Abstract
Purpose
This study aimed to investigate the incidence of rim uptake (RU) or multifocal uptake (MU) by invasive breast cancers on a ring-type dedicated breast positron emission tomography (dbPET) scanner compared with whole-body PET (wbPET) scanner imaging and to correlate uptake patterns with pathological features and prognosis.
Methods
Between 2009 and 2011, 76 lesions in 74 patients with primary invasive breast cancers were included. Each patient underwent dbPET and wbPET scanning on the same day after administration of 18F-fluorodeoxyglucose (FDG). The images were evaluated to identify specific uptake patterns (RU and MU). Their association with pathological characteristics and prognosis was analyzed.
Results
On dbPET, RU and MU patterns were observed in 18 lesions (24%) and 28 lesions (37%), respectively. On wbPET, RU and MU patterns were observed in six lesions (8%) and 17 lesions (22%), respectively. Lesions with RU on dbPET were of higher grade than lesions without RU (P = 0.024) and a higher Ki-67 index (mean; 31% vs. 18%, P = 0.015). They tended to be triple-negative (33% vs. 12%, P = 0.046) and less likely to be luminal A subtype (17% vs. 47%, P = 0.020). On wbPET, however, no significant differences in these markers were seen between RU and non-RU. The MU pattern did not correlate with pathological characteristics in either scanner. Lesions with RU or MU were not significantly associated with disease-free survival.
Conclusions
DbPET can identify detailed FDG distribution patterns of breast cancer better than wbPET. Breast cancer with RU on dbPET was associated with higher grade and triple-negative subtype.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a heterogeneous disease which comprises of different biological characteristics and clinical outcomes. The Nottingham (Elston–Ellis) modification of the Scarff–Bloom–Richardson histopathological grading system, also known as the Nottingham Grading System (NGS), is commonly accepted as a powerful indicator of aggressiveness, useful for prognosis [1]. Gene expression profiling is another system linked to prognosis and treatment selection. It uses a simplified immunohistochemical classification using estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) oncogene expression and/or amplification [2]. Ki-67 [3] is a nuclear protein present in all proliferating cells and its index is used as a proliferation marker [4, 5]. The status of these markers can identify the four main intrinsic subtypes of breast cancer: luminal A, luminal B, HER2-enriched, and triple negative [6].
Positron emission tomography (PET) with 18F-fluorodeoxyglucose (FDG), often combined with computed tomography (PET/CT) has been widely used for the evaluation of breast cancer patients, for staging and assessment of treatment response [7]. The role in evaluating local breast lesions is limited in part due to the low spatial resolution.
Dedicated breast PET (dbPET) scanners have been developed to overcome the limitations of wbPET/CT (whole-body PET/CT). DbPET scanners are classified into two types: positron emission mammography (PEM) and ring-type dbPET [8]. The major advantages of dbPET include higher spatial resolution and improved geometric sensitivity compared to wbPET [9]. Those benefits enable us to evaluate the FDG distribution pattern of the primary tumor. The higher resolution of dbPET allows better identification of separate foci, and patterns of uptake such as rim uptake (RU), similar to contrast-enhanced MRI, compared with wbPET [10]. Some evidence indicates that a rim or ring-like distribution pattern is associated with poor prognosis in head and neck cancer and gastrointestinal stromal tumors [11, 12]. We hypothesized that such FDG distribution patterns on pretreatment dbPET scans could be useful for predicting outcome.
The aim of this study was to investigate the pathological features of invasive breast cancer showing RU or multifocal uptake (MU) by dbPET and wbPET scanners, and to assess for correlation between uptake patterns and the pathological features and prognosis.
Methods
Patients and lesion characteristics
Our institutional review board approved the study, and written informed consent was obtained from all patients. Between November 2009 and August 2011, consecutive 137 women who were known to have or suspected of having invasive breast carcinoma underwent conventional wbPET followed by dbPET. 63 patients were excluded, including patients who had history of breast cancer, or patients with distant metastases. For the purpose of morphological assessment of the uptake, we also excluded patients with their breast lesions completely or partly out of the FOV of the dbPET (Fig. 1). Therefore, 76 lesions in 74 women (2 patients with bilateral lesions) (age range 31–89 years, mean 54.6 years) with biopsy-proven primary invasive breast carcinoma, which were detectable in the dbPET scanner field of view (FOV), enrolled in this study. Characteristics of lesions evaluated by dbPET are summarized in Table 1. Follow-up data of these patients up to 31 July 2017 were searched using the electronic medical records of our hospital. They were regarded as recurrence-free if the record said “recurrence-free.” If recurrence/metastasis was described, or the date of recurrence/metastasis was identified, locations of metastasis and the outcome (alive or dead) were recorded.
Whole-body PET/CT scanning and dbPET scanning
Patients fasted for at least 4 h before the examination and their plasma glucose level was checked just before the administration of approximately 3.7 MBq/kg weight of 18F-fluorodeoxyglucose (18F-FDG). There were no patients with a plasma glucose level > 200 mg/dL in this population. Approximately 1 h later, conventional wbPET/CT scanning was performed using a combined PET/CT scanner (Discovery ST Elite, GE Healthcare, Waukesha, WI, USA), followed by breast scanning using a ring-type dbPET scanner (a prototype of Elmammo, Shimadzu Co., Kyoto, Japan) for 5 min for each breast. The mean time duration between 18F-FDG injection and start of dbPET scanning was 104.7 min.
WbPET images were attenuation-corrected using CT data, and reconstructed with a 3D ordered-subsets expectation–maximization algorithm called VUE Point Plus (14 subsets, 2 iterations, 128 × 128 matrix, a voxel size of 4.69 × 4.69 × 3.27 mm, and postfiltering at 5.14 mm FWHM).
The dbPET system has a full-ring, four-layer depth-of-interaction (DOI) detector, which consists of 36 detector modules arranged in a three-ring configuration with a diameter of 195 mm and length of 155.5 mm. The detectors were arranged in a circle horizontally for scanning in the prone position. The transaxial effective FOV was 180 mm in diameter. The spatial resolution measured with an 18F point was estimated to be < 2 mm FWHM in effective FOV. The sensitivity of the dbPET scanner measured with a 22Na point source was 11.2% [13]. DbPET images were reconstructed without postfiltering (β = 100) with 128 subsets, 1 iteration, no attenuation correction, and a voxel size of 0.78 × 0.78 × 0.78 mm.
Image analysis
The 18F-FDG wbPET/CT data and dbPET data were evaluated by two board-certified radiologists who specialize in breast imaging (R.S. and S.K.). PET images were evaluated on a workstation (Advantage Workstation ver. 4.4, GE Healthcare, Barrington, IL, USA) together with the CT images. DbPET images were analyzed on another workstation (Aquarius Net, TeraRecon, Tokyo, Japan). Readers were blinded to all clinical information and other radiological findings. We reviewed the images separately, and then assessed the reproducibility. RU and MU were assessed based on the following definition: the term “RU” was defined for lesions with a complete rim of uptake, so lesions with an incomplete rim were not classified as “RU.” The term “MU” was defined as two or more foci of uptake adjacent to each other (Fig. 2).
Schematic figure of distribution pattern: rim uptake (RU) and multifocal uptake (MU). Distribution patterns on wbPET and dbPET images were evaluated with the following definitions: rim uptake (RU) was defined as an uptake pattern consisting of a complete rim (left). Lesions with unclear rim or semi-round uptake were not classified as RU. Multifocal uptake (MU) was defined as two or more foci of uptake adjacent to each other (right)
Pathological analysis
All the tumors were histopathologically examined by core needle biopsy, vacuum-assisted breast biopsy, or excision. Pathological diagnoses were made by specialists in breast pathology. The pathologists were informed of clinical information, yet were blinded to the wb/dbPET findings. They were graded by the Modified Scarff–Bloom–Richardson (SBR) system and immunohistochemically by estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2) and Ki-67 index status. HER2 was classified negative for a score of 0 or 1 and positive for a score of 3. If the score was 2, we added double color in situ hybridization (DISH) analysis. Subanalysis was conducted for lesions undergoing surgery without neoadjuvant therapy and histopathologically assessed for the presence of central necrosis and fibrotic foci, both of which suggest aggressive tumors. Absolute value of the time interval between wb/dbPET scanning and pathological diagnoses was 14.35 days.
Statistical analysis
Per lesion analysis for association between distribution pattern (RU, MU) of the lesions and histological grade, clinicopathological subtype, and Ki-67 index were performed with the Mann–Whitney test, using JMP10 (SAS institute). A P value < 0.05 was regarded as statistically significant.
Interobserver variability were evaluated by Kappa statistics; Kappa values ≤ 0.20 indicate poor agreement between the two readers; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and > 0.80, almost perfect agreement [14]. If different assessments were assigned by the two readers, the findings were discussed to reach consensus.
To assess the impact of distribution patterns on patient’s outcome, survival data of these patients were analyzed by Kaplan–Meier analysis. The larger lesion was used for analysis for one patient with two invasive cancers in the contralateral breast. The survival analysis and Kappa statistics were calculated using STATA version 13 (STATA Corp., Texas, USA).
Results
All 76 lesions showed FDG uptake on both db and wb PET. Out of 76 lesions, 18 lesions (24%) demonstrated the RU pattern and 28 lesions (37%) demonstrated the MU pattern in dbPET, while 6 (7.9%) lesions and 17 (22%) lesions demonstrated the RU and MU pattern in wbPET, respectively. Three lesions (3.9%) demonstrated both RU and MU patterns on dbPET, while one lesion (1.3%) did on wbPET. On dbPET, both RU and MU patterns were identified more frequently than on wbPET (P = 0.002 and 0.002, respectively). Interobserver agreement was almost perfect with Kappa coefficients of 0.89 (dbPET) and 1.00 (wbPET) for the RU pattern, and 0.88 (dbPET) and 0.84 (wbPET) for MU pattern. Representative cases are shown in Figs. 3, 4 and 5.
Invasive carcinoma of left breast in 57-year-old female. Axial wbPET image of left breast shows homogeneous intense uptake, suggesting breast cancer (a), whereas axial dbPET image revealed rim uptake (RU) (b). Axial post-contrast MRI shows rim enhancement similar to the distribution pattern on dbPET image (c). Hematoxylin–Eosin stain of surgical specimen showed peripheral rim arrangement of breast cancer cells with central scar (d)
Invasive carcinoma of right breast in a 41-year-old female. Sagittal wbPET image of left breast shows homogeneous intense uptake, suggesting breast cancer (a). Sagittal dbPET image shows both RU and multiple uptake (MU) (b). Sagittal post-contrast MRI shows multifocal lesions including rim enhancement, corresponding to dbPET image (c). Fusion image of MRI and dbPET (multi-color) enables us to see the correlation of those images (d)
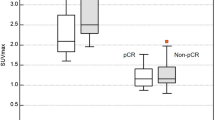
Lesions with RU in dbPET showed a histopathologically significant higher grade than lesions without RU (Modified SBR Grade 1, 2, 3: 11%, 50%, 39% vs. 22%, 66%, 12%, respectively; P = 0.024). They were significantly more likely to be triple negative (33% vs. 12%, P = 0.046) and less likely to be luminal A (17% vs. 47%, P = 0.02). In addition, the Ki67 index value was significantly higher in lesions with RU (mean value, 31% vs. 18%, P = 0.015) (Table 1). No significant differences in histopathology were seen between RU and non-RU in wbPET. The MU pattern did not affect the prevalence of higher grade, subtype, and Ki-67 for either scanner (Table 2).
Twenty-nine lesions which were surgically removed without PST were histologically assessed for the presence of central necrosis or fibrotic foci. Five lesions showed fibrotic foci, one lesion showed central necrosis, and one lesion showed both fibrotic foci and central necrosis. Six out of the seven lesions with central necrosis and/or fibrotic foci (86%) showed RU on both wb/db PET (n = 2) or dbPET (n = 4), while only one out of 22 lesions without necrosis and/or fibrotic foci showed RU on dbPET.
Follow-up data of 74 patients for ≥ 5 years were successfully retrieved from the electronic medical record of our hospital. During the follow-up period, six patients moved to other hospitals and one patient chose not to have treatment. The median follow-up period was 75 months, with 73% of patients with > 5-years follow-up. Recurrence occurred in 14 (19%) of 74 patients, including 8 patients who died. Bone was the most common initial recurrence site (n = 7), followed by lymph nodes (n = 4), lung (n = 3), skin (n = 2), liver (n = 1), pleura (n = 1), and local recurrence (n = 1) (There were three patients with two recurrences in a different location). Among these 14 patients with recurrence, three (36%) had had RU lesions and seven (50%) had had MU lesions on dbPET. A Kaplan–Meier curve of groups with RU/MU uptake on dbPET vs. those with disease-free survival showed crossing of the curves, making further analysis difficult (Fig. 6), suggesting that the RU/MU uptake pattern was not related to disease-free survival.
Kaplan–Meier curve of recurrence-free survival (RFS) for patients according to the status of (a) rim uptake (RU) and (b) multifocal uptake (MU) on dbPET. RU (+) indicates patients whose breast lesion showed RU, while RU (−) indicates patients whose breast lesion did not show RU on dbPET. Similarly, MU (+) represents those whose breast lesion showed MU, while RU (−) represents those whose breast lesion did not show MU. Both curves in RU and MU, curves of two groups cross over, indicating no significant difference in RFS between these groups with different distribution patterns
Discussion
We showed that dbPET scanner demonstrated RU and MU patterns of invasive breast cancer more frequently than wbPET, suggesting the potential of morphological assessment by high-resolution dbPET as a new approach of oncologic nuclear medicine. Another new finding was an association between RU pattern and aggressive features; higher histological grade, high Ki-67 index, and triple-negative subtype, which was observed only on dbPET.
In our study, we could detect incidences of RU on dbPET four times as often as those on wbPET. This can be explained by the high spatial resolution of dbPET of < 2.0 mm. There is increasing interest in the creation of dedicated breast PET, such as positron emission mammography (PEM) or dbPET, and those are now applied in the clinical setting. DbPET images are generated by prone positioning, avoiding the uncomfortable compression of mammography. DbPET images are comparable with breast MRI, and also enable us to obtain 3D images such as MRI [10, 14]. These strengths contribute to sensitive detection of morphology and intratumoral heterogeneity. Higher incidence of RU on dbPET might be related to the difference in scan timing; wbPET was performed at approximately 60 min, whereas dbPET was performed at approximately 105 min after the administration of FDG. Unfortunately, the current study was not designed to examine the changes in RU pattern over time. Further study is needed to determine the optimal scan timing to evaluate RU.
Our data showed that breast cancers with RU on dbPET tended to have aggressive pathological findings. The importance of morphological assessment in FDG-PET agree with other tumors in different locations. For example, Koyasu et al. assessed ring-shaped 18F-FDG uptake pattern qualitatively and suggested that ring-shaped uptake provides important prognostic information in head and neck squamous cell carcinoma [11], but this study was not analyzed quantitatively. Thereafter, Miyake et al. demonstrated the potential utility of ring-shaped 18F-FDG uptake in predicting the risk of postoperative recurrence for localized primary GIST [12]. These studies assessed the features of tumors morphologically, not quantitatively. RU in malignant tumors might be a common feature which suggests aggressiveness among various organs.
Recently Masumoto et al. [15] evaluated intratumoral heterogeneity among 195 patients with invasive breast cancer using dbPET and showed that intratumoral heterogeneous distribution was significantly related with high nuclear grade and high Ki-67 index. These relationships could not be found using wbPET, indicating the added value of dbPET in predicting pathological features. Although their definition of “intratumoral heterogeneous uptake” does not equal to “RU” in our series, it is plausible that both feature capture spatial heterogeneity of the breast cancer and its association with aggressive tumors.
Dynamic contrast-enhanced MR has proved useful in the evaluation of intratumoral morphology of breast cancer. However, MR imaging is contraindicated for patients with an implanted metal device or claustrophobia. Breast dynamic MRI cannot be performed for those who have allergy to contrast agent, or impaired renal function [16]. With dbPET, detailed intratumoral morphology can be obtained for those who do not fit for dynamic MRI. Rim on dbPET can be more obvious than rim enhancement on dynamic MRI (Fig. 5) due to the different distribution mechanism between 18F-FDG and gadrinium agents.
To describe morphological characteristics of the lesion, standardization of terminology will be an important issue for assessing the intratumoral heterogeneity, such as RU or MU. There is no consensus on how to define qualitative findings, but it can affect the result of analyses. Miyake et al. [12] defined “ring-shaped” uptake as round or semi-round uptake with an apparent central defect in evaluation of GIST. We used the term “RU” only for lesions with a complete rim, so we did not classify lesions with semi-round uptake as “RU.” There is significant overlap between the concept of “rim uptake” in PEM and our RU. In fact, “rim” is well known as a word describing enhancement on breast MRI. According to BI-RADS-MRI 2013, “rim enhancement” is defined as “enhancement is more pronounced at the periphery of the mass” [17]. The description did not clarify whether the “rim” should be a complete rim or not. Effort should be made to standardize terminology of RU and or MU on dbPET.
One possible explanation of RU’s association with aggressive tumor can be the presence of centrally necrotizing carcinoma (CNC)/fibrotic focus (FF). CNC is large, contiguous, central, and characterized by aggressive behavior and a poor prognosis [18], often associated with basal-like immunophenotype [19]. FF consists mainly of fibroblasts and collagen fibers, and can occupy almost the entire center of an invasive ductal carcinoma (IDC) [20]. IDCs with FF have more aggressive characteristics, significantly greater tumor angiogenesis and higher tumor cell proliferative activity than IDCs without FF. The presence of FF is an independent prognostic parameter for IDC patients [21]. Therefore, the association between RU and tumor aggressiveness may be pathologically explained by the proportions of CNC and FF. Other group comparing the distribution of FDG uptake on DbPET with pathological findings with HE staining also concluded that the defect of FDG uptake represented fibrosis or necrosis [15], which agrees with our hypothesis.
No significant relationships were found between the lesions with RU or MU and disease-free survival. This could be attributed to the improvement in systemic treatment, which lowered the recurrence rate in this study population. Patients with ER − and/or PR − disease are known to have higher risks of mortality compared to patients with ER − and/or PR + disease. However, the management of HER2-positive breast cancer has dramatically evolved, mainly because of widespread use of HER2-directed therapy, including monoclonal antibodies, small molecule inhibitors, and antibody drug conjugates [22]. The recent introduction of platinum agents as neoadjuvant chemotherapy in triple-negative breast cancers may also contribute to longer recurrence-free survival [23].
There are several limitations in this work. First, assessment of RU/MU is qualitative by observer and can be subjective, although the interobserver agreement in our study was almost perfect. Second, image quality was sometimes degraded by noise. Further improvement in image quality will be required to evaluate the detailed features in all FOVs. Third, the study population was small and facing various treatment options including surgery, neoadjuvant chemotherapy, and neoadjuvant hormonal therapy. That heterogeneity in management may lead to variations in prognostic value.
Conclusion
DbPET detected detailed distribution patterns of breast cancer more frequently than wbPET. Invasive breast cancer with RU on dbPET tended to show aggressive pathological features, but there was no long-term impact on survival.
References
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991;19:403–10.
Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–74.
Prat A, Perou CM. Deconstructing the molecular portraits of breast cancer. Mol Oncol. 2011;5:5–23.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, et al. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–47.
Romero Q, Bendahl PO, Klintman M, Loman N, Ingvar C, Rydén L, et al. Ki67 proliferation in core biopsies versus surgical samples—a model for neo-adjuvant breast cancer studies. BMC Cancer. 2011;11:341.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100:8418–23.
Groheux D, Espie M, Giacchetti S, Hindie E. Performance of FDG PET/CT in the clinical management of breast cancer. Radiology. 2013;266:388–405.
Bowen SL, Wu Y, Chaudhari AJ, Fu L, Packard NJ, Burkett GW, et al. Initial characterization of a dedicated breast PET/CT scanner during human imaging. J Nucl Med. 2009;50:1401–8.
Koolen BB, Vogel WV, Vrancken Peeters MJ, Loo CE, Rutgers EJ, Valdes Olmos RA. Molecular imaging in breast cancer: from whole-body PET/CT to dedicated breast PET. J Oncol. 2012;2012:438647.
Iima M, Nakamoto Y, Kanao S, Sugie T, Ueno T, Kawada M, et al. Clinical performance of two dedicated PET scanners for breast imaging: initial evaluation. J Nucl Med. 2012;53:1534–42.
Koyasu S, Nakamoto Y, Kikuchi M, Suzuki K, Hayashida K, Itoh K, et al. Prognostic value of pretreatment 18F-FDG PET/CT parameters including visual evaluation in patients with head and neck squamous cell carcinoma. AJR Am J Roentgenol. 2014;202:851–8.
Miyake KK, Nakamoto Y, Mikami Y, Tanaka S, Higashi T, Tadamura E, et al. The predictive value of preoperative (18)F-fluorodeoxyglucose PET for postoperative recurrence in patients with localized primary gastrointestinal stromal tumour. Eur Radiol. 2016;26:4664–74.
Miyake KK, Matsumoto K, Inoue M, Nakamoto Y, Kanao S, Oishi T, et al. Performance evaluation of a new dedicated breast PET scanner using NEMA NU4-2008 standards. J Nucl Med. 2014;55:1198–203.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Masumoto N, Kadoya T, Sasada S, Emi A, Arihiro K, Okada M. Intratumoral heterogeneity on dedicated breast positron emission tomography predicts malignancy grade of breast cancer. Breast Cancer Res Treat. 2018;171:315–23.
Broome DR. Nephrogenic systemic fibrosis associated with gadolinium based contrast agents: a summary of the medical literature reporting. Eur J Radiol. 2008;66(2):230–4.
Morris EA, Comstock CE, Lee CH, et al. ACR BI-RADS® magnetic resonance imaging. In: ACR BI-RADS® Atlas, breast imaging reporting and data system. Reston: American College of Radiology; 2013
Jimenez RE, Wallis T, Visscher DW. Centrally necrotizing carcinomas of the breast: a distinct histologic subtype with aggressive clinical behavior. Am J Surg Pathol. 2001;25:331–7.
Yu L, Yang W, Cai X, Shi D, Fan Y, Lu H. Centrally necrotizing carcinoma of the breast: clinicopathological analysis of 33 cases indicating its basal-like phenotype and poor prognosis. Histopathology. 2010;57:193–201.
Hasebe T, Tsuda H, Hirohashi S, Shimosato Y, Iwai M, Imoto S, et al. Fibrotic focus in invasive ductal carcinoma: an indicator of high tumor aggressiveness. Jpn J Cancer Res. 1996;87:385–94.
Van den Eynden GG, Colpaert CG, Couvelard A, Pezzella F, Dirix LY, Vermeulen PB, et al. A fibrotic focus is a prognostic factor and a surrogate marker for hypoxia and (lymph)angiogenesis in breast cancer: review of the literature and proposal on the criteria of evaluation. Histopathology. 2007;51:440–51.
Ahmed S, Sami A, Xiang J. HER2-directed therapy: current treatment options for HER2-positive breast cancer. Breast Cancer. 2015;22:101–16.
Petrelli F, Coinu A, Borgonovo K, Cabiddu M, Ghilardi M, Lonati V, et al. The value of platinum agents as neoadjuvant chemotherapy in triple-negative breast cancers: a systematic review and meta-analysis. Breast Cancer Res Treat. 2014;144:223–32.
Acknowledgements
The authors would like to thank Dr. Mami Iima from Department of Diagnostic Imaging and Nuclear Medicine of Kyoto University Graduate School of Medicine for the excellent and knowledgeable support. We also thank Dr. Libby Cone from Edanz Group (www.edanzediting.com) for editing a draft of this manuscript.
Funding
This work was supported by Shimadzu Co., Kyoto, Japan, and a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (C:22591329).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was supported by Shimadzu Co., Kyoto, Japan, and a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (C:22591329).
Rights and permissions
About this article
Cite this article
Sakaguchi, R., Kataoka, M., Kanao, S. et al. Distribution pattern of FDG uptake using ring-type dedicated breast PET in comparison to whole-body PET/CT scanning in invasive breast cancer. Ann Nucl Med 33, 570–578 (2019). https://doi.org/10.1007/s12149-019-01364-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-019-01364-7