Abstract
Purpose of review
The goal of this manuscript is to provide an overview and analysis of bundled payment models for joint replacement and select spine procedures. Advantages and disadvantages of bundled payment models will be discussed.
Recent findings
In select populations, bundled payment models have been shown to reduce costs while maintaining satisfactory outcomes. These models have not been tested with complex patient cohorts, such as older adults with fragility hip fractures, and limited data exist with bundled payment analysis in spine procedures.
Summary
The reduction of healthcare costs, satisfactory patient outcomes, and favorable payments to healthcare systems can be achieved through bundled payments. Modifications of existing bundled payment models should be critically tested prior to implementation across higher risk populations. Bundled payment models will also require healthcare systems to define what services are necessary for an episode of care regarding a specific condition or disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Bundled Payments for Care Improvement (BPCI) initiative is comprised of four broadly defined models of care that link payments to multiple services that beneficiaries receive during an episode of care. Under the initiative, organizations enter payment models that include financial and performance accountability for episodes of care with a goal of higher quality and more coordinated care at a lower cost to Medicare [1]. This episode-based “cost containment” system was initially described in 1986 with Medicare’s prospective payment system (PPS), a model which encouraged hospitals to discharge Medicare patients in an expedited manner with incentives to utilize skilled nursing facilities and home health agencies for post-hospital care [2]. This model, however, led to adverse outcomes from patients being discharged “quicker and sicker” to these facilities [2]. These concerns led to the call for extension of PPS to assume financial responsibility for post-hospital care for cost containment. The current proposed mandate by the Centers for Medicare & Medicaid Services (CMS) now includes a Comprehensive Care for Joint Replacement (CJR) initiative, a 90-day bundled payment model for a given episode of care for Medicare beneficiaries undergoing elective total knee arthroplasty (TKA) or total hip arthroplasty (THA) [3•].
Current published perspectives support the need for a more cost effective and patient-centered healthcare delivery system that places value not only on access to care but the quality of care that patients receive from healthcare providers [1, 3•, 4••, 5••]. Several published studies assess the impact of bundled payment models for orthopedic procedures by measuring outcomes highlighting length of stay, readmission, cost effectiveness, perceived quality of care, and physician or hospital reimbursement [4••, 6,7,8]. These data suggest that bundled payment systems can be leveraged as tools to implement patient care pathways that ultimately provide comprehensive and coordinated perioperative patient care and effectively reduce cost, providing benefit to both the patient and healthcare system.
Additionally, existing literature notes potential unintended consequences arising from a strict mandate that does not account for a patient’s socioeconomic status, non-compliance, medical comorbidities, or severity of illness during an episode of care, all of which have demonstrated a negative impact on outcomes. Furthermore, if the primary aim of the BPCI is to ensure accountability for quality and cost of care, institutions will then be responsible for patient outcomes, some of which may extend outside the scope of the target initiative. An example of a misapplication of the BPCI model would be the implementation of bundled payments for hip fractures treated with joint replacement without a payment adjustment compared with elective joint replacement. In a recent editorial, Joseph Bernstein uses “Learned Helplessness” to describe the accountability that extends outside the control of the bundled payment system’s intent [9]. He evaluates the current data and reported outcomes that focus primarily on bundled payment systems for joint replacement procedures, hip fractures, and spinal fusion procedures. He also describes the despair that arises when one is held accountable for adverse events that are beyond control of the care team. These payment models can result in misalignment of goals of care such that suboptimal procedures are selected to avoid classification into a bundled payment.
Bundled payments in total joint arthroplasty and hip fractures
Total joint replacement for hips and knees is the most common inpatient surgery for Medicare beneficiaries and can require lengthy recovery and rehabilitation periods. In 2014, there were more than 450,000 such procedures (Table 1), costing more than $7 billion for the hospitalizations alone [3•]. Despite the high volume of these surgeries, quality and costs of care for hip and knee replacements still vary greatly among providers and hospitals [3•]. The CJR model aims to support more efficient and higher quality care for beneficiaries undergoing these procedures while standardizing payments.
The CJR model incentivizes increased coordination of care among the many healthcare providers involved in a patient’s care by holding participant hospitals financially accountable for the quality and cost of a CJR episode of care. The episode of care begins with the beneficiary’s admission to a participant hospital with a discharge diagnosis that falls under Medicare severity diagnosis-related groups (MS-DRG) 469 (major joint replacement or reattachment of lower extremity with major complications or comorbidities) or 470 (major joint replacement or reattachment of lower extremity without major complications or comorbidities). The episode ends 90 days post-discharge, thereby including the primary recovery period of beneficiaries. Contained within this episode are all related items and services paid under Medicare Part A and Part B for all fee-for-service beneficiaries except certain exclusions such as systemic infectious diseases, neurologic diseases, pregnancy-related conditions, and malignancies [3•].
Total joint bundled payments: advantages
Previous publications have highlighted the advantages of the bundled payment system for total joint replacement [5••, 8, 10]. Value-based payment and alternative payment models incentivize the provision of efficient, high quality, patient-centered care through financial penalties and rewards [11, 12]. In the BCPI model, the financial burden is transferred from commercial insurers and government sponsored payers to healthcare systems and providers. The primary benefits of this model are cost reductions and higher quality of care through comprehensive medical management [11].
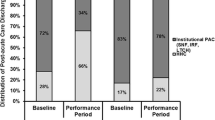
Early results of a prospective bundled payment program have shown 97% patient satisfaction and 22% lower medical costs compared with traditional fee-for-service models [8]. Additional research evaluated whether BPCI was associated with a greater reduction in Medicare payments without loss of quality of care for lower extremity joint (primarily hip and knee) replacement episodes initiated in BPCI-participating hospitals [4••]. In the first 21 months of the BPCI initiative, Medicare payments declined more for lower extremity joint replacement episodes provided in BPCI-participating hospitals than for those provided in comparison hospitals without a significant change in quality outcomes. The BPCI mean Medicare episode payments were $30,551 at baseline and declined to $27,265 in the intervention period [4••], as compared with non-BPCI hospitals from $30,057 baseline period to $27,938 [4••]. The mean $1166 payment decline was primarily due to reduced use of institutional post-acute care, without changes in readmission rates, mortality, or other quality measures [4••].
Current limitations of this model include: (1) data limited to the institutions involved, (2) regional variation of patient demographics, and (3) the often retrospective and short-term outcomes reported. We are unable to predict the sustainability of this payment model and its long-term effects, especially the long-term economic feasibility for payers and providers as well as the outcomes of quality of care for every patient that undergoes joint replacement. Preliminary data does highlight that value-based models are seemingly more cost effective and may provide a higher standard for quality care than the current fee-for-service model. In other words, BCPI may be an answer but not the entire answer to better comprehensive patient-centered care.
Total joint bundled payments: challenges
There have been several perceived and demonstrated challenges to bundled payment system implementation. In addition to the incentives currently used to provide comprehensive patient-centered care at the lowest possible cost, the potential also exists to incentivize withholding care [5••]. The current fee-for-service model could influence healthcare providers to utilize healthcare resources that increase reimbursement, whereas the bundled payment model may decrease healthcare resource utilization for cost containment. Unfortunately, costly diagnostics or further interventions may be withheld in a bundled payment model to avoid financial disincentives to the organization or provider. Additional costs per episode of care may be incurred by patients undergoing joint replacement with comorbidities associated with higher complication rates and subsequent increased length of stay and readmissions. Recent studies have called for adjustments in the alternative payment model for certain patient populations such as those with higher risk for complications and increased hospitalization [13, 14].
Patients undergoing elective joint arthroplasty with a Charlson comorbidity index of greater than five were associated with prolonged hospitalization; chronic kidney disease and chronic obstructive pulmonary disease were independent risk factors contributing to increased length of stay and higher readmission rates [13]. The 30-day readmissions due to these factors reduced profit and contribution margins by nearly 40% [13].
Lower socioeconomic status has also been correlated with increased resource utilization following total joint replacement. One study utilized the Michigan Arthroplasty Registry Collaborative Quality Initiative database to review a consecutive series of 4168 primary TKA and THA patients over a 3-year period [14]. Demographics, medical comorbidities, length of stay, discharge destination, and readmission rates were compared between two groups stratified by socioeconomic status. A lower socioeconomic status was an independent risk factor for a longer hospital length of stay, higher likelihood of discharge to a rehabilitation facility, and higher readmission rate within 90 days [14].
Furthermore, a bundled payment system is susceptible to unintended consequences such as bias and discrimination against certain patient populations with a higher financial risk for providers. In the absence of significant risk adjustment of bundled payments, providers may select low-risk patients and avoid those with higher risks (and costs) [10, 15]. Therefore, risk stratification must be considered for reimbursement fees per episode of care for higher risk patient populations.
Spine bundled payments: why they work better than in total joint arthroplasty
In contrast to joint replacement BCPI, bundled payments in spine surgery are neither as well defined nor as well investigated, but may ultimately prove to be a more cost effective initiative.
An analysis of Medicare data over a recent 10-year period shows that the incidence of spinal fusion has increased at a higher rate than total joint arthroplasty. Of greater concern is that hospital charges for this procedure experienced a 3.3-fold increase compared with 2.3-fold increases in charges associated with joint replacement, resulting in a $33.9 billion national expense in 2008 [16]. This disproportionate rise in costs for spinal fusion is likely due to a variety of factors, including costs associated with new implants, new alternatives in bone grafting, and the approval of bone morphogenetic protein usage in clinical practice.
An expected result of a bundled payment reimbursement system for spine fusion would be decreased cost of spine implants and inter-physician cost variations. By requiring vendors to meet a uniform price for each spinal implant to remain on an “approved devices” list within hospital systems, some centers have demonstrated savings of $950 per single level anterior cervical discectomy and fusion (ACDF) [17]. Bundled payments may also affect the location of and disposition following the procedure. A shift in case volume will continue towards ambulatory surgical centers. Early data suggest that, with the correct indications and patient population, decreases in cost, morbidity, and re-operation are observed [18].
Bundled payment models may stimulate further technology in spine surgery, driving further developments in minimally invasive procedures that can be done safely and with less morbidity, thereby lowering cost of care in a 90-day period.
A recent analysis of Medicare reimbursement payments of 4506 patients receiving one-and two-level ACDF procedures over a 7-year period demonstrated that complications were relatively infrequent, accounting for only 0.7% of the total 90-day reimbursement fund [19••]. Furthermore, only 3.1% of reimbursements were allocated for physical therapy, skilled nursing facilities, or home health services (compared with 36% in TKA), resulting in a total 90-day mean reimbursement of $15,417 ± $947 (Table 2) [19••, 20]. These statistics, however, represent only one procedure used in the treatment of one region of the spine.
Spine bundled payments: why they may not work as well as in total joint arthroplasty
With the option of decompression and/or fusion of 29 vertebral levels, there is a huge number of possible procedures, limiting the homogeneity and reproducibility required for data collection, analysis, and ultimately success of a bundled payment system. A recent study evaluating reimbursement payments as a function of MS-DRG noted that, even within the same MS-DRG, variations in payments range from $87,000 to $253,000 [20].
Most studies for bundled payments have examined the MS-DRG. The MS-DRG is somewhat of a misnomer because it is not a “diagnosis” that is being assessed but rather a selection of procedures to which associated diagnoses are attached. For example, MS-DRG 491 is defined as a “back or neck procedure except spinal fusion without comorbidity or major comorbidity” [21]. MS-DRG 460 is defined as a “spinal fusion except cervical without major comorbidity” [21]. If the payor’s goal is to obtain cost effective spinal surgery through standardization, then applying bundled payments in relation to a specific MS-DRG may be flawed. For example, it is currently at the surgeon and patient’s discretion whether the ICD-9 738.4 (acquired spondylolisthesis) is treated with MS-DRG 460 or 491. The variability of MS-DRG options for a specific diagnosis, therefore, allows wide latitude for the surgeon’s choice of treatment based upon individualized patient care. This presents standardization and reproducibility problems when the goal is to pay for the most cost effective care for a certain diagnosis.
Spine bundled payments: advantages
Despite the limitations noted above, several medical centers and health organizations have initiated episodic-based reimbursement models for spine surgery. A recent review of 12 centers assessed the reasons for implementation of bundled payment models [22]. The most common motivation for bundled payment reimbursement was increased volume from large employers such as Walmart and third-party administrators. Pre-screening mechanisms, which increase the percentage of clinic patients who require surgery, and the prospect of profit sharing between physicians and hospitals when efficiency improvement efforts were met, were two other reasons for bundled payment implementation [22]. Additional considerations include negotiations with vendors for implant, graft, and instrumentation pricing to drive down overall cost of surgery.
Spine bundled payments: disadvantages
Like joint replacement models, there are several drawbacks associated with bundled payments, and these may be further magnified in spine surgery. Although bundled payments incentivize lower total cost of care for a single episode, there has been no demonstration in reduction of total procedural volume, and indications for surgery are excluded from bundled payment models [22]. Because multiple procedures and techniques exist for the treatment of the same diagnosis, surgeons could be influenced to recommend an alternate procedure with less direct costs or increased reimbursement [6]. For example, surgeons may treat a patient with cervical arthroplasty instead of an ACDF due to differences in 30-day direct costs ($19,425 vs. $26,095) [22].
As bundled payments continue to be integrated into the reimbursement landscape, patient selection will become an increasingly important consideration. If bundled payments become the primary means of reimbursement, healthcare systems will be forced to calculate financial risk based on patients’ demographics and comorbidities. Some spine programs already have explicit guidelines which exclude smokers, patients with body mass index >40, and patients with a prior lumbar fusion [22]. These financial risk calculations have inherent ethical implications.
Conclusions
In summary, bundled payment models may help control healthcare costs for commonly performed surgical procedures, but patient comorbidities, socioeconomic factors, and payment inconsistencies limit universal application of these models. Early data has shown that costs can be controlled without compromising quality of care in bundled payment models involving hip and knee arthroplasty, but potential dangers such as denial of care or less effective treatments in higher risk patients to avoid bundling requires further research. Limited data is available for spine bundled payments specific to ACDF, but has also shown promise in cost reduction while maintaining high quality outcomes. Reimbursement models should reflect not only the variable breakdown of costs by procedure associated with an episode of care, but also the risk assumed by the healthcare system of what costs can be influenced and those that are less likely to change. This information will enable healthcare systems to critically evaluate cost allocation across an episode of care and identify areas for improvement. Reimbursement models should also include payment incentives to manage higher risk populations, potentially at larger centers where multidisciplinary care is available.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
(2016) Bundled Payments for Care Improvement (BPCI) Initiative: General Information | Center for Medicare & Medicaid Innovation. In: Innovation.cms.gov. https://innovation.cms.gov/initiatives/bundled-payments/. Accessed 25 Oct 2016.
Neu CR, Palmer A, Henry DP, Olson GT, Harrison S. Extending the Medicare prospective payment system to posthospital care. Planning a demonstration (PDF). Santa Monica: RAND Corporation; 1986. Retrieved 2010-03-11
• (2016) Comprehensive Care for Joint Replacement Model | Center for Medicare & Medicaid Innovation. In: Innovation.cms.gov. https://innovation.cms.gov/initiatives/CJR. Accessed 25 Oct 2016. Describes the CJR bundled payment initiative from CMS .
•• Dummit LA, Kahvecioglu D, Marrufo G, Rajkumar R, Marshall J, Tan, Press MJ, Flood S, Muldoon LD, Gu Q, Hassol A, Bott DM, Bassano A, Conway PH. Association between hospital participation in a Medicare bundled payment initiative and payments and quality outcomes for lower extremity joint replacement episodes. JAMA. 2016; doi:10.1001/jama.2016.12717. Early results of >29,000 Medicare beneficiaries who underwent joint replacement surgery at BPCI-participating hospital demonstrating reduced payment without significant change in quality
•• Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction Clin Orthop Relat Res 2014; 472(1): 188–193. Published online 2013 May 7. doi: 10.1007/s11999-013-3034-3. Describes cost components of total joint arthroplasty and implications of these costs in a bundled payment model .
Clair AJ, Evangelista PJ, Lajam CM, Slover JD, Bosco JA, Iorio R. Cost analysis of total joint arthroplasty readmissions in a bundled payment care improvement initiative. J Arthroplast. 2016; doi:10.1016/j.arth.2016.02.029.
Schwartz AJ, Fraser JF, Shannon AM, Jackson NT, Raghu TS. Patient perception of value in bundled payments for total joint arthroplasty. J Arthroplast. 2016; doi:10.1016/j.arth.2016.05.050.
Expanded collaboration provides BCBSNC customers with 10–20 percent savings on hip replacement surgeries. Blue Cross and Blue Shield of North Carolina website. http://mediacenter.bcbsnc.com/ news/expanded-collaboration-provides-bcbsnc-customers-with −10-20-percent-savings-on-hip-replacement-surgeries. Published February 6, 2014.
Bernstein J. Not the last word: learned helplessness and Medicare’s bungled bundled payment program. Clin Orthop Relat Res. 2016 Sep;474(9):1919–23. doi:10.1007/s11999-016-4935-8.
Hussey PS, Mulcahy AW, Schnyer C, Schneider EC. Closing the quality gap: revisiting the state of the science (vol. 1: bundled payment: effects on health care spending and quality). 2012 Aug;(208.1):1–155.
Alternative Payment Model Framework and Progress Tracking (APM FPT) Work Group. Alternative Payment Model (APM) Framework. https://hcp-lan.org/groups/alternative-payment -model-apm-framework-and-progress-trackingwork-group/.
Rosenthal MB. Beyond pay for performance—emerging models of provider-payment reform. N Engl J Med. 2008 Sept 18;359(12):1197–200.
Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee GC. Should all patients be included in alternative payment models for primary total hip arthroplasty and total knee arthroplasty? J Arthroplast. 2016 Sep;31(9 Suppl):45–9. doi:10.1016/j.arth.2016.03.020.
Courtney PM, Huddleston JI, Iorio R, Markel DC. Socioeconomic risk adjustment models for reimbursement are necessary in primary total joint arthroplasty. J Arthroplast. 2016; doi:10.1016/j.arth.2016.06.050.
Medicare Payment Advisory Commission. Report to the Congress: reforming the delivery system. MedPAC. Washington, DC: Jun; 2008.
Rajaee SS, Bae Hw Fau-Kanim LEA, Kanim Le Fau - Delamarter RB, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. (1528–1159 [Electronic]).
Oren J, Hutzler LH, Hunter T, Errico T, Zuckerman J, Bosco J. Decreasing spine implant costs and inter-physician cost variation. Bone Joint J. 2015 Aug;97-B(8):1102–5.
McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus. 2015 Dec;39(6):E9.
•• Virk SS, Phillips FM, Khan SN. Reimbursement related to a 90-day episode of care for a one or two-level anterior cervical discectomy and fusion. J Bone Joint Surg Am. 2016;98(16):1378–84. First peer-reviewed published report on Medicare bundled payment models for one- or two-level ACDF procedures
Ugiliweneza B, Kong M, Nosova K, Huang KT, Babu R, Lad SP, Boakye M. Spinal surgery: variations in health care costs and implications for episode-based bundled payments. Spine (Phila Pa 1976). 2014 Jul 1;39(15):1235–42. doi:10.1097/BRS.0000000000000378.
Draft ICD-10-CM/PCS MS-DRGv28 Definitions Manual. Draft ICD-10-CM/PCS MS-DRG v28 Definitions Manual. Centers for Medicaid and Medicare Services, n.d. Web. 22 Nov. 2016.
Kazberouk A, McGuire K, Landon BE. A survey of innovative reimbursement models in spine care. Spine (Phila Pa 1976). 2016 Feb;41(4):344–52. doi:10.1097/BRS.0000000000001212.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tadhg O’Gara is a board member for FirstLineMeds Inc.
Cynthia L. Emory reports grants from Orthopedic Research and Education Foundation, Golfers Against Cancer, Musculoskeletal Transplant Foundation, and IlluminOss Medical, Inc. She is a consultant for BoardVitals.
All other authors declare no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Orthopaedic Health Policy
Rights and permissions
About this article
Cite this article
Sullivan, R., Jarvis, L.D., O’Gara, T. et al. Bundled payments in total joint arthroplasty and spine surgery. Curr Rev Musculoskelet Med 10, 218–223 (2017). https://doi.org/10.1007/s12178-017-9405-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-017-9405-8