Abstract
Who should undergo hybrid AF ablation?
Patients with symptomatic persistent or long-standing persistent atrial fibrillation refractory to pharmacological or routine catheter ablation can be considered for hybrid epicardial-endocardial AF ablation. Although it seems clear that patient selection should be important when considering hybrid AF ablation for optimal results, unfortunately, available data on the outcomes of hybrid epicardial-endocardial ablation is limited. Hybrid ablation is rarely compared to stand-alone catheter ablation, the surgical approach (access site, lesion set, ablation tool) is inconsistent, and the patient population studied is often suitable for a catheter ablation approach (paroxysmal AF, minimal structural heart disease). We believe that the hybrid approach should be considered in patients who either have had unsuccessful catheter ablations or have significant structural heart disease evident by enlarged left atrial size or atrial fibrosis. These are the patients who warrant the added risk of a hybrid approach and who stand to benefit from a more extensive ablation including isolation of the posterior wall of the left atrium. Multi-center studies with a uniform hybrid ablation approach and comparison with a stand-alone catheter ablation approach are needed to help clarify the role of hybrid AF ablation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interventional approaches to rhythm control are widely used for treatment of symptomatic atrial fibrillation in patients who do not respond well to pharmacotherapy. The Cox-Maze III procedure, a stand-alone surgical approach to AF ablation, has long been considered the gold standard surgical treatment for AF but is complex and requires patients to be placed on cardiopulmonary bypass [1]. In order to limit bypass time, the modified Cox-Maze IV procedure uses a combination of radiofrequency and cryoablation to achieve a similar lesion set [2, 3]. However, current surgical ablation approaches remain morbid procedures and generally do not utilize precise mapping of ablation circuits to determine the adequacy of lesion sets and target organized dysrhythmias.
Since the seminal report of Haissaguerre et al., the most common current approach for AF ablation is endocardial catheter-based pulmonary vein isolation [4]. This approach works well in paroxysmal AF but success rates are lower in those with persistent and long-standing persistent AF. The best approach to catheter ablation in patients with persistent AF remains unclear. Catheter-based approaches have included linear ablation lesions in an attempt to “debulk” the left atrium, posterior wall isolation and/or isolation of other low voltage regions distant from the posterior wall, ganglionated plexi ablation, or targeted ablation at sites of potential driver activity. However, comparative studies of these approaches have demonstrated no clear long-term benefit over antral pulmonary vein isolation.
Significant technical advances in catheter ablation technology have accompanied the investigation of lesion patterns. These include high-density automated mapping of tachycardia substrates, and force sensing and other technologies to improve lesion formation. Nevertheless, catheter ablation remains limited by inadequacy of linear lesion formation, particularly on the posterior left atrial wall where collateral damage to the esophagus is a concern. In general, it remains unclear whether failed endocardial ablation for AF results from an inappropriate lesion set or inadequate lesion delivery.
In addition, although endocardial catheter ablation has reasonable short-term benefit, success rates do not plateau with recurrences mounting over time. In a meta-analysis of long-term (> 3 years) outcomes of catheter ablation, single procedure, drug free, freedom from atrial arrhythmia at long-term follow-up was found to be 54.1% in paroxysmal AF and 41.8% in persistent or long-standing persistent AF [5]. With multiple procedures, the long-term success rate can be up to 80%. However, in patients with significant cardiac structural abnormalities such as significant left atrial enlargement or hypertrophic cardiomyopathy, rates of AF recurrence are even higher [6].
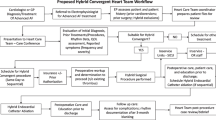
With these limitations of surgical- and catheter-based ablations, the hybrid ablation approach offers a minimally invasive option for interventional rhythm control of atrial fibrillation taking advantage of both approaches. In a hybrid ablation, the surgical component is performed through bilateral thoracoscopic or transabdominal or subxiphoid pericardioscopic approaches. The minimally invasive nature of these surgical incisions allows for faster recovery yet still provides direct visualization of the myocardium for the surgeon to perform epicardial ablation. In comparison with catheter ablation, the risk of damaging surrounding structures, such as the phrenic nerve and the esophagus, is lowered substantially. Depending on the surgical approach, left atrial appendage exclusion can be achieved during these procedures. The subsequent endocardial part of the hybrid procedure provides the opportunity to access areas that are difficult to reach epicardially, such as the mitral isthmus and the cavotricuspid isthmus. It also allows for utilization of sophisticated mapping techniques to specifically target any gaps in the epicardial ablation and map any residual organized atrial tachyarrhythmias (Fig. 1).
Left atrial voltage map (posterior-anterior view) after a hybrid epicardial-endocardial ablation. Gray area indicates portions of the left atrium (pulmonary veins and posterior left atrial wall) which have been electrically isolated. Note the red lesions at sites of endocardial ablation necessary to close gaps in the epicardial lesion set.
Importantly, a hybrid ablation program comes with particular challenges, including the requirement for a multidisciplinary management approach, consideration of the sequence of the procedure, requirement of a hybrid laboratory for non-staged procedures, and particular attention to the anticoagulation strategy. In addition, the surgical component of the hybrid approach does carry a higher complication risk due to the invasive nature of the procedure. There is added risk of thoracic injury, including hemothorax, laceration of the pulmonary veins, left atrial perforation, pericarditis, and significant bleeding. However, with experience and a dedicated team, a hybrid AF ablation program can provide significant benefits with limited risk to a challenging AF patient population.
Treatment
Interventional procedures
Several different ablation tools and surgical approaches with corresponding lesion sets have been utilized for hybrid AF ablation. Multiple studies have been performed using bipolar radiofrequency pulmonary vein clamps and a linear ablation pen utilizing a bilateral anterior thoracoscopic approach for the epicardial portion of the procedure. There is more limited experience with a unilateral right thoracoscopic or mini-thoracotomy approach with a combined unipolar and bipolar vacuum-assisted RF linear ablation catheter that encircles the pulmonary veins. In order to avoid chest incisions, a unipolar or bipolar vacuum-assisted RF linear ablation catheter can also be maneuvered in the epicardial space through a transabdominal, transdiaphragmatic approach or a subxiphoid approach by way of a pericardioscopic access cannula. In addition, with any of these surgical approaches, a decision needs to be made whether the ablation procedure will be performed in stages with the endocardial component performed several weeks or months after the epicardial component. Or the procedure can be performed with the endocardial component immediately following the epicardial component in a hybrid ablation laboratory.
Bilateral thoracoscopic hybrid ablation approach
The bilateral thoracoscopic approach starts with deflation of the right lung, followed by insertion of a trocar into the sixth intercostal space. Another port is placed in the third intercostal space. Blunt dissection is done using the thoracoscope for guidance to expose the right-sided pulmonary veins. The bipolar clamp is used to isolate the pulmonary veins. The same technique is applied on the left side to isolate the left-sided pulmonary veins. A linear pen is used to complete roof and inferior left atrial (LA) ablation to create a posterior “box” lesion. Additional ganglionated plexi ablation can be performed. The left atrial appendage can be excluded. Endocardial ablation is used to confirm and complete the epicardial lesion set. Additional linear ablation (mitral isthmus, cavotricuspid isthmus) or focal ablation can be performed. Several studies have used this surgical ablation approach with either a staged or sequential strategy (Table 1).
Sequential hybrid ablation using a bilateral thoracoscopic approach was studied in 15 patients with persistent or long-standing persistent AF, despite prior catheter ablation, by Mahapatra et al. [7]. This procedure was compared to catheter ablation alone. Bilateral thoracoscopic off-pump epicardial ablation was performed, along with autonomic ganglionated plexi (GP) ablation using the Dallas lesion set. The endocardial procedure was performed a few days later. Cavotricuspid isthmus linear ablation, coronary sinus, and superior vena cava (SVC) isolation were performed and pulmonary vein (PV) isolation was confirmed. After a mean follow-up of 20.7 months, 86.7% of the patients who underwent the hybrid approach compared with 53% of the patients who had catheter-based ablation were free of AF off anti-arrhythmic drugs.
Bulava et al. described their experience with a staged hybrid approach in 50 patients with long-standing persistent, symptomatic, and anti-arrhythmic refractory AF [8]. Epicardial ablation was done first with a bipolar RF ablation clamp and linear ablation including pulmonary vein isolation (PVI), posterior box isolation, GP ablation, and left atrial appendage (LAA) exclusion. The EP procedure was performed 6–8 weeks later. All four pulmonary veins were isolated in 74% of the patients. If the patient was in sinus rhythm, RF ablation of the cavotricuspid isthmus was performed. In patients who were not in sinus rhythm, pulmonary vein isolation was confirmed first, prior to proceeding to additional LA and cavotricuspid isthmus ablation. After a 12-month follow-up period, using 7-day Holter monitors, 94% of the patients were in normal sinus rhythm with antiarrhythmic drugs (AADs) and 84% without AADs.
Krul et al. performed hybrid ablation via a bilateral thoracoscopic approach in 31 AF patients (16 paroxysmal, 13 persistent, and 2 long-standing persistent) [9]. The epicardial ablation included isolation of the pulmonary veins and ligament of Marshall ablation in all patients. In patients with persistent and long-standing persistent AF, additional linear posterior LA ablation was performed. The left atrial appendage was removed in 94% of patients. The endocardial portion included confirmation of isolation of the pulmonary veins and posterior LA. During the median follow-up of 375 days, 86% of the patients were free from atrial arrhythmias without requiring anti-arrhythmics.
Pison et al. used the thoracoscopic hybrid approach in 26 patients who had either failed prior catheter ablation, had an enlarged LA, or had persistent (n = 10) or long-standing persistent AF (n = 1) [10]. The epicardial ablation comprised PV isolation, along with roof and inferior lines for a complete posterior box lesion. Entrance and exit block was confirmed. The LAA was excluded in a subset. Upon completion of the surgical procedure, the endocardial portion of the procedure focused on confirmation of PV isolation and ablation of any conduction gaps left identified from the epicardial ablation. At a median follow-up period of 24 months, 74% of the patients with long-standing persistent and 62% of the patients with persistent AF were free of AF.
La Meir et al. compared the hybrid approach to a minimally invasive epicardial-only ablation in patients with paroxysmal (16), persistent (8), and long-standing persistent (LSP) (8) AF [11]. In this study, 35 patients underwent both epicardial and endocardial ablation and 28 patients had epicardial-only ablation using the bilateral thoracoscopic approach. The epicardial ablation included PVI, posterior box, and GP ablation. Endocardial ablation focused on confirmation and completion of the PV and posterior LA isolation. In patients with persistent AF, a mitral line was created as well. LAA exclusion was done in patients with CHADS2 score > 1 or in the setting of LAA tachycardia. Patients were followed with 7-day Holter monitors. At 1-year follow-up, 91% of the patients from the hybrid group were free of AF compared to 82% in the surgical group.
In a study of Pison et al., 78 patients underwent hybrid ablation using the bilateral thoracoscopic technique [12]. Of these, 37.2% had paroxysmal, 43.6% had persistent, and 19.2% had long-standing persistent AF. The lesion set for epicardial ablation included pulmonary vein and posterior box isolation. Endocardial mapping and ablation were used to confirm and complete these lesions. LAA exclusion was done in patients with LAA tachycardia or CHADS2 score ≥ 1. The patients were followed using Holter monitoring. At a median follow-up of 2 years, 87% of the patients were in sinus rhythm, although 13% of the patients required repeat ablation. The single ablation success rate without AADs was 74%. Success rate was 100% in LSP, 62% in persistent, and 76% in paroxysmal AF.
Kurfirst et al. used a staged hybrid strategy in 30 patients with persistent (17%) and long-standing persistent (83%) AF [13]. For the epicardial ablation, a bilateral thoracoscopic approach was utilized and included isolation of pulmonary veins, posterior wall box lesion, and GP ablation. LAA was also excluded. The endocardial ablation was done 3 months after the surgical procedure and focused on completion of PVI and posterior box isolation. Anterior mitral isthmus and cavotricuspid isthmus lines were also completed routinely. At a mean follow-up of 208 days, 90% of the patients were in sinus rhythm without AADs and 93% with AADs.
Unilateral thoracoscopic hybrid ablation approach
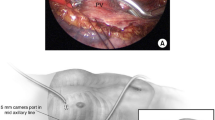
In the unilateral thoracoscopic approach, the right lung is deflated and three ports, one for the camera and two for the instruments, are placed in the third, fourth, and fifth intercostal spaces. Blunt dissection between the SVC and the right superior pulmonary vein is done, followed by blunt dissection between the IVC and the right inferior pulmonary vein. A vacuum-assisted radiofrequency linear ablation catheter is used to deliver a continuous lesion encircling the origin of all the pulmonary veins. When compared to the bilateral thoracoscopic approach, the unilateral approach helps limit post-operative gas exchange problems. Three studies have been reported using a unilateral thoracoscopic surgical approach.
La Meir et al. performed hybrid AF ablation using this technique in 19 patients with lone AF [14]. This included patients with paroxysmal (n = 5), persistent (n = 4), and long-standing persistent AF (n = 10). A right thoracoscopic approach was employed to isolate the pulmonary veins. GP ablation was performed as well. Endocardial ablation included confirmation of PV isolation with entrance and exit block. At 1-year follow-up, only 36.8% of the patients remained in sinus rhythm without anti-arrhythmics. The 1-year success rates were worst in patients with long-standing persistent AF at 20% and followed by persistent AF at 50%, and paroxysmal AF had the best results at 60%.
Munretto et al. performed staged hybrid ablations in 36 patients with either long-standing persistent (n = 28) or persistent AF (n = 8) [15]. A unilateral thoracoscopic approach was used for combined PV and posterior LA isolation with entrance and exit block confirmed epicardially. The endocardial procedure was done within 30 to 45 days of the surgical ablation to close gaps within the surgical lesion set. At a follow-up period of 30 months, 91.6% of the patients remained in sinus rhythm.
Bisleri et al. used a staged approach in 45 patients with long-standing persistent AF [16]. The patients initially underwent the thoracoscopic right-sided approach for pulmonary vein and posterior LA isolation. After the surgical ablation, all patients were brought back within 30–45 days for endocardial evaluation. If they were found to have conduction gaps, catheter ablation was performed. After surgical ablation, 66.7% of the patients were in sinus rhythm while the remainder required electrical cardioversion to achieve sinus rhythm. At the time of electrophysiological evaluation, four patients required additional endocardial ablation. An implantable loop recorder was placed in all patients after completion of the surgical ablation. The patients were followed for about 28 months and 40 out of 45 patients (88.9%) remained in sinus rhythm.
Transabdominal/transdiaphragmatic pericardioscopic hybrid ablation approach
The pericardioscopic, transdiaphragmatic approach consists of a 2-cm epigastric incision and insertion of two laparoscopic ports. Through these ports, the central fibrous part of the diaphragm and the pericardium is accessed. A cannula is then inserted into the pericardial space and provides endoscopic visualization and access to the left atrium. A unipolar vacuum-assisted RF linear ablation catheter is used to perform antral PV ablation and posterior LA box ablation, although the extent of the epicardial lesion set is limited by the pericardial reflections. Endocardial ablation is used to confirm and complete the epicardial lesion set. Additional linear ablation (mitral isthmus, cavotricuspid isthmus) or focal ablation can be performed. Several studies have used this surgical ablation approach all with a sequential strategy.
One-year outcomes of the transdiaphragmatic pericardioscopic approach in 101 patients with paroxysmal (n = 17), persistent (n = 47), or long-standing persistent (n = 37) AF were reported by Gehi et al. [17•]. The epicardial ablation included ablation on the antrum of all four pulmonary veins, posterior left atrial wall, lateral right atrium, and the ligament of Marshall. The endocardial ablation was performed immediately after and included confirmation of antral pulmonary vein isolation, posterior LA isolation, coronary sinus, mitral isthmus, and a cavotricuspid linear ablation. At 12-month follow-up, 66% of the patients who had undergone a single ablation remained free of arrhythmia recurrence and 71% after repeat ablation.
Gersak et al. used a similar surgical approach in 50 patients with persistent or long-standing AF [18]. The epicardial ablation lesion set included antral pulmonary vein ablation along with the posterior wall. Once the epicardial ablation had been completed, endocardial ablation followed and included endocardial ablation of the pulmonary veins and posterior LA as necessary. The patients had a loop recorder implanted for arrhythmia surveillance. At a follow-up interval of 12 months, 88% of the patients were free of arrhythmia recurrence.
Outcomes of a similar approach at four European centers was presented in a study by Gersak et al. [19•]. The 73 AF patients [persistent (30.1%), long-standing persistent (69.9%)] had surgical ablation via transdiaphragmatic access. The epicardial lesion set included ablation of the PV and the posterior LA. The endocardial ablation focused on complete isolation of the pulmonary veins and the posterior LA. Arrhythmia monitoring was performed using either an implantable loop recorder or a Holter. At 1 year follow-up, 80% of the patients were in sinus rhythm, of which 4% had required repeat ablation, and 52% of the patients were free of arrhythmias and not requiring AADs.
Civello et al. conducted a single-center study in 104 patients and included patients with paroxysmal (n = 28, 28%), persistent (n = 31, 30%), and long-standing persistent AF (n = 45, 43%) [20]. Epicardial ablation was performed using the transdiaphragmatic approach and the antrums of the pulmonary veins along with the posterior LA were isolated. Endocardial ablation confirmed posterior wall and pulmonary vein isolation. Mitral annular lines were completed in patients who had atrial flutter. Post-procedure, patients were started on AAD therapy which was continued for 8 weeks. At 12-month follow-up, 72% of the patients were in sinus rhythm and not on any AADs, and 87.5% of the patients were in sinus rhythm with or without AADs.
A single-center study was reported by Zembala et al. using a pericardioscopic approach [21]. A total of 27 patients with persistent (n = 5) and long-standing persistent AF (n = 22) participated in the study. The surgical procedure used the pericardioscopic access and isolated the pulmonary veins and the posterior wall of the LA. Subsequent endocardial ablation was performed to achieve pulmonary vein and posterior LA silence and mitral isthmus ablation. At a follow-up period of 6 months, 18 patients presented for follow-up and 72.2% of them were in sinus rhythm and 66.5% of the patients were no longer requiring AADs.
Finally, Kress et al. retrospectively compared the outcomes of endocardial ablation with hybrid ablation in 133 patients with persistent and long-standing persistent AF [22•]. They compared 69 patients who had endocardial-only ablation and 64 patients who had hybrid ablation using a transabdominal endoscopic approach. The epicardial lesion set comprised of PVI and posterior LA wall ablation. The endocardial portion was done next to complete PVI using either radiofrequency ablation (RFA) or the cryoballoon. Next, CFAEs were ablated using RFA and in patients who continued to remain in AF, LA roof line and mitral isthmus lines were created as well. At a median follow-up of 16 months, 72% of the patients in the hybrid group were free of AF compared to 51% in the endocardial ablation-only group. There was no difference in AAD use between the two groups (55% in hybrid, 48% in the endocardial ablation only).
Subxiphoid pericardioscopic hybrid ablation approach
The subxiphoid approach to pericardioscopic ablation is a novel technique for surgical epicardial access. Through a midline incision, the fascia is incised, the xiphoid is removed, and the sternum is elevated. The pericardial sac is directly entered through a pericardioscopic approach. This avoids a transabdominal, transdiaphragmatic access with its potential risks for abdominal complications (ileus, bleeding, etc.).
The subxiphoid pericardioscopic hybrid approach was described by Gehi et al. in 30 patients, of which 6 had long-standing persistent AF, 23 had persistent AF, and 3 had paroxysmal AF [23]. Using a linear ablation device, epicardial lesions were created around the pulmonary veins with or without right atrial lesions. Additionally, the LAA was excluded. This was then followed by endocardial ablation to complete pulmonary vein isolation, posterior LA isolation, and cavotricuspid isthmus ablation. At a median follow-up of 189 days, 76% of the patients were free of AF.
Summary of different hybrid ablation approaches
Although each of the hybrid ablation approaches described above has its own merits, none is clearly superior to the others. It is difficult to understand the overall value of a hybrid ablation approach and is even more difficult to compare efficacy and safety of the approaches described in these studies for a number of reasons. The surgical access, ablation tools, and lesions sets are variable and are frequently determined by the particular skills and preferences of the surgeon. The patient population differs with many studies including paroxysmal AF patients or those with early persistent AF and without structural heart disease who may be well served with an endocardial catheter ablation procedure. The level of monitoring is variable with some studies performing periodic Holter monitoring and others using implantable loop recorders. And finally, the case series often include a limited number of patients from a single center.
Staged vs. non-staged
Staging ablation (i.e., having a period between the epicardial and endocardial component of the hybrid ablation) allows for the maturing of epicardial lesions, eliminates the effect of edema, and may allow for better evaluation of gaps in the lesion set. However, staging the ablation procedure creates an interim period where patients may have unstable iatrogenic flutters which sometimes complicate epicardial-only ablation, particularly in patients undergoing a de novo hybrid ablation procedure (rather than a redo ablation procedure).
One study by Richardson et al. compared the staged vs. sequential approaches to determine whether one may be better for efficacy [24]. They retrospectively analyzed patients who underwent thoracoscopic epicardial and endocardial ablation in either a staged or a sequential manner. A total of 83 patients with long-standing persistent AF underwent the procedure with 52 undergoing a sequential approach on the same day and 31 following a staged approach. They concluded that the staged approach allowed for better detection of incomplete PV isolation but it did not improve outcomes in regard to recurrence of atrial arrhythmia.
Conclusion
Hybrid AF ablation offers the potential for synergistic benefits of the epicardial and endocardial ablation approaches. However, although several studies of hybrid AF ablation have demonstrated clear benefit, it remains unclear which lesion set, ablation tool, and surgical approach provides the most efficacious procedure while minimizing the risk for complications. Nevertheless, until catheter ablation approaches demonstrate improved efficacy in patients with persistent and long-standing persistent AF or those with significant structural heart disease, there remains a potential role for hybrid AF ablation.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Prasad SM, Maniar HS, Camillo HS, et al. The Cox maze III procedure for atrial fibrillation: long-term efficacy in patients undergoing lone vs. concomitant procedures. J Thorac Cardiovasc Surg. 2003;126(6):1822–8. https://doi.org/10.1016/S0022-5223(03)01287-X.
Robertson JO, Saint LL, Leidenfrost JE, Damiano RJ Jr. Illustrated techniques for performing Cox-Maze IV procedure through a right mini-thoracotomy. Ann Cardiothorac Surg. 2014;3(1):105–16. https://doi.org/10.3978/j.issn.2225-319X.2013.12.11.
Cox JL. The surgical treatment of atrial fibrillation. IV. Surgical technique. J Thorac Cardiovasc Surg. 1991;101(4):584–92.
Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339(10):659–66. https://doi.org/10.1056/NEJM199809033391003.
Ganesan AN, Shipp NJ, Brooks AJ, et al. Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(2):e004549. https://doi.org/10.1161/JAHA.112.004549.
McCready J, Smedley T, Lambiase PD, et al. Predictors of recurrence following radiofrequency ablation for persistent atrial fibrillation. Eur Secur. 2011;13:355–61.
Mahapatra S, LaPar DJ, Kamath S, Payne J, Bilchick KC, Mangrum JM, et al. Initial experience of sequential surgical epicardial-catheter endocardial ablation for persistent and long-standing persistent atrial fibrillation with long-term follow-up. Ann Thorac Surg. 2011;91(6):1890–8. https://doi.org/10.1016/j.athoracsur.2011.02.045.
Bulava A, Mokracek A, Hanis J, Kurfirst V, Eisenberger M, Pesl L. Sequential hybrid procedure for persistent atrial fibrillation. J Am Heart Assoc. 2015;4(3):e001754. https://doi.org/10.1161/JAHA.114.001754.
Krul SP, Driessen AH, van Boven WJ, et al. Thoracoscopic video-assisted pulmonary vein antrum isolation, ganglionated plexus ablation, and periprocedural confirmation of ablation lesions: first results of a hybrid surgical-electrophysiological approach for atrial fibrillation. Circ Arrhythm Electrophysiol. 2011;4(3):262–70. https://doi.org/10.1161/CIRCEP.111.961862.
Pison L, La Meir M, van Opstal J, Blaauw Y, Maessen J, Crijns HJ. Hybrid thoracoscopic surgical and transvenous catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2012;60(1):54–61. https://doi.org/10.1016/j.jacc.2011.12.055.
La Meir M, Gelsomino S, Luca F, et al. Minimally invasive surgical treatment of lone atrial fibrillation: early results of hybrid versus standard minimally invasive approach employing radiofrequency sources. Int J Cardiol. 2013;167(4):1469–75. https://doi.org/10.1016/j.ijcard.2012.04.044.
Pison L, Gelsomino S, Luca F, et al. Effectiveness and safety of simultaneous hybrid thoracoscopic and endocardial catheter ablation of lone atrial fibrillation. Ann Cardiothorac Surg. 2014;3(1):38–44. https://doi.org/10.3978/j.issn.2225-319X.2013.12.10.
Kurfirst V, Mokracek A, Bulava A, et al. Two-staged hybrid treatment of persistent atrial fibrillation: short-term single-centre results. Interact Cardiovasc Thorac Surg. 2014;18(4):451–6. https://doi.org/10.1093/icvts/ivt538.
La Meir M, Gelsomino S, Luca F, Lorusso R, Gensini GF, Pison L, et al. Minimally invasive thoracoscopic hybrid treatment of lone atrial fibrillation: early results of monopolar versus bipolar radiofrequency. Interact Cardiovasc Thorac Surg. 2012;14(4):445–50. https://doi.org/10.1093/icvts/ivr142.
Munretto C, Bisleri G, Bontempi L, et al. Successful treatment of long persistent atrial fibrillation by means of a hybrid thoracoscopic-transcatheter approach. Innovations. 2012;7(4):254–8.
Bisleri G, Rosati F, Bontempi L, Curnis A, Muneretto C. Hybrid approach for the treatment of long-standing persistent atrial fibrillation: electrophysiological findings and clinical results. Eur J Cardiothorac Surg. 2013;44(5):919–23. https://doi.org/10.1093/ejcts/ezt115.
• Gehi AK, Mounsey JP, Pursell I, et al. Hybrid epicardial-endocardial ablation using a pericardioscopic technique for the treatment of atrial fibrillation. Heart Rhythm. 2013;10(1):22–8. This is one the largest series of hybrid AF ablation using the pericardioscopic technique which allows for direct access to the pericardium with shorter recovery times compared to the other surgical approaches. It included patients with serious comorbidities and found a reasonable success rate in this complex patient population. https://doi.org/10.1016/j.hrthm.2012.08.044.
Gersak B, Pernat A, Robic B, et al. Low rate of atrial fibrillation recurrence verified by implantable loop recorder monitoring following a convergent epicardial and endocardial ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2012;23(10):1059–66. https://doi.org/10.1111/j.1540-8167.2012.02355.x.
• Gersak B, Zembala MO, Muller D, et al. European experience of the convergent atrial fibrillation procedure: multicenter outcomes in consecutive patients. J Thorac Cardiovasc Surg. 2014;147(4):1411–6. This is one of the only multi-center studies of hybrid AF ablation and it only included patients with either LSP or persistent AF. It showed that the convergent hybrid procedure is successful at achieving sinus rhythm in this patient population and the need for repeat procedures is low. https://doi.org/10.1016/j.jtcvs.2013.06.057.
Civello KC, Smith CA, Boedefeld W, et al. Combined endocardial and epicardial ablation for symptomatic atrial fibrillation: single center experience. J Innov Card Rhythm Mgmt. 2013;4(9):1367.
Zembala M, Filipiak K, Kowalski O, Boidol J, Sokal A, Lenarczyk R, et al. Minimally invasive hybrid ablation procedure for the treatment of persistent atrial fibrillation: one year results. Kardiol Pol. 2012;70(8):819–28.
• Kress DC, Erickson L, Choudhuri I, et al. Comparative effectiveness of hybrid ablation versus endocardial catheter ablation alone in patients with persistent atrial fibrillation. JACC: Clinical Electrophysiology. 2017;3(4):341–9. This is the most recent study looking at hybrid AF ablation vs. endocardial catheter ablation. It showed that the hybrid group had higher freedom from AF and less need for repeat ablation.
Gehi AG, Caranasos T, Mounsey JP et al. Initial experience with trans-xiphoid hybrid endocardial and epicardial ablation for atrial fibrillation. HRS Abstract. Heart Rhythm. 2017;14(5)Supp:S181.
Richardson TD, Shoemaker BM, Whalen SP, et al. Staged versus simultaneous thoracoscopic hybrid ablation for persistent atrial fibrillation does not affect time to recurrence of atrial arrhythmia. J Cardiovasc Electrophysiol. 2016;27(4):428–43. https://doi.org/10.1111/jce.12906.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Khola Tahir and Thomas Caranasos each declare no potential conflicts of interest. Andy Kiser is a consultant for Atricure, Inc. J. Paul Mounsey is a consultant for Atricure, Inc., Boston Scientific, and Medtronic. Anil Gehi reports research funding from Bristol-Myers Squibb Foundation and speaker’s honoraria from Zoll Inc. and Abbott Inc.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Arrhythmia
Rights and permissions
About this article
Cite this article
Tahir, K., Kiser, A., Caranasos, T. et al. Hybrid Epicardial-Endocardial Approach to Atrial Fibrillation Ablation. Curr Treat Options Cardio Med 20, 25 (2018). https://doi.org/10.1007/s11936-018-0613-3
Published:
DOI: https://doi.org/10.1007/s11936-018-0613-3