causes, or due to a primary genetic defect. Malignancy is the most common underlying disease in adults with HLH, with lymphomas being the most common malignancy. Lymphoma-associated hemophagocytic syndrome (LAHS) typically follows a rapidly progressive clinical course and is associated with poor prognosis. We herein present four patients with HLH associated with aggressive lymphoma. At initial presentation, the underlying etiology of the HLH was unclear. Two patients were eventually diagnosed with anaplastic large cell lymphoma, while the other two had diffuse large B cell lymphoma. Two of the patients experienced rapid clinical deterioration, one at diagnosis and the other at relapse, and both died prior to diagnosis of lymphoma despite HLH-directed therapy. These cases highlight the need for intensive management in adults with HLH without a clear etiology, especially in cases when lymphoma-associated HLH is suspected. We describe the current pitfalls in diagnosis and treatment of LAHS and discuss possible ways to improve patient management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemophagocytic lymphohistiocytosis (HLH) is a rare hyper-inflammatory syndrome, with a wide range of clinical presentations. The estimated yearly incidence of HLH is one per 800,000 people, and 1–10 per million children [1]. There is no pathognomonic feature for the diagnosis of HLH, but rather an accepted set of 8 clinical and laboratory diagnostic criteria supported by the pathological evidence of hemophagocytosis [2], as detailed in Table 1. The underlying etiologies for HLH include infectious and inflammatory disorders, as well as malignancies. Genetic or “primary” HLH refers to patients with defects in genes involved in cytotoxic granule exocytosis or function [3]. The frequency of each etiology varies according to the patient population, with age being a major determinant. Malignancy-associated HLH is more prevalent among adults, whereas congenital and infection-associated HLH are more common in the pediatric population [1]. When no etiology is detected HLH is considered idiopathic, accounting for 5–10% of the adult HLH population [4]. Table 2 lists some of the auxiliary tests suggested for a workup of an underlying disease.
Patients with HLH can present with signs and symptoms such as fever and splenomegaly, which can be related to an underlying pathological process, to the HLH itself or to both. Due to this myriad of non-specific clinical presentations, diagnosing HLH as well as its underlying pathological process can be puzzling. This is particularly true in the case of malignancy-associated HLH, which is generally associated with dismal prognosis [5, 6]. Hematological malignancies, including T cell lymphomas, B cell lymphomas and leukemias are the most common underlying malignancies representing up to 97% of cases in a recent literature review [6].
There are two key aspects of HLH management which require simultaneous consideration: first, identifying and treating the underlying disease; and second, treating the inflammatory process with HLH treatment protocols. The HLH-94 protocol includes a core of 8 weeks of induction treatment with dexamethasone and etoposide with subsequent steroid tapering off according to disease response [7]. Clinical response to both etoposide and steroids can be achieved when HLH is secondary to a hematologic malignancy, yet this can merely reflect the effectiveness of these agents in treating the HLH per se.
There is limited data to guide treatment of adults with HLH. One of the largest cohorts of adults with secondary HLH (n = 162) included 92 patients (56.8%) with hematologic malignancies, mainly non-Hodgkin lymphoma (NHL) (n = 57, 35.2%) [8]. Sixty-one of the 162 patients received treatment for the underlying cause of HLH without receiving HLH-specific treatment. Of the remaining 101 patients receiving HLH-specific treatment, 57.4% received only glucocorticoids (n = 19) or etoposide (n = 39), while 41.6% received both. 20% of the patients died within 1 month, with inferior survival for malignancy-associated HLH. Therefore, patients with malignancy-associated HLH have adverse short-term outcomes, suggesting that current management approaches are inadequate.
We herein present four patients with HLH as the presenting symptom of aggressive lymphoma. At initial presentation, the underlying etiology of the HLH was unclear. These cases highlight the need for intensive management in adults with HLH without a clear etiology, especially in cases when lymphoma-associated HLH is suspected.
Case presentation
Case 1
A 65-year-old female with no significant previous medical history and no relevant family history was admitted to an internal medicine ward due to fever during the previous two weeks. Following a thorough workup, seven of the eight diagnostic criteria for HLH were met as detailed in Table 1, including reduced natural killer cell (NK) activity of 16% and elevated soluble IL2 receptor (sIL2-r) level of 10,700 U/ml (normal range 300–2000 U/ml). At HLH diagnosis, the patient was hemodynamically stable without organ failure. Multiple diagnostic tests failed to reveal an underlying cause of HLH. Table 2 lists the steps which should be considered when investigating the underlying cause of idiopathic HLH, and shows which of them were performed in this and the other cases.
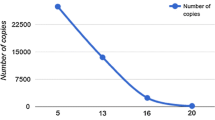
Serological tests were negative for various infectious as well as connective tissue diseases, including Epstein–Barr virus (EBV), cytomegalovirus (CMV) and human immunodeficiency virus (HIV). Total body computerized tomography (CT) was unremarkable apart from mild splenomegaly. Bone marrow biopsy revealed a lymphoid infiltrate which was deemed reactive by morphology and immunohistochemistry. The working diagnosis at this stage was idiopathic HLH, and the patient received dexamethasone at a dose of 10 mg/m2/day, followed by gradual steroid tapering off over a cumulative period of 10 weeks, with clinical and laboratory improvement. Due to good clinical status and rapid response to steroid treatment alone, etoposide or cyclosporine A (CSA) were not utilized at this stage. Figure 1 shows the major clinical events, diagnostic advances, treatment, and laboratory markers of disease activity along the timeline from when HLH was first suspected in this patient.
Diagnostic workup, treatment, and response for case 1. Figure shows HLH activity represented by sIL2R and ferritin on a timeline from hospital admission until death. Treatment and diagnostic workup for causes of HLH are shown on this timeline. Asterisk, tapering off steroids down to 2 mg twice a week. Double asterisk, ferritin units: ng/ml; sIL2R units: U/ml. BMB bone marrow biopsy, CSA cyclosporine A, CT Computed tomography, HLH hemophagocytic lymphohistiocytosis, PET CT positron emission tomography CT, Rx treatment, sIL2R soluble interleukin 2 receptor
Six weeks after complete cessation of steroid therapy HLH relapsed, with palpable splenomegaly, high lactate dehydrogenase (LDH) levels, worsening anemia and rising levels of sIL2-r. Upon relapse, she received retreatment with daily dexamethasone 10 mg/m2, weekly etoposide 100 mg/m2 and CSA according to the HLH-2004 protocol. The patient responded very well clinically to this treatment, and her blood count, biochemistry and sIL2-r normalized, although ferritin remained elevated. Repeat bone marrow biopsy was negative for an underlying lymphoproliferative disease, showing only reactive changes. In light of the presence of splenomegaly, a reactive lymphoid bone marrow infiltrate and relapsed adult HLH and in view of lack of an alternative cause, an underlying hematologic malignancy, especially lymphoma, was suspected. A fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT scan was performed, which demonstrated only a spleen size of 12 cm, with diffuse high uptake of FDG, without other signs of malignancy.
Three weeks later, while she was receiving dexamethasone at a dose of 2 mg twice a week, and CSA at therapeutic levels, the patient presented with an aggressive relapse of her symptoms, manifested by night sweats and fever. A laboratory workup showed elevated LDH [4800 U/L; upper limit of the norm (ULN) = 450], increased sIL2-r (4 × ULN), abnormal liver enzymes as well as anemia and thrombocytopenia. Renal failure also ensued, which continued to progress despite discontinuation of the CSA. Another thorough workup was performed, including PET/CT, infectious and autoimmune investigation, skin biopsy and bone marrow biopsy and aspiration; however, preliminary results failed to provide an underlying cause for the HLH. The patient was retreated with dexamethasone at a dose of 20 mg per day, and 4 biweekly doses of etoposide at a dose of 100 mg/m2 were given. Although lymphoma was suspected, due to the lack of histological proof of malignancy, chemotherapy was not administered and the patient continued to receive HLH-targeted treatment only. Her clinical condition deteriorated and she died within 19 days of admission and 225 days after initial presentation. An autopsy revealed diffuse large B cell lymphoma (DLBCL) of the spleen and bone marrow with ki67 of 70%. In addition, the bone marrow biopsy performed shortly before her death showed similar findings, but the report was finalized only after her death (Fig. 2a–c).
Bone marrow and spleen biopsy findings in Case 1. a BMB while alive with PAX5 immunostaining (× 20 magnification) showing large lymphoid cells with an interstitial pattern of infiltration. The B cells are positive for both CD20 and nuclear PAX5; b BMB PM with CD20 immunostaining (× 40) showing a BM infiltrated by large lymphoid cells (interstitial pattern of infiltration), highlighted by CD20; c Spleen biopsy PM with an HE stain (× 40) showing splenic tissue entirely infiltrated by large atypical lymphocytes. BMB bone marrow biopsy, HE hematoxylin and eosin, CD cluster of differentiation, DLBCL diffuse large B cell lymphoma, PAX5 paired box protein 5, PM postmortem, RBC red blood cells
Case 2
A 68-year-old male with a previous medical history of ischemic heart disease, celiac disease, gout and osteoporosis was admitted due to significant weight loss during the prior 2 months, fever and pancytopenia. His blood tests showed elevated LDH (6500 U/L, ULN = 450I/L) and high ferritin (19,642 ng/ml; ULN 306.8 ng/ml) as well as increases in total bilirubin (11 mg/dL; ULN 1.2 mg/dL), alkaline phosphatase (904 U/L; ULN 120 U/L) and alanine aminotransferase (2741 U/L; ULN 34 U/L). Coagulopathy was evident with prolonged PT and PTT (28.1 s ULN 13.5 s, and 52.7 s ULN 40 s, respectively) and low fibrinogen levels of 70 mg/dL (normal range 200–530 mg/dL). sIL2-r levels were normal. Total body CT including CT enterography revealed diffuse lymphadenopathy and isodense findings in the liver.
The presumptive diagnosis was HLH meeting 6/8 diagnostic criteria (Table 1) with a suspected underlying malignancy. High-dose dexamethasone and etoposide were started according to the HLH-94 protocol. Preliminary results of a biopsy obtained from an inguinal lymph node were suggestive of histiocytic sarcoma, rarely reported in association with HLH [9]. Despite 4 days of dexamethasone therapy, the patient’s clinical status rapidly deteriorated over several days, with multi-organ failure, culminating in cardiovascular collapse. The patient died within 11 days of hospital admission. The clinical course is shown in Fig. 3. A final pathological diagnosis from the inguinal lymph node obtained 3 days following the patient’s death was compatible with ALK1-negative anaplastic large cell lymphoma. Bone marrow and lymph node biopsy findings are shown in Fig. 4a–c.
Bone marrow and lymph node biopsy findings in Case 2. a BMB with HE stain (× 40 magnification) showing hypercellular marrow with extensive hemophagocytosis. Numerous histiocytes are seen, most of them showing intra-cytoplasmatic and “cigarette-packed” RBCs compatible with severe hemophagocytosis (denoted by arrows); b Inguinal lymph node with HE stain (× 20) showing fibro-fatty tissue involved in nodules of large atypical lymphocyte cells, some of them spindle shaped with a clear and wide cytoplasm and nuclear atypia; c Inguinal lymph node with CD30 immune staining, showing strong membranous staining of the large anaplastic cells. BMB bone marrow biopsy, CD cluster of differentiation, HE hematoxylin and eosin, RBC red blood cells
Case 3
A 64-year-old male with metastatic non-small cell lung carcinoma and no other significant comorbidities presented with 3 months of fever, lymphadenopathy and pancytopenia. The patient was diagnosed with lung cancer 2.5 years earlier and had been receiving treatment with carboplatin and pemetrexed up to 5 months prior to presentation with HLH. Chemotherapy was suspended prior to admission due to declining blood counts. Workup included total body CT, which revealed lymphadenopathy on both sides of the diaphragm and splenomegaly. Bone marrow biopsy revealed hemophagocytosis. CT-guided biopsy from a retroperitoneal lymph node showed a lymphoid aggregate. Due to worsening thrombocytopenia (nadir = 8000 K/µL) suspected as immune thrombocytopenic purpura, the patient was treated with intravenous immunoglobulins and high-dose dexamethasone with a short-lived increase in platelet counts. Repeat bone marrow examination revealed anaplastic large cell lymphoma. The patient received cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP) treatment, and achieved complete remission per PET-CT after 3 courses of chemotherapy.
Case 4
An 86-year-old male with marginal zone lymphoma (MZL) and no other significant medical history presented with weight loss, vomiting and melena. He was diagnosed with nodal MZL in an enlarged cervical lymph node earlier that year, which did not require therapy. At presentation, laboratory tests revealed pancytopenia with a neutrophil count of 440 cells/µL, hemoglobin of 9 g/dL and a platelet count of 90,000 cells/µL. The blood count 1 month earlier was normal. Alkaline phosphatase was elevated (137 U/L) and ferritin was 1079 ng/ml. Gastroduodenoscopy revealed an ulcerated lesion between the gastric antrum and pylorus, which was biopsied.
Two days later the patient developed high fever and a chest radiogram revealed a small pleural effusion with small infiltrates. Empirical antibiotic treatment with piperacillin–tazobactam was administered. An extensive workup including EBV and CMV serologies, blood cultures and bronchoscopy was unrevealing, and bone marrow biopsy was performed. The patient had reduced NK activity of 2.28% and sIL2-r level of 12,719 U/ml (normal range 300–2000 U/ml); ferritin rose to 2735 ng/dl. A presumptive diagnosis of malignancy-associated HLH was made, meeting 6/8 HLH criteria (Table 1).
Dexamethasone at a dose of 10 mg/m2/day was initiated, with the biopsy results still pending. A few days later the gastric biopsy pathology report revealed gastric mucosa involved by DLBCL, positive for Helicobacter pylori infection. The bone marrow biopsy also showed involvement by DLBCL. Treatment for Helicobacter pylori infection with pantoprazole, amoxycillin, clarithromycin and metronidazole was initiated. A marked clinical and laboratory improvement was noted. Subsequently, treatment with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) was initiated, and steroids were gradually tapered down. Despite clinical improvement after two courses of R-CHOP, severe pancyctopenia prevented completion of the chemoimmunotherpay regimen. During the tapering down of steroids, the HLH relapsed, accompanied by respiratory syncytial virus (RSV) respiratory infection. His clinical status rapidly deteriorated, and both ferritin and C-reactive protein (CRP) levels rose again (4634 ng/dl and 27 ng/dl, respectively). Despite high-dose steroids and broad spectrum antibiotic therapy, the patient’s neurologic and general clinical condition further deteriorated and he eventually died 71 days after his initial hospital admission.
Discussion
In the current report, we describe 4 patients with HLH as the presenting feature of aggressive lymphoma. Two of the patients were diagnosed with anaplastic large cell lymphoma and two with DLBCL. All four fulfilled the required diagnostic criteria for HLH. Patients 1, 2 and 4 received at least partial HLH-directed treatment with steroids, within 3 and 7 and 9 days after presentation with compatible signs and symptoms, respectively. In Case 3, treatment was delayed because an alternative cause of cytopenia was suspected. No alternative underlying cause of HLH was apparent when the initial HLH diagnosis was made. Temporary clinical improvement after the initiation of an HLH protocol was seen in Cases 1 and 4; however in Case 2 there was rapid clinical deterioration despite therapy. Importantly, in 2 of the 4 patients a definitive diagnosis of the underlying aggressive lymphoma was reached only postmortem.
The cases presented herein underscore some of the difficulties in managing adult patients with suspected lymphoma-associated hemophagocytic syndrome (LAHS). As exemplified by these cases, the main stumbling blocks in LAHS are delays in diagnosis and treatment of lymphoma, as well as delays in treatment of the HLH.
Diagnosing LAHS
High suspicion of underlying cancer in idiopathic HLH
Adult patients with suspected idiopathic HLH should have a thorough investigation to exclude malignancy [10] (Table 2), with lymphoma being the most prevalent malignancy [6]. This may prove especially prudent in the elderly population, as demonstrated in a large Japanese study which found that among HLH patients over the age of 60 years, 68% had lymphoma as an underlying cause [11]. This is in contrast to pediatric patients, who have a very low incidence of malignancy-associated HLH. Furthermore, the presence of one existing malignancy does not exclude the development of a new one, as illustrated in Cases 3 and 4. Similarly, the occurrence of infection does not rule out LAHS because infection might be a co-trigger for LAHS [12].
There have been several attempts to improve identification of certain subsets of adult HLH. Initially, Shimazaki et al and Takahashi et al proposed novel criteria for defining LAHS, largely relying on the HLH-2004 criteria, with the addition of LDH and D-dimers [13, 14]. Recently, additional attempts have been made to identify various categories of secondary HLH. The HScore aims to identify secondary HLH, especially malignancy-associated HLH, and includes 9 clinical (underlying immunosuppression, fever, organomegaly), laboratory (triglyceride, ferritin, serum glutamic oxaloacetic transaminase and fibrinogen levels, cytopenia) and histological (hemophagocytosis in bone marrow) variables [15]. Tamamyan et al reported diagnostic criteria specifically for malignancy-associated HLH, comprised of an extended set of 18 factors [16]. Other studies have focused on LAHS, showing that high serum sIL2-r /ferritin ratio [17] and higher levels of serum adenosine deaminase were associated with LAHS [18]. Collaboration between centers is imperative to improve and validate these scores for use in idiopathic adult HLH.
Delays in diagnosis of underlying lymphoma
Delayed diagnosis of the underlying aggressive lymphoma in patients with HLH might delay lifesaving treatment. If an underlying malignancy is left undetected, treatment of the HLH alone will not suffice, and remission may be short lived with aggressive relapses, as seen in Case 1 [5]. Diagnosis of LAHS is especially challenging since constitutional symptoms due to lymphoma might be falsely attributed to the HLH. Clinical deterioration can be rapid in these cases, and patients often die shortly after HLH presents or relapses, before effective treatment is provided for the underlying cancer. This was the case in two of our patients as previously described in the literature [19]. Importantly, as highlighted by the clinical course of Case 1, initial response to HLH treatment does not rule out the possibility of an underlying lymphoma, since this malignancy may respond transiently to steroids (with or without etoposide).
Expedite biopsies and perform repeated diagnostic tests
In a recent report, diagnosis of LAHS more than 20 days after presentation was associated with reduced overall survival, presumably due to delay in anti-lymphoma therapy [20]. Steroid treatment, alone or as part of one of the HLH-94 or HLH-2004 protocols, may be needed to provide effective, albeit temporary, relief of HLH signs and symptoms. However, steroid therapy (and etoposide) might mask an underlying lymphoma by reducing the diagnostic sensitivity of both laboratory studies and tissue biopsies. Therefore, when LAHS is suspected, definitive biopsies (i.e., adequate quantity and quality) should be performed as soon as possible. Case 1 exemplifies the importance of recurrent diagnostic tests because of sampling error and possible masking due to steroid therapy, since only the 3rd bone marrow biopsy eventually provided the diagnosis of lymphoma. More invasive procedures, such as diagnostic splenectomy, may be needed to confirm the suspicion for lymphoma in these patients, as might have been relevant in Case 1. Splenectomy also has therapeutic potential in relapsed idiopathic HLH [21].
Treating LAHS
Treat LAHS as early as possible
Another key concept in the management of LAHS is the admission of timely treatment for both the HLH and the underlying disease. A recent consensus review suggested a two-step approach to treatment of malignancy-associated HLH in adults [22]. First, the cytokine storm and T cell proliferation is targeted, initially with steroids, etoposide and IVIG. Salvage therapies include chemotherapy, such as liposomal doxorubicin, etoposide and methylprednisolone, or plasmapheresis, among others [23]. The second step is tumor-specific therapy targeting the underlying malignancy, once vital organ function has been restored.
Treatment of HLH in adults relies mostly upon studies and experience with the pediatric population. The HLH-94 protocol was used in a prospective study and includes a core of 8 weeks of induction treatment with dexamethasone and etoposide [7] with subsequent steroid tapering off according to disease response. This treatment resulted in 3 year overall survival (OS) of 55%, amongst 113 patients included in the original trial. Importantly, the study population included children aged 15 years or less, and bone marrow transplantation (BMT) was part of the treatment protocol.
Prospective studies involving adult HLH patients are rare. Shin et al investigated the CHOP chemotherapy regimen in 17 adult patients with HLH. Only seven of these patients had LAHS, all had lymphoma. Five patients had EBV-associated HLH and the remainder (n = 5) had HLH of unknown cause. Despite the heterogeneous etiologies of HLH, the overall response rate was 58.8%, with a similar response rate achieved in the EBV-related HLH subgroup (60%) [24]. Of note, 5 of the patients without an underlying lymphoma also responded to the CHOP combination. The small sample size and lack of a control group preclude definite conclusions.
New therapeutic options that are more precisely targeted to the underlying immuno-pathophysiology of HLH and are less cytotoxic are currently being tested in pilot studies. These include agents such as anti-interferon gamma monoclonal antibody [25], alemtuzumab, tocilizumab and the januse kinase (JAK)1/2 inhibitor ruxolutinib. The initial results from these studies are promising [26] and might be especially relevant to the elderly patient with LAHS.
Consider more aggressive management when underlying lymphoma is suspected
Due to the often rapidly progressive nature of LAHS as exemplified in Case 2, a more aggressive treatment strategy should be evaluated. One theoretical option and aim could be the earlier administration of chemotherapy to patients with a high index of suspicion of LAHS and an adverse prognosis, even before the establishment of a diagnosis of lymphoma. In cases of HLH without an overt underlying cause, a high index of suspicion for LAHS could be extrapolated from one of the new diagnostic scores discussed above [13, 15,16,17]. Amongst these patients, if no underlying etiology is discovered in first tier testing (Table 2), we believe a certain subgroup may benefit from a more aggressive management scheme. These are the patients with rapid clinical deterioration, which could be evaluated by severity indices analogous to the APACHE score in the intensive care unit [27].
In this subgroup (high suspicion; adverse prognosis), it seems a reasonable option to administer empirical chemotherapy, such as CHOP, directed at a possible underlying lymphoma, in addition to the etoposide which is incorporated in the HLH-2004 protocol. This controversial and non-evidence-based proposal could be considered on a case-by-case basis, especially when rapid relapses occur and when the patient deteriorates despite appropriate HLH treatment, as in Case 1. Of note, LAHS may present or recur with an accompanying infection, as in Case 4, and this may further complicate administration of chemotherapy. Given the gravity of the situation and lack of evidence, a shared and informed decision-making together with patients and their families, after outlining the pros and cons of this approach, is imperative.
If empirical chemotherapy is initiated, how many courses should be administered? Since there is currently no hard evidence to guide any specific regimen, treatment duration should be considered on a case-by-case basis. We propose several principles which could inform this decision. First, treatment strategy should be reevaluated after 1–2 courses of empirical chemotherapy, along with repeated diagnostic testing such as PET/CT, and biopsy of relevant sites. Second, if the HLH progresses despite two courses of lymphoma-directed empirical chemotherapy or if there is excessive treatment-related toxicity, chemotherapy discontinuation should be seriously considered. Third, if no new information to guide therapy is available, and the patient is improving clinically without significant treatment-related toxicity, completion of the standard 6 courses of CHOP chemotherapy recommended for lymphoma should be considered [28, 29]. Nonetheless, administering a full course of chemotherapy without a tissue diagnosis has important medico-legal implications and can lead to patient and physician anxiety. Therefore, we reiterate that empirical treatment should only be considered in patients with a high probability of lymphoma (as discussed above) and a dismal short-term (e.g. 30 day) prognosis, who consent to this approach after full disclosure of the lack of evidence guiding this strategy.
Conclusion
In an adult patient with HLH, a vigorous search for an underlying malignancy should be conducted, especially for occult aggressive lymphomas. Risk assessment models may help define the probability of LAHS and risk of clinical deterioration. In cases with a high index of suspicion for LAHS and adverse prognosis, we propose an approach of empirical treatment with at least 1–2 courses of chemotherapy on a case-by-case basis, even prior to histological confirmation of the malignancy. This strategy should be assessed prospectively as part of a multinational collaboration.
References
Ramos-Casals M, Brito-Zeron P, Lopez-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet. 2014;383:1503–16.
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J, Janka G. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31.
Janka GE, Lehmberg K. Hemophagocytic lymphohistiocytosis: pathogenesis and treatment. Hematol Am Soc Hematol Educ Progr. 2013;2013:605–11.
Schram AM, Berliner N. How I treat hemophagocytic lymphohistiocytosis in the adult patient. Blood. 2015;125:2908–14.
Machaczka M, Vaktnas J, Klimkowska M, Hagglund H. Malignancy-associated hemophagocytic lymphohistiocytosis in adults: a retrospective population-based analysis from a single center. Leuk Lymphoma. 2011;52:613–9.
Vick EJ, Patel K, Prouet P, Martin MG. Proliferation through activation: hemophagocytic lymphohistiocytosis in hematologic malignancy. Blood Adv. 2017;1:779–91.
Henter JI, Samuelsson-Horne A, Arico M, Egeler RM, Elinder G, Filipovich AH, Gadner H, Imashuku S, Komp D, Ladisch S, Webb D, Janka G, Histocyte S. Treatment of hemophagocytic lymphohistiocytosis with HLH-94 immunochemotherapy and bone marrow transplantation. Blood. 2002;100:2367–73.
Riviere S, Galicier L, Coppo P, Marzac C, Aumont C, Lambotte O, Fardet L. Reactive hemophagocytic syndrome in adults: a retrospective analysis of 162 patients. Am J Med. 2014;127:1118–25.
Veerakul G, Sanpakit K, Tanphaichitr VS, Mahasandana C, Jirarattanasopa N. Secondary hemophagocytic lymphohistiocytosis in children: an analysis of etiology and outcome. J Med Assoc Thai. 2002;85(Suppl 2):530–41.
Lehmberg K, Nichols KE, Henter JI, Girschikofsky M, Greenwood T, Jordan M, Kumar A, Minkov M, La Rosee P, Weitzman S. Study Group on Hemophagocytic Lymphohistiocytosis Subtypes of the Histiocyte S: Consensus recommendations for the diagnosis and management of hemophagocytic lymphohistiocytosis associated with malignancies. Haematologica. 2015;100:997–1004.
Ishii E, Ohga S, Imashuku S, Yasukawa M, Tsuda H, Miura I, Yamamoto K, Horiuchi H, Takada K, Ohshima K, Nakamura S, Kinukawa N, Oshimi K, Kawa K. Nationwide survey of hemophagocytic lymphohistiocytosis in Japan. Int J Hematol. 2007;86:58–65.
Lehmberg K, Sprekels B, Nichols KE, Woessmann W, Muller I, Suttorp M, Bernig T, Beutel K, Bode SF, Kentouche K, Kolb R, Langler A, Minkov M, Schilling FH, Schmid I, Vieth S, Ehl S, Zur Stadt U, Janka GE. Malignancy-associated haemophagocytic lymphohistiocytosis in children and adolescents. Br J Haematol. 2015;170:539–49.
Shimazaki C, Inaba T, Nakagawa M. B-cell lymphoma-associated hemophagocytic syndrome. Leuk Lymphoma. 2000;38:121–30.
Takahashi N, Nakahachi A. Clinicopathological characteristics of adult patients with lymphoma-associated hemophagocytic syndrome in Japan. Rinsho Ketsueki. 1999;40:96–8.
Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, Coppo P, Hejblum G. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66:2613–20.
Tamamyan GN, Kantarjian HM, Ning J, Jain P, Sasaki K, McClain KL, Allen CE, Pierce SA, Cortes JE, Ravandi F, Konopleva MY, Garcia-Manero G, Benton CB, Chihara D, Rytting ME, Wang S, Abdelall W, Konoplev SN, Daver NG. Malignancy-associated hemophagocytic lymphohistiocytosis in adults: relation to hemophagocytosis, characteristics, and outcomes. Cancer. 2016;122:2857–66.
Tsuji T, Hirano T, Yamasaki H, Tsuji M, Tsuda H. A high sIL-2R/ferritin ratio is a useful marker for the diagnosis of lymphoma-associated hemophagocytic syndrome. Ann Hematol. 2014;93:821–6.
Chen W, Zhang S, Zhang W, Yang X, Xu J, Qiu H, Zhang X, Li J. Elevated serum adenosine deaminase levels in secondary hemophagocytic lymphohistiocytosis. Int J Lab Hematol. 2015;37:544–50.
Kim JE, Kim CW, Park SH, Chi JG. Hemophagocytic syndrome associated with occult B-cell lymphoma: an autopsy case. J Korean Med Sci. 1998;13:77–80.
Chang Y, Cui M, Fu X, Han L, Zhang L, Li L, Li X, Sun Z, Wu J, Zhang X, Li Z, Nan F, Yan J, Sheng G, Zhang M. Lymphoma associated hemophagocytic syndrome: A single-center retrospective study. Oncol Lett. 2018;16:1275–84.
Jing-Shi W, Yi-Ni W, Lin W, Zhao W. Splenectomy as a treatment for adults with relapsed hemophagocytic lymphohistiocytosis of unknown cause. Ann Hematol. 2015;94:753–60.
Daver N, McClain K, Allen CE, Parikh SA, Otrock Z, Rojas-Hernandez C, Blechacz B, Wang S, Minkov M, Jordan MB, La Rosee P, Kantarjian HM. A consensus review on malignancy-associated hemophagocytic lymphohistiocytosis in adults. Cancer. 2017;123:3229–40.
Wang Y, Huang W, Hu L, Cen X, Li L, Wang J, Shen J, Wei N, Wang Z. Multicenter study of combination DEP regimen as a salvage therapy for adult refractory hemophagocytic lymphohistiocytosis. Blood. 2015;126:2186–92.
Shin HJ, Chung JS, Lee JJ, Sohn SK, Choi YJ, Kim YK, Yang DH, Kim HJ, Kim JG, Joo YD, Lee WS, Sohn CH, Lee EY, Cho GJ. Treatment outcomes with CHOP chemotherapy in adult patients with hemophagocytic lymphohistiocytosis. J Korean Med Sci. 2008;23:439–44.
Jordan M: A novel targeted approach to the treatment of hemophagocytic lymphohistiocytosis (HLH) with an anti-interferon gamma (IFNγ) monoclonal antibody (mAb), NI-0501: first results from a Pilot Phase 2 study in children with primary HLH. Blood. 2015;126: LBA-3.
Ehl S. Etoposide for HLH: the limits of efficacy. Blood. 2017;130:2692–3.
Salluh JI, Soares M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care. 2014;20:557–65.
d’Amore F, Gaulard P, Trumper L, Corradini P, Kim WS, Specht L, Bjerregaard Pedersen M, Ladetto M, Committee EG. Peripheral T-cell lymphomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v108–115.
Tilly H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, Lopez-Guillermo A, Walewski J, Andre M, Johnson PW, Pfreundschuh M, Ladetto M, Committee EG. Diffuse large B-cell lymphoma (DLBCL): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v116–125.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Pasvolsky, O., Zoref-Lorenz, A., Abadi, U. et al. Hemophagocytic lymphohistiocytosis as a harbinger of aggressive lymphoma: a case series. Int J Hematol 109, 553–562 (2019). https://doi.org/10.1007/s12185-019-02623-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-019-02623-z