Abstract
Purpose of Review
Traditional surgical ablation and endocardial catheter ablation have historically been the primary ablation approaches for treating atrial fibrillation (AF) concomitantly with another surgical procedure or as a standalone procedure, respectively. In the last several years, hybrid epicardial-endocardial ablation utilizing a subxiphoid approach for epicardial left atrial ablation combined with endocardial catheter ablation (converge procedure) has been an emerging hybrid approach to standalone AF catheter ablation. The procedure was developed as a treatment option for patients with advanced AF in which traditional catheter ablation had limited efficacy and relief. The technique combines the benefits of both endocardial and epicardial ablation in a minimally invasive manner to provide a comprehensive lesion set characterized by durable transmural lesions. The Convergent technique involves a minimally invasive surgical addition to standard endocardial ablation. Identifying appropriate patients for this approach and optimizing procedural details will assist clinicians in decision-making. In this review we discuss optimization of patient selection for the convergent procedure and tools and techniques to maximize workflow and clinical outcomes.
Recent Findings
The dual epicardial-endocardial nature of hybrid may be in part why the hybrid convergent procedure has been successful in treating even longstanding persistent AF (LSPAF), which was previously thought to be permanent with high recurrence rates that have not improved despite advances in catheter ablation technology (Winkle et al., 2023). As shown in randomized and propensity score-matched cohorts, effectiveness rates for hybrid convergent ablation are improved compared to endocardial ablation for advanced AF. Adverse events can be minimized through best practice risk mitigations resulting in an acceptable safety profile (Makati et al., in Heart Rhythm 18(2):303-312, 2021; Eranki et al., in J Cardiothorac Surg 17(1), 2022).
Summary
Treating advanced AF with endocardial ablation alone has been challenging, and outcomes have been suboptimal. The convergent procedure has proven to be more effective but does require the addition of minimally invasive surgery. As more centers implement hybrid AF ablation, attention must turn to improving the procedural approach and optimizing patient selection based on available clinical data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traditional surgical ablation and endocardial catheter ablation have historically been the primary ablation approaches for treating atrial fibrillation (AF) concomitantly with another surgical procedure or as a standalone procedure, respectively. In the last several years, hybrid epicardial-endocardial ablation utilizing a subxiphoid approach for epicardial left atrial ablation combined with endocardial catheter ablation (converge procedure) has been an emerging hybrid approach to standalone AF catheter ablation. The procedure was developed as a treatment option for patients with advanced AF in which traditional catheter ablation had limited efficacy and relief. The technique combines the benefits of both endocardial and epicardial ablation in a minimally invasive manner to provide a comprehensive lesion set characterized by durable transmural lesions. The dual epicardial-endocardial nature of hybrid may be, in part, why the hybrid convergent procedure has been successful in treating even longstanding persistent AF (LSPAF), which was previously thought to be permanent with high recurrence rates that have not improved despite advances in catheter ablation technology [1]. As shown in randomized and propensity score-matched cohorts, effectiveness rates for hybrid convergent ablation are improved compared to endocardial ablation for advanced AF. Adverse events can be minimized through best practice risk mitigations resulting in an acceptable safety profile [2••, 3]. As more centers implement hybrid AF ablation, attention must turn to improving the procedural approach and optimizing patient selection based on available clinical data.
CONVERGE Trial and Real-World Evidence
The CONVERGE trial provided compelling data to support superior effectiveness of the hybrid convergent procedure versus catheter ablation in LSPAF through 12 and 18 months post procedure [4••]. As a randomized clinical trial, the CONVERGE study had set parameters on inclusion, exclusion, and the procedure including no prior ablation, left ventricular ejection fraction (LVEF) ≥ 40%, and only same-day procedures. However, additional published evidence shows that in real-world practice, effectiveness and safety are consistent even with some parameters that differ from the trial. A meta-analysis of CONVERGE hybrid procedures and five published observational studies of contemporary hybrid convergent ablation showed a pooled 12-month freedom from atrial arrhythmia rate of 69% (95% CI: 61–78%), which was 50% (95% CI: 42–58%) off antiarrhythmic drugs (AADs) [5]. Major adverse event rates were 6% (95% CI: 4–8%) within 30 days. Another meta-analysis evaluated only studies comparing hybrid convergent to catheter ablation, reporting freedom from AF of 73% versus 49%, respectively, at last follow-up [3]. The reported pooled complication rate was higher with hybrid convergent ablation; however, 24% (5/21) of the hybrid complications occurred after the endocardial procedure.
Heart Team Approach to Hybrid Ablation
Optimal patient selection and procedural workflows for hybrid convergent ablation are best determined by a dedicated heart team. As the care and treatments for AF have evolved, the need has arisen for a patient-centered, multi-disciplinary heart team approach to AF management, which is recommended by the 2020 European Society for Cardiology (ESC) guidelines [6••]. The individual patient is the central focus of the team, and the composition of the team surrounding the patient should consist not only of the heart team but also any other providers involved in the patient’s care, such as those managing existing comorbidities. Although there is limited evidence on the effectiveness of the heart team approach for AF management, there have been some promising research results that report lower rates of hospitalization and death as well as lower oral anticoagulation use, according to the 2020 ESC Guidelines.
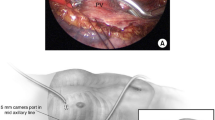
For hybrid procedures specifically, the heart team should consist at minimum of a cardiothoracic surgeon familiar with arrhythmia treatment, possessing the appropriate knowledge and experience with minimally invasive surgery and ablation, as well as an electrophysiologist (EP) with experience in catheter-based AF management. Beyond these staple members of the team, additional support staff such as advanced practice providers or dedicated AF clinic nurse should round out the team [7]. Assembling the heart team with expertise in specifically treating AF patients with hybrid procedures will allow for more seamless coordination and collaboration, with the goal of optimizing success of the program and patient outcomes [2••]. Despite institutional differences and variations, identification of team members and a well-thought-out workflow that includes referral patterns, screening criteria, pre-procedural evaluation, and standard follow-up guidelines along with evaluation of procedural success are cornerstones for a successful hybrid convergent program. While protocols and workflows should be in place at the institutional level, there should also be flexibility to change and adapt these based on decisions at the individual patient level and as the team grows more experienced and knowledgeable to improve the hybrid heart team process. Additionally, pre-operative and post-operative care protocols should be developed to include institution-specific staff training and patient education for pre- and post-operative care as well as mitigation of periprocedural complications [2••]. A proposed hybrid convergent heart team workflow is depicted in Fig. 1 and can be modified to reflect individual center practices.
The hybrid approach requires the cardiac surgeon and EP to learn each other’s terminology to understand both the epicardial and endocardial procedures and how they complement each other. While EPs tend to routinely follow patients long-term for rhythm monitoring and AF recurrences, surgeons may be accustomed to focusing primarily on preoperative and postoperative care visits surrounding the index surgical procedure. However, it was shown in a study of follow-up after surgical ablation that there is a significant increase in the likelihood of being in sinus rhythm at 2 years post-ablation when consistent follow-up protocols were followed [8]. For hybrid convergent procedures, it is imperative that the surgeon and EP both consider long-term clinical outcomes and create a feedback loop to review and discuss all procedural outcomes, including successes and areas for improvement for optimizing their hybrid approach and outcomes.
Same Day Versus Sequential Settings
Deciding on whether to perform both epicardial and endocardial procedures in a single length of stay versus staged/dual length of stay methods is dependent upon several factors. Both the surgeon and the EP should agree upon which method to utilize as this should become part of their hybrid protocol and workflow, allowing deviations from the plan for individual patients when applicable. Establishing a standard for the program is necessary to train all staff and to ensure the appropriate personnel and resources are available. This includes a hybrid electrophysiology suite with operating room capabilities conducive to performing a single-setting approach in the same room, or coordination of both the operating room and electrophysiology lab if performing the two parts of the procedure in separate rooms, whether during the same day or staged on separate days. Institutional logistics and physician preferences will drive this, and patient characteristics, such as the ability to follow up for a staged procedure, will certainly influence the process [2••]. With an improved procedural approach, a center can turn their focus to consistently implementing best practices.
Initial Patient Screening for Hybrid Convergent Procedures
Best Practices
Screening potential patients for hybrid convergent often begins with the general practitioner and/or cardiologist who initially diagnosed the AF and with strong referral patterns, an early referral to an EP that is part of or has knowledge of a hybrid convergent care team. Weighing the benefits and risks of each treatment is paramount to optimizing success in proper patient selection. Patients with AF and structural heart disease are best treated with surgical ablation concomitant with their cardiac surgery for valve repair/replacement or coronary artery bypass graft, as it is not ideal or recommended to perform a hybrid procedure and then later determine the patient needs an open-heart surgery. However, AF patients who have a prolonged duration of persistent AF with obvious symptoms and deteriorated quality of life, as well as those with prior failed catheter ablations, may be relevant to consider for a hybrid approach with additional clinical evidence. Standalone epicardial surgical ablation was not shown to be more effective than endocardial catheter ablation in treating LSPAF in CASA-AF [9]. There are limited data comparing the outcomes of hybrid AF ablation as a de novo procedure compared to hybrid AF ablation after prior ablations. In a retrospective comparison by Kress et al.[10], there were no differences in arrhythmia-free survival between the two groups.
It is important to proactively identify patients with an existing thrombus in the left atrial appendage (LAA) with a comprehensive screening process as they would not be an appropriate candidate for the hybrid convergent procedure. This should be addressed during pre-admission screening as well as just prior to the surgical procedure. The presence of multiple pericardial adhesions due to multiple prior ablations may impede the necessary access to the posterior wall during the surgical ablation portion and limit the ability to adequately perform the hybrid AF convergent procedure; thus, this could potentially increase the risks of the procedure. This emphasizes the need for a thorough patient workup to include not only prior imaging but also a complete patient history of symptoms and prior ablations. Pre-procedural imaging should not be solely relied upon to identify pericardial adhesions, which may not be apparent on imaging. Other contraindications are previous sternotomy or heart surgery, unstable coronary artery disease, stroke or myocardial infarction in prior 3 months, history of Barrett’s esophagitis, active infection or sepsis, and pregnancy.
Beginning a hybrid convergent screening and patient selection process more conservatively while rolling out the program and adjusting the workflows is most prudent. As the heart team gains experience and knowledge, then patient selection can begin to expand beyond the most conservative guidelines [2••]. Patients with advanced comorbidities such as renal failure and ischemic heart disease would not be ideal patients for most heart teams as the risk for adverse events may be exacerbated.
Optimizing Patient Selection
The CONVERGE trial evaluated patients who were undergoing de novo ablation for symptomatic drug-refractory persistent AF or LSPAF. There was no upper limit on the duration of persistent AF; however, patients who had left atrial diameter > 6.0 cm or LVEF < 40% were excluded. Patients in the hybrid arm were treated with hybrid convergent in a single setting, and there was no left atrial appendage closure during the procedure in either arm. Based on the results of the CONVERGE trial that showed significantly improved effectiveness with hybrid convergent compared to catheter ablation in the LSPAF population[11], the EPi-sense device received US FDA approval for the treatment of drug-refractory, symptomatic LSPAF (continuous atrial fibrillation greater than 12 months duration) when augmented in a hybrid procedure with an endocardial catheter. Outside of the CONVERGE trial, there is emerging evidence for the potential utility of the hybrid convergent procedure in patients with advanced AF as defined by other parameters. Additionally, based on clinical gaps for specific patient populations, there may be other groups to consider for future research on hybrid convergent procedures. Table 1 provides the patient characteristics and outcome measures for contemporary research in addition to the CONVERGE trial results.
Defining Advanced Atrial Fibrillation
CONVERGE and other studies have shown a marked improvement in rhythm outcomes after hybrid convergent in patients with LSPAF [4••, 12, 13]. Most contemporary catheter ablation trials have not included significant numbers of LSPAF patients in their inclusion criteria, whereas CONVERGE sought to elucidate the most effective treatment options for persistent and LSPAF patients. Per guidelines, persistent AF is defined as continuous AF for more than 7 days, which becomes LSPAF if continuous for greater than 12 months’ duration. The arbitrary cutoff of 12 months has never been assessed to determine its suitability and significance for defining LSPAF [6••]. First, this definition can be challenging because in some cases, the details specifying time since diagnosis are practically difficult to acquire as a referred patient may not recall historical details of their diagnostic timeline and if they have experienced continuous or recurrent AF. Reliance on the assumption that a complete clinical history can be obtained in addition to available rhythm data to determine the AF pattern as paroxysmal vs non-paroxysmal is outdated. Further testing and imaging could reveal progressive disease that is not adequately described by duration of AF. Physician classification of AF pattern can differ between practitioners [14] according to a study by Charitos et al. [15] The study found a poor correlation between classification of AF pattern derived by clinicians compared to the pattern recorded on devices. As such, it may be relevant to explore other ways of defining advanced AF, including extent of anatomical substrate or structural remodeling, that may better characterize a disease state that warrants ablation beyond pulmonary vein isolation (PVI). For example, a novel approach to wholly characterizing, rather than discretely classifying AF, has been proposed. The 4S-AF scheme considers the following factors: stroke risk, symptoms, severity of burden, and substrate rather than the 3-P classification (paroxysmal, persistent/LSPAF, permanent) based on AF episode duration and temporal patterns [6••, 16]. This type of approach could allow heart care teams to consider the patient’s current condition, symptoms, history, and other underlying comorbidities (i.e., obesity, sleep apnea, hypertension) that contribute to AF progression and substrate remodeling and thus compound the detrimental effects of AF. The following sections describe the current available evidence for hybrid convergent being used in patients characterized not only by their chronicity of AF but by other markers of advanced AF.
High AF Burden
The standard definition of recurrence based upon a 30-s episode of AF is controversial, and AF burden reduction has been proposed as an alternative endpoint for non-paroxysmal AF studies [17]. AF burden assessment requires a degree of continuous monitoring rather than standard 12-lead ECG. The CONVERGE trial and other real-world evidence studies have reported on AF burden following hybrid convergent ablation based upon rhythm monitoring for 24 h or more, including Holter monitor, 7-day e-patches, implantable loop recorders, and existing implanted devices [4••, 13, 18, 19]. Long-term results from 18 months to more than 5 years of follow-up show substantial reductions in AF burden or low residual AF burden after hybrid convergent ablation [4, 18]. In CONVERGE, AF burden reduction (defined as ≥ 90% reduction in AF burden from baseline) at 12 months was 80% versus 56.8% in the hybrid convergent and catheter ablation groups, respectively (p = 0.007). This significant difference was sustained at 18 months with 74% versus 55% AF burden reduction in the hybrid convergent and catheter ablation groups, respectively (p = 0.0395), based on 7-day Holter monitoring. Our center’s analysis of patients with continuous monitoring found that even patients who experienced atrial arrhythmia recurrence after hybrid convergent still had a low mean AF burden of < 5%, with only 3% of patients having relatively high AF burden following the procedure [19].
Low Ejection Fraction and Heart Failure
Heart failure and AF can occur concurrently in the same patients given shared risk factors and comorbidities, such that approximately 40% of patients with one of the conditions will develop coexisting AF and heart failure [20]. The shared presence of AF and heart failure compounds the risk of adverse outcomes, including mortality. Chronic AF can induce cardiomyopathy resulting in heart failure with reduced left ventricular ejection fraction (LVEF) [21]. In patients with heart failure coexisting with AF, catheter ablation provided improved survival outcomes compared to first-line medical therapy intended for rate or rhythm control through 5 years post-procedure. Catheter ablation results were superior to medical therapy (28.5% versus 44.6% death or heart failure hospitalization) yet left room for continued improvement in efficacy to achieve sinus rhythm and AF burden reduction [22]. In patients who received catheter ablation, sinus rhythm was observed in approximately 55–65% of patients. AF burden per patient (in percent of time) was 20–30% through 5 years of follow-up. Eighteen percent of the catheter ablation patients experienced burden for ≥ 10% during the study compared to the 45% documented in the medical therapy group [22].
While CONVERGE excluded patients with LVEF < 40%, real-world use of hybrid convergent ablation in patients with severely reduced LVEF has been reported. In a study of 67 persistent AF (80% LSPAF) patients who were treated with hybrid convergent ablation at a single center, almost 20% had co-existing low LVEF (defined as 40% or less) and 12% had dilated cardiomyopathy [23]. Those with a history of prolonged AF duration were at higher risk of recurrence at 12 months and those with a history of greater than 5 years of AF duration had the shortest time to recurrence. Despite this, the cohort had overall success rates of 81.3% and 61.5% freedom from AF recurrence at 1 year and over a mean 2.8 years of follow-up, respectively, highlighting a need to close the treatment gap that exists for patients who have long suffered debilitating symptoms and impaired quality of life because of AF. In their single-center experience with hybrid convergent procedure, Gulkarov et al. reported that 16% of their 31-patient series had hypertrophic cardiomyopathy [24, 25]. In a study by our center and two other institutions, we reported that AF patients with moderately to mildly reduced LVEF (40–55%) and moderately to severely reduced LVEF (< 40%) experienced significantly improved LVEF after hybrid convergent procedures, with 7–9 months of mean follow-up [26]. Similarly, a single center reported significant improvements in LVEF in patients with baseline LVEF < 55% after hybrid convergent. Improvements in LVEF in patients with tachycardia-mediated cardiomyopathy were recently reported after thoracoscopic hybrid ablation with left atrial appendage exclusion in a retrospective review [18]. Although not a convergent approach, over 60% of the patients achieved rhythm success (< 30 s of AF/AFL/AT off class I/III AADs) at 1, 2, and 3 years, with a mean of 3.5 ± 1.9 years follow-up after thoracoscopic hybrid ablation. Significant improvement in LVEF (mean 12%), significant decrease in mean LA size, and improvement of heart failure classification were also reported [27]. The results of hybrid approaches in patients with reduced LVEF and/or heart failure suggest additional research in this area is warranted.
Enlarged Left Atrium
Left atrial (LA) size as measured by LA diameter or volume is another anatomical consideration to characterize advanced AF and potentially guide treatment decisions. Atrial fibrillation that results in the occurrence of increased LA size may be a marker of progression to advanced AF, regardless of time since first diagnosis [28, 29]. Conversely, an enlarged left atrium can increase the risk of AF itself [29]. Regardless of the temporality, this progression in severity to advanced AF can raise the risk of additional morbidity and mortality for the patient [30]. The presence of left atrial enlargement in the context of AF has been associated with increased recurrence rates after endocardial catheter ablation, suggesting that patients with AF and enlarged left atrium need a better intervention that treats the AF more effectively and durably [28, 31]. Furthermore, the occurrence of LA enlargement may be undercounted as measures of LA diameter are thought to be less reliable than volumetric measurements due to the inherent asymmetry of the LA. The CONVERGE trial allowed patients with LA diameter up to 6 cm [4••]. Therefore, it is currently unknown how the hybrid convergent procedure will perform in patients with severe LA enlargement. Cox-Maze surgical ablation has been shown to be effective up to 8 cm after which efficacy drops below 50% [32].
Hybrid convergent teams should consider utilizing transthoracic echocardiography (TTE) versus transesophageal echocardiography (TEE) to obtain these 3-dimensional volume assessments rather than single internal linear measures [33, 34].
The Role of the Left Atrial Appendage
The LAA is the site where the majority of thrombi form in the context of non-valvular and valvular AF [35]. Percutaneous endocardial and surgical LAA closure have been shown to reduce stroke risk in AF patients [36-38]. Additionally, the LAA is a potential site of AF triggers particularly in non-paroxysmal AF [39]. Beginning in 2017, some physicians began adding epicardial LAA exclusion to the hybrid convergent procedure [40]. To date, exclusion techniques and initial single-center outcomes of hybrid convergent with LAA exclusion have been reported [41-43]. As part of the preoperative workup, a TEE should be performed by an experienced clinician to rule out a preoperative thrombus in the LAA. Use of a simultaneous TEE during LAA exclusion ensures that the LAA was excluded properly with minimal residual stump remaining and no residual blood flow between the LAA and left atrium, to prevent a location for any future thrombi to occur [40].
Conclusion
There is new real-world evidence and literature supporting clinical success of hybrid convergent with results aligned with CONVERGE trial. Because these studies were performed in routine practice, their results also suggest that additional patient characteristics may be relevant to consider when determining benefit risk of hybrid convergent, depending on the patients’ clinical condition. Further development of heart team approach is critical to further evaluate the role for hybrid convergent in patient groups that may not have been previously considered and/or have been overlooked in AF management.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Winkle RA, Mead RH, Engel G, Salcedo J, Brodt C, Barberini P, et al. Very long term outcomes of atrial fibrillation ablation. Heart Rhythm. 2023. https://doi.org/10.1016/j.hrthm.2023.02.002.
Makati KJ, Sood N, Lee LS, Yang F, Shults CC, DeLurgio DB, et al. Combined epicardial and endocardial ablation for atrial fibrillation: best practices and guide to hybrid convergent procedures. Heart Rhythm. 2021;18(2):303–12. https://doi.org/10.1016/j.hrthm.2020.10.004. Hybrid ablation procedures of atrial fibrillation – how to optimize patient selection and improve the procedural approach.
Eranki A, Wilson-Smith AR, Williams ML, et al. Hybrid convergent ablation versus endocardial catheter ablation for atrial fibrillation: a systematic review and meta-analysis of randomised control trials and propensity matched studies. J Cardiothorac Surg. 2022;17(181). https://doi.org/10.1186/s13019-022-01930-7.
DeLurgio DB, Crossen KJ, Gill J, Blauth C, Oza SR, Magnano AR, et al. Hybrid convergent procedure for the treatment of persistent and long-standing persistent atrial fibrillation: results of CONVERGE Clinical Trial. Circ Arrhythm Electrophysiol. 2020;13(12):e009288. https://doi.org/10.1161/CIRCEP.120.009288. Hybrid ablation procedures of atrial fibrillation – how to optimize patient selection and improve the procedural approach.
Shrestha S, Plasseraud KM, Makati K, Sood N, Killu AM, Contractor T, et al. Hybrid convergent ablation for atrial fibrillation: A systematic review and meta-analysis. Heart Rhythm O2. 2022;3(4):396–404. https://doi.org/10.1016/j.hroo.2022.05.006.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612. Hybrid ablation procedures of atrial fibrillation – how to optimize patient selection and improve the procedural approach.
Van Loo I, Asmundis CD, Meir ML. The 7 pillars of a successful hybrid atrial fibrillation program. Innov: Technol Tech Cardiothorac Vasc Surg. 2019;14(6):493–7. https://doi.org/10.1177/1556984519877264.
Ad N, Henry L, Hunt S, Stone L. The implementation of a comprehensive clinical protocol improves long-term success after surgical treatment of atrial fibrillation. J Thorac Cardiovasc Surg. 2010;139(5):1146–52. https://doi.org/10.1016/j.jtcvs.2010.01.034.
Haldar S, Khan HR, Boyalla V, Kralj-Hans I, Jones S, Lord J, et al. Catheter ablation vs. thoracoscopic surgical ablation in long-standing persistent atrial fibrillation: CASA-AF randomized controlled trial. Eur Heart J. 2020;41(47):4471–80. https://doi.org/10.1093/eurheartj/ehaa658.
Kress DC. Characterizing recurrence following hybrid ablation in patients with persistent atrial fibrillation. J Patient-Centered Res Rev. 2020;7(3):227–38.
Delurgio DB, Blauth C, Halkos ME, Crossen KJ, Talton D, Oza SR, et al. Hybrid epicardial-endocardial ablation for long-standing persistent atrial fibrillation: a subanalysis of the CONVERGE trial. Heart Rhythm. 2022. https://doi.org/10.1016/j.hroo.2022.11.007.
Maclean E, Yap J, Saberwal B, Kolvekar S, Lim W, Wijesuriya N, et al. The convergent procedure versus catheter ablation alone in longstanding persistent atrial fibrillation: a single centre, propensity-matched cohort study. Int J Cardiol. 2020;303:49–53. https://doi.org/10.1016/j.ijcard.2019.10.053.
Makati KJ, Sherman AJ, Gerogiannis I, Sood N. Safety and efficacy of convergent hybrid procedure using cryo as endocardial energy source for the treatment of atrial fibrillation. Circ Arrhythm Electrophysiol. 2020;13(11):e008556. https://doi.org/10.1161/CIRCEP.120.008556.
Mittal S. Differentiating paroxysmal from persistent atrial fibrillation. J Am Coll Cardiol. 2014;63(25):2849–51. https://doi.org/10.1016/j.jacc.2014.04.020.
Charitos EI, Pürerfellner H, Glotzer TV, Ziegler PD. Clinical classifications of atrial fibrillation poorly reflect its temporal persistence: insights from 1,195 patients continuously monitored with implantable devices. J Am Coll Cardiol. 2014;63(25, Part A):2840–8. https://doi.org/10.1016/j.jacc.2014.04.019.
Potpara TS, Lip GYH, Blomstrom-Lundqvist C, Boriani G, Van Gelder IC, Heidbuchel H, et al. The 4S-AF scheme (stroke risk; symptoms; severity of burden; substrate): a novel approach to in-depth characterization (rather than classification) of atrial fibrillation. Thromb Haemost. 2021;121(03):270–8. https://doi.org/10.1055/s-0040-1716408.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. Europace. 2018;20(1):157–208. https://doi.org/10.1093/europace/eux275.
Kerendi F, Tschopp D, Maningat A, Hyde B, Coffeen P, Punske BB. Abstract 13439: long-term outcomes from continuous rhythm monitoring after hybrid convergent procedure in longstanding persistent atrial fibrillation patients. Circulation. 2021;144(Suppl_1):A13439-A. https://doi.org/10.1161/circ.144.suppl_1.13439.
Larson J, Merchant FM, Patel A, Ndubisi NM, Patel AM, DeLurgio DB, et al. Outcomes of convergent atrial fibrillation ablation with continuous rhythm monitoring. J Cardiovasc Electrophysiol. 2020;31(6):1270–6. https://doi.org/10.1111/jce.14454.
Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality. Circulation. 2003;107(23):2920–5. https://doi.org/10.1161/01.cir.0000072767.89944.6e.
Gopinathannair R, Chen LY, Chung MK, Cornwell WK, Furie KL, Lakkireddy DR, Marrouche NF, Natale A, Olshansky B, Joglar JA; on behalf of the American Heart Association Electrocardiography and Arrhythmias Committee and Heart Failure and Transplantation Committee of the Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Hypertension; Council on Lifestyle and Cardiometabolic Health; and the Stroke Council. Managing atrial fibrillation in patients with heart failure and reduced ejection fraction: a scientific statement from the American Heart Association. Circ Arrhythm Electrophysiol. 2021;14:e000078.https://doi.org/10.1161/HAE.0000000000000078.
Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018;378(5):417–27. https://doi.org/10.1056/nejmoa1707855.
Mannakkara NN, Porter B, Child N, Sidhu BS, Mehta VS, Elliott MK, et al. Convergent ablation for persistent atrial fibrillation: outcomes from a single-center real-world experience. Eur J Cardiothorac Surg. 2022. https://doi.org/10.1093/ejcts/ezac515.
Gulkarov I, Wong B, Kowalski M, Worku B, Afzal A, Ivanov A, et al. Convergent ablation for persistent atrial fibrillation: single center experience. J Card Surg. 2019;34(10):1037–43. https://doi.org/10.1111/jocs.14204.
Derejko P, Polańska M, Chojnowska L, Michałowska I, Wójcik A, Piotrowicz E, et al. Catheter ablation of atrial fibrillation in patients with hypertrophic cardiomyopathy: atrial fibrillation type determines the success rate. Kardiol Pol. 2013;71(1):17–24.
Oza S, Crossen K, Magnano AR, Merchant FM, Joseph L, De Lurgio DB. Emerging evidence of improvement in left ventricular ejection fraction after convergent ablation in persistent and long-standing persistent AF patients with reduced ejection fraction. D-PO03-015 to DPO03-237. Heart Rhythm. 2020;17(5):S291-S382. https://cslide-us.ctimeetingtech.com/hrs20/attendee/eposter/poster/1155?q=Oza.
Kiankhooy A, Pierce C, Burk S, Phillips A, Eisenberg S, Dunnington G. Hybrid ablation of persistent and long-standing persistent atrial fibrillation with depressed ejection fraction: a single center observational study. JTCVS Open. 2022. https://doi.org/10.1016/j.xjon.2022.08.014.
Zhuang J, Wang Y, Tang K, Li X, Peng W, Liang C, et al. Association between left atrial size and atrial fibrillation recurrence after single circumferential pulmonary vein isolation: a systematic review and meta-analysis of observational studies. Europace. 2012;14(5):638–45. https://doi.org/10.1093/europace/eur364.
Vaziri SM, Larson MG, Benjamin EJ, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation. 1994;89(2):724–30. https://doi.org/10.1161/01.cir.89.2.724.
Patel DA, Lavie CJ, Milani RV, Shah S, Gilliland Y. Clinical implications of left atrial enlargement: a review. Ochsner J. 2009;9(4):191–6.
Njoku A, Kannabhiran M, Arora R, Reddy P, Gopinathannair R, Lakkireddy D, et al. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: a meta-analysis. Europace. 2018;20(1):33–42. https://doi.org/10.1093/europace/eux013.
Damiano RJ Jr, Schwartz FH, Bailey MS, Maniar HS, Munfakh NA, Moon MR, et al. The Cox maze IV procedure: predictors of late recurrence. J Thorac Cardiovasc Surg. 2011;141(1):113–21. https://doi.org/10.1016/j.jtcvs.2010.08.067.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003.
Wang Y, Gutman JM, Heilbron D, Wahr D, Schiller NB. Atrial volume in a normal adult population by two-dimensional echocardiography. Chest. 1984;86(4):595–601. https://doi.org/10.1378/chest.86.4.595.
Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755–9. https://doi.org/10.1016/0003-4975(95)00887-x.
Whitlock RP, Belley-Cote EP, Paparella D, Healey JS, Brady K, Sharma M, et al. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med. 2021;384(22):2081–91. https://doi.org/10.1056/nejmoa2101897.
Lakkireddy D, Thaler D, Ellis CR, Swarup V, Sondergaard L, Carroll J, et al. Amplatzer amulet left atrial appendage occluder versus watchman device for stroke prophylaxis (amulet IDE): a randomized, controlled trial. Circulation. 2021;144(19):1543–52. https://doi.org/10.1161/circulationaha.121.057063.
Reddy VY, Doshi SK, Kar S, Gibson DN, Price MJ, Huber K, et al. 5-year outcomes after left atrial appendage closure: from the PREVAIL and PROTECT AF Trials. J Am Coll Cardiol. 2017;70(24):2964–75. https://doi.org/10.1016/j.jacc.2017.10.021.
Di Biase L, Burkhardt JD, Mohanty P, Sanchez J, Mohanty S, Horton R, et al. Left atrial appendage. Circulation. 2010;122(2):109–18. https://doi.org/10.1161/circulationaha.109.928903.
Wats K, Kiser A, Makati K, Sood N, DeLurgio D, Greenberg Y, et al. The convergent atrial fibrillation ablation procedure: evolution of a multidisciplinary approach to atrial fibrillation management. Arrhythm Electrophysiol Rev. 2020;9(2):88–96. https://doi.org/10.15420/aer.2019.20.
Lee LS. Subxiphoid minimally invasive epicardial ablation (convergent procedure) with left thoracoscopic closure of the left atrial appendage. Oper Tech Thorac Cardiovasc Surg. 2019;23(4):152–65. https://doi.org/10.1053/j.optechstcvs.2019.04.002.
Gegechkori N. The effect of left atrial appendage closure on patients undergoing hybrid / convergent atrial fibrillation ablation. J Atr Fibrillation Electrophysiol. 2022;15(4):66–71.
Tonks R, Lantz G, Mahlow J, Hirsh J, Lee LS. Short and intermediate term outcomes of the convergent procedure: initial experience in a tertiary referral center. Ann Thorac Cardiovasc Surg. 2020;26(1):13–21. https://doi.org/10.5761/atcs.oa.19-00164.
Acknowledgements
Kristen Plasseraud, PhD (AtriCure, Inc.) provided medical writing and editing assistance under the direction of Dr. De Lurgio.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. De Lurgio is a consultant and speaker for AtriCure and Boston Scientific, as well as a consultant to Medtronic.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De Lurgio, D.B., Meador, M.R. Hybrid Ablation Procedures of Atrial Fibrillation—How to Optimize Patient Selection and Improve the Procedural Approach. Curr Cardiovasc Risk Rep 17, 133–141 (2023). https://doi.org/10.1007/s12170-023-00722-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12170-023-00722-5