Abstract
Purpose of Review
This review aims to provide an overview of how cardiovascular imaging can help individualize preventive cardiovascular care, while focusing on the implications of various recent noninvasive and invasive imaging studies for the field of preventive cardiology.
Recent Findings
Coronary artery calcium (CAC) has established itself as a well-validated tool for detecting the presence or absence of coronary atherosclerosis and thus can provide a more precise measurement of risk than many commonly used risk scores. While individuals with no CAC have an excellent prognosis, those with even minimal CAC have an increased risk of adverse cardiovascular outcomes. These findings have now been extended across several different patient cohorts, including younger patients (e.g., age 35–46 years), for whom the presence of any plaque is associated with a substantially higher risk. Aside from helping to guide the need for various preventive therapies, the detection of CAC may lead to improved risk factor modifications and enhance patient compliance. The implications of these studies include the fact that the incidental identification of CAC on nongated chest CT scans in patients without prior known CAD should prompt intensification of preventive therapies. Recent trials have suggested that among patients with stable symptoms, coronary CTA, as compared to functional testing, leads to higher initiation and intensification of preventive strategies, and a lower incidence of future myocardial infarction. As such, it imperative to use the results of cardiovascular imaging tests—which are often ordered to evaluate symptoms, and not necessarily for implementing preventive therapies—in a way that would promote more aggressive preventive therapies to individuals who have evidence of subclinical atherosclerotic cardiovascular disease.
Summary
Cardiovascular imaging in both asymptomatic and symptomatic patients can have significant implications on long-term preventive treatments and allows for a more precise assessment of risk. Consequently, physicians should routinely incorporate the results of any available imaging studies together with clinical data, when deciding on the role and intensity of various pharmacologic and lifestyle changes. Communication of such findings with patients could enhance adherence and is essential for optimal patient-centered care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of morbidity and mortality in the world, and represents a continuing crisis of epidemic proportions. With escalating health care costs, there has been an increasing emphasis on how to improve efforts to prevent ASCVD. In healthy individuals without prior history of ASCVD, the risk of development of ASCVD is highly influenced by the interplay between multiple risk factors. These risk factors, which include hypertension, dyslipidemia, diabetes mellitus, and obesity, form the cornerstone of ASCVD prevention.
Cardiovascular prevention efforts are often guided by the assessment of a patient’s overall cardiovascular risk based on probabilistic risk scores which utilize cardiovascular risk factors to estimate future ASCVD risk. For instance, the widely utilized Framingham risk score (FRS) uses age, gender, total cholesterol, high-density lipoprotein cholesterol, smoking status, systolic blood pressure and blood pressure treatment status to estimate the 10-year risk of a myocardial infarction in patients without heart disease or diabetes. However, limitations have emerged regarding the FRS, including concerns about whether it can be generalized to nonwhite populations, and its applicability to women [1]. Accordingly, the more recently released 2013 American College of Cardiology/American Heart Association (ACC/AHA) has developed an ASCVD risk equation that was derived from multiple patient cohorts, and provides equations for men and women, in addition to different equations for white and African-American individuals [2].
The traditional paradigms for the prevention of ASCVD have embraced such risk-based approaches, linking the intensity of preventive therapy with a calculation of an individual’s absolute risk. However, multiple studies have now highlighted the underlying shortcomings when applying these probabilistic scores derived from large populations to an individual patient. For example, it is estimated that current pooled cohort equation may broadly overestimate ASCVD risk [3], potentially leading to overtreatment in individuals unlikely to benefit from long-term treatment with statins and aspirin, with potential for increased cost and adverse clinical consequences.
In order to better match the intensity of preventive therapies with an individual’s risk, more refined approaches to risk assessment are needed. Ideally, we should be able to accurately assess the absolute cardiovascular risk of an individual patient, calculate the likelihood of benefit or harm from an intervention, and prescribe therapies after a frank discussion of specific risks and benefits. Indeed, such a process would allow for a model of shared decision making between providers and patients. Cardiovascular imaging can provide an objective assessment of the extent and severity of atherosclerosis, and offers the strongest measure of future risk. This may be due to the fact that the burden of plaque represents the interplay of multiple pathways resulting from the lifetime exposure to both known and unknown risk factors. Early detection and visualization of disease may represent an opportunity for patients and health care providers alike to modify the disease process by implementing evidence-based therapies and adoption of a healthy lifestyle.
Over the past few years, there have been a number of clinical studies in the field of cardiovascular imaging, which have important implications for the prevention of ASCVD events. In addition, several studies have highlighted that incorporating imaging into the primary prevention decision making strategy may result in superior diagnostic accuracy with improved cost-effectiveness. The role of this current review is to provide an overview of these cardiovascular imaging-based clinical studies and highlight the potential implication of these studies for the paradigm of primary prevention of ASCVD.
Detection of Underlying Coronary Artery Disease
Coronary Artery Calcium Scoring Studies
Coronary artery calcium (CAC) scoring provides a quantitative and reproducible measurement of the calcified portion of coronary plaque that, when elevated, is pathognomonic for coronary atherosclerosis and strongly predictive of future coronary heart disease events. Measurement of CAC allows for a score which integrates the effect of exposure to both known and unknown risk factors in an individual patient. Unlike risk factors, CAC scanning can be used to accurately estimate actual atherosclerotic disease burden, as previously shown by Rumberger et al. [4]. In the 2010 American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) Task Force on Practice Guidelines for the assessment of cardiovascular risk in asymptomatic adults, measurement of CAC with CT imaging received a Class IIa recommendation stating that “measurement of CAC is reasonable for cardiovascular risk assessment in asymptomatic adults at intermediate risk (10% to 20% 10-year risk).” [5] The potential role of CAC assessment was also stated in the updated 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk, which stated that “assessing CAC is likely to be the most useful of the current approaches to improving risk assessment among individuals found to be at intermediate risk after formal risk assessment” [2].
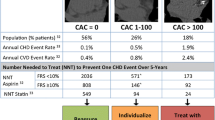
To date, CAC screening has been studied in more than 100,000 patients, including multiple large prospective studies with long-term follow-up of up to 10 years [6, 7]. A common theme across all these studies has been the consistent ability of CAC to assess cardiovascular risk in asymptomatic patients beyond that provided by other noninvasive tests and risk calculators. Multiple studies have demonstrated that assessment of CAC can reclassify patients deemed intermediate risk by the traditional risk calculators, into low- and high-risk categories—an important distinction when counseling patients and directing therapies. In two large studies, Multi-Ethnic Study of Atherosclerosis (MESA) and Heinz-Nixdorf Recall studies, net reclassification improvement was achieved in 54.4 and 65.6% of patients, respectively, who were deemed “intermediate” risk by standard assessment [8]. Assessment of CAC can also highlight the discordance between assessment of traditional risk factors and underlying CAC [9•]. Data from MESA has highlighted the discordance of risk factors and CAC severity, where CAC = 0 was observed in 35% of patients with ≥3 modifiable risk factors, compared with 12 and 5% of patients with no risk factors having CAC >100 and >300, respectively [10]. Importantly, patients with CAC but no risk factors have a substantially higher event rate than those who have multiple risk factors but no CAC [10] (Fig. 1). Thus, even patients with low and high risk by traditional risk assessment tools may benefit from CAC testing.
Discrepancy between CAC and traditional risk factor burden. Total (a) and hard (b) coronary heart disease event rates (per 1000 person-years) with increasing coronary artery calcium (CAC) score according to risk factor burden in the Multi-Ethnic Study of Atherosclerosis (MESA) evaluating a prospective observational cohort of 6814 men and women, aged 45–84 years without known cardiovascular disease. The overall event rate is low among patients with zero CAC score even with the presence of significant risk factors. (Used with permission from European Heart Journal (2014) 35, 2232–2241)
An important feature of CAC testing is its high sensitivity level, and subsequently its greatest value lies in its negative predictive value when the CAC score is 0. Numerous studies have now shown that individuals with CAC = 0 have an excellent prognosis. Across studies, patients with CAC = 0 have a very low risk of future events (<0.1%/year risk of coronary heart disease [CHD]). Conversely, patients with CAC ≥ 100 are at significant risk of CHD with a tenfold increased event rate compared with CAC = 0. Even minimal CAC (CAC = 1–10) carries a twofold increase in CV events (stroke, myocardial infarction, or cardiac death) over 10 years compared with CAC = 0 [11].
While most of the trials have established the role of CAC in patients older than 45 years, the recently published Coronary Artery Risk Development in Young Adults (CARDIA) Study established the prognostic role of CAC among young patients with potential implications on primary prevention [12]. This study evaluated CAC in 3043 adults aged 32 to 46 years, with a mean age of only 40.3 years. In this young cohort, 10.2% of patients were noted to have any CAC, which 5-years later increased to 20.1%, and 10-years later increased to 28.4%. During the 12½ years of follow up, among the 309 participants (10.2%) who were noted to have any CAC there was a higher incidence of coronary heart disease (hazard ratio 5.0) and cardiovascular disease (hazard ratio 3.0), after adjusting for CVD risk factors and demographic variables. Even low CAC scores (i.e., 1–19 and 20–99) at young age were associated with CHD events by middle age. It has long been recognized based on autopsy studies that most persons between 20 and 29 years of age have some degree of coronary fatty streaks, regardless of sex, race, or national origin [13]. While this fatty streaking is clinically harmless and potentially reversible, progression to fibrous plaques and more advanced lesions often leads to a critical stage of atherosclerosis in which clinical disease develops. The CARDIA study is an important step forward which has highlighted the increase in the prevalence of CAC among adults from their third to fifth decade of life. This striking increase of CAC suggests that aggressive medical management of risk factors and implementation of preventive measures at an early age may be a key component for improving outcomes related to ASCVD.
The role of CAC in primary prevention was explored in the Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research (EISNER) trial, which highlighted the potential role of CAC scoring in guiding physician behavior for primary prevention of ASCVD [14]. In the EISNER study, 2137 subjects with underlying coronary artery disease risk factors were randomized to either a CAC scan at baseline or no CAC scan at baseline in a 2:1 ratio. In addition, all subjects received a one-time risk factor counseling session after risk assessment. During a follow-up period of 4 years, the CAC scan group manifested a net favorable improvement in serum low-density lipoprotein, systolic blood pressure, and weight (for those who were overweight at baseline) with an overall more favorable change in FRS, as compared to the group that was randomized to risk factor counseling without CAC scanning (Tables 1). Notably, the observed benefit in the scan group was attributable to a favorable increase in medications among those with increasing CAC scores.
Since cardiac imaging tests themselves do not directly influence patient outcomes, the proposed mechanism for any benefits is via improved downstream lifestyle changes and medical management. As suggested by the EISNER study and others, CAC scanning can provide a unique opportunity to not only provide a better estimation of an individual’s risk, but also to initiate more aggressive medical management based on the presence and magnitude of CAC abnormality. The direct visualization of plaque can concretize the reality of disease for patients, thus serving to increase patients’ motivation. This may serve as motivation to adopt a healthier lifestyle and adhering to both, pharmacological treatments as shown by Kalia et al. [15], or to non-pharmacological interventions, such as dietary changes and exercise, as shown by Schawrtz et al. [16]. In the latter study, after a mean of 6 years, those with a CAC score greater than 0 were more likely to increase their exercise (19 vs 12%, P < .01) and change their diet (33 vs 21%, P < .01). A recent meta-analysis evaluated the changes in pharmacological and lifestyle cardiovascular preventive therapies in patients with non-zero versus zero CAC score [17]. This meta-analysis, which evaluated six studies, found that identifying calcified coronary plaque, significantly increased the likelihood of initiation of aspirin and blood pressure lowering medications, initiation and continuation of lipid lowering medications, as well as intensification of exercise and dietary changes.
While the prognostic role of measured CAC score has been widely described and validated, in recent years there have been a few studies which have highlighted the finding of incidental coronary artery calcium on non-contrast chest CT scans obtained for indications other than evaluation of coronary artery disease. Prior studies have shown that there is a good correlation between the CAC score obtained from 3 mm thick slices ECG-gated CT scans performed exclusively for CAC score evaluation, vis-à-vis 6 mm thick non-gated chest CT scans which are routinely performed for other clinical indications. In a nested case study by Hughes-Austin et al. which evaluated 157 deaths and 494 controls in a cohort of 4544 symptomatic individuals undergoing both 6 mm non-contrast non-gated CT scans and 3 mm non-contrast gated electron beam CT scans, the correlation coefficient for Agatston CAC scores was 0.93 (p < 0.001); with median CAC Agatston scores lower for the 6 mm scans (22 vs. 104), as would be expected with thicker slices [21]. In addition, each SD higher CAC score on 6 mm CTs was associated with 50% higher odds of death (odds ratio 1.5; 95% confidence interval 1.2 to 1.9), similar to the 50% higher odds for the 3 mm electrocardiography-gated CTs (odds ratio 1.5; 95% confidence interval 1.1 to 1.9). Similar hazard ratios were noted for CAC categories between the non-gated and gated scans: 1.9 and 2.1 for CAC 1 to 100, 2.3 and 2.1 for CAC 101 to 300, and 2.6 and 2.9 for CAC >300. This study highlights that it is important for radiologists to report and treating physicians to use any data which may be available to them from chest CT scans, and how incidental CAC can play a pivotal role in tailoring primary prevention strategies for prevention of ASCVD related morbidity and mortality.
There is now an increasing number of non-gated chest CT scans that are expected to be performed, due to the recent endorsement by the 2014 US Preventive Services Task Force for low-dose lung CT scanning for cancer detection, and the 2014 Center for Medicare and Medicaid Services decision to provide coverage for lung scans in a defined high-risk population estimated to be >7 million individuals [22]. This represents a substantial opportunity to expand primary prevention strategies among patients found to have incidental CAC. However, there remain challenges regarding both the reporting, and the interpretation of incidentally noted CAC score. These challenges were highlighted in a study published by Uretsky et al., in which 201 patients without a history of ASCVD who were referred for a noncoronary chest CT scan for noncardiac indications were evaluated for the presence of CAC [23]. In this study, 53% patients (108/201) had incidentally noted CAC, of which 69% patients (74/108) had the presence of incidental CAC mentioned on their report. Of note, among the 74 patients with reported incidental CAC, there was an increase in statin and aspirin prescription of only 4 and 5%, respectively, prior to hospital discharge. These findings underscore the importance of both, training imager to detect and report CAC on non-cardiac CT studies, and educating clinicians and patients regarding the prognostic and clinical implications of detecting CAC. It is also important to recognize that despite the high correlation for CAC score between non-gated and gated chest CT scans, non-gated chest CT is not as sensitive as the standard ECG-gated 3 mm CAC [21]. Low CAC scores detected by standard CAC scans may not be visible. Thus, it would not be appropriate to use these scans for purposes of downscaling treatment.
Coronary CTA Studies
Coronary CTA has emerged as a powerful tool for the diagnosis of CAD and has been shown in multiple large trials to have the highest sensitivity of all noninvasive tests for detecting obstructive CAD and a high negative predictive value (>95%). CTA has the unique advantages over CAC testing of detecting non-calcified coronary plaque and assessing the presence and degree of coronary stenosis. However, while the utility of coronary CTA in patients with underlying symptoms is well established, its routine use in asymptomatic patients is not currently recommended, given the lack of demonstrable benefits [24, 25], particularly when compared with CAC testing [26, 27].
Over the last few years, coronary CTA is being increasingly utilized for the evaluation of patients with chest pain. A few recently concluded multicenter studies which evaluated patients with stable chest pain, including the PROspective Multicenter Imaging Study for Evaluation of chest pain (PROMISE) trial [18] and the Scottish COmputed Tomography of the HEART (SCOT-HEART) trial [19], provide important information about the potential impact of coronary CTA on the downstream clinical outcomes. In the SCOT-HEART study, during a median follow up period of 1.7 years, patients were randomly assigned to either standard care—which was most commonly an exercise treadmill test, or to standard care plus CAC score and coronary CTA. This imaging based arm was associated with a 38% reduction in fatal and nonfatal myocardial infarction (HR 0·62, 95% CI 0·38–1·01; p = 0·0527). The reduction in MI was even more significant (HR 0.50 p = 0.02) when differences in outcomes were only compared after 50 days in a post-hoc analysis, given that changes in patient management did not occur directly after the imaging tests were performed. Subsequently, in a small meta-analysis, involving a cohort of 14,637 patients among three studies, a statistically significant reduction in the risk of myocardial infarction after coronary CTA was noted compared to usual standard of care (relative risk 0.68; 95% CI 0.49–0.98; P = 0.038) (Fig. 2) [28•].
Three meta-analysis studies. Forest plot of the pooled weighted annualized incidence rate ratio for myocardial infarction, demonstrating the reduced incidence of myocardial infarction among stable chest pain patient randomized to coronary CT as compared to usual care or functional testing. (Used with permission from Circ Cardiovasc Imaging. 2016 Apr;9(4):e004419)
Although these studies are not sufficiently powered to determine the possible reason for lower incidence of myocardial infarction during follow-up, one proposed hypothesis is that since coronary CTA has high sensitivity to detect any coronary artery plaque, this aids in the early detection of coronary artery disease and subsequently leads to a higher utilization of primary prevention strategies, including aggressive risk factor modification and promotion of healthy behaviors [29••]. The data from the SCOT-HEART and PROMISE trials provide credence to this hypothesis. In the SCOT-HEART trial, there was an increase in the use of preventive strategies in the coronary CTA arm as compared to the usual standard of care arm (18 vs. 4% respectively; p < 0·0001). Similarly, in the PROMISE trial, at a median of 60 days after the initial test, the coronary CTA strategy was associated with a higher proportion of patients newly initiating aspirin (11.8 vs. 7.8%), statins (12.7 vs. 6.2%), and b-blockers (8.1 vs. 5.3%), compared to functional testing (P < 0.0001 for each) [29••].
These results highlight that in appropriately selected patients, use of coronary CTA may help guide patient management and implement preventive therapies. Interestingly, in a secondary analysis of the PROMISE study, a positive initial test result, either CCTA or functional testing, and early revascularization, compared with negative initial test results or no early revascularization were associated with higher aspirin (71.2 vs. 49.4%), statin (70.7 vs. 50.6%), and b-blocker (48.8 vs. 26.8%) use at 60 days (P < 0.0001 for each) [29••]. The authors of this study concluded that positive initial test results and revascularization are primary drivers of changes in preventive medical and lifestyle practices, with test type only making secondary contributions.
It is important to emphasize that other clinical data, such as risk factors can also drive primary prevention management, among patients undergoing cardiac imaging procedures. This ability is well illustrated in a study by Uretsky et al., in which patients admitted to hospital with acute chest pain and unremarkable troponins and electrocardiographic findings were randomized to either cardiac imaging stress test or CCTA [30]. Following hospital admission, there was a similar overall increase in the use of medical therapy between the CCTA arm and the stress test arm, including aspirin (24 vs. 16%; p = 0.3), statin (18 vs. 17%, p = 0.7), and beta blockers (8 vs. 6%, p = 0.9). It is interesting to highlight that while only 5% of the stress tests were abnormal, the absolute increase in the use of aspirin and statins was 24 and 18%, respectively. Among patients undergoing coronary CTA, 49% of patients had underlying coronary artery disease, while the prevalence of obstructive CAD (>50%) was 11%. In the coronary CTA arm, the absolute increase in the use of aspirin and statins was 16 and 17%, respectively.
Invasive Coronary Imaging
Invasive cardiovascular imaging with intravascular ultrasound (IVUS) has played a central role in one of the recent clinical trials evaluating the role of PCSK-9 inhibitors. The GLAGOV (Global Assessment of Plaque Regression With a PCSK9 Antibody as Measured by Intravascular Ultrasound) study evaluated 968 patients with underlying ASCVD who were treated with evolocumab, a PCSK-9 inhibitor, or placebo for 76 weeks, and who underwent serial intravascular ultrasound studies for determination of coronary atheroma volume [20••]. In this study, the use of evolocumab was associated with a marked reduction in LDL cholesterol as well as a reduction in percent atheroma volume.
The use of IVUS in the GLAGOV study provided evidence that achieving very low LDL cholesterol levels (time weighted mean LDL cholesterol of 36.6 mg/dl) can lead to small, yet significant, plaque regression, and that this benefit may occur regardless of baseline LDL cholesterol level. In addition, the study results suggest that there may be a linear association between achieved LDL cholesterol and plaque volume regression for LDL-C levels ranging from 110 mg/dl to as low as 20 mg/dl. Importantly, the use of evolocumab has also been shown to decrease cardiovascular events in the FOURIER trial [31]. Both of these studies suggest that plaque regression may play a mechanistic role in reducing CV events. While both the GLAGOV and FOURIER studies were conducted in patients with known ASCVD, PCSK9 inhibitors may ultimately have a role in primary prevention, especially in patients with sub-optimal LDL-C levels despite high dose statins or those who are intolerant of statins. However, given the increased cost of PCSK9 inhibitors, these agents are likely to be most cost effective in those who have the highest absolute risk. Importantly, CV imaging has the greatest potential to identify such patients, as patients who have a significant burden of CAC or ischemia, often have an event rate which is comparable to those who have established ASCVD. The salient clinical features of the important clinical trials discussed in this review are summarized in Table 2.
Conclusions
Although the rate of death from ASCVD has been on the decline over the past several decades, ASCVD still remains the most common cause of morbidity and mortality in most countries. Thus, there is a need to improve our ability to assess patient risk and improve risk factor management. As the options and costs of preventive therapies increase, such as the recent advent of PCSK9 inhibitors, it is becoming ever more imperative that we improve our accuracy in ascertaining which patients are at high or low risk for adverse cardiac events—both to maximize the usage of prevention management for those at greatest risk and decrease unnecessary therapies for those at low risk. Based on data reviewed herein, we propose a conceptual framework by which cardiovascular imaging may improve ASCVD risk assessment and management through multiple avenues and across different patient populations (Fig. 3). In asymptomatic subjects, coronary calcium scanning may be used to guide the intensity of risk factor management. Among patients with chest pain symptoms, either work-up through atherosclerotic imaging (coronary CTA or CAC scanning) or ischemia testing (either using exercise ECG or more advanced stress imaging) may be used to determine if CAD is present and guide patient management according to the presence and magnitude of atherosclerotic disease or ischemia. Improved risk assessment can assist physicians by helping them to identify those patients who are at high and low risk, thereby helping them to better gauge the required need and intensity of risk factor management and the required degree of follow-up and monitoring that will be required of their patients. Similarly, more accurate and confident risk assessment can help improve patient self-management by making patients cognizant of their clinical risk, motivating those at identified high risk to make necessary lifestyle changes, and assisting patients in making meaningful shared decisions about their care with their physicians.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nasir K, Blaha MJ. Short and lifetime cardiovascular risk estimates: same wine, different bottles. Do we have the COURAGE to abandon risk scores? J Nucl Cardiol. 2014;21:46–9.
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol. 2014;63:2935–59.
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet (London, England). 2013;382:1762–5.
Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157–62.
Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice guidelines. Circulation. 2010;122:e584–636.
Gibson AO, Blaha MJ, Arnan MK, et al. Coronary artery calcium and incident cerebrovascular events in an asymptomatic cohort. The MESA study. JACC Cardiovasc Imaging. 2014;7:1108–15.
Kavousi M, Elias-Smale S, Rutten JH, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156:438–44.
Nasir K, Shaw LJ, Budoff MJ, Ridker PM, Pena JM. Coronary artery calcium scanning should be used for primary prevention: pros and cons. JACC Cardiovasc Imaging. 2012;5:111–8.
• Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (multi-ethnic study of atherosclerosis). J Am Coll Cardiol. 2015;66:1657–68. This paper provided useful information on how the ASCVD risk score can be used in selecting individuals who are most likely to benefit from CAC testing.
Silverman MG, Blaha MJ, Krumholz HM, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the multi-ethnic study of atherosclerosis. Eur Heart J. 2014;35:2232–41.
Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009;2(6):675–88.
Carr JJ, Jacobs DR Jr, Terry JG, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol. 2017;2(4):391–9.
Strong JP, Malcom GT, Newman WP 3rd, Oalmann MC. Early lesions of atherosclerosis in childhood and youth: natural history and risk factors. J Am Coll Nutr. 1992;11(Suppl):51s–4s.
Rozanski A, Gransar H, Shaw LJ, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (early identification of subclinical atherosclerosis by noninvasive imaging research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–32.
Kalia NK, Miller LG, Nasir K, Blumenthal RS, Agrawal N, Budoff MJ. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. 2006;185:394–9.
Schwartz J, Allison M, Wright CM. Health behavior modification after electron beam computed tomography and physician consultation. J Behav Med. 2011;34:148–55.
Gupta A, Varshney R, Lau E, Hulten E, Bittencourt MS, Blaha MJ, et al. The identification of coronary atherosclerosis is associated with initiation of pharmacologic and lifestyle preventive therapies: a systematic review and metaanalysis. Poster presented at: 2016 American College of Cardiology (ACC). 65th Annual scientific session and expo; Chicago, IL.
Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372:1291–300.
SCOT-HEART investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet (London, England). 2015;385:2383–91.
•• Nicholls SJ, Puri R, Anderson T, et al. Effect of evolocumab on progression of coronary disease in statin-treated patients: the GLAGOV randomized clinical trial. JAMA. 2016;316:2373–84. This study showed that lower LDL can cause plaque regression; this benefit may occur at any LDL level.
Hughes-Austin JM, Dominguez A 3rd, Allison MA, et al. Relationship of coronary calcium on standard chest CT scans with mortality. JACC Cardiovasc Imaging. 2016;9:152–9.
Moyer VA, Force USPST. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:330–8.
Uretsky S, Chokshi N, Kobrinski T, et al. The interplay of physician awareness and reporting of incidentally found coronary artery calcium on the clinical management of patients who underwent noncontrast chest computed tomography. Am J Cardiol. 2015;115:1513–7.
Muhlestein JB, Lappe DL, Lima JA, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA. 2014;312:2234–43.
Cho I, Chang HJ, Sung JM, et al. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM registry (coronary CT angiography evaluation for clinical outcomes: an international multicenter registry). Circulation. 2012;126:304–13.
Hulten E, Bittencourt MS, Ghoshhajra B, et al. Incremental prognostic value of coronary artery calcium score versus CT angiography among symptomatic patients without known coronary artery disease. Atherosclerosis. 2014;233:190–5.
Bittencourt MS, Hulten E, Ghoshhajra B, et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ Cardiovasc Imaging. 2014;7:282–91.
• Bittencourt MS, Hulten EA, Murthy VL, et al. Clinical outcomes after evaluation of stable chest pain by coronary computed tomographic angiography versus usual care: a meta-analysis. Circ Cardiovasc Imaging. 2016;9:e004419. This meta-analysis shows that when compared to patients randomized to functional testing, those who were randomized to CTA had a 32% reduction in the risk of subsequent MI.
•• Ladapo JA, Hoffmann U, Lee KL, et al. Changes in medical therapy and lifestyle after anatomical or functional testing for coronary artery disease. J Am Heart Assoc. 2016;5:e003807. This study highlights the increased use and intensification of primary prevention medications after coronary CTA as compared to functional testing.
Uretsky S, Argulian E, Supariwala A, et al. Comparative effectiveness of coronary CT angiography vs stress cardiac imaging in patients following hospital admission for chest pain work-up: The Prospective First Evaluation in Chest Pain (PERFECT) Trial. J Nucl Cardiol. 2016. doi: 10.1007/s12350-015-0354-6.
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 2017; 376:1713–1722.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Agarwal, Shaw, Berman, Nasir, and Rozanski have no conflicts of interests to disclose.
Dr. Blankstein reports and is a Member, Board of Directors, Society of Cardiovascular Computed Tomography and American Society of Nuclear Cardiology. Dr. Blankstein reports research support from Amgen Inc, Gilead Inc, and has served as a consultant to Amgen Inc. and EKOS Inc.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Novel and Emerging Risk Factors
Rights and permissions
About this article
Cite this article
Agarwal, V., Shaw, L.J., Berman, D. et al. Implications of Recent Clinical Trials in Cardiovascular Imaging on Primary Prevention Therapies. Curr Cardiovasc Risk Rep 11, 20 (2017). https://doi.org/10.1007/s12170-017-0545-6
Published:
DOI: https://doi.org/10.1007/s12170-017-0545-6