Abstract
This observational study aimed to assess real-world treatment patterns and clinical outcomes for patients with chronic immune thrombocytopenia (ITP) currently being treated with eltrombopag or romiplostim after switching from corticosteroids, rituximab, or the alternate thrombopoietin receptor agonist (TPO-RA). The study examined the rationale for switching to TPO-RA therapy using aided responses. Dosing patterns were also analyzed before and after switching. Treatment outcomes were assessed through platelet counts at multiple time points including treatment initiation and after switching at the last office visit. A total of 280 patients were enrolled whose active therapy for ITP was replaced with either eltrombopag (n = 130) or romiplostim (n = 150). Efficacy-related issues (desired platelet count not achieved and/or lack of response to prior therapy) were the main drivers for therapy switching among all patients (54 % for eltrombopag vs. 57 % for romiplostim). Platelet counts at the last office visit showed improvement compared with counts at the initiation of either eltrombopag or romiplostim treatment. No significant differences were noted when comparing clinical outcomes between the eltrombopag and romiplostim treatment cohorts. Our results suggest that switching to the other TPO-RA may be beneficial if there is inadequate response to treatment with the initial TPO-RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune thrombocytopenia (ITP) is estimated to affect 60,000 adult patients in the United States [1]. It is characterized by low platelet counts and the attendant risk of bleeding. For patients with chronic ITP, the persistently low platelet counts present real and perceived risks for serious and even fatal bleeding events [2], and may therefore require emergency department visits and hospitalization [3]. Decreased platelet counts, disease symptoms, and treatment side effects have a notable impact on the overall quality of life for patients with ITP [2, 4–7].
Standard first-line therapy for the treatment of ITP includes corticosteroids, anti-D/anti-RhD immunoglobulin, or intravenous immunoglobulins (IVIg) [8, 9]. Corticosteroids are usually only given for a few months at a time, as patients are at risk of developing corticosteroid-related complications [9]. When first-line therapy is ineffective or results in side effects intolerable for the patient, various second-line drug, medical, or surgical therapies may be considered [9].
There are currently two thrombopoietin receptor agonists (TPO-RAs), eltrombopag and romiplostim, approved by the US Food and Drug Administration for the treatment of thrombocytopenia in patients with chronic ITP who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy [10–12]. Both therapies have demonstrated sustained platelet response with continuous administration regardless of splenectomy status. Romiplostim, a thrombopoietin peptide mimetic, and eltrombopag, a non-peptide mimetic, have different mechanisms of action and methods of administration. Romiplostim is administered once weekly as a subcutaneous injection and eltrombopag is administered once daily as a tablet [7, 13–15].
Although recommendations for the use of TPO-RAs are included in recent guidelines [8, 9], real-world treatment patterns of TPO-RAs have not been examined. Clinical outcomes and treatment responses among patients who switched from a prior ITP treatment to eltrombopag or romiplostim in current practice are lacking, and few comparisons of clinical outcomes between the two drugs have been made [16]. In the absence of randomized controlled trials comparing patients prescribed each TPO-RA or switched between TPO-RAs, it is critical to use clinical practice data to evaluate the treatment patterns and effectiveness in patients using eltrombopag and romiplostim. The purpose of this study was to characterize treatment use in real-world clinical practice for patients recently switched to eltrombopag or romiplostim from corticosteroids, rituximab, or the alternate TPO-RA. The objectives of this study were to better understand the rationale for switching to a TPO-RA, dosing patterns associated with switching, and to determine if clinical outcomes, assessed through platelet counts and reported symptoms, improve after a switch to either eltrombopag or romiplostim.
Materials and methods
Study design and selection of participants
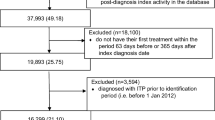
This was an observational retrospective medical chart review of patients with ITP who were currently being treated with a TPO-RA having switched from corticosteroids, rituximab, or the alternate TPO-RA. Physicians were selected from a representative sample [17] of oncology practices from the four census regions (Northeast, South, Midwest, and West) to ensure geographic diversity. Prior to study enrollment, investigators were pre-screened with a customized questionnaire. After the physician screening process, 42 oncology practices were responsible for selection of patient cohorts and chart data abstraction from patient medical records. A random selection method utilizing patient birth month as a selection variable was employed. Study investigators were provided with patient birth month as a random patient selection criterion to ensure representativeness of eltrombopag and romiplostim patients. For example, the physician study investigator was instructed to “select one patient chart for a patient currently being treated with eltrombopag whose birth month was either January, February, or March” or “select one patient chart for a patient currently being treated with romiplostim whose birth month was either July, August, or September”, etc. Data collection took place from January 3 to June 17, 2011.
Patients were included in the study if they (1) were ≥18 years of age at study enrollment; (2) had a diagnosis of ITP for at least 12 months; (3) switched from another ITP therapy (i.e., corticosteroids, rituximab, or the alternate TPO-RA); (4) were currently receiving eltrombopag or romiplostim for at least 4 weeks from the date of study enrollment; (5) had available medical history from ITP diagnosis through their most recent office visit; and (6) were capable of completing the self-administered general health and satisfaction questionnaires. Patients enrolled in clinical trials at the time of study initiation were excluded from the study. Patient cohorts were assigned 1:1 based on their current TPO-RA therapy (i.e., eltrombopag vs. romiplostim) and further stratified 1:1:1 based on immediate prior therapy (i.e., corticosteroids, rituximab, or the alternate TPO-RA). The study was HIPAA (Health Insurance Portability and Accountability Act of 1996) compliant, and human subject research exempt status was obtained from the New England Institutional Review Board.
Data collection
A customized patient case report form was used by physicians to record information abstracted from chart data. Key data elements collected in the patient case report form included: ITP patient profile and diagnosis information; ITP therapies received prior to, in combination with, and subsequent to TPO-RA use; TPO-RA treatment dosing and duration; platelet counts; platelet transfusion details; splenectomy status/details; chronic ITP-related emergency department visits; ITP-related hospitalizations; and current insurance coverage.
Outcomes
The rationale for switching to a TPO-RA was captured using aided responses. Responses were categorized as follows: efficacy (based on physician assessment), tolerability, patient preference, affordability, and benefit/risk of bleeding. Multiple responses per patient were allowed. Other outcomes of interest recorded were TPO-RA dosing and dosage changes, platelet counts reported at current TPO-RA initiation and up to the last office visit, bleeding symptoms reported after the switch to the current TPO-RA up to the last office visit, any emergency department visits, hospitalizations, IVIg and anti-D/anti-RhD immunoglobulin administration, and platelet transfusions reported after the switch to the current TPO-RA.
Statistical analysis
Patient demographic, clinical, and treatment-related characteristics were described and analyzed by treatment cohort using χ 2 and Fisher exact tests for categorical variables. Continuous variables were analyzed by treatment cohort using t tests and the one-way analysis of variance method. Tests for statistical significance were evaluated at a two-tailed P value of <0.05.
Results
Patient demographic and clinical characteristics
A total of 280 patients met the inclusion criteria (eltrombopag, n = 130; romiplostim, n = 150). Table 1 shows the demographic and clinical characteristics for the eltrombopag and romiplostim treatment cohorts. Both cohorts were comparable with respect to most patient characteristics. The mean time since ITP diagnosis was similar for both cohorts (eltrombopag, 1.5 years; romiplostim, 1.7 years; P = 0.36), and patients had an average of two prior therapies before switching to TPO-RA treatment. By design, equal proportions of patients in the eltrombopag cohort were receiving corticosteroid (n = 44), rituximab (n = 44), and romiplostim (n = 42) as their immediate prior therapy. Similar numbers were seen in the romiplostim cohort (corticosteroid, n = 58; rituximab, n = 48; eltrombopag, n = 44). The mean time on the immediate prior therapy before the switch was 14.4 weeks (median 7.5 weeks) for patients switching to eltrombopag and 15.1 weeks (median 7.1 weeks) for those switching to romiplostim (P = 0.81).
For patients taking the alternate TPO-RA as their immediate prior therapy, the mean time on romiplostim therapy before switching to eltrombopag was 15.8 versus 10.6 weeks on eltrombopag before switching to romiplostim (P = 0.08). Only one-half of patients were taking the highest indicated doses of eltrombopag or romiplostim before switching. Specifically, 50 % of patients who switched from eltrombopag to romiplostim were on 75 mg daily, and only 45 % of patients who switched from romiplostim to eltrombopag were on a dose of 5 µg/kg or greater weekly.
The time lapse between medication switch was longest for patients on immediate prior therapy with rituximab (52.2–70.1 days), followed by corticosteroids (25.3–37.5 days) and the alternate TPO-RA (romiplostim to eltrombopag, 7.2 days; eltrombopag to romiplostim, 10.8 days). Patients had been on their current TPO-RA for a similar number of weeks (18.6 weeks for eltrombopag patients and 17.4 weeks for romiplostim patients; P = 0.40).
Treatment decision
Current TPO-RA treatment, immediate prior therapy, and rationale for switching to TPO-RA treatment, which could include more than one response for any patient, are presented in Table 2. Overall, efficacy issues were the main motivations for switching to either eltrombopag or romiplostim. “Desired platelet count was not achieved and/or there was a lack of response to prior therapy” was the most frequently reported rationale for all patients (54 % for eltrombopag vs. 57 % for romiplostim), followed by “desired platelet count achieved but not sustained on prior therapy” (23 % for eltrombopag vs. 28 % for romiplostim). “Patient preference” was also cited as a reason for switching (eltrombopag, 32 %; romiplostim, 22 %).
For patients who switched from romiplostim to eltrombopag or from eltrombopag to romiplostim, the top rationales given were lack of efficacy and patient preference. There were 10 patients who switched to eltrombopag and 14 patients who switched to romiplostim that had both “desired platelet count was not achieved and/or there was a lack of response to prior therapy” and “desired platelet count achieved but not sustained on prior therapy” as reasons for switching, although such reasons were meant to be mutually exclusive.
Dosing for eltrombopag and romiplostim
Information regarding dosing for the eltrombopag and romiplostim cohorts is included in Table 3. Seventy-seven percent of eltrombopag patients received an initial dose of 50 mg daily and a similar proportion (79 %) received that dose most recently, regardless of prior treatment and prescribing information suggestions for initial dosing or dose titration. The majority of romiplostim patients (89 %) were given an initial dose of 1 mcg/kg weekly as per prescribing information. The majority reported titration to higher doses at their most recent office visit. Romiplostim patients had twice as many dose changes as eltrombopag patients (2.2 vs. 1.1, respectively; P < 0.001), with the mean time to that dose change significantly longer in eltrombopag patients compared with romiplostim patients (8.9 vs. 5.4 weeks; P = 0.004).
Efficacy measures
Descriptive information for platelet counts at current TPO-RA initiation and at the most recent office visit is reported in Table 4. Although platelet counts showed improvements compared with counts at TPO-RA initiation, there was no statistical difference in platelet counts between cohorts at the most recent office visit (P = 0.07). Patients reported few symptoms at their most recent office visit and there were no statistically significant differences between the cohorts. Platelet transfusions were rarely reported while on either TPO-RA treatment (eltrombopag, n = 2; romiplostim, n = 2). No patients required either IVIg or anti-D/anti-RhD immunoglobulin administration. No hospitalizations or emergency department visits were reported since the medication switch for either cohort.
Two post hoc sensitivity analyses were conducted among patients who were switched to the respective TPO-RA due to efficacy-related concerns while on the immediate prior treatment. Table 5 includes patients whose rationale for switching included either “desired platelet count not achieved and/or lack of response” or “platelet count achieved but not sustained”. Approximately 83 % of patients had a platelet count of <50 × 109/L at initiation of eltrombopag or romiplostim therapy. At the most recent office visit, the mean platelet counts in each cohort were >100 × 109/L, regardless of whether efficacy with the immediate prior therapy was never achieved or efficacy was not maintained over time. Table 6 includes patients whose immediate prior treatment was the alternate TPO-RA. At the time of initiation of the current TPO-RA, the majority of patients taking the alternate TPO-RA had a platelet count of <50 × 109/L. After switching to either eltrombopag or romiplostim from the alternate TPO-RA, mean platelet count improved.
Discussion
This study provides descriptive data on patients switching to TPO-RA treatment in a nationally representative population being treated in a real-world clinical practice setting. Patients included in the study recently switched to eltrombopag or romiplostim from corticosteroids, rituximab, or the alternate TPO-RA. Patients in this study were stratified 1:1:1 based on immediate prior therapy and therefore approximately one-third of patients had received each immediate therapy by design. In this study, efficacy was cited as the primary reason for switching to TPO-RA treatment. Mean platelet counts were at relatively low levels prior to switching to TPO-RA treatment, leaving patients at potentially increased risk for bleeding. After switching to a TPO-RA, the average platelet counts in each cohort were >100 × 109/L, regardless of whether efficacy with the prior treatment was never achieved or efficacy was not maintained over time. Additionally, patients in both cohorts reported few symptoms associated with thrombocytopenia at their most recent office visit. Furthermore, no patients required hospitalization or emergency department visits due to bleeding while on either therapy, none required IVIg or anti-D/anti-RhD immunoglobulin administration, and platelet transfusions were rare.
Patient preference was also commonly reported by physicians as a reason for switching to a TPO-RA. Although this study did not use preference elicitation methods to quantitatively measure preferences, some important factors to consider when evaluating the value of a medication from a patient’s perspective include side effect profile, dose schedule, and route of administration. Brown et al. [4] assessed patient-perceived and patient-reported treatment side effects, patient-perceived burden or bother, and need to reduce or stop treatment associated with these side effects among adult patients with chronic ITP. More than two-thirds of the patients surveyed reported experiencing side effects. Patients treated with corticosteroids reported more side effects with the highest magnitude of bother, which resulted in one-third of patients stopping or reducing treatment. Preference of dosing route or frequency of administration may have driven patient preference. Romiplostim is a subcutaneous weekly product administered in a physician’s office, whereas eltrombopag is an oral tablet self-administered daily. In addition to factors related to formulation, patient and physician preferences could also determine the therapy of choice. Physician comfort and experience along with patients’ prior history have been cited as possible reasons for medication preference [18].
Dosing regimens for both TPO-RAs are individualized based on platelet counts. The median starting doses for eltrombopag and romiplostim were 50 mg daily and 1 µg/kg weekly, respectively. Significantly more romiplostim patients (56 %) reported a dose change than eltrombopag patients (36 %). This is consistent with recommended dosing schedules in prescribing information for both products. At the most recent office visit, the median dose for eltrombopag was the same as the initial dose. The median dose at the most recent office visit for patients receiving romiplostim was 2 µg/kg. Per the product labeling for romiplostim, doses can be titrated to a maximum weekly dose of 10 µg/kg [10]. The dose of romiplostim at the most recent office visit was lower than what has been reported in other real-world and clinical trials, with average doses reported between 3.6 and 5.9 µg/kg [19, 20]. Even in patients who were switched from romiplostim to eltrombopag due to efficacy concerns, many patients did not receive the maximum dose prior to switching. Physician experience with both products and the patient’s disease profile may have influenced doses prescribed.
Our study suggests a benefit in switching to the other TPO-RA in patients who fail to respond to the initial TPO-RA. We found that the majority of patients taking the first TPO-RA, who reported a lack of efficacy as the rationale for switching to the second TPO-RA, improved their platelet counts after switching. This is consistent with other recent reports, case studies [21, 22], and a small study in France [16] that evaluated the merits of switching between the two TPO-RAs. These studies suggest that each product can be effective when taken by patients with a less-than-optimal response on the first TPO-RA prescribed [21, 22]. The French study, which was a retrospective evaluation of 45 patients switching between the two products [16], reported that most patients switched between products because of suboptimal platelet response or platelet count instability, although eight patients switching from romiplostim to eltrombopag did so because they desired an oral regimen. Variation in treatment efficacy, such that some patients selectively respond to only one TPO-RA, could also drive patient preference for switching between medications. Regardless of the rationale for switching, the study suggested that there is merit in switching between TPO-RAs to achieve efficacy and optimize the patient’s experience.
While this study provides important information on real-world treatment patterns of patients switched to TPO-RA treatment, limitations on data interpretation should be noted. Patients were not randomized to treatment groups in this retrospective study design, and current treatment choice may reflect consideration of multiple patient, physician, and disease characteristics, not all of which were measured in this study. In addition, rationale for switching patients to another therapy was captured using a set of aided responses. Acceptable platelet count thresholds used for determining “platelet count not achieved and/or lack of response” and “platelet count achieved but not sustained” were left to the treating physician’s discretion. Finally, data were collected via medical chart review, and the quality of data is vulnerable to how well medical charts were documented.
In conclusion, this study identified that switching to TPO-RA treatment from prior ITP treatment was largely driven by both lack of efficacy and patient preference. Platelet counts showed improvements compared with counts at TPO-RA initiation. No significant differences were noted when comparing clinical outcomes between the eltrombopag and romiplostim treatment cohorts. Our results also support the benefit of switching from one TPO-RA to the other among patients who fail to respond to treatment with the initial TPO-RA.
References
Feudjo-Tepie MA, Robinson NJ, Bennett D. Prevalence of diagnosed chronic immune thrombocytopenic purpura in the US: analysis of a large US claim database: a rebuttal. J Thromb Haemost. 2008;6:711–2.
McMillan R, Bussel JB, George JN, Lalla D, Nichol JL. Self-reported health-related quality of life in adults with chronic immune thrombocytopenic purpura. Am J Hematol. 2008;83:150–4.
Danese MD, Lindquist K, Gleeson M, Deuson R, Mikhael J. Cost and mortality associated with hospitalizations in patients with immune thrombocytopenic purpura. Am J Hematol. 2009;84:631–5.
Brown TM, Horblyuk RV, Grotzinger KM, Matzdorff AC, Pashos CL. Patient-reported treatment burden of chronic immune thrombocytopenia therapies. BMC Blood Disord. 2012;12:2.
Tarantino MD, Mathias SD, Snyder CF, Isitt JJ, Gernsheimer T, Young J. Impact of ITP on physician visits and workplace productivity. Curr Med Res Opin. 2009;26:319–28.
Mathias SD, Gao SK, Miller KL, Cella D, Snyder C, Turner R, et al. Impact of chronic immune thrombocytopenic purpura (ITP) on health-related quality of life: a conceptual model starting with the patient perspective. Health Qual Life Outcomes. 2008;6:13.
Cheng G, Saleh MN, Marcher C, Vasey S, Mayer B, Aivado M, et al. Eltrombopag for management of chronic immune thrombocytopenia (RAISE): a 6-month, randomised, phase 3 study. Lancet. 2010;377:393–402.
Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, Crowther MA. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190–207.
Provan D, Stasi R, Newland AC, Blanchette VS, Bolton-Maggs P, Bussel JB, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2009;115:168–86.
Nplate (romiplostim) for subcutaneous injection: US prescribing information. 2014. http://pi.amgen.com/united_states/nplate/nplate_pi_hcp_english.pdf. Accessed 17 June 2014.
Promacta (eltrombopag) tablets, for oral use: US prescribing information. https://www.gsksource.com/gskprm/htdocs/documents/PROMACTA.PDF. Accessed 7 June 2014.
Kuter DJ. The biology of thrombopoietin and thrombopoietin receptor agonists. Int J Hematol. 2013;98:10–23.
Kuter DJ, Bussel JB, Lyons RM, Pullarkat V, Gernsheimer TB, Senecal FM, et al. Efficacy of romiplostim in patients with chronic immune thrombocytopenic purpura: a double-blind randomised controlled trial. Lancet. 2008;371:395–403.
Bussel JB, Cheng G, Saleh MN, Psaila B, Kovaleva L, Meddeb B, et al. Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura. N Engl J Med. 2007;357:2237–47.
Kuter DJ, Rummel M, Boccia R, Macik BG, Pabinger I, Selleslag D, et al. Romiplostim or standard of care in patients with immune thrombocytopenia. N Engl J Med. 2010;363:1889–99.
Khellaf M, Vialard JF, Hamidou M, Cheze S, Roudot-Thoraval F, Lefrere F, et al. A retrospective pilot evaluation of switching thrombopoietic receptor-agonists in immune thrombocytopenia. Haematologica. 2013;98:881–7.
Firstmark, Inc. Physicians by specialty database: hematologist/oncologists. Campton, NH. www.firstmark.com/category_lists/doctors_list.htm. Accessed 18 June 2014.
Ghanima W, Godeau B, Cines DB, Bussel JB. How I treat immune thrombocytopenia: the choice between splenectomy or a medical therapy as a second-line treatment. Blood. 2012;120:960–9.
Bussel JB, Kuter DJ, Pullarkat V, Lyons RM, Guo M, Nichol JL. Safety and efficacy of long-term treatment with romiplostim in thrombocytopenic patients with chronic ITP. Blood. 2009;113:2161–71.
Janssens A, Tarantino MD, Bird R, Mazzucconi MG, Boccia RVV, Lopez-Fernandez MF, et al. Final results from an international, multi-center, single-arm study evaluating the safety and efficacy of romiplostim in adults with primary immune thrombocytopenia (ITP) (abstract). Blood. 2011;118:Abstract 3279.
Aoki T, Harada Y, Matsubara E, Suzuki T, Oyama T, Kasai M, et al. Thrombopoietin receptor agonists in refractory immune thrombocytopenia: differential responses to eltrombopag and romiplostim: a case report and possible explanations. J Clin Pharm Ther. 2012;37:729–32.
D’Arena G, Guariglia R, Mansueto G, Martorelli MC, Pietrantuono G, Villani O, et al. No cross-resistance after sequential use of romiplostim and eltrombopag in chronic immune thrombocytopenic purpura. Blood. 2013;121:1240–2.
Acknowledgments
This study was conducted in partnership with Medical Data Analytics, which received funding from GlaxoSmithKline for data collection, analysis, and interpretation of results. We would like to acknowledge the following individuals: Robert Simons, PhD, President, Global Health Economics and Outcomes Research (GHEOR) for analytical support; Lavanya Sudharshan, MS, Lead Analyst, Pharmerit International, for medical writing support. All listed authors meet the criteria for authorship set forth by the International Committee for Medical Journal Editors (ICMJE). D.K., P.F.W., and K.G. contributed to study design and reviewed data. C.M. contributed to data collection. K.G. and S.P. contributed to data analyses. C.M., K.G., S.P., K.G., M.W., P.F.W., and D.K. contributed to interpretation of results. S.P., D.K., K.D., and M.W. helped with writing of the manuscript. All authors revised the manuscript and approved its final contents.
Conflict of interest
David J. Kuter serves as a consultant to Amgen, ONO, Eisai, Kirin, and Suppremol. Kelly M. Grotzinger, Sara A. Poston, and Melea Ward are employees of GlaxoSmithKline. Peter Feng Wang is currently employed by Bristol-Myers Squibb. Katie L. Dawson is currently employed by Katie-Louise Dawson, LLC. Both authors were employees of GlaxoSmithKline at the time this study was conducted. Cynthia Macahilig is an employee of Medical Data Analytics.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kuter, D.J., Macahilig, C., Grotzinger, K.M. et al. Treatment patterns and clinical outcomes in patients with chronic immune thrombocytopenia (ITP) switched to eltrombopag or romiplostim. Int J Hematol 101, 255–263 (2015). https://doi.org/10.1007/s12185-014-1731-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1731-7