Abstract
Chemotherapy agents have greatly improved outcomes and survival of patients with cancer but have also been associated with significant cardiotoxicity. The advent of cardiotoxicity is detrimental to patients both during cancer therapy, by limiting the extent of therapy and therefore chance of cure, and also during cancer survivorship, by causing devastating cardiac morbidity and mortality. In this article, we not only review the types of agents most often associated with cardiotoxicity, proposed mechanisms of cardiac injury, but more importantly, how to attenuate or prevent it all together. We review the available data and evidence for different strategies to prevent cardiac damage during chemotherpathy and propose our own protocols for risk stratification, monitoring, and prevention of cardiotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The discovery of drugs such as anthracyclines, HER2-antagonists and tyrosine kinase inhibitors have transformed some cancers into curable or chronic diseases, albeit at the cost of significant short and long-term cardiac toxicities. With over 18 million survivors expected in the United States alone by 2020 [1], long-term cardiac side-effects of therapy that can impair quality and length of survival [2] have become increasingly more relevant to patients and physicians alike. Whereas late cardiotoxicity can cause crippling cardiac morbi-mortality that may require advanced therapies [3••, 4], acute cardiotoxicity can hinder continued cancer treatment thwarting its success and decreasing survival [5•].
Mounting recognition of this problem has led to the advent of onco-cardiology [6, 7], a collaborative effort between cardiologists and oncologists aimed at reducing cardiotoxicity and mortality of cancer patients and survivors. Whereas much focus has been directed at monitoring and predicting onset of cardiotoxicity, it is clear that measures to prevent it altogether are likely to have a greater impact on outcomes.
Therefore, we herein review the available data on risk evaluation, early detection and, more importantly, prevention of cardiotoxicity in patients undergoing treatment with anthracyclines, HER-2 antagonists and tyrosine kinase inhibitors. We also offer our own approach to managing these patients.
Overview of Types and Mechanisms of Preventable Cardiotoxicity
It has been estimated that up to 42 % of patients receiving anthracyclines and trastuzumab for breast cancer develop heart failure or cardiomyopathy within 3 years of treatment [8]. Conservatively, there are an estimated 20,000-100,000 breast cancer patients with chemotherapy-related cardiotoxicity in the United States [9], and around 100,000-250,000 with established chemotherapy-induced cardiomyopathy [4, 5•, 10, 11]. While most patients are managed medically, some patients progress to end-stage heart failure and may require advanced therapies, such as mechanical circulatory support and heart transplantation [3••, 4].
Anthracyclines, widely used for breast cancer and lymphomas, have traditionally been associated with cardiotoxicity [12] that can be acute, early chronic, or late chronic [13]. Acute cardiotoxicity develops in 3.2 % of patients within days of administration, appears to be inflammatory in nature, and is usually reversible rarely resulting in refractory heart failure (<1 %). The main drawback of acute anthracycline cardiotoxicity is that it often leads to treatment interruption and typically discontinuation of further anthracycline-based therapy, causing the patient to be treated with second line agents that may not be as effective. Acute cardiotoxicity, therefore, needs to be avoided because it decreases the potency and efficacy of treatment and consequently, the chances of cure. The early-onset and late-onset chronic progressive types develop within and after the first year after therapy, respectively, with estimated incidences of 2 % and 5 % of patients [14]. The latter forms of cardiotoxicity can lead to end-stage HF with biventricular dysfunction and require advanced heart failure therapies. This type of cardiotoxicity reduces the quality of life and longevity of cancer survivors and requires enhanced awareness so that patients exposed to anthracyclines get screened at regular intervals for development of subclinical LV dysfunction. Early discovery and treatment of LV dysfunction at Stage B HF, may prolong survival and negate need for advanced therapies [15, 16].
Few risk factors for anthracycline cardiotoxicity have been identified [9, 17], but incidence increases with higher cumulative doses. Diastolic dysfunction occurs at accumulative dose of 200 mg/m2 and systolic dysfunction usually appears at accumulative dose of 400-500 mg/m2 [9, 18]. The risk of developing heart failure increases with the total dose of doxorubicin. The probability of developing heart failure is 5 % at 400 mg/m2, 26 % at 550 mg/m2 and goes up to 48 % at 700 mg/m2 [18]. Other factors that can increase the risk of cardiotoxicity are extremes of age, concomitant or previous chemotherapy, female sex, pre-existing heart disease, hypertension and mediastinal radiation [14, 19, 20].
Trastuzumab is a HER2-antagonist that is used for HER2+ breast cancer as mono- or adjuvant therapy. In phase III trials, 27 % of patients who received trastuzumab-anthracyclines developed HF, compared with 8 % in the anthracycline-only group [21]. Similarly, 13 % of patients receiving trastuzumab-paclitaxel developed HF, compared with 1 % receiving paclitaxel alone [21]. Other studies have reported cardiotoxicity in 3-7 % of patients when trastuzumab is used alone, and as much as 27 % when combined with anthracyclines [22]. Trastuzumab not only increases the incidence of HF, but also its severity. Compared with anthracycline-only group and paclitaxel-only group, patients who received anthracycline-trastuzumab combination therapy were more likely to develop advanced (NYHA class III/IV) heart failure (3 % vs. 16 %, and 1 % vs. 2 %, respectively) [21]. In the experience of the authors and others [23], it is becoming increasingly apparent that trastuzumab alone is only capable of inducing transient LV dysfunction and heart failure, which is usually reversible once it is interrupted and HF treatment is started. The only patients that appear to progress to end-stage HF are those with previous exposure to anthracyclines and/or pre-existing structural heart disease.
Risk factors for trastuzumab-cardiotoxicity have been identified and are useful in selecting a population that may benefit the most from preemptive cardioprotection. Advanced age (>80 years) appears to be a significant risk factor for developing cardiotoxicity (HR, 1.53; 95 % CI, 1.16 - 2.10) [24]. Paradoxically, an abnormal baseline LVEF has not been associated with increased risk for cardiotoxicity [25], however, patients with low EF are usually excluded from therapy with trastuzumab. Also, while concurrent or previous anthracycline use certainly increases the likelihood of LV dysfunction from trastuzumab [21, 22], concomitant radiation therapy to the chest does not [26]. In general, patients with history of pre-existing structural cardiovascular disease and cardiovascular risk factors (diabetes, dyslipidemia, hypertension) are also more likely to develop cardiotoxicity with trastuzumab [27, 28].
Tyrosine kinase inhibitors (TKIs) are yet another group that has been associated with cardiotoxicity. This family of drugs is mainly used for treatment of leukemia and renal cell carcinoma [29–31]. They are multitargeted medications with affinity for VEGF receptor (VEGFR) 1–3, PDGFR, c-Kit, CSF-1R among others [32]. The major toxicities related to these drugs are hypertension, myocardial ischemia and left ventricular dysfunction. Hypertension results from VEGF pathway inhibition, leading to vasoconstriction and microvascular dysfunction, a pathway common to all TKIs targeting VEGF-receptors [33]. Hypertension occurs in more than half of the patients on several TKIs up to 66 % in patients with Lifinanib [34]. Acute coronary syndrome has been associated with sorafenib and occurred in 2.9 % (vs. 0.4 % in the placebo group) [35], a phenomenon that might be associated with angiogenesis inhibition and LV remodeling in response to hypertension. LV systolic dysfunction (grade 3/4) occurs in up to 5-28 % of patients treated with sunitinib [29]. These toxicities are usually managed medically and can be reversible, but little is known about their long-term prognosis [29, 36].
The antimetabolite 5-fluorouracil and its pro-drug capecitabine, are widely used for treatment of gastrointestinal tumors with a wide spectrum of cardiotoxicity reported at 1.2-18 % [37, 38]. The most common cardiac side effect is that of coronary vasospasm, through activation of protein-kinase C [39], which can be exacerbated by the presence coronary artery disease [40]. Anecdotal evidence suggests that vasodilators (e.g., nitroglycerin) and calcium channel blockers may protect against vasospasm [41, 42], however failure with this strategy has also been reported [43].
Diagnosis and Surveillance
Imaging
Conventional Echocardiography and Multiple Gated Acquisition (MUGA) scan
Cardiotoxicity is defined clinically as a greater than 10 % decrement in LVEF from baseline measurement. This definition has been endorsed by ASCO and guidelines recommend serial LVEF measurements in patients receiving high doses of doxorubicin [44]. Owing to its wide availability and wealth of information it provides, echocardiography is the modality of choice for monitoring and detection of cardiotoxicity. The major disadvantage of echocardiography is that it is largely operator-dependent and therefore has higher intra and inter-observer variability when compared to multiple gated acquisition (MUGA) scans [45, 46]. Although choice of modality is institution-dependent, it is important that the same method be used consistently for reliable LVEF comparisons. It is also essential that LVEF be always measured as recommended by the American Society of Echocardiography [47] and not be visually estimated, and although commonly used, ranges should be avoided and a definite number be given in the report. The reason for this is that small changes in LVEF can be predictors of significant future cardiotoxicity. For example, in patients with non-Hodgkin lymphoma receiving doxorubicin at doses of 200 mg/m2, a decrease of 4 % in LVEF or more predicted later cardiotoxicity (decrease LVEF < 10 %, and LVEF < 50 %) [48]. However, not surprisingly, cardiotoxicity as expressed by LVEF reductions, has poor correlation with NYHA class.
While LVEF by 2D echocardiography is still the most commonly used method for monitoring and diagnosing cardiotoxicity, 3D LVEF measurements are more accurate and reproducible [49]. In a study of patients with breast cancer receiving cardiotoxic therapies, serial LVEF measurement by 3D echocardiography had less interobserver and intraobserver variability than biplane 2D LVEF measurements over 1 year follow-up (0.017 vs. 0.033, and 0.027 vs. 0.04) [50]. Indeed, among breast cancer patients treated with HER2 antagonists after doxorubicin, MUGA scan and LVEF by 3D echocardiography showed better correlation with cardiac MRI measurements than LVEF by 2D echocardiogram at 12 months (r = 0.95 vs. r = 0.90 vs. r = 0.69) [51].
Lastly, although conventional echocardiography is reliable in diagnosing cardiotoxicity, EF reduction is a relatively late event in the cardiotoxic cascade, and once it occurs, the probability of recovery is just above 50 % [5•]. This realization has prompted development of newer techniques to detect cardiotoxicity more prematurely.
Strain Echocardiography
Strain and strain-rate (deformation imaging) have recently gained attention as potential early markers of cardiotoxicity [52]. Strain echocardiography uses two main methods: speckle tracking and tissue Doppler to assess myocardial dynamics. Strain is presented as percent change, with positive numbers referring to thickening, and negative numbers referring to shortening. Strain rate is the change of strain over time [53] and can measured in different axes, namely: longitudinal, circumferential, and radial (see Fig. 1) [54•]. In mouse models of doxorubicin-induced cardiotoxicity, changes in endocardial systolic velocity and strain rate correlated with hemodynamic changes, preceded changes in LVEF, were associated with late cardiotoxicity, and predicted doxorubicin-induced mortality [55]. Recent reports have validated these findings in humans [56, 57].
Strain imaging in a patient starting chemotherapy (a) longitudinal, (b) radial, and (c) circumferential. Adapted from Thavendiranathan et al. [54•]
In a study of 43 patients with breast cancer followed by echocardiography, longitudinal strain decreased by 11 % at 3 months. This decrease was detected in the midwall (p = 0.008) and the lateral (p = 0.01) and anterior (p = 0.01) segments. The change in longitudinal strain (OR 500, p = 0.01) and radial strain (OR 250, p = 0.02) at 3 months were significantly different in the cardiotoxicity group. Negative predictive value for 10 % decrease in longitudinal strain was 93 % [56]. Other studies have showed similar results with strain imaging. In a study of 81 patients with breast cancer receiving trastuzumab (+/- doxorubicin, +/- radiation), 11 % reduction in GLS had 95 % specificity for cardiotoxicity [58]. In another study of 74 patients with cancer receiving anthracycline-based therapy, 13 % relative reduction in global longitudinal shortening had 79 % sensitivity for cardiotoxicity [59].
In a systematic review on the use of strain for monitoring chemotherapy-induced cardiotoxicity, peak systolic longitudinal strain using Doppler-based strain imaging most consistently detected early cardiotoxicity during chemotherapy [54•]. In fact, a decrement in GLS by 10-15 % was the most useful parameter to predict LVEF reduction and heart failure [54•]. Reductions in circumferential and radial strains are also common, but less consistently reproducible [54•]. However, the management of cardiotoxicity based on strain data is yet to be validated.
Serum Biomarkers
Both animal [60] and human studies [60–62] have shown that troponin can be an early marker of chemotherapy-induced cardiotoxicity. Patients receiving chemotherapy who have high post-treatment troponin levels are more likely to develop LVEF reduction or HF [63]. The level of troponin elevation may even predict reversibility of LVEF abnormalities during treatment [64]. The duration of troponin elevation also seem to be a marker of late development of heart failure or other cardiac events. In 703 cancer patients, early elevation in troponin I was associated with 37 % cardiac events, and persistent elevation was associated with 84 % compared with 1 % cardiac events [62].
Despite these findings, troponin elevation has been an inconsistent marker of cardiotoxicity. Some studies failed to detect troponin elevations even in the presence of echocardiographic findings [65–67]. While sensitivity is unreliable, normal troponin levels during chemotherapy administration can identify patients with the lowest risk for cardiotoxicity (negative predictive value of 99 %) at least one year after chemotherapy while troponin elevation at 3 months can predict cardiotoxicity prior to changes in LVEF [56]. Further, the patterns of troponin elevations may correlate with the severity of cardiotoxicity [60]. Because of logistical issues with timing of blood draws and absence of assay standardization, troponin use is not routinely recommended for monitoring cardiotoxicity.
In a multicenter study of 78 patients with breast cancer receiving doxorubicin and trastuzumab, Ky et al. measured and followed eight biomarkers in association with cardiotoxicity. Risk of cardiotoxicity was higher with changes in troponin I (HR: 1.38 per SD, p = 0.02), and myeloperoxidase (MPO) (HR: 1.34 per SD, p = 0.048). In patients with largest changes in TnI (ΔTnI >121.8 μg/l; ΔMPO >422.6 pmol/l), risk of cardiotoxicity was 46.5 % [68].
Likewise, while some studies have shown increase in BNP levels after chemotherapy, evidence from animal studies have suggested that anthracyclines may decrease the production of BNP and thus levels may be paradoxically low [69].
Subsequent studies evaluating the role of BNP measurement in monitoring patients receiving chemotherapy are promising. Lenihan et al. followed 111 patients receiving anthracycline-based regimens with cardiac biomarkers (troponins and BNP) at baseline and before and after up to six cycles of treatment. BNP was elevated only in the group that developed cardiotoxicity ((heart failure, LVD, sudden death, or arrhythmia) [70].
Skovgaard et al. followed 333 patients receiving cardiotoxic agents for a mean of 1360 days. Sing a BNP of more than 100 pg/ml predicted CHF (HR 5.5; CI 1.8–17.2; p = 0.003). Furthermore, BNP (>100 pg/ml) but not LVEF predicted overall death (HR 1.9; CI 1.3-2.9; p = 0.002) [71].
While BNP can and should be used in patients at higher risk of developing HF for diagnostic purposes, its usefulness in monitoring cardiotoxicity is not yet established.
Endomyocardial Biopsy
Although not useful in trastuzumab or TKI-induced cardiotoxicity, endomyocardial biopsy (EMB) remains the gold standard for diagnosis and grading of anthracycline-induced myocardial damage. Despite being invasive and requiring transvenous approach, EMB carries less than a 6 % risk of complications [72], which include bleeding, transient arrhythmia, valvular injury, pulmonary embolism, and cardiac chamber perforation [73, 74]. Because there is variable myocardial regional involvement, 4-6 biopsies are usually taken from the right and occasionally left ventricle to maximize diagnostic yield [75]. Electron microscopy shows characteristic depletion of myofibrillar bundles, distortion and disruption of the Z-lines, mitochondrial disruption, and myocyte vacuolization [76]. Grading of cardiotoxicity has close correlation with development of left ventricular dysfunction and heart failure [9]. However, given its invasiveness and ready availability of imaging, EMB is usually reserved for cases where there is need to exclude alternative explanations for cardiotoxicity [77].
Medical Prevention of Cardiotoxicity
Advances in detection however, have not translated into significant attenuation of cardiotoxicity, and thus current focus has shifted toward prevention. While animal studies have shown promise in the prevention of chemotherapy, large-scale human studies are still lacking. In a meta-analysis of 14 cardiotoxicity prevention studies with 2015 patients treated with anthracyclines and/or trastuzumab, 83 cardiac events occurred in the treatment group compared with 304 in the control group (RR = 0.31, p < 0.00001). Reduction in cardiac events was attributed to statins (69 % reduction), beta-blockers (69 % reduction), angiotensin antagonists (89 % reduction), and dexrazoxane (65 % reduction) [78••], Table 1.
Statins
Statins have reduced mortality in patients with high risk cardiovascular profiles through lipid lowering and pleotropic effects [79]. However, their use as cardioprotective agents in chemotherapy-induced cardiomyopathy is still equivocal. With inflammation and oxidative stress playing a role in the development of cardiotoxicity, statins’ anti-inflammatory and anti-oxidative properties have the potential to attenuate detrimental effects of chemotherapy on cardiomyocytes.
In cultured cardiomyocytes, pitavastatin attenuated doxorubicin-induced oxidative stress, DNA damage, and p53 accumulation and thus apoptosis [80]. In fact, fluvastatin-pretreated mice receiving doxorubicin, had higher cardiac outputs and lower LV pressures compared to non-statin treated mice. They also showed reduced cardiac expression of nitrotyrosine, enhanced expression of the mitochondrial located antioxidative SOD 2, attenuated mitochondrial apoptotic pathways, and diminished cardiac inflammatory response, thus reducing cardiac toxicity [81]. Iliskovic et al. reported complete prevention of adriamycin cardiotoxicity with probucol, a lipid reducing and antioxidant agent in rats, with improved glutathione peroxidase activity and reduced lipid peroxidation [82].
Similarly, Cheng et al. reported that pravastatin-pretreated mice receiving carbaplatin had decreased apoptosis, caspase 3, 9, and cyctochrome C activity, reactive oxygen species, with improved cardiac function and survival. This was achieved via Akt activation and restoration of normal mitochondrial HAX-1 in heart tissue, suggesting that pravastatin has cytoprotective effects in carboplatin-induced cardiotoxicity [83].
Small human studies have also been promising. In a retrospective observational study of patients with breast cancer who received anthracyclines, uninterrupted statin therapy reduced incident heart failure by 70 % compared with patients who did not receive statin [HR] of 0.3 (95 % confidence interval [CI]: 0.1 to 0.9; p = 0.03) [84].
In the only randomized clinical trial so far, Acar et al. randomized 40 patients receiving anthracycline-based chemotherapy to atorvastatin (40 mg/day) versus placebo and found that significant decreases in LVEF were only noted in the control group but not in the statin-group [85].
From these preliminary data, it appears that statins may have a cardioprotective role in the prevention of chemotherapy-induced cardiotoxicity through reduction of the oxidative stress. Because of the paucity of other available cardioprotective therapies, the authors recommend use of statins in patients at moderate to high risk of cardiotoxicity.
Beta-blockers
Cellular and animal studies suggest that beta-blockers may have protective activity against doxorubicin cardiotoxicity [86–88]. The suggested mechanism of cardioprotection is believed to be primarily through neurohormonal blockade [89], antioxidant effects [86], and inhibition of apoptosis [86].
To date, only a few studies have supported these effects in humans. Seicean et al. published a retrospective, database-derived study, reporting outcomes of 106 breast cancer patients who were on various beta-blockers while receiving anthracyclines or trastuzumab. Compared with propensity-matched controls, those on beta-blockers had a significant reduction in the risk for new HF events (HR 0.2, 95 % CI 0.1-0.5, p = 0.003) [90].
Kalay et al. randomized 50 patients treated with anthracycline therapy to carvedilol (12.5 mg daily) or placebo. After completion of therapy, LVEF was higher in patients receiving carvedilol (69.9 % vs. 52.3 %), and both systolic and diastolic diameters were significantly increased compared with basal measures in the control group [91].
The only randomized, blinded placebo controlled trial to date, OVERCOME (Enalapril and Carvedilol for Preventing Chemotherapy-Induced Left Ventricular Systolic Dysfunction in Patients With Malignant Hemopathies) has provided further validation for the cardioprotective role of beta-blockers and ACE-I. Ninety patients with acute leukemias or malignant hemopathies without left ventricular systolic dysfunction were randomized to receive carvedilol and enalapril or placebo. At 6 month follow-up, LVEF did not change in the intervention group, but decreased in controls (-3.1 %, p = 0.035) by echocardiography. More importantly, patients who received carvedilol/enalapril had lower incidence of death or heart failure (6.7 % vs. 22 %, p = 0.036) [92••].
There is evidence, that not all beta-blockers confer the same degree of cardioprotection. For example, in mice treated with anthracyclines, carvedilol but not atenolol was effective in reducing apoptosis [93]. Similarly, Georgakopoulos et al. reported a retrospective analysis of 42 patients treated for lymphoma with metoprolol versus placebo and were unable to demonstrate significant reduction in cardiotoxicity among the groups [94].
Based on these data, we currently consider carvedilol as the beta-blocker of choice for prevention of cardiotoxicity.
ACE-Inhibitors and Angiotensin Receptor Blockers
In addition to their pivotal role in HF [95, 96], angiotensin-converting enzyme inhibitors (ACE-I) appear to have cardioprotective properties against cardiotoxicity [97–99]. Through mechanisms other than attenuating remodeling and neurohormonal activation after an initial myocardial insult [100], ACE inhibition may prevent cardiotoxicity related to chemotherapy. Hiona el al. showed that enalapril protects against doxorubicin-induced LV dysfunction by preserving mitochondrial respiratory efficiency and reducing free radical generation [101].
In the largest study thus far, Cardinale et al. randomized 114 chemotherapy-treated patients with high troponins to received ACE-inhibitors or placebo, showing a 10 % reduction in LVEF and increase in end-diastolic and end-systolic volumes among the control but not the ACE-I group, with incidence of 43 % vs. 0 % (p < 0.001). These data suggest that ACE-I may prevent late cardiomyopathy in patients with biomarker evidence of myocardial damage from chemotherapy [102]. However, in a smaller study of 43 patients with lymphoma receiving enalapril or placebo, failed to show significant reduction in cardiac events [94].
Angiotensin receptor blockers (ARBs) may have similar cardioprotective properties as ACE-I. Among 40 lymphoma patients receiving CHOP, valsartan 80 mg/day versus placebo, those on valsartan had lower increases in BNP and more favorable diastolic parameters [103].
The use combination of beta-blocker (metoprolol) and angiotensin-receptor blockers (candesartan) in prevention of cardiotoxicity from anthracyclines and HER2-antagonists is underway in the PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy (PRADA) study [104].
Despite the absence of randomized clinical trials, current data supports the use of ACE-I and ARBs for prevention of chemotherapy-induced cardiotoxicity. We recommend their use in patients at risk for cardiotoxicity.
Dexrazoxane
As oxidative stress is the main driving event toward cardiomyocyte apoptosis, antioxidants may be beneficial in the prophylaxis against chemotherapy-induced cardiomyopathy.
Dexrazoxane is an EDTA-chelating agent that may decrease cardiotoxicity by binding iron that is implicated in the formation of ROS, and preventing mitochondrial dysfunction and thus apoptosis [105]. The use of dexrazoxane in cardioprotection, however, has been controversial.
In a meta-analysis of six RCTs, dexrazoxane given with anthracycline-based therapy reduced risk of clinical cardiotoxicity ([OR]:0.21; 95 % CI: 0.13- 0.33; p < 0.0001), subclinical cardiotoxicity ([RR]:0.33; 95 % CI: 0.20-0.55; p < 0.0001), and any cardiotoxic event (clinical and sub-clinical) ([RR]:0.34; 95 % CI: 0.27- 0.45; p < 0.0001) [106].
However, there is a concern that dexrazoxane may interfere with cancer response rate and be associated with an increase in secondary malignancies [107, 108]. The use of dexrazoxane was associated with increase in acute myeloid leukemia/myelodysplastic syndrome rate (2.55 % vs. 0.85 %) and secondary malignancy rate (3.43 % vs. 0.85 %) in children with Hodgkin’s lymphoma and lymphoblastic leukemia [109]. In a trial of patients with breast cancer, dexrazoxane was associated with decreased response rate to anthracycline therapy, however other trials did not confirm this finding [110, 111].
Given the conflicting data and the uncertainty of its effects, ASCO guidelines do not recommend the routine use of dexrazoxane in patients with initial dose anthracyclines [44]. However, patients with metastatic disease, history of more than 400 mg/kg/m2 of doxorubicin, and those whom continuous use of doxorubicin is recommended despite lower LVEF, may be good candidates for dexrazoxane therapy.
Other Therapies
Probucol is a lipid-lowering agent with antioxidant properties that can protect the myocardium from anthracycline by activation superoxidative dismutase and glutathione peroxidase in animals although its role in protection for anthracycline cardiotoxicity in human is not known [112].
In a meta-analysis [106] and Cochrane review [113] of cardioprotective agents in prevention of chemotherapy-induced cardiotoxicity, no conclusion was deducted on the effects of N-acetylcystine, amifostine, vitamin E, coenzyme Q10, phenethylamines, and L-carnitine.
Ascensão et al. showed that both short and long-term exercise can be protective from doxorubicin cardiotoxicity by up-regulation of antioxidant capacity and increased expression of heat shock protein (HSP) and other anti-apoptotic proteins through potentiating mitochondrial plasticity and adaptations to the toxic effect of doxorubicin [114].
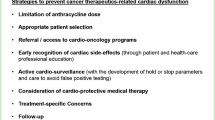
Recommended Approach to Risk Stratification, Chemoprevention and Surveillance of Cardiotoxicity
Risk Stratification and Chemoprevention for Patients Prior to Anthracycline Therapy
In our Institution, all patients whose anti- neoplastic treatment plan includes cardiotoxic therapy, or have underlying heart disease are referred to the Onco-Cardiology Program. Within it, patients are evaluated with the objective of stratifying cardiovascular risk and optimizing pre-existing cardiovascular disease. In addition to a detailed history, physical examination, electrocardiography and baseline b-type natriuretic peptide and troponin I, risk stratification includes e 3D echocardiography (3D LVEF) with strain imaging (average peak systolic global longitudinal strain) prior to starting chemotherapy. Pre-emptive medical therapy is then recommended based on the perceived risk (Fig. 2).
Surveillance of Patients on Anthracyclines
During monitoring, if there is a drop in EF, but it remains ≥ 50 % or there is a greater than 12 % decrement in GLS, patients are started on carvedilol with or without ACE inhibitors, statins and dexrazoxane (depending on discussions with the oncologists) and anthracyclines are continued. From then on, we repeat echocardiography with strain before each scheduled anthracycline cycle and obtain TNI at the end of each infusion. Conversely, if the EF decreases to less than 50 %, or there is development of clinical heart failure, anthracyclines are held, and appropriate guideline-directed medical HF therapy is initiated. If anthracyclines are required to continue, then an endomyocardial biopsy is done. If the biopsy shows a grade of <1.5, repeat echocardiograms are done monthly, and liposomal anthracyclines are started when EF is recovered, however with addition of dexrazoxane. If the biopsy shows a grade >1.5, anthracyclines are then permanently contraindicated, Fig. 3.
Risk Stratification and Chemoprevention for Patients on Trastuzumab and Other TKI’s
Patients planned to start trastuzumab or TKIs are also seen in the oncocardiology program before intiating treatment. History and physical exam, biomarkers, and 3D echocardiogram with GLS measurement are obtained. If patients have preserved EF (>50 %) and GLS of more than -18 % or have no cardiovascular risk factors and they are below age of 65 years old, no preemptive treatment is required and we repeat echocardiogram every 3 months while on treatment. If patients have reduced EF (<50 %) or GLS < -18 % or they have HF or age 65 years or older, we usually start them on carvedilol and statin, with or without ACE inhibitors. We then proceed with trastuzumab treatment, and repeat echo with serum biomarkers before each dose, Fig. 4.
Surveillance of Patients on Trastuzumab and Other TKI’s
A similar approach is taken for patients planned to receive trastuzumab (Fig. 4). Initial clinical assessment with echocardiogram is done prior to receiving trastuzumab, at one month and every 3 months while on the treatment. If repeat echocardiograms shows EF drop of 10 % or more, but still >50 %, or there is more than 12 % drop in GLS, carvedilol with or without ACE-inhibitors and statins are started, and monthly echocardiogram is required. If there is a drop in EF to less than 50 %, or there is clinical heart failure, we initiate guideline-directed medical therapy for heart failure, trastuzumab is held, and a monthly echocardiogram is indicated until EF recovers, at which time trastuzumab is resumed, Fig. 5.
Special Considerations in Other Chemotherapy Regimens
Patients who are started on TKIs are at high risk to develop hypertension. We usually pre-treat those patients with ACE-I, beta-blockers (e.g., Nebivolol), or calcium channel blockers (Nifedipine XL) to counteract the vasoconstriction in those patients as tolerated. Studies are required to validate this approach in prevention of hypertension in those patients.
Patients who receive 5-fluorouracil and capecitabine are at higher risk for coronary vasospasm. Although there is lack of evidence on this specific population, extrapolating data from idiopathic coronary vasospasm [115, 116], we recommend starting long-acting nifedipine and long acting nitrates on patients who develop angina while receiving 5-FU. In those who develop angina while on oral therapy, we admit them to the hospital and administer 5-FU in conjunction with intravenous nitrates and calcium channel blockers, such as nicardipine. Prophylactically, we recommend this regimen in patients without angina but with known coronary disease.
In all patients, we recommend statins for primary/secondary prevention of cardiovascular disease following the 2013 AHA/ACC guidelines on cholesterol treatment [117].
Conclusions
Compelling rationale and tentative evidence exist to support preventive medical interventions in cancer patients receiving potentially cardiotoxic chemotherapy. As better mechanistic understanding and stronger clinical data accrue, strategies to prevent cardiotoxicity will become more effective, hopefully rendering cardiotoxicity an ailment of the past.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Horner MJRL, Krapcho M, Neyman N, Aminou R, Howlader N, et al. SEER cancer statistics review, 1975–2006. Bethesda (MD): National Cancer Institute; 2009.
Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13(3):R64. doi:10.1186/bcr2901.
Oliveira GH, Dupont M, Naftel D, Myers SL, Yuan Y, Tang WH, et al. Increased need for right ventricular support in patients with chemotherapy-induced cardiomyopathy undergoing mechanical circulatory support: outcomes from the INTERMACS Registry (Interagency Registry for Mechanically Assisted Circulatory Support). J Am Coll Cardiol. 2014;63(3):240–8. doi:10.1016/j.jacc.2013.09.040. This study of patients undergoing mechanical support for cardiomyopathy provided novel insights into right ventricular failure in patients with chemotherapy-induced cardiomyopathy.
Oliveira GH, Hardaway BW, Kucheryavaya AY, Stehlik J, Edwards LB, Taylor DO. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2012;31(8):805–10. doi:10.1016/j.healun.2012.03.018.
Oliveira GH, Mukerji S, Hernandez AV, Qattan MY, Banchs J, Durand JB, et al. Incidence, predictors, and impact on survival of left ventricular systolic dysfunction and recovery in advanced cancer patients. Am J Cardiol. 2014;113(11):1893–8. doi:10.1016/j.amjcard.2014.03.018. This study provides insights into the natural course of chemotherapy induced LV dysfunction, with analysis of potential predictors.
Lenihan DJ, Cardinale D, Cipolla CM. The compelling need for a cardiology and oncology partnership and the birth of the International CardiOncology Society. Prog Cardiovasc Dis. 2010;53(2):88–93. doi:10.1016/j.pcad.2010.06.002.
Yeh ET. Onco-cardiology: the time has come. Tex Heart Inst J / from the Texas Heart Institute of St Luke's Episcopal Hospital, Texas Children's Hospital. 2011;38(3):246–7.
Chen J, Long JB, Hurria A, Owusu C, Steingart RM, Gross CP. Incidence of heart failure or cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Coll Cardiol. 2012;60(24):2504–12. doi:10.1016/j.jacc.2012.07.068.
Von Hoff DD, Layard MW, Basa P, Davis Jr HL, Von Hoff AL, Rozencweig M, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91(5):710–7.
Rakar S, Sinagra G, Di Lenarda A, Poletti A, Bussani R, Silvestri F, et al. Epidemiology of dilated cardiomyopathy. A prospective post-mortem study of 5252 necropsies. The Heart Muscle Disease Study Group. Eur Heart J. 1997;18(1):117–23.
Felker GM, Thompson RE, Hare JM, Hruban RH, Clemetson DE, Howard DL, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342(15):1077–84. doi:10.1056/NEJM200004133421502.
Singal PK, Iliskovic N. Doxorubicin-induced cardiomyopathy. N Engl J Med. 1998;339(13):900–5. doi:10.1056/NEJM199809243391307.
Wouters KA, Kremer LC, Miller TL, Herman EH, Lipshultz SE. Protecting against anthracycline-induced myocardial damage: a review of the most promising strategies. Br J Haematol. 2005;131(5):561–78. doi:10.1111/j.1365-2141.2005.05759.x.
Kremer LC, van Dalen EC, Offringa M, Ottenkamp J, Voute PA. Anthracycline-induced clinical heart failure in a cohort of 607 children: long-term follow-up study. J Clin Oncol Off J Am Soc Clin Oncol. 2001;19(1):191–6.
Colucci WS, Kolias TJ, Adams KF, Armstrong WF, Ghali JK, Gottlieb SS, et al. Metoprolol reverses left ventricular remodeling in patients with asymptomatic systolic dysfunction: the REversal of VEntricular Remodeling with Toprol-XL (REVERT) trial. Circulation. 2007;116(1):49–56. doi:10.1161/CIRCULATIONAHA.106.666016.
Daubert C, Gold MR, Abraham WT, Ghio S, Hassager C, Goode G, et al. Prevention of disease progression by cardiac resynchronization therapy in patients with asymptomatic or mildly symptomatic left ventricular dysfunction: insights from the European cohort of the REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction) trial. J Am Coll Cardiol. 2009;54(20):1837–46. doi:10.1016/j.jacc.2009.08.011.
Khakoo AY, Liu PP, Force T, Lopez-Berestein G, Jones LW, Schneider J, et al. Cardiotoxicity due to cancer therapy. Tex Heart Inst J / from the Texas Heart Institute of St Luke's Episcopal Hospital, Texas Children's Hospital. 2011;38(3):253–6.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79. doi:10.1002/cncr.11407.
Hershman DL, McBride RB, Eisenberger A, Tsai WY, Grann VR, Jacobson JS. Doxorubicin, cardiac risk factors, and cardiac toxicity in elderly patients with diffuse B-cell non-Hodgkin's lymphoma. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(19):3159–65. doi:10.1200/JCO.2007.14.1242.
Pinder MC, Duan Z, Goodwin JS, Hortobagyi GN, Giordano SH. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25(25):3808–15. doi:10.1200/JCO.2006.10.4976.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92. doi:10.1056/NEJM200103153441101.
Keefe DL. Trastuzumab-associated cardiotoxicity. Cancer. 2002;95(7):1592–600. doi:10.1002/cncr.10854.
Ewer MS, Vooletich MT, Durand JB, Woods ML, Davis JR, Valero V, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol Off J Am Soc Clin Oncol. 2005;23(31):7820–6. doi:10.1200/JCO.2005.13.300.
Chavez-MacGregor M, Zhang N, Buchholz TA, Zhang Y, Niu J, Elting L, et al. Trastuzumab-related cardiotoxicity among older patients with breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(33):4222–8. doi:10.1200/JCO.2013.48.7884.
Seidman A, Hudis C, Pierri MK, Shak S, Paton V, Ashby M, et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol Off J Am Soc Clin Oncol. 2002;20(5):1215–21.
Halyard MY, Pisansky TM, Dueck AC, Suman V, Pierce L, Solin L, et al. Radiotherapy and adjuvant trastuzumab in operable breast cancer: tolerability and adverse event data from the NCCTG Phase III Trial N9831. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27(16):2638–44. doi:10.1200/JCO.2008.17.9549.
Serrano C, Cortes J, De Mattos-Arruda L, Bellet M, Gomez P, Saura C, et al. Trastuzumab-related cardiotoxicity in the elderly: a role for cardiovascular risk factors. Ann Oncol Off J Eur Soc Med Oncol / ESMO. 2012;23(4):897–902. doi:10.1093/annonc/mdr348.
Bonifazi M, Franchi M, Rossi M, Moja L, Zambelli A, Zambon A, et al. Trastuzumab-related cardiotoxicity in early breast cancer: a cohort study. Oncologist. 2013;18(7):795–801. doi:10.1634/theoncologist.2013-0065.
Chu TF, Rupnick MA, Kerkela R, Dallabrida SM, Zurakowski D, Nguyen L, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet. 2007;370(9604):2011–9. doi:10.1016/S0140-6736(07)61865-0.
Schmidinger M, Zielinski CC, Vogl UM, Bojic A, Bojic M, Schukro C, et al. Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(32):5204–12. doi:10.1200/JCO.2007.15.6331.
Khakoo AY, Kassiotis CM, Tannir N, Plana JC, Halushka M, Bickford C, et al. Heart failure associated with sunitinib malate: a multitargeted receptor tyrosine kinase inhibitor. Cancer. 2008;112(11):2500–8. doi:10.1002/cncr.23460.
Chen MH, Kerkela R, Force T. Mechanisms of cardiac dysfunction associated with tyrosine kinase inhibitor cancer therapeutics. Circulation. 2008;118(1):84–95. doi:10.1161/CIRCULATIONAHA.108.776831.
Hayman SR, Leung N, Grande JP, Garovic VD. VEGF inhibition, hypertension, and renal toxicity. Curr Oncol Rep. 2012;14(4):285–94. doi:10.1007/s11912-012-0242-z.
Tannir NM, Wong YN, Kollmannsberger CK, Ernstoff MS, Perry DJ, Appleman LJ, et al. Phase 2 trial of linifanib (ABT-869) in patients with advanced renal cell cancer after sunitinib failure. Eur J Cancer. 2011;47(18):2706–14. doi:10.1016/j.ejca.2011.09.002.
Kane RC, Farrell AT, Saber H, Tang S, Williams G, Jee JM, et al. Sorafenib for the treatment of advanced renal cell carcinoma. Clin Cancer Res Off J Am Assoc Cancer Res. 2006;12(24):7271–8. doi:10.1158/1078-0432.CCR-06-1249.
Francis J, Ahluwalia MS, Wetzler M, Wang E, Paplham P, Smiley S, et al. Reversible cardiotoxicity with tyrosine kinase inhibitors. Clin Adv Hematol Oncol H&O. 2010;8(2):128–32.
Meydan N, Kundak I, Yavuzsen T, Oztop I, Barutca S, Yilmaz U, et al. Cardiotoxicity of de Gramont's regimen: incidence, clinical characteristics and long-term follow-up. Jpn J Clin Oncol. 2005;35(5):265–70. doi:10.1093/jjco/hyi071.
Sorrentino MF, Kim J, Foderaro AE, Truesdell AG. 5-fluorouracil induced cardiotoxicity: review of the literature. Cardiol J. 2012;19(5):453–8.
Mosseri M, Fingert HJ, Varticovski L, Chokshi S, Isner JM. In vitro evidence that myocardial ischemia resulting from 5-fluorouracil chemotherapy is due to protein kinase C-mediated vasoconstriction of vascular smooth muscle. Cancer Res. 1993;53(13):3028–33.
Labianca R, Beretta G, Clerici M, Fraschini P, Luporini G. Cardiac toxicity of 5-fluorouracil: a study on 1083 patients. Tumori. 1982;68(6):505–10.
Oleksowicz L, Bruckner HW. Prophylaxis of 5-fluorouracil-induced coronary vasospasm with calcium channel blockers. Am J Med. 1988;85(5):750–1.
Jensen SA, Sorensen JB. Risk factors and prevention of cardiotoxicity induced by 5-fluorouracil or capecitabine. Cancer Chemother Pharmacol. 2006;58(4):487–93. doi:10.1007/s00280-005-0178-1.
Akpek G, Hartshorn KL. Failure of oral nitrate and calcium channel blocker therapy to prevent 5-fluorouracil-related myocardial ischemia: a case report. Cancer Chemother Pharmacol. 1999;43(2):157–61. doi:10.1007/s002800050877.
Hensley ML, Hagerty KL, Kewalramani T, Green DM, Meropol NJ, Wasserman TH, et al. American Society of Clinical Oncology 2008 clinical practice guideline update: use of chemotherapy and radiation therapy protectants. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27(1):127–45. doi:10.1200/JCO.2008.17.2627.
van Royen N, Jaffe CC, Krumholz HM, Johnson KM, Lynch PJ, Natale D, et al. Comparison and reproducibility of visual echocardiographic and quantitative radionuclide left ventricular ejection fractions. Am J Cardiol. 1996;77(10):843–50.
Nousiainen T, Vanninen E, Jantunen E, Puustinen J, Remes J, Rantala A, et al. Comparison of echocardiography and radionuclide ventriculography in the follow-up of left ventricular systolic function in adult lymphoma patients during doxorubicin therapy. J Intern Med. 2001;249(4):297–303.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2005;18(12):1440–63. doi:10.1016/j.echo.2005.10.005.
Nousiainen T, Jantunen E, Vanninen E, Hartikainen J. Early decline in left ventricular ejection fraction predicts doxorubicin cardiotoxicity in lymphoma patients. Br J Cancer. 2002;86(11):1697–700. doi:10.1038/sj.bjc.6600346.
Gopal AS, Shen Z, Sapin PM, Keller AM, Schnellbaecher MJ, Leibowitz DW, et al. Assessment of cardiac function by three-dimensional echocardiography compared with conventional noninvasive methods. Circulation. 1995;92(4):842–53.
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popovic ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013;61(1):77–84. doi:10.1016/j.jacc.2012.09.035.
Walker J, Bhullar N, Fallah-Rad N, Lytwyn M, Golian M, Fang T, et al. Role of three-dimensional echocardiography in breast cancer: comparison with two-dimensional echocardiography, multiple-gated acquisition scans, and cardiac magnetic resonance imaging. J Clin Oncol Off J Am Soc Clin Oncol. 2010;28(21):3429–36. doi:10.1200/JCO.2009.26.7294.
Abraham TP, Dimaano VL, Liang HY. Role of tissue Doppler and strain echocardiography in current clinical practice. Circulation. 2007;116(22):2597–609. doi:10.1161/CIRCULATIONAHA.106.647172.
Dandel M, Lehmkuhl H, Knosalla C, Suramelashvili N, Hetzer R. Strain and strain rate imaging by echocardiography - basic concepts and clinical applicability. Curr Cardiol Rev. 2009;5(2):133–48. doi:10.2174/157340309788166642.
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy - a systematic review. J Am Coll Cardiol. 2014. doi:10.1016/j.jacc.2014.01.073. This study provides a systematic analysis of the use of strain imaging in detection and monitoring of chemotherapy-induced cardiotoxicity.
Neilan TG, Jassal DS, Perez-Sanz TM, Raher MJ, Pradhan AD, Buys ES, et al. Tissue Doppler imaging predicts left ventricular dysfunction and mortality in a murine model of cardiac injury. Eur Heart J. 2006;27(15):1868–75. doi:10.1093/eurheartj/ehl013.
Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Cohen V, et al. Early detection and prediction of cardiotoxicity in chemotherapy-treated patients. Am J Cardiol. 2011;107(9):1375–80. doi:10.1016/j.amjcard.2011.01.006.
Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Tan TC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging. 2012;5(5):596–603. doi:10.1161/CIRCIMAGING.112.973321.
Negishi K, Negishi T, Hare JL, Haluska BA, Plana JC, Marwick TH. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2013;26(5):493–8. doi:10.1016/j.echo.2013.02.008.
Mornos C, Petrescu L. Early detection of anthracycline-mediated cardiotoxicity: the value of considering both global longitudinal left ventricular strain and twist. Can J Physiol Pharmacol. 2013;91(8):601–7. doi:10.1139/cjpp-2012-0398.
Herman EH, Zhang J, Lipshultz SE, Rifai N, Chadwick D, Takeda K, et al. Correlation between serum levels of cardiac troponin-T and the severity of the chronic cardiomyopathy induced by doxorubicin. J Clin Oncol Off J Am Soc Clin Oncol. 1999;17(7):2237–43.
Sparano JA, Wolff AC, Brown D. Troponins for predicting cardiotoxicity from cancer therapy. Lancet. 2000;356(9246):1947–8. doi:10.1016/S0140-6736(00)03304-3.
Cardinale D, Sandri MT, Colombo A, Colombo N, Boeri M, Lamantia G, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109(22):2749–54. doi:10.1161/01.CIR.0000130926.51766.CC.
Auner HW, Tinchon C, Linkesch W, Tiran A, Quehenberger F, Link H, et al. Prolonged monitoring of troponin T for the detection of anthracycline cardiotoxicity in adults with hematological malignancies. Ann Hematol. 2003;82(4):218–22. doi:10.1007/s00277-003-0615-3.
Cardinale D, Sandri MT, Martinoni A, Tricca A, Civelli M, Lamantia G, et al. Left ventricular dysfunction predicted by early troponin I release after high-dose chemotherapy. J Am Coll Cardiol. 2000;36(2):517–22.
Koseoglu V, Berberoglu S, Karademir S, Kismet E, Yurttutan N, Demirkaya E, et al. Cardiac troponin I: is it a marker to detect cardiotoxicity in children treated with doxorubicin? Turk J Pediatr. 2005;47(1):17–22.
Mathew P, Suarez W, Kip K, Bayar E, Jasty R, Matloub Y, et al. Is there a potential role for serum cardiac troponin I as a marker for myocardial dysfunction in pediatric patients receiving anthracycline-based therapy? A pilot study. Cancer Investig. 2001;19(4):352–9.
Morris PG, Chen C, Steingart R, Fleisher M, Lin N, Moy B, et al. Troponin I and C-reactive protein are commonly detected in patients with breast cancer treated with dose-dense chemotherapy incorporating trastuzumab and lapatinib. Clin Cancer Res Off J Am Assoc Cancer Res. 2011;17(10):3490–9. doi:10.1158/1078-0432.CCR-10-1359.
Ky B, Putt M, Sawaya H, French B, Januzzi Jr JL, Sebag IA, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in patients with breast cancer treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol. 2014;63(8):809–16. doi:10.1016/j.jacc.2013.10.061.
Chen S, Garami M, Gardner DG. Doxorubicin selectively inhibits brain versus atrial natriuretic peptide gene expression in cultured neonatal rat myocytes. Hypertension. 1999;34(6):1223–31.
Lenihan DJMM, Baysinger K, Steinert D, Fayad L, Yusuf SW, Chiu A, et al. Early detection of cardiotoxicity during chemotherapy using biomarkers. J Clin Oncol. 2007;25(18S):19521.
Skovgaard D, Hasbak P, Kjaer A. BNP predicts chemotherapy-related cardiotoxicity and death: comparison with gated equilibrium radionuclide ventriculography. PLoS One. 2014;9(5):e96736. doi:10.1371/journal.pone.0096736.
From AM, Maleszewski JJ, Rihal CS. Current status of endomyocardial biopsy. Mayo Clin Proc. 2011;86(11):1095–102. doi:10.4065/mcp.2011.0296.
Han J, Park Y, Lee H, Kang H, Kim H, Yang DH, et al. Complications of 2-D echocardiography guided transfemoral right ventricular endomyocardial biopsy. J Korean Med Sci. 2006;21(6):989–94.
Sloan KP, Bruce CJ, Oh JK, Rihal CS. Complications of echocardiography-guided endomyocardial biopsy. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2009;22(3):324.e1–4. doi:10.1016/j.echo.2008.12.023.
Cooper Jr LT. Role of left ventricular biopsy in the management of heart disease. Circulation. 2013;128(14):1492–4. doi:10.1161/CIRCULATIONAHA.113.005395.
Meinardi MT, van der Graaf WT, van Veldhuisen DJ, Gietema JA, de Vries EG, Sleijfer DT. Detection of anthracycline-induced cardiotoxicity. Cancer Treat Rev. 1999;25(4):237–47. doi:10.1053/ctrv.1999.0128.
Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. J Am Coll Cardiol. 2007;50(19):1914–31. doi:10.1016/j.jacc.2007.09.008.
Kalam K, Marwick TH. Role of cardioprotective therapy for prevention of cardiotoxicity with chemotherapy: a systematic review and meta-analysis. Eur J Cancer. 2013;49(13):2900–9. doi:10.1016/j.ejca.2013.04.030. This study provides a metaanalysis of cardioprotective agents in cardioprotection of chemotherapycardiotoxicity.
Brugts JJ, Yetgin T, Hoeks SE, Gotto AM, Shepherd J, Westendorp RG, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ. 2009;338:b2376. doi:10.1136/bmj.b2376.
Yoshida M, Shiojima I, Ikeda H, Komuro I. Chronic doxorubicin cardiotoxicity is mediated by oxidative DNA damage-ATM-p53-apoptosis pathway and attenuated by pitavastatin through the inhibition of Rac1 activity. J Mol Cell Cardiol. 2009;47(5):698–705. doi:10.1016/j.yjmcc.2009.07.024.
Riad A, Bien S, Westermann D, Becher PM, Loya K, Landmesser U, et al. Pretreatment with statin attenuates the cardiotoxicity of Doxorubicin in mice. Cancer Res. 2009;69(2):695–9. doi:10.1158/0008-5472.CAN-08-3076.
Iliskovic N, Singal PK. Lipid lowering: an important factor in preventing adriamycin-induced heart failure. Am J Pathol. 1997;150(2):727–34.
Cheng CF, Juan SH, Chen JJ, Chao YC, Chen HH, Lian WS, et al. Pravastatin attenuates carboplatin-induced cardiotoxicity via inhibition of oxidative stress associated apoptosis. Apoptosis Int J Program Cell Death. 2008;13(7):883–94. doi:10.1007/s10495-008-0214-9.
Seicean S, Seicean A, Plana JC, Budd GT, Marwick TH. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J Am Coll Cardiol. 2012;60(23):2384–90. doi:10.1016/j.jacc.2012.07.067.
Acar Z, Kale A, Turgut M, Demircan S, Durna K, Demir S, et al. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2011;58(9):988–9. doi:10.1016/j.jacc.2011.05.025.
Spallarossa P, Garibaldi S, Altieri P, Fabbi P, Manca V, Nasti S, et al. Carvedilol prevents doxorubicin-induced free radical release and apoptosis in cardiomyocytes in vitro. J Mol Cell Cardiol. 2004;37(4):837–46. doi:10.1016/j.yjmcc.2004.05.024.
de Nigris F, Rienzo M, Schiano C, Fiorito C, Casamassimi A, Napoli C. Prominent cardioprotective effects of third generation beta blocker nebivolol against anthracycline-induced cardiotoxicity using the model of isolated perfused rat heart. Eur J Cancer. 2008;44(3):334–40. doi:10.1016/j.ejca.2007.12.010.
Matsui H, Morishima I, Numaguchi Y, Toki Y, Okumura K, Hayakawa T. Protective effects of carvedilol against doxorubicin-induced cardiomyopathy in rats. Life Sci. 1999;65(12):1265–74.
Fujita N, Hiroe M, Ohta Y, Horie T, Hosoda S. Chronic effects of metoprolol on myocardial beta-adrenergic receptors in doxorubicin-induced cardiac damage in rats. J Cardiovasc Pharmacol. 1991;17(4):656–61.
Seicean S, Seicean A, Alan N, Plana JC, Budd GT, Marwick TH. Cardioprotective effect of beta-adrenoceptor blockade in patients with breast cancer undergoing chemotherapy: follow-up study of heart failure. Circ Heart Fail. 2013;6(3):420–6. doi:10.1161/CIRCHEARTFAILURE.112.000055.
Kalay N, Basar E, Ozdogru I, Er O, Cetinkaya Y, Dogan A, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006;48(11):2258–62. doi:10.1016/j.jacc.2006.07.052.
Bosch X, Rovira M, Sitges M, Domenech A, Ortiz-Perez JT, de Caralt TM, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies). J Am Coll Cardiol. 2013;61(23):2355–62. doi:10.1016/j.jacc.2013.02.072. This is the first big-scale randomized controlled trial that provided insight into prophylaxis of chemotherapy-induced cardiotoxicity with ACE inhibitors and carvedilol.
Oliveira PJ, Bjork JA, Santos MS, Leino RL, Froberg MK, Moreno AJ, et al. Carvedilol-mediated antioxidant protection against doxorubicin-induced cardiac mitochondrial toxicity. Toxicol Appl Pharmacol. 2004;200(2):159–68. doi:10.1016/j.taap.2004.04.005.
Georgakopoulos P, Roussou P, Matsakas E, Karavidas A, Anagnostopoulos N, Marinakis T, et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin-treated lymphoma patients: a prospective, parallel-group, randomized, controlled study with 36-month follow-up. Am J Hematol. 2010;85(11):894–6. doi:10.1002/ajh.21840.
Gorkin L, Norvell NK, Rosen RC, Charles E, Shumaker SA, McIntyre KM, et al. Assessment of quality of life as observed from the baseline data of the Studies of Left Ventricular Dysfunction (SOLVD) trial quality-of-life substudy. Am J Cardiol. 1993;71(12):1069–73.
Rutherford JD, Pfeffer MA, Moye LA, Davis BR, Flaker GC, Kowey PR, et al. Effects of captopril on ischemic events after myocardial infarction. Results of the survival and ventricular enlargement trial. SAVE Investigators. Circulation. 1994;90(4):1731–8.
Sacco G, Bigioni M, Evangelista S, Goso C, Manzini S, Maggi CA. Cardioprotective effects of zofenopril, a new angiotensin-converting enzyme inhibitor, on doxorubicin-induced cardiotoxicity in the rat. Eur J Pharmacol. 2001;414(1):71–8.
Tokudome T, Mizushige K, Noma T, Manabe K, Murakami K, Tsuji T, et al. Prevention of doxorubicin (adriamycin)-induced cardiomyopathy by simultaneous administration of angiotensin-converting enzyme inhibitor assessed by acoustic densitometry. J Cardiovasc Pharmacol. 2000;36(3):361–8.
Ibrahim MA, Ashour OM, Ibrahim YF, El-Bitar HI, Gomaa W, Abdel-Rahim SR. Angiotensin-converting enzyme inhibition and angiotensin AT(1)-receptor antagonism equally improve doxorubicin-induced cardiotoxicity and nephrotoxicity. Pharmacol Res Off J Ital Pharmacol Soc. 2009;60(5):373–81. doi:10.1016/j.phrs.2009.05.007.
Cohn JN. Structural basis for heart failure. Ventricular remodeling and its pharmacological inhibition. Circulation. 1995;91(10):2504–7.
Hiona A, Lee AS, Nagendran J, Xie X, Connolly AJ, Robbins RC, et al. Pretreatment with angiotensin-converting enzyme inhibitor improves doxorubicin-induced cardiomyopathy via preservation of mitochondrial function. J Thorac Cardiovasc Surg. 2011;142(2):396–403.e3. doi:10.1016/j.jtcvs.2010.07.097.
Cardinale D, Colombo A, Sandri MT, Lamantia G, Colombo N, Civelli M, et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006;114(23):2474–81. doi:10.1161/CIRCULATIONAHA.106.635144.
Nakamae H, Tsumura K, Terada Y, Nakane T, Nakamae M, Ohta K, et al. Notable effects of angiotensin II receptor blocker, valsartan, on acute cardiotoxic changes after standard chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone. Cancer. 2005;104(11):2492–8. doi:10.1002/cncr.21478.
Heck SL, Gulati G, Ree AH, Schulz-Menger J, Gravdehaug B, Rosjo H, et al. Rationale and design of the prevention of cardiac dysfunction during an Adjuvant Breast Cancer Therapy (PRADA) Trial. Cardiology. 2012;123(4):240–7. doi:10.1159/000343622.
Seifert CF, Nesser ME, Thompson DF. Dexrazoxane in the prevention of doxorubicin-induced cardiotoxicity. Ann Pharmacother. 1994;28(9):1063–72.
Smith LA, Cornelius VR, Plummer CJ, Levitt G, Verrill M, Canney P, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer. 2010;10:337. doi:10.1186/1471-2407-10-337.
Seymour L, Bramwell V, Moran LA. Use of dexrazoxane as a cardioprotectant in patients receiving doxorubicin or epirubicin chemotherapy for the treatment of cancer. The Provincial Systemic Treatment Disease Site Group. Cancer Prev Control: CPC = Prevention Control Cancerologie: PCC. 1999;3(2):145–59.
Swain SM. Adult multicenter trials using dexrazoxane to protect against cardiac toxicity. Semin Oncol. 1998;25(4 Suppl 10):43–7.
Tebbi CK, London WB, Friedman D, Villaluna D, De Alarcon PA, Constine LS, et al. Dexrazoxane-associated risk for acute myeloid leukemia/myelodysplastic syndrome and other secondary malignancies in pediatric Hodgkin's disease. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25(5):493–500. doi:10.1200/JCO.2005.02.3879.
Lopez M, Vici P, Di Lauro K, Conti F, Paoletti G, Ferraironi A, et al. Randomized prospective clinical trial of high-dose epirubicin and dexrazoxane in patients with advanced breast cancer and soft tissue sarcomas. J Clin Oncol Off J Am Soc Clin Oncol. 1998;16(1):86–92.
Venturini M, Michelotti A, Del Mastro L, Gallo L, Carnino F, Garrone O, et al. Multicenter randomized controlled clinical trial to evaluate cardioprotection of dexrazoxane versus no cardioprotection in women receiving epirubicin chemotherapy for advanced breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 1996;14(12):3112–20.
Walker JR, Sharma A, Lytwyn M, Bohonis S, Thliveris J, Singal PK, et al. The cardioprotective role of probucol against anthracycline and trastuzumab-mediated cardiotoxicity. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2011;24(6):699–705. doi:10.1016/j.echo.2011.01.018.
van Dalen EC, Caron HN, Dickinson HO, Kremer LC. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev. 2008;2, CD003917. doi:10.1002/14651858.CD003917.pub3.
Ascensao A, Ferreira R, Magalhaes J. Exercise-induced cardioprotection–biochemical, morphological and functional evidence in whole tissue and isolated mitochondria. Int J Cardiol. 2007;117(1):16–30. doi:10.1016/j.ijcard.2006.04.076.
Freedman SB, Richmond DR, Kelly DT. Long-term follow-up of verapamil and nitrate treatment for coronary artery spasm. Am J Cardiol. 1982;50(4):711–5.
Antman E, Muller J, Goldberg S, MacAlpin R, Rubenfire M, Tabatznik B, et al. Nifedipine therapy for coronary-artery spasm. Experience in 127 patients. N Engl J Med. 1980;302(23):1269–73.
Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013. doi:10.1161/01.cir.0000437738.63853.7a.
Compliance with Ethics Guidelines
Conflict of Interest
Guilherme H. Oliveira, Marwan Qattan, Sadeer Al-Kindi and Ahmad Younes have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sadeer Al-Kindi and Ahmad Younes contributed to this work equally.
This article is part of the Topical Collection on Heart Failure Prevention
Rights and permissions
About this article
Cite this article
Al-Kindi, S., Younes, A., Qattan, M. et al. Preemptive Cardioprotective Strategies in Patients Receiving Chemotherapy. Curr Cardiovasc Risk Rep 8, 406 (2014). https://doi.org/10.1007/s12170-014-0406-5
Published:
DOI: https://doi.org/10.1007/s12170-014-0406-5