Abstract
Advances in oncologic therapies have led to considerable improvements in prognosis and survival. However, these improvements may ultimately be diminished by the increase of cardiovascular side effects. Typically, both conventional and new antitumoral therapies may induce asymptomatic or symptomatic left ventricular dysfunction. Its development still remains a major deterrent that may compromise clinical effectiveness of cancer treatment, independently of the oncologic prognosis, having a serious impact on the patient’s survival and quality of life. Hence, prevention of cardiotoxicity remains a crucial topic both for cardiologists and oncologists. Many strategies to mitigate the risk of cardiotoxicity have been developed, including cardiac function monitoring, limitation of chemotherapy doses, use of anthracycline analogues and cardioprotectants, and early detection of cardiotoxicity by biomarkers, followed by prophylactic intervention in selected high risk patients. We reviewed the currently available approaches which have been demonstrated to be effective in preventing or limiting cancer drug-induced cardiotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer therapy, which today can rely on a combination of traditional chemotherapeutic drugs, novel targeted drugs, radiation therapy, and more radical surgery techniques, has led to a considerable improvement in patient survival [1, 2•]. Cardiotoxicity, however, still remains a major limitation of many anticancer agents that can compromise their clinical benefits, independently of the oncologic prognosis and affect the patient’s survival and quality of life [1, 2•]. At present, the problem of cancer therapy-related cardiovascular diseases is rising, due to the increasing number of long-term cancer survivors, the frequent use of anthracyclines still in use today, new antitumor agents with potential cardiotoxic effects, as well as treatments combinations with synergistic harmful effects [2•, 3]. It is estimated that there are more than 14 million cancer survivors in the US, and this number is expected to reach 19 million by 2024 [1]; the risk of cardiovascular death in this population may exceed that of tumor recurrence for many forms of cancer [1, 2•, 3, 4]. Therefore, the prevention of cardiotoxicity has become a crucial goal presently for both cardiologist and oncologist, and the cooperation between these two areas is an actual need, which led to the development of a novel medical discipline, named cardioncology. Its aim is to investigate innovative strategies, collect evidence-based indications, and develop interdisciplinary expertise which will be able to manage this growing category of patients, guarantee correct clinical administration, and provide the best therapeutic opportunities, particularly in terms of impact on both cardiological and oncological prognosis.
The spectrum of abnormalities that can impair the cardiovascular system after cancer therapy includes acute coronary syndromes, hypertension, arrhythmias, and thromboembolic events. However, the most frequent, and feared manifestation of cardiotoxicity is the development of left ventricular dysfunction (LVD) [2•]. Even when asymptomatic, LVD not only negatively influences patients’ cardiac outcome, but it also seriously limits their therapeutic opportunities when adjunctive oncologic therapy for cancer relapse or persistence is required. In the past, cardiotoxicity was nearly always associated with anthracyclines. However, many novel oncologic drugs may interfere with intracellular mechanisms that are crucial to maintain normal cardiac cell homeostasis, leading to relatively high incidences of subclinical and overt cardiotoxicity (Table 1) [2•, 5, 6••]. In particular, the recognition of cardiotoxicity induced by trastuzumab, which belongs to the class of monoclonal antibodies against human epidermal receptor-2 (HER2), introduced some years ago to treat breast cancer, has been a paradigmatic example, revealing the potential for unexpected cardiotoxic effects of new anticancer agents [7, 8].
The best treatment of cancer drug-induced LVD is prevention of the disorder in the first instance. Accordingly, several preventive strategies to reduce the risk of cardiotoxicity have been proposed in the cardioncology setting. Cardiotoxicity prevention may be primary prevention, extended to all patients scheduled for potential cardiotoxic therapy, or could be performed in selected high-risk patients, showing preclinical signs of cardiotoxicity, or belatedly in patients showing initial LVD, in order to promptly start a treatment against progression to overt HF (Fig. 1).
Schematic representation of the possible strategies for cancer drug-induced cardiotoxicity detection, prevention, and treatment. AC=anthracycline; ACEI=angiotensin-converting enzyme inhibitors; BB=beta-blockers; CV=cardiovascular; GLS=global longitudinal strain; HF=heart failure; LVD=left ventricular dysfunction; RAS=renin-angiotensin system
Primary Prevention of Cardiotoxicity
Prevention of cardiotoxicity begins before starting anti-cancer therapy, with the cardiologist and oncologist working together. The evaluation of the cardiovascular profile by the cardiologist should be considered by the oncologists when selecting the best therapeutic approach for each individual patient, in terms of drug choice and schedule of administration.
Control/Correction of Pre-existing Cardiovascular Risk Factors
The presence of cardiovascular risk factors may increase the risk of cardiotoxicity [2•, 9, 10]. Cardiovascular risk factor reduction with appropriate control of blood pressure, cholesterol, and blood glucose, as well as smoking cessation are suggested in all patients for primary prevention of cardiotoxicity [11, 12].
Reduction of Cardiotoxic Direct Effect
Limiting Anthracycline Cumulative Dose
According to findings that indicate a rapid increase in cardiotoxicity at high doses [4, 5, 13], current oncologic guidelines suggest limiting the maximal cumulative dose of anthracycline to 450-550 mg/m2 [14]. This, however, can compromise the clinical success of the treatment. In addition, great variability exists in the dose of anthracyclines tolerated by patients; thus, some patients may show LVD at standard doses, whereas others may tolerate a cumulative dose twofold higher than the conventional dose limitation [13].
Altering Anthracycline Administration
Administering anthracyclines via continuous infusion rather than as a bolus dose, has been proposed to limit peak dose levels and reduce cardiac side effects. Accordingly, prolonged anthracycline infusion schedules have been shown to be associated with a lower incidence of cardiotoxicity, when compared to bolus therapy [13]. However, this remains a controversial issue. If, on one hand, continuous infusion limits peak anthracyclines levels, on the other, it prolongs the patient’s exposure to the drug’s toxic effects. Experimentally, a longer exposure time has been shown to counteract functional recovery of the cardiomyocytes damaged by anthracyclines [13, 15].
Using Less Cardiotoxic Anthracycline Analogues
In the attempt to create drugs as effective as conventional anthracyclines, but with a lower risk of inducing cardiotoxicity, various novel anthracycline analogues have been developed over the past years. Epirubicin, idarubicin, and mitoxantrone have shown lower cardiotoxicity in some preclinical and clinical studies [13, 15]. Despite the fact that cardiotoxicity occurs at a higher cumulative dose of epirubicin than doxorubicin, epirubicin must be administered at higher doses than doxorubicin to obtain the same clinical response (epirubicin 90 mg/m2=doxorubicin 60 mg/m2) [13]. Idarubicin has also shown a lower cardiotoxic profile than doxorubicin in preclinical and animal studies; however, subsequent clinical studies have not confirmed these findings [13, 15]. Conflicting data also exist for mitoxantrone, an anthracenedione derivative of doxorubicin [2•, 13, 15].
Using Liposomal Anthracycline Formulations
Liposomal anthracyclines were developed to reduce the cardiotoxicity of doxorubicin while preserving its antitumor efficacy. Liposomes have several advantages over non-capsulated drugs [16]: first, improved pharmacokinetics and drug release; second, enhanced cellular penetration through different mechanisms, such as fusion of the liposomal membrane with the cellular plasma membrane; third, the possibility of selectively targeting anticancer drugs directly to the tumor, preventing side effects to healthy tissues [16]. Liposomes cannot escape the vascular space where capillaries have tight junctions, found in the heart and the gastrointestinal tract. The tendency to accumulate in myocardial cells is reduced, lowering cardiotoxicity. Conversely, they exit the circulatory system in areas where capillaries are disrupted by tumor growth, resulting in high concentrations directly at tumor sites [15, 16]. Currently, several liposomal anticancer drugs for the treatment of Kaposi’s sarcoma, ovarian cancer, breast cancer, and hematological malignancies are available or are in advanced stages of clinical development [16].
Pharmacologic Prevention
Adding Cardioprotectants to Chemotherapy
In the cardioncology setting, there is great interest in using cardioprotectant agents for abating the cardiotoxicity of antineoplastic drugs, and this seems to be a promising alternative to changing or even stopping treatment.
The hypothesis that chelation of iron could reduce anthracycline-induced cardiotoxicity suggests that dexrazoxane could be an important, specific, and clinically useful cardioprotective agent against anthracyclines [17]. Other iron chelators, such as deferasirox or ICRF-161, however, did not provide these effects [15]. It has been shown that dexrazoxane has additional mechanisms that might explain its cardioprotective action. Besides iron chelation, dexrazoxane is a catalytic inhibitor of DNA topoisomerase II (Top2). Top2ß was recently indicated as the key mediator of anthracycline-induced cardiotoxicity [15]. Doxorubicin is a strong inhibitor of Top2, and causes the trapping of the enzyme on DNA as a covalent complex. Lyu et al. [18] demonstrated that dexrazoxane changes Top2’s configuration to a closed-clamp form through tight binding to Top2’s ATP-binding sites, which prevents anthracycline from binding to the Top2 complex. Dexrazoxane significantly reduces anthracycline-related cardiotoxicity in adults with varied solid tumors and in children with acute lymphoblastic leukemia and Ewing’s sarcoma [19]. There is strong evidence that patients who were treated with dexrazoxane had a lower incidence of HF compared to those who were not. Despite these consistently positive findings, the use of dexrazoxane has not been widely adopted and is recommended as a cardioprotectant only in patients with metastatic breast cancer who have already received >300 mg/m2 of doxorubicin [20]. Suspicion of interference with the efficacy of anthracyclines, and the occurrence of secondary malignancies, in addition to its possible myelosuppressor effect might explain this [19]. In a recent meta-analysis of ten studies enrolling over 1600 patients, however, patients treated with dexrazoxane in conjunction with anthracyclines had about 1/3 lower risk of HF compared to patients given anthracyclines without dexrazoxane, with similar response rate and survival. Moreover, no significant difference in the occurrence of secondary malignancies was identified. Therefore, if cardiotoxicity risk is expected to be high, using dexrazoxane in patients treated with anthracycline seems to be justified [19].
Other cardioprotective agents such as coenzyme Q10, carnitine, N-acetylcysteine, antioxidant vitamins E and C, erythropoietin, endothelin-1 receptor antagonist bosentan, lipid-lowering agent probucol, iron-chelating agents such as desferoxamine and EDTA have been investigated in animal models and small clinical studies. Preliminary evidence shows that these agents may have cardioprotective effects, but their utility in preventing anthracycline-induced cardiotoxicity requires further investigation [13, 19].
Adding Cardiovascular Agents to Chemotherapy (Table 2)
The cardioprotective effect of carvedilol was first demonstrated in animals and in-vitro studies [13, 21]. The first clinical study in an adult population was a randomized, placebo-controlled trial in which carvedilol prevented LVD in a small number of patients treated with anthracyclines [21]. In patients co-administered carvedilol together with anthracyclines, left ventricular ejection fraction (LVEF) did not change during the 6-month follow-up, but decreased in the control group (69% vs. 52%; p<0.001), which also had higher mortality.
Exactly why carvedilol has a protective effect is not clear. However, it seems due to its antioxidant activity, rather than its ß-blocking action [22]. A study comparing carvedilol to atenolol, a β1 selective antagonist without antioxidant properties, showed that carvedilol prevented mitochondrial damage and reduced the histopathologic changes associated with doxorubicin cardiotoxicity as opposed to atenolol [16]. Furthermore, in some tumor cells, carvedilol increased the cytotoxicity of doxorubicin by reversing tumor multi-drug resistance via inhibition of the efflux protein p-glycoprotein. Thus, carvedilol seems to be very effective as a cardioprotective agent without impairing the antineoplastic activity of anthracyclines [22].
The protective effect against anthracycline-induced cardiotoxicity of nebivolol, a ß1 selective antagonist with NO-dependent vasodilatory properties, has been demonstrated in a small randomized trial [23]. In 27 patients with breast cancer, nebivolol was initiated 7 days before anthracycline-based chemotherapy and continued for 6 months. In these patients, LVEF and N-terminal pro-brain natriuretic peptide (NT-proBNP) remained unchanged after 6 months; in the placebo group (n=18) however, a significant decrease in LVEF was observed along with an increase in NT-proBNP.
In a recent retrospective study by Seicean et al. [24] including 106 breast cancer patients, the continuous use of beta-blockers during cancer treatment, which included anthracyclines, trastuzumab, or anthracyclines followed by trastuzumab, was associated with a decreased incidence of HF over a 5-year period. The authors, however, did not match their results according to chemotherapy type or the many types of beta-blockers utilized in their study population [22]. Several preclinical studies show that not all β-blockers are equally effective: some data suggest that β1 selective antagonists, rather than non-selective β-blockers, might offer better protection against anthracycline-induced cardiotoxicity. However, analysis of cancer registry data suggests that β2 limits breast cancer–specific mortality but β1 does not [22]. Therefore, their net effect in preventing cancer therapy-related cardiotoxicity remains unclear. While carvedilol and nebivolol seem beneficial, non-selective β-blockers such as propranolol are possibly cardiotoxic, and the effect of metoprolol appears neutral [25, 26].
Experimental data imply that the cardiac renin-angiotensin system (RAS) could play a significant role in the development and progression of anthracycline-induced cardiotoxicity [6••, 27], highlighting the possible beneficial effects of angiotensin-converting enzyme inhibitors (ACEI) [27]. Treatment with lisinopril, when initiated after the termination of chemotherapy, significantly inhibited cardiac ACE activity and improved mortality, cardiac remodelling and LVD in hamsters [28]. In a canine model of doxorubicin-induced cardiomyopathy, enalapril treatment blunted LVEF decrease and reduced mortality by 64% [29]. The authors attributed the effect to the direct scavenging action of enalapril on the free radical production induced by doxorubicin, because increased oxidative stress has been suggested as a possible primary cause in the development of anthracycline-induced cardiotoxicity. Enalapril, however, does not include the sulfhydryl group, required for the optimal free radical scavenging, in its structure [30]. Other studies, have found that ACEI, both including and excluding the sulfhydryl group are effective against anthracycline-induced cardiotoxicity. Abd El-Aziz et al. [30] compared captopril, containing a sulfhydryl group, and enalapril that does not in male rats; both drugs created similar protection against adriamycin-induced cardiotoxicity, suggesting that their protective effect may be exerted by mechanisms other than the anti-oxidant effect [27–29].
Nakamae et al. [31] conducted a randomized trial, showing valsartan, an angiotensin II receptor blocker (ARB), when given at the same time as anthracycline-containing chemotherapy, prevents increase in atrial natriuretic peptide and brain natriuretic peptide, acute increase in left ventricular diastolic diameter, and prolongation and dispersion in QTc interval, in a small population. Since no significant change was observed in blood pressure or heart rate between the valsartan and control groups, the authors hypothesize that the beneficial effects of valsartan on acute cardiotoxicity could not be mediated by its hemodynamic effects, but by the direct inhibition of angiotensin II receptors, supporting previous findings in animal models demonstrating a key role of the local RAS in doxorubicin-induced cardiotoxicity [27–29].
Telmisartan, another ARB, was studied in a randomized trial including 49 patients free of cardiovascular diseases and treated with epirubicin for a variety of solid cancers [32]. Twenty-five patients started telmisartan 1 week before epirubicin and showed no relevant diminution in myocardial deformation parameters (peak strain rate) as revealed by tissue Doppler echocardiography, nor any significant increase in reactive oxygen species or in interleukin-6, after 18 months of follow-up, as found in 24 patients receiving only epirubicin. The authors assumed that the beneficial effect of telmisartan is affected not only by RAS blockade, but also by its anti-inflammatory and anti-oxidant properties.
The results of the PRADA (Prevention of Cardiac Dysfunction during Adjuvant Breast Cancer Therapy) trial have very recently demonstrated that candesartan—but not metoprolol—concomitantly administrated with adjuvant chemotherapy including epirubicin, with or without trastuzumab, can protect against early decline in LVEF, assessed with cardiac magnetic resonance [33].
The use of perindopril versus bisoprolol in patients with HER2+ breast cancer undergoing treatment with trastuzumab in the prevention of LVD has been investigated in the MANTICORE-101 (Multidisciplinary Approach to Novel Therapies in Cardiology Oncology Research). At the end of trastuzumab therapy, neither drug had an impact on left ventricular end-diastolic volume (primary outcome of change from baseline in the study). In univariate analysis only bisoprolol was associated with preservation of baseline function (from 62% to 61%) (secondary outcome). However, in multivariate analysis, use of both cardiac drugs significantly predicted preserved LV function (for perindopril, P = 0.013; for bisoprolol, P < 0.001) [34].
Aldosterone antagonism has very recently been evaluated in a trial including 83 patients randomized to receive spironolactone, or not, and concomitant anthracycline-containing chemotherapy [35]. Three weeks after the end of chemotherapy, spironolactone had prevented a decrease in LVEF, blunted the increase in troponin I and NT-proBNP, and also preserved diastolic function.
The preventive efficacy of a combination of enalapril and carvedilol was recently tested in the OVERCOME (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies) trial, including anthracycline-treated patients [36]. Subjects were randomized to enalapril plus carvedilol (n=45) or the control group (n=45). After 6 months, LVEF did not change in the intervention group but significantly decreased in controls (P=0.035). When compared with controls, the intervention group showed a lower rate of the combined event of death or HF (6.7% vs. 22%; P=0.036), or of death, HF and a final LVEF <45% (7% vs. 24%; P=0.02).
Statins’ potential role in the prevention of anthracycline induced-cardiotoxicity comes from their pleiotropic effects, particularly their anti-oxidative properties [5]. Riad et al. [37] showed that pre-treatment utilizing fluvastatin is cardioprotective against doxorubicin in mice, decreasing oxidative stress, enhancing expression of anti-oxidative enzyme mitochondrial superoxide-dismutase2, reducing cardiac inflammation and cytokine release. Very recently, Henninger et al. [38] demonstrated that lovastatin prevented decrease in fractional shortening and in LVEF in doxorubicin-treated mice. In the clinical setting, the only trial available is by Acar et al. [39] Forty patients—all without pre-existing cardiovascular abnormalities—were randomized into statin or control groups. The statin group received 40 mg/day of atorvastatin before chemotherapy, regardless of baseline lipid values, and therapy was continued for 6 months. In the statin group decrease in high-sensitivity C-reactive protein levels was observed without difference in LVEF from baseline to final value (61±8% vs. 63±9%; p=0.144). Conversely, LVEF decrease in the control group was significant (63±7% vs. 55±9%; p<0.0001).
In a retrospective observational study of 67 anthracycline-treated breast cancer patients who had already received statins for other indications, uninterrupted statin use was associated with a notable reduction of HF risk and cardiac-related mortality over 2.2±1.7 years of follow-up, versus the 134 propensity-matched controls (HR 0.3, CI 95%.0.1-0.9; p=0.03) [40]. More recently, Chotenimitkhun et al. [41] published a prospective observational study showing persons already receiving statin therapy for prevention of cardiovascular disease experienced less reduction in LVEF at 6 months after anthracycline-containing chemotherapy, than those not receiving statins. Additional, larger studies are needed to confirm the promising role of statins as cardioprotective agents.
Detection of Preclinical Cardiotoxicity and LVD Prevention
Role of Biomarkers
Early identification of patients at high risk of cardiotoxicity by cardiac biomarkers—in particular troponin—provides a rationale for targeted preventive strategies against cancer therapy-induced LVD and its associated clinical complications, with the advantage of limiting prophylactic therapy only to a restricted number of patients. We can speculate that cardioprotective therapies that limit or prevent an increase in cardiac biomarkers after chemotherapy, as well as cardiac treatments that interfere with their persistence, could improve cardiac prognosis of these patients [42, 43••].
The usefulness of troponin I for the selection of patients requiring prophylactic therapy was investigated in a randomized, controlled trial in which the cardioprotective effect of enalapril was evaluated [27]. In 58 out of 114 patients with early troponin I positivity after high-dose chemotherapy, enalapril was initiated 1 month after the completion of chemotherapy, titrated as tolerated, and continued for 1 year. None of the treated patients developed LVD vs. 43% of Controls, during the follow-up period. Moreover, a significantly lower incidence of adverse cardiac events was observed in enalapril treated patients. These findings confirm that cardiotoxicity can effectively be prevented by such an approach, and that this prophylactic strategy can be easily and safely applied in daily clinical practice in selected high-risk patients.
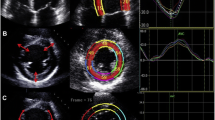
Role of Myocardial Deformation Parameters
Several small studies evaluating tissue Doppler and strain rate imaging detected early subclinical changes in cardiac function during and after chemotherapy that preceded a decrease in LVEF [44]. By using tissue Doppler-based strain imaging, peak systolic longitudinal strain rate has reliably recognized most early myocardial variations during anticancer therapy, whereas with speckle tracking echocardiography (STE), peak systolic global longitudinal strain (GLS) would appear to be the most accurate measure. A 10 to 15% early decrease in GLS by STE during therapy seems to be the most useful parameter for the prediction of cardiotoxicity, defined as a drop in LVEF or HF. An ongoing randomized trial (www.clinicaltrials.gov NCT02177175) is assessing the use of carvedilol for the prevention of anthracycline/trastuzumab-associated cardiotoxicity among women with HER2-positive breast cancer using myocardial strain for early risk stratification. In this trial carvedilol is started in women showing an absolute decrease in GLS below 19% or in case of a decrease ≥11% from baseline.
Detection OF LVD and Prevention of Symptomatic Heart Failure
Close Monitoring of Cardiac Function
For patients receiving potentially cardiotoxic anticancer therapy, the international cardiologic guidelines recommend routine periodic assessment of LVEF [45, 46]. However, most methods utilized in clinical practice (echocardiography, radionuclide-angiocardiography, etc.), have low sensitivity and poor predictive value [47, 48]. This is largely because no considerable change in LVEF occurs until a critical amount of myocardial damage has taken place. Therefore, the diagnosis of cardiotoxicity by the decrease in LVEF precludes, by definition, any chance of prevention. In addition, the measurement of LVEF presents a number of challenges related to image quality, assumption of left ventricular geometry, load dependency, and expertise [47, 48].
In a recent prospective study involving a large population treated with anthracycline, close monitoring of LVEF by echocardiography, during the first 12 months after the completion of chemotherapy, allowed early detection of almost all (98%) cases of cardiotoxicity, and prompt treatment with enalapril and carvedilol, or bisoprolol, which led to normalization of LVEF in 82% of cases. However, only 11% of patients had a full recovery (a LVEF equal to that before chemotherapy initiation); in the remaining 89% of patients, LVEF resulted below the baseline value [49].
Guidelines for monitoring patients receiving trastuzumab are specifically focused on the continuation/withdrawal/resumption of trastuzumab according to LVEF value assessed during administration [14, 50, 51]. No evidence-based recommendations for the treatment of patients developing LVD during and after trastuzumab therapy have been formulated thus far. To date, the evidence supporting the use of ACEI and beta-blockers in this setting is limited to case series. However, follow-up data from the largest trials show that, in many patients treated with anthracyclines and, subsequently, with trastuzumab, LVD does not recover, that up to 2/3 of patients continue to receive cardiac medications after complete functional recovery, and that many patients show LVEF lower than that at baseline, despite optimal HF therapy [52]. This evidence suggests that strategies aimed at preventing the development of LVD appear strategically more effective than interventions aimed at counteracting extant LVD, which can be progressive and irreversible in many cases.
Future Directions
Ongoing Studies
Further studies are ongoing to evaluate cardiovascular drugs as cardioprotectant agents. The ICOS-ONE trial (International CardiOncology Society; NCT01968200) [2•] is a randomized trial designed to compare the use of enalapril concomitantly with anthracycline-containing chemotherapy vs. enalapril administration after preclinical cardiotoxicity detection, revealed by the increase in troponins.
The SAFE (Cardiotoxicity Prevention in Breast Cancer Patients Treated with Anthracycline and/or Trastuzumab) trial is assessing whether the use of ramipril or bisoprolol, or their combination can prevent the development of HF in women receiving neoadjuvant or adjuvant anthracycline-containing chemotherapy, with or without trastuzumab.
In NCT01708798, the potential ability of the aldosterone antagonist, eplerenone, to prevent doxorubicin-induced cardiotoxicity, will be explored in a randomized controlled trial of breast cancer patients [2•].
To our knowledge, studies focused on prevention of LVD in patients treated with anticancer therapy different from anthracyclines, taxanes, trastuzumab or their combination are still lacking. To investigate preventive pharmacologic strategies also in populations treated with novel anticancer drugs, which have demonstrated unexpectedly high incidence of LVD, is a current need in the field of cardioncology, besides being a stimulating incentive.
Cardiac Progenitor Cells
In a future perspective, cardiac progenitor cells may find a role in the prevention and treatment of anthracycline-induced cardiotoxicity, possibly promoting cardiac repair. Autologous cardiac progenitor cells can be obtained prior to antineoplastic drug administration and subsequently given to those individuals particularly predisposed to cardiotoxicity [53–56].
Exercise
Positive health-promoting behavior, including lifestyle factors (healthy diet, smoking cessation, regular exercise, weight control) should be strongly advised by both cardiologists and oncologists. In particular aerobic exercise is considered a promising non-pharmacological strategy to prevent and or treat chemotherapy-induced cardiotoxicity.
Mainly, walking and cycling activities, also associated with strength exercises have been tested, and the benefit is greater when the exercises are more intense but not up until exhaustion, which should be strongly discouraged. Patients receiving cancer treatment often have multiple physical and psychological adverse effects. A multidisciplinary approach is essential for long-term management of cancer patients. A review of 56 trials including 4826 participants showed an improvement in quality of life and physical ability during and after the exercise training program [57].
Exercise training could reduce cardiotoxicity after anthracycline therapy. Aerobic exercise has been shown to mediate doxorubicin-induced cardiotoxicity in animal models, supposing mechanisms including decreased ROS formation, reduced expression of pro-apoptotic signaling, preservation of cardiomyocyte proliferation, improved calcium handling, and triggering the AMP-activated-protein-kinase pathway, which results in improved myocardial energetics [58, 59].
It has been shown that exercise can be effective in abating chemotherapy-induced cardiotoxicity risk in breast cancer survivors [6••, 60]. Ninety breast cancer patients receiving doxorubicin-cyclophosphamide were randomized to receive doxorubicin-cyclophosphamide alone or in combination with supervised endurance exercise training (cycle ergometry, 60 min/3 times/week at 60% of baseline VO2 peak), for 12 weeks. Doxorubicin-cyclophosphamide-induced increase in atrial natriuretic peptide was attenuated by exercise training [61]. Exercise has been shown to decrease all-cause mortality in the oncologic patient population [5]. Studies to define the effect of exercise on cardiotoxicity in this population are warranted; some of these trials are ongoing (NCT01943695) [6••].
Conclusions
Cancer therapy-induced cardiotoxicity still remains a serious problem, strongly affecting both quality of life and overall survival of cancer patients. Several strategies for preventing cardiotoxicity have been developed to minimize cardiac-related mortality and morbidity. There is encouraging evidence that prevention of cardiotoxicity is achievable, but it requires a multidisciplinary approach and a close collaboration among oncologists and cardiologists. The most effective approach for minimizing cardiotoxicity is its early detection and prompt prophylactic treatment initiation. The use of troponins for identification of patients with subclinical cardiotoxicity and their treatment with ACEI, for prevention of LVD and cardiac events, seems to be an effective strategy against these complications. When this kind of approach is not feasible, a complete LVEF recovery and a parallel reduction of cardiac events may still be obtained, if LVD is detected early after the end of chemotherapy and treatment with ACEI and beta-blockers is promptly initiated [13]. However, the optimal approach to minimize cardiotoxicity, the best method for its early detection, and the more effective medical regimen to prevent it, are at present still an object of debate.
Cardioncology is a new medical and interdisciplinary field of growing interest, based on a comprehensive approach for the management of cardiovascular outcomes in patients undergoing anticancer therapy. Because of the scarcity of evidence-based indications and the urgent need for expertise in this area, cardioncology represents a novel, topical research and clinical discipline still largely unexplored. Involved clinicians and researchers have the formidable task of investigating this setting and charting new evidence-based guidelines. In particular, this represents a sizable challenge for both cardiologists and oncologists, which presents, at the same time, a stimulating incentive.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
DeSantis C, Lin C, Mariotto A, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–71.
Truong J, Yan AT, Cramarossa G, Chan KKW. Chemotherapy-induced cardiotoxicity: detection, prevention and management. Can J Cardiol. 2014;30:869–78. A complete overview on incidence, detection, prevention, management, and clinical importance of cardiotoxicity.
Lenihan D, Cardinale D. Late cardiac effects of cancer treatment. J Clin Oncol. 2012;30:3657–64.
Carver JRSC, Ng A, et al. American society of clinical oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008.
Yeh ETH, Bickford CL. Cardiovascular complications of cancer therapy. Incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53:2231–47.
Hahn VS, Lenihan DJ, Ky B. Cancer therapy-induced cardiotoxicity: basic mechanisms and potential cardioprotective therapies. J Am Heart Assoc. 2014;3, e000665. An excellent review focusing on basic and clinical data to support use of specific potential cardioprotective agents against cancer therapy-induced cardiotoxicity.
Ewer SM, Ewer MS. Cardiotoxicity profile of trastuzumab. Drug Saf. 2008;31:459–67.
Tocchetti CG, Ragone G, Coppola C, Rea D, Piscopo G, Scala S. Detection, monitoring, and management of trastuzumab-induced left ventricular dysfunction: an actual challenge. Eur J Heart Fail. 2012;14:130–7.
Lotrionte M, Biondi-Zoccai G, Abbate A, et al. Review and meta-analysis of incidence and clinical predictors of anthracycline cardiotoxicity. Am J Cardiol. 2013;112:1980–4.
Pinder MC, Duan Z, Goodwin JS, Hortobagyi GN, Giordano SH. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol. 2007;25:3808–15.
Albini A, Pennesi G, Donatelli F, Cammarota R, De Flora S, Noonan DM. Cardiotoxicity of anticancer drugs: the need for cardio-oncology and cardio-oncological prevention. J Natl Cancer Inst. 2010;102:14–25.
Lenihan DJ, Esteva FJ. Multidisciplinary strategy for managing cardiovascular risks when treating patients with early breast cancer. Oncologist. 2008;13:1224–34.
Wouters KA, Kremer LCM, Miller TL, Herman EH, Lipshultz SE. Br J Haematol. 2005;131:561–78.
Curigliano G, Cardinale D, Suter T, et al. ESMO guidelines working group. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO clinical practice guidelines. Ann Oncol. 2012;23:vii155–66. Available from: www.annonc.oxfordjournals.org .
Vejpongsa P, Yeh ET. Prevention of anthracycline-induced cardiotoxicity: challenges and opportunities. J Am Coll Cardiol. 2014;64:938–45.
Slingerland M, Guchelaar HJ, Gelderblom H. Liposomal drug formulations in cancer therapy: 15 years along the road. Drug Discov Today. 2012;17:160–6.
Nitiss K, Nitiss J. Twisting and ironing: doxorubicin cardiotoxicity by mitochondrial DNA damage. Clin Cancer Res. 2014;20:4737–9.
Lyu YL, Kerrigan JE, Lin CP, Azarova AM, Tsai YC, Ban Y, et al. Topoisomerase IIbeta mediated DNA double-strand breaks: implications in doxorubicin cardiotoxicity and prevention by dexrazoxane. Cancer Res. 2007;67:8839–46.
Van Dalen EC, Caron HN, Dickinson HO, Kremer LC. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev. 2011;CD003917.
FDA statement on Dexrazoxane. www.fda.gov/Drugs/DrugSafety/ucm263729.htm.
Kalay N, Basar E, Ozdogru I, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006;48:2258–62.
Nohria A. Beta-adrenergic blockade for anthracycline- and trastuzumab-induced cardiotoxicity. Is prevention better than cure? Circ Heart Fail. 2013;6:358–61.
Kaya MG, Ozkan M, Gunebakmaz O, et al. Protective effects of nebivolol against anthracycline-induced cardiomyopathy: a randomized control study. Int J Cardiol. 2013;167:2306–10.
Seicean S, Seicean A, Alan N, Plana JC, Budd GT, Marwick TH. Cardioprotective effect of β-adrenoceptor blockade in patients with breast cancer undergoing chemotherapy: follow-up study of heart failure. Circ Heart Fail. 2013;6:420–6.
Choe JY, Combs AB, Folkers K. Potentiation of the toxicity of adriamycin by propranolol. Research communications in chemical pathology and pharmacology. Res Commun Chem Pathol Pharmacol. 1978;21:577–80.
Georgakopoulos P, Matsakas E, Karavidas A, et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin-treated lymphoma patients: a prospective, parallel-group, randomized, controlled study with 36-month follow-up. Am J Hematol. 2010;85:894–6.
Cardinale D, Colombo A, Sandri MT, et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006;114:2474–81.
Okumura K, Jin D, Takai S, Miyazaki M. Beneficial effects of angiotensin-converting enzyme inhibition in adriamycin-induced cardiomyopathy in hamsters. Jpn J Pharmacol. 2002;88:183–8.
Vaynblat M, Shah HR, Bhaskaran D, et al. Simultaneous angiotensin converting enzyme inhibition moderates ventricular dysfunction caused by doxorubicin. Eur J Heart Fail. 2002;4:583–6.
Abd El-Aziz MA, Othman AI, Amer M, El-Missiry MA. Potential protective role of angiotensin-converting enzyme inhibitors captopril and enalapril against adriamycin-induced acute cardiac and hepatic toxicity in rats. J Appl Toxicol. 2001;21:469–73.
Nakamae H, Tsumura K, Terada Y, et al. Notable effects of angiotensin II receptor blocker, valsartan, on acute cardiotoxic changes after standard chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone. Cancer. 2005;104:2492–8.
Cadeddu C, Piras A, Mantovani G, et al. Protective effects of the angiotensin II receptor blocker telmisartan on epirubicin-induced inflammation, oxidative stress, and early ventricular impairment. Am Heart J. 2010;160:4871.e1–7.
Gulati G, Heck SL, Ree AH, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): primary results of a randomized, 2 × 2 factorial, placebo-controlled, double blind clinical trial. AHA 2015; abstract 2015-LBCT-20236-AHA.
Pituskin E, Mackey JR, Koshman S, et al. Prophylactic beta blockade preserves left ventricular ejection fraction in HER2-overexpressing breast cancer patients receiving trastuzumab: Primary results of the MANTICORE randomized controlled trial. SABCS 2015; abstract S1-05.
Akpek M, Ozdogru I, Sahin O, et al. Protective effects of spironolactone against anthracycline-induced cardiomyopathy. Eur J Heart Fail. 2015;17:81–9.
Bosch X, Rovira M, Sitges M, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies). J Am Coll Cardiol. 2013;61:2355–62.
Riad A, Bien S, Westermann D, et al. Pretreatment with statin attenuates the cardiotoxicity of doxorubicin in mice. Cancer Res. 2009;69:695–9.
Henninger C, Huelsenbeck S, Wenzel P, et al. Chronic heart damage following doxorubicin treatment is alleviated by lovastatin. Pharmacol Res. 2015;91:47–56.
Acar Z, Kale A, Turgut M, et al. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2011;58:988–9.
Seicean S, Seicean A, Plana JC, Budd GT, Marwick TH. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J Am Coll Cardiol. 2012;60:2384–90.
Chotenimitkhun R, D’Agostino Jr R, Lawrence JA, et al. Chronic statin administration may attenuate early anthracycline-associated declines in left ventricular ejection function. Can J Cardiol. 2015;31:302e–7a.
Cardinale D, Salvatici M, Sandri MT. Role of biomarkers in cardioncology. Clin Chem Lab Med. 2011;49:1937–48.
Christenson ES, James T, Agrawal V, Park BH. Use of biomarkers for the assessment of chemotherapy-induced cardiac toxicity. Clin Biochem. 2015;48:223–35. Excellent review on strength and weakness points for the use of various biomarkers in the detection of chemotherapy-induced cardiotoxicity.
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63:2751–68.
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG. Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1–90.
Eschenhagen T, Force T, Ewer MS, De Keulenaer GW, Suter TM, Anker SD. Cardiovascular side effects of cancer therapies: a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2011;13:1–10.
Cardinale D, Bacchiani G, Beggiato M, Colombo A, Cipolla CM. Strategies to prevent and treat cardiovascular risk in cancer patients. Semin Oncol. 2013;40:186–98.
Lenihan DJ, Oliva S, Chow EJ, Cardinale D. Cardiac toxicity in cancer survivors. Cancer. 2013;119:2131–42.
Cardinale D, Colombo A, Bacchiani G, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–8.
Sengupta PP, Northfelt DW, Gentile F, Zamorano JL, Khandheria BK. Trastuzumab-induced cardiotoxicity: heart failure at the crossroads. Mayo Clin Proc. 2008;83:197–203.
Martin M, Esteva FJ, Alba E, Khandheria B, Pérez-Isla L, Garcìa-Sàenz JA. Minimizing cardiotoxicity while optimizing treatment efficacy with trastuzumab: review and expert recommendations. Oncologist. 2009;14:1–11.
Telli ML, Hunt SA, Carlson RW, Guardino AE. Trastuzumab-related cardiotoxicity: calling into question the concept of reversibility. J Clin Oncol. 2007;25:3525–33.
De Angelis A, Piegari E, Cappetta D, et al. Anthracycline cardiomyopathy is mediated by depletion of the cardiac stem cell pool and is rescued by restoration of progenitor cell function. Circulation. 2010;121:276–92.
Sharp III TE, George JC. Stem cell therapy and breast cancer treatment: review of stem cell research a potential therapeutic impact against cardiotoxicities due to breast cancer treatment. Front Oncol. 2014;4:299.
Oliveira MS, Carvalho JL, De Angelis Campo AC, et al. Doxorubicin has in vivo toxicological effects on ex vivo cultured mesenchymal stem cells. Toxicol Lett. 2014;224:380–6.
De Angelis A, Piegari E, Cappetta D, et al. SIRT1 activation rescues doxorubicin-induced loss of functional competence of human cardiac progenitor cells. Int J Cardiol. 2015;189:30–44.
Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev. 2012;8, CD008465. doi:10.1002/14651858.
Ascensão A, Oliveira PJ, Magalhães J. Exercise as a beneficial adjunct therapy during doxorubicin treatment. Role of mitochondria in cardioprotection. Int J Cardiol. 2012;156:4–10.
Marques-Aleixo I, Santos-Alves E, Mariani D, et al. Physical exercise prior and during treatment reduces sub-chronic doxirubicin-induced mitochondrial toxicity and oxidative stress. Mitochondrion. 2015;20:22–33.
Scott JM, Khakoo A, Mackey JR, Haykowsky MJ, Douglas PS, Jones LW. Modulation of anthracycline-induced cardiotoxicity by aerobic exercise in breast cancer: current evidence and underlying mechanisms. Circulation. 2011;124:642–50.
Jones L, Dolinsky VW, Haykowsky MJ, et al. Effects of aerobic training to improve cardiovascular function and prevent cardiac remodeling after cytotoxic therapy in early breast cancer. AACR 2011; abstract 5024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Daniela Cardinale, Gina Biasillo, and Carlo Maria Cipolla declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cardio-Oncology
Rights and permissions
About this article
Cite this article
Cardinale, D., Biasillo, G. & Cipolla, C.M. Curing Cancer, Saving the Heart: A Challenge That Cardioncology Should Not Miss. Curr Cardiol Rep 18, 51 (2016). https://doi.org/10.1007/s11886-016-0731-z
Published:
DOI: https://doi.org/10.1007/s11886-016-0731-z