Abstract
Objective
Neoadjuvant chemoradiotherapy (CMRT) is the most effective treatment of stage III non-small-cell lung cancer (NSCLC). The present study aimed at assessing FDG PET/CT for defining the response of N2 disease to neoadjuvant CMRT, as surgical resection after such therapy significantly improves 5-year survival in responding N2 disease.
Methods
Forty-five patients with locally advanced NSCLC underwent both pre-neoadjuvant therapy FDG PET/CT and post-neoadjuvant therapy FDG PET/CT followed by anatomical resection of lung and ipsilateral mediastinal lymph nodes (LN). Seventeen of these patients who had PET/CT studies in our institution and were operated after CMRT were retrospectively included in the study group (12 males, ages 43–78 years; stage IIIA: 14 patients, stage IIIB: 3 patients). PET/CT response in N2 was visually scored per-lymph node station and per patient. Quantitative N2 response was evaluated by SUVmax and total lesion glycolysis (TLG) measurements after therapy alone and in comparison with pre-therapy values. PET/CT N2 response was confirmed at surgery.
Results
Seventeen NSCLC patients with 29 metastatic N2 lymph nodes (LN) were assessed. Histopathology confirmed 14 responders and 3 non-responders, and was available in 20/29 metastatic LN, showing complete response in 17 and residual disease in 3 LN. LN-based visual analysis of N2 response on PET/CT defined 3 TP, 16 TN and 1 FP, for sensitivity, specificity, accuracy, negative and positive predictive values (NPV and PPV) of 100, 94, 95, 100 and 75 %, respectively. Patient-based visual analysis defined 3 TP, 13 TN and 1 FP study, for sensitivity, specificity, accuracy, NPV and PPV of 100, 93, 94, 100 and 75 %, respectively. Nodal-based quantitative analysis of FDG uptake in N2 nodes revealed a significant difference between responding and non-responding LN only of SUVmax post-therapy (2.5 ± 1.21 vs. 3.5 ± 2.36, P = 0.04).
Conclusion
FDG PET/CT after neoadjuvant therapy accurately defined response in metastatic N2 nodes of NSCLC patients, presenting very high sensitivity and NPV for detecting responding nodes. PET/CT may enable selection of candidates for curative resection of stage III NSCLC. Mediastinoscopy may not be mandatory in patients with a negative PET/CT after neoadjuvant therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer death worldwide, with mortality rate greater than the sum of all other solid common tumors [1–4]. The low overall 5-year survival of non-small cell lung cancer (NSCLC) of 15 % is mainly the result of an advanced metastatic stage at initial presentation in about 40 % of patients [5]. Only 30 % of NSCLC patients present with an early disease limited solely to the lung, which allows surgical resection, alone or as part of a combined treatment, with improved survival rates.
For 28 % of patients presenting with locally advanced disease (stage IIIA), combined treatment options are currently available [6]. For patients with a typical stage IIIA NSCLC disease, the currently most effective treatment is the combination of neoadjuvant preoperative chemo- or chemo-radiotherapy followed by surgical resection, yielding a cure rate of 25–35 % [7]. Stage IIIA of NSCLC includes a variety of patients, with either a primary tumor of stages T1–T3 and metastatic lymph nodes (LN) at N2 station or a primary T4 tumor and lymph nodes metastases at stations N1 or N2 [8]. The status of N2 nodal disease after neoadjuvant therapy is of paramount prognostic and clinical significance.
Patients with N2 lymph node metastases will be referred to an operative resection only in the presence of responding mediastinal disease, since only with such response, surgical resection will increase postoperative survival in these patients [9–13]. Correct identification of response to neoadjuvant chemotherapy in mediastinal lymph nodes is therefore very important; it allows the appropriate selection of surgical candidates and prevents futile operative procedures [14].
Monitoring response to therapy in NSCLC patients is mainly based on RECIST criteria assessing changes in tumor size on CT, which may not necessarily correlate with pathological response [15–18]. Several studies have suggested, in variable groups of patients, that decreased FDG uptake in sites of disease on PET/CT after therapy may be used to define response of NSCLC to neoadjuvant chemotherapy [14, 17–19].
The current study aimed at examining the value of FDG PET/CT in assessing the response to neoadjuvant chemotherapy at mediastinal lymph nodes among a homogenous selected group of NSCLC patients with N2 disease and otherwise resectable disease, since N2 status is one of the major factors directing surgical management and affecting outcome. To assess specifically and accurately the value of FDG PET/CT for defining response of N2 disease sites, we choose to selectively evaluate only patients with surgically confirmed nodes. Although by that we could reliably assess only the negative and not the positive predictive value of FDG PET/CT after CMRT, we considered the ability to non-invasively exclude non-responding patients from futile operation as a clinically significant issue.
Materials and methods
Patients
Forty-five patients with locally advanced stage III NSCLC disease involving N2 lymph nodes who (1) were referred to neoadjuvant chemotherapy or chemoradiotherapy, (2) underwent FDG PET/CT before and after neoadjuvant therapy, and (3) were operated in the Department of General Thoracic Surgery at Rambam Health Care Campus from January 1, 2008 to January 1, 2011 were retrospectively recruited. The study was approved by the Local Ethics Committee in accordance with the Helsinki Declaration. Patients who failed to demonstrate a favorable response of the primary tumor (as assessed by the multidisciplinary meeting held per patient, please see “Surgical procedure” hereunder), patients in whom clinical status or technical surgical difficulties hindered the performance of complete mediastinal lymphadenectomy during surgery after neoadjuvant CMRT, or patients whose either pre- or post-CMRT PET/CT were not performed in our institution, were excluded.
Surgical procedure
The decision to operate patients after neoadjuvant CMRT was based on (1) the presence of an N2 disease with the clinical staging of IIIA, and (2) a clinical determination of a favorable response in terms of reduction of both size and uptake of the mediastinal lymph nodes as well as the primary tumor in response to neoadjuvant therapy, made by a multidisciplinary tumor assessment board of specialists from the fields of pathology, imaging, oncology, pulmonology, and thoracic surgery. The aforementioned routine clinical workup did not include a pre-neoadjuvant therapy mediastinoscopy to confirm N2 disease. All operated patients underwent a posterolateral or lateral thoracotomy operation and ipsilateral thoracic lymphadenectomy, including hilar and mediastinal lymph nodes. Special attention was given to resection of lymph nodes that were positive in the pre-therapy PET/CT study. All patients had complete anatomical lung resection with negative margins.
Pathologic analysis
A pathologist evaluated all surgical resection specimens of mediastinal lymph nodes to determine pathological tumor response. Pathological response to neoadjuvant therapy of mediastinal lymph node metastases was classified as pathological complete response when there were no tumor cells in the mediastinal lymph nodes and as pathological non-response in the presence of residual microscopic or macroscopic disease in mediastinal N2 lymph nodes.
Imaging protocol
A hybrid PET/CT system (GE Discovery LS, GE, Milwaukee, USA) was used for a four slice, helical CT acquisition, followed by a full-ring dedicated PET scan of the same axial range. The CT component was operated with an X-ray tube voltage peak of 140 keV, 80 mA, 6:1 pitch and slice thickness of 4.25 mm, with a rotational speed of 0.8 s per rotation. Post-therapy FDG PET/CT was performed in a median of 31 days before surgery (range 5–85).
Patients were instructed to fast for at least 4 h before injection (except for glucose-free oral hydration), and blood glucose was measured before injection of the tracer. No CT contrast agents were administered. Pre-therapy FDG PET/CT was performed 107 ± 12 min after injection of 12.8 ± 1.4 mCi of 18F-FDG. Post-therapy FDG PET/CT was performed 99 ± 11 min after the injection of 14.1 ± 2.2 mCi 18F-FDG. PET was performed for 5 min per field of view, each covering 14.5 cm, at an axial sampling of 4.25 mm/slice. Both PET and CT were performed with normal tidal breathing. PET images were reconstructed using ordered subset expectation maximization (OSEM) software, using CT-derived attenuation correction. The attenuation-corrected PET images, the CT images and the fused PET-CT images were available for review in axial, coronal and sagittal planes, as was a cine display of maximum intensity projections (MIP) of the PET data, and for analysis using the manufacturer’s review station (Xelerisand AW, GE, Milwaukee, USA).
FDG PET/CT interpretation
To create homogeneity in the interpretation of the imaging tests before and after neoadjuvant treatment, both FDG PET/CT studies were retrospectively reviewed and interpreted by two senior, highly experienced nuclear medicine specialists (BSR and KO); disagreements were resolved by consensus. The interpretation of both tests was performed visually and semi-quantitatively while being blinded to the operation results and consequent follow-up.
Visual interpretation
A pathological FDG uptake was defined when not following physiological FDG distribution pattern and/or when not explained by a known benign process. A focal FDG uptake in mediastinal lymph nodes of intensity significantly greater than the background mediastinal blood pool activity was defined as positive for malignancy. Pre- and post-therapy FDG PET/CT studies were compared with regard to the presence of malignant mediastinal nodes at N2 stations. Treatment response of N2 mediastinal lymph node metastases was visually defined using the following score:
Score 1: Complete response: No pathological uptakes at mediastinal LN metastases.
Score 2: Significant response: A substantial reduction in area and intensity of FDG uptake in mediastinal LN, with only a residual mild uptake of intensity equal or lower than that of normal mediastinum. Background mediastinal blood pool activity was evaluated in the region of either the ascending or descending thoracic aorta.
Score 3: Partial response: Reduction in area and intensity of FDG uptake in mediastinal LN, with residual pathological uptake of intensity greater than that of mediastinum.
Score 4: No response: No change in findings as compared with pre-treatment PET/CT.
Score 5: Progression: Worsening of findings as compared to the pre-therapy FDG PET/CT, with increased uptake in prior sites or appearance of new foci of disease.
PET/CT studies with visual scores 1–2 were considered as negative and scores 3–5 were considered positive for residual LN disease on PET/CT.
PET/CT results in terms of treatment response of mediastinal LN were confirmed by postoperative histopathology of these sites.
For patient-based analysis, in patients with more than one N2 station involved, response on PET/CT was defined based on the worst response within N2 nodes (i.e., the node which showed the smallest decrease of FDG uptake).
Semi-quantitative interpretation
Semi-quantitative analysis of treatment response in mediastinal LN metastases on PET/CT after therapy was performed using SUVmax and TLG after therapy in sites of pre-therapy uptake in N2 lymph nodes. TLG reflects metabolic volume and is expressed as the product of the average uptake intensity (SUVaverage) and the uptake volume at the area where the uptake intensity is at least 42 % of the maximal uptake. In addition, the percent changes in SUVmax (ΔSUV) and in TLG (ΔTLG) at N2 nodes between pre- and post-treatment studies were assessed.
Statistical analysis
All analyses were conducted using SPSS (Statistical Package for the Social Sciences), Version 21 (SPSS Inc., Chicago, IL, USA). Data are presented as median [25th–75th percentile; interquartile range] values and proportions. Primary outcome measures were analyzed using two-tailed, non-parametric Mann–Whitney U tests. Sensitivity, specificity, accuracy, and negative/positive predictive values were calculated using standard definitions. Statistical significance was set at P < 0.05.
Results
Seventeen patients with N2 NSCLC (12 males; 5 females) involving 29 FDG-avid N2 mediastinal lymph nodes were retrospectively included in the final study group. Twenty N2 lymph nodes (LN) were available for histological confirmation. Patients’ demographics, clinical and pre-therapy PET/CT data are detailed in Table 1.
Pathological complete response was observed in 14 of 17 patients (82 %) and in 17 (85 %) of the 20 LNs which were available for histological confirmation. Residual disease was found in 3 LNs in 3 patients. No correlation was found between the type of neoadjuvant therapy and pathological complete response rate (75 % in chemotherapy and 78 % in chemoradiotherapy patients, P = 0.9).
PET/CT response: visual analysis
Visual analysis agreement between the two authors who reviewed the PET/CT data (BSR and KO) was reached regarding 15 patients (out of 17; 88 %) and 27 FDG-avid N2 mediastinal lymph nodes (out of 29; 93 %). The precise location of two lymph nodes was achieved by consensus.
Nodal-based FDG PET/CT visual analysis of 29 pre-treatment PET/CT positive N2 LNs yielded 23 (79 %) negative LNs, including 21 (72 %) nodes with complete response (score 1) and 2 (7 %) nodes with significant response (score 2). There were 6 positive nodes (21 %) including 5 (17 %) nodes with partial response (score 3), and a single node (3 %) with stable disease (score 4). Analysis of 20 histologically confirmed N2 LNs defined 16 true-negative (TN) nodes, 3 true positives (TP), 1 false positive (FP) with antracosis in a patient treated with chemotherapy alone, and no false negative (FN) nodes (Fig. 1). Sensitivity, specificity, accuracy, negative and positive predictive values (NPV and PPV) of FDG PET/CT for detecting residual N2 disease after neoadjuvant were 100, 94, 95, 100 and 75 %, respectively.
A True-negative FDG PET/CT images of a 54-year-old male patient with right lower lobe adenocarcinoma (clinical staging III A, T1N2M0). a Pre-therapy FDG PET/CT axial images (from left to right: CT, PET/CT, PET), demonstrating pathological FDG uptake at subcarinal station #7. b Post-therapy FDG PET/CT axial images (from left to right: CT, PET/CT, PET) taken 7 weeks after the patient’s completion of four courses of taxol and carboplatin. Images demonstrate a complete response due to the absence of pathological subcarinal FDG uptake and decrease in adenopathy. The patient underwent a right lower lobe resection, after which the pathological examination demonstrated no evidence of malignancy. B True-positive FDG PET/CT images of a 78-year-old female patient with right lower lobe adenocarcinoma (clinical staging III A, T1N2M0). a Pre-therapy FDG PET/CT axial images [from left to right: CT, PET/CT, PET, maximal intensity projection (MIP) PET], demonstrating pathological FDG uptake at subcarinal station #7 (SUVmax = 5.5). b Post-therapy FDG PET/CT axial images (from left to right: CT, PET/CT, PET, MIP PET) taken 4 weeks after the patient’s completion of four courses of alimta and carboplatin. Images demonstrate a partial response, since although reduction in the intensity and area of pathological FDG uptake at the subcarinal station is evident, pathological uptake is still present (SUVmax = 3.5, ∆SUVmax = 37.1). The patient underwent a right lower lobe resection, after which the pathological examination demonstrated evidence of residual malignancy
Patient-based visual analysis of N2 response on FDG PET/CT revealed 13 TN studies, 3 TP studies and 1 FP study for residual N2 disease, for sensitivity, specificity, accuracy, NPV and PPV for detecting responding N2 patients after neoadjuvant therapy of 100, 93, 94, 100 and 75 %, respectively.
There was no statistical difference in the values of TP, TN and FP of post-CMRT PET/CT between patients with squamous cell vs. adenocarcinoma (Ps >0.38) or between patients treated with chemo- vs. chemo-radiotherapy (Ps >0.51).
PET/CT response: semi-quantitative analysis (SUVmax and TLG)
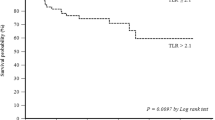
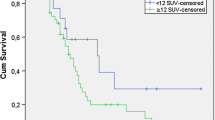
A significant difference was found in SUVmax values after therapy between responding and non-responding N2 nodes. Median SUVmax of N2 nodes after neoadjuvant therapy was significantly lower in 17 responding nodes as compared with 3 non-responding nodes (2.5 ± 1.21 vs. 3.5 ± 2.36, P = 0.04).
There was no significant difference in TLG after therapy between responding and non-responding N2 nodes (Table 2).
As compared with pre-treatment measurements, SUVmax and TLG values were significantly decreased after neoadjuvant therapy in all patients. Mean SUVmax in N2 nodes decreased from 5.6 to 2.5 after treatment and TLG decreased from 16.7 to 5.4 (P < 0.0001). However, there was no significant difference in the percentage of reduction between responding and non-responding patients for either ΔSUVmax or ΔTLG (Table 2).
Discussion
Multimodality therapeutic approach including preoperative chemoradiotherapy has led to a substantial improvement in survival of patients with locally advanced NSCLC [2].
Response of mediastinal lymph nodes to neoadjuvant therapy (LN downstaging) is the best-studied prognostic factor, with 5-year survival of 15 % for patients with persistent pN2 disease after induction therapy as compared with 30–40 % for patients with pN0 disease [4–8]. Confirmation of response in previously involved N2 nodal stations after neoadjuvant therapy is therefore crucial for appropriate selection of surgical candidates. This usually requires invasive procedures, including redo transesophageal ultrasound, redo mediastinoscopy, anterior mediastinotomy, video-assisted thoracoscopy, and/or thoracotomy, all involved with increased morbidity and cost.
The value of FDG-PET/CT for defining resectability after neoadjuvant chemo- or chemo-radiotherapy in patients with locally advanced NSCLC has been investigated by several authors. Most of these studies aimed at assessing therapy response in the primary tumor while only limited data specifically targeted response of N2 alone, showing that FDG-PET/CT results correlated with the pathologic response of the most metabolically active mediastinal node. Other authors, however, indicated limitation of FDG PET/CT after induction therapy in detecting microscopic tumor foci and small tumors surrounded by background soft tissue activity deep in the mediastinum that remain after induction therapy [20].
In the present study, we aimed at assessing specifically and exclusively a homogenous group of N2 disease patients and sites, as this is one of the major variables affecting surgical decision and is the best-known factor for favorable outcome. The potential ability to non-invasively assess N2 nodal status may simplify the algorithm of patient selection so that surgery can be suggested without preoperative invasive interventions. Our study demonstrated that FDG PET/CT had sensitivity and NPV of 100 % for defining histological response to neoadjuvant therapy in N2 nodes of this limited and selected group of NSCLC patients. Our visual scoring system indicated that after neoadjuvant therapy only high-intensity nodal uptake should be considered abnormal, while some mild residual uptake is of no clinical significance. This was also expressed by the significant difference of post-therapy SUVmax values within N2 nodes found between responding and non-responding nodes.
Surprisingly, we did not find significant difference in ΔSUV measurements before and after therapy between responding and non-responding sites. We believe this finding is related to the intense pre-therapy uptake seen on metastatic nodes, coupled with the overall significant decrease in FDG uptake, which was observed post-therapy in all patients. In spite of the post-therapy significant difference between responding and non-responding nodes, the percentage of decrease—relative to the initial intense uptake—was statistically insignificant. While this may be associated with the relatively small size of the study population, we believe this is chiefly related to the overall significant decrease in FDG uptake seen after therapy in the entire study group, indicating that the task is really to detect a small fraction of residual resistant disease on the “background” of an overall significantly responding tumor mass.
Although our initial aim was to use TLG measurements to assess the impact of “volume” measurements on response evaluation as well, we found that this parameter had no significant diagnostic value for monitoring response either after therapy alone or as ∆TLG. The significant decrease in FDG uptake in disease sites after therapy probably hampered the ability to accurately define the “metabolic volume” within mediastinal background activity.
Most prior studies assessed FDG PET/CT for monitoring both primary tumor and nodal response together and only few assessed N2 response alone. Cerfolio et al. [21] evaluated the FDG-PET in 34 NSCLC patients, only 11 of whom had N2 disease. The sensitivity, specificity, accuracy, PPV and NPV of FDG PET after neoadjuvant therapy for response in N1 and N2 nodes were comparable to our results, namely 97, 67, 94, 97, 67, respectively. Performance was slightly better for paratracheal N2 nodes as compared with other N2 stations.
In another study of 26 NSCLC patients, Yamamoto et al. assessed the ability of FDG-PET after induction chemoradiotherapy to predict pathological response of primary tumor and nodal disease [22]. Using an arbitrary SUV threshold of 4.5 as the cut-off value for differentiating responders from non-responders, post-chemoradiotherapy PET scan accurately predicted nodal response in 22 (85 %) of 26 patients with either N1, N2 or N3 disease before induction therapy. Post-therapy PET predicted all 18 patients with postoperative pN0 disease.
Several reports indicated possible interference of radiation with FDG PET interpretation and better accuracy for FDG PET after neoadjuvant therapy in squamous cell lung cancer as compared with adenocarcinomas, mainly for assessing the primary tumor response [10, 14, 23, 24]. In present study, we selectively assessed mediastinal nodes and found no differences between PET/CT performance in different type of neoadjuvant therapy or type of lung malignancy.
The main limitations of our study are its retrospective nature, the small size of study population and mainly the selection bias related to the evaluation of N2 pathologically confirmed nodes only. Patients who were omitted from surgery, among other factors due to positive PET/CT results, were not included in the current assessment; therefore, since potential false positive PET/CT studies may have missed our data regarding specificity and PPV values should be critically considered.
Nevertheless, the very high values of sensitivity and NPV found in the present study are significant and of incremental value as histologically confirmed in this highly homogenous group of patients and nodal metastatic sites. This is reflected by the relatively high complete pathologic response rate of 82 % in N2 nodes in the present study as compared with 27–34 % rate in other studies [24]. The high NPV of PET/CT in these patients suggests that mediastinoscopy may not be necessary for patients with a negative PET/CT after neoadjuvant therapy, but this should be further evaluated in large-scale prospective studies. In addition, specificity issues of PET/CT related to N2 nodal response should be clarified before excluding curative surgery based on positive PET/CT results after neoadjuvant therapy.
Conclusion
FDG PET-CT is highly accurate for detecting responding N2 nodes after neoadjuvant therapy of NSCLC, enabling the selection of surgical candidates for successful curative resection of stage III disease, preventing surgery of non-responding patients. The potential possibility suggested by present retrospective study results, to use this high NPV of PET/CT to omit mediastinoscopy in patients with a negative PET/CT after neoadjuvant therapy, should be further assessed in large-scale prospective studies.
References
Weir HK, Thun MJ, Hankey BF, Ries LA, Howe HL, Wingo PA, et al. Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention. J Nat Cancer Ins. 2003;95(17):1276–9.
Jemal A, Murray T, Samuels A, Ghafoor A, Ward E, Thun MJ. Cancer statistics, 2003. CA Cancer J Clin. 2003;53:5–26.
Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of eighteen major cancers in 1985. Int J Cancer. 1993;54:594–606.
Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med. 2004;3550:379–92.
Kobrinsky NL, Klug MG, Hokanson PJ, Sjolander DE, Burd L. Impact of smoking on cancer stage and diagnosis. J Clin Oncol. 2003;21:907.
Shields T. General thoracic surgery. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
Poettgen C, Theegarten D, Eberhardt W, Levegruen S, Gauler T, Krbek T, et al. Correlation of PET/CT findings and histopathology after neoadjuvant therapy in non-small cell lung cancer. Oncology. 2007;73:316–23.
Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, et al. The IASLC Lung Cancer Staging Project: Proposals for the revision of the TNM stage groups in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol. 2007;2:706.
Weber WA, Petersen V, Schmidt B, Tyndale-Hines L, Link T, Peschel C, et al. Positron emission tomography in non-small-cell lung cancer: prediction of response to chemotherapy by quantitative assessment of glucose use. J Clin Oncol. 2003;21(14):2651–7.
Pisters KM, Ginsberg RJ, Giroux DJ, Putnam JB Jr, Kris MG, Johnson DH, et al. Induction chemotherapy before surgery for early-stage lung cancer: a novel approach. Bimodality Lung Oncology Team. J Thorac Cardiovasc Surg. 2000;119(3):429–39.
Roth JA, Atkinson EN, Fossella F, Komaki R, Bernadette Ryan M, Putnam JB Jr, Lee JS, Dhingra H, De Caro L, Chasen M, Hong WK. Long-term follow-up of patients enrolled in a randomized trial comparing perioperative chemotherapy and surgery with surgery alone in resectable stage IIIA non-small-cell lung cancer. Lung Cancer. 1998;21:1–6.
Felip E, Rosell R. Is the evidence in favour of neoadjuvant chemotherapy in stage IIIA (N2) non-small cell lung cancer solid enough? Monaldi Arch Chest Dis. 2000;55:305–10.
Betticher DC, Hsu Schmitz SF, Tötsch M, Hansen E, Joss C, von Briel C, Schmid RA, et al. Mediastinal lymph node clearance after docetaxel-cisplatin neoadjuvant chemotherapy is prognostic of survival in patients with stage IIIA pN2 non-small-cell lung cancer: a multicenter phase II trial. J Clin Oncol. 2003;21(9):1752–9.
Cerfolio RJ, Bryant AS, Winokur TS, Ohja B, Bartolucci AA. Repeat FDG-PET after neoadjuvant therapy is a predictor of pathologic response in patients with non-small cell lung cancer. Ann Thorac Surg. 2004;78:1903–9.
Therasse P, Eisenhauer EA, Verweij J. RECIST revisited: a review of validation studies on tumour assessment. Eur J Cancer. 2006;42:1031–9.
Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981;47:207–14.
Mac Manus MP, Hicks RJ, Matthews JP, McKenzie A, Rischin D, Salminen EK, et al. Positron emission tomography is superior to computed tomography scanning for response-assessment after radical radiotherapy or chemoradiotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2003;21:1285–92.
Vansteenkiste J, Fischer BM, Dooms C, Mortensen J. Positron-emission tomography in prognostic and therapeutic assessment of lung cancer: systematic review. Lancet Oncol. 2004;5:531–40.
deGeus-Oei LF, van der Heijden HF, Corstens FH, Oven WJ. Predictive and prognostic value of FDG-PET in nonsmall-cell lung cancer: a systematic review. Cancer. 2007;110:1654–64.
Akhurst T, Downey RJ, Ginsberg MS, Gonen M, Bains M, Korst R, et al. An initial experience with FDG-PET in the imaging of residual disease after induction therapy for lung cancer. Ann Thorac Surg. 2002;73:259–66.
Cerfolio RJ, Ojha B, Mukherjee S, Pask AH, Bass CS, Katholi CR. Positron emission tomography scanning with 2-fluoro-2-deoxy-d-glucose as a predictor of response of neoadjuvant treatment for non-small cell carcinoma. J Thorac Cardiovasc Surg. 2003;125(4):938–44.
Yamamoto Y, Nishiyama Y, Monden T, Sasakawa Y, Ohkawa M, Gotoh M, et al. Correlation of FDG-PET findings with histopathology in the assessment of response to induction chemoradiotherapy in non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2006;33:140–7.
Ryu JS, Choi NC, Fischman AJ, Lynch TJ, Mathisen DJ. FDG-PET in staging and restaging non-small cell lung cancer after neoadjuvant chemoradiotherapy: correlation with histopathology. Lung Cancer. 2002;35:179–87.
Hicks Rodney J. Role of 18F-FDG PET in assessment of response in non-small cell lung cancer. J Nucl Med. 2009;50:31S–42S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kremer, R., Peysakhovich, Y., Dan, LF. et al. FDG PET/CT for assessing the resectability of NSCLC patients with N2 disease after neoadjuvant therapy. Ann Nucl Med 30, 114–121 (2016). https://doi.org/10.1007/s12149-015-1038-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-015-1038-7