Abstract
Purpose
To investigate the surgical prognosis and efficacy of adjuvant therapy in non-small cell lung cancer (NSCLC) with occult lymph node metastasis (ONM) defined by positron emission tomography/computed tomography (PET/CT).
Methods
A total of 3537 NSCLC patients receiving surgical resection were included in this study. The prognosis between patients with ONM and evident nodal metastasis, ONM patients with and without adjuvant therapy was compared, respectively.
Results
ONM was associated with significantly better prognosis than evident nodal metastasis whether for patients with N1 (5-year OS: 56.8% versus 52.3%, adjusted p value = 0.267; 5-year RFS: 44.7% versus 33.2%, adjusted p value = 0.031) or N2 metastasis (5-year OS: 42.8% versus 32.3%, adjusted p value = 0.010; 5-year RFS: 31.3% versus 21.6%, adjusted p value = 0.025). In ONM population, patients receiving adjuvant therapy yielded better prognosis comparing to those without adjuvant therapy (5-year OS: 50.1% versus 33.5%, adjusted p value < 0.001; 5-year RFS: 38.4% versus 22.1%, adjusted p value < 0.001).
Conclusions
ONM defined by PET/CT identifies a unique clinical subtype of lung cancer, ONM is a favorable prognostic factor whether for pathological N1 or N2 NSCLC and adjuvant therapy could provide additional survival benefits for ONM patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lymph node staging is a critical determinant for the therapeutic strategy in patients with non-small cell lung cancer (NSCLC). The occurrence of lymph node metastasis generally heralds a more guarded prognosis [1] and therefore calls for a more aggressive treatment [2]. For NSCLC with lymph node involvement, surgery alone cannot provide adequate oncological efficacy, adjuvant therapy has been proved to confer additional survival benefits [3,4,5,6,7,8].
In the clinical practice of lymph node staging, there is a highly specialized population of occult lymph node metastasis (ONM), in whom lymph nodal metastasis is ignored by preoperative staging modalities but unexpectedly recognized during surgery. ONM presents specific clinicopathologic characteristics and may represent a distinct invasive extent from clinically evident nodal metastasis [9, 10], which implies the prognostic and therapeutic uniqueness of ONM.
However, the prognosis and treatment strategy of ONM have not been clarified. For one thing, the controversy continues on the oncological results of ONM. Previous publications tended to favour ONM, demonstrating that ONM yielded better prognosis than clinically evident nodal metastasis [11, 12]. Conversely, there were also several studies drawing a negative conclusion, revealing ONM was not a significant prognostic factor in NSCLC with lymph node involvement [13, 14]. And the existing evidences only limited in the N2 subgroup, the significance of ONM in N1 population remains ambiguous. For another, the therapeutic strategy of ONM has not been fully investigated yet. The most common option for ONM is probably to proceed with surgery and administer adjuvant therapy. However, the benefits of adjuvant therapy remain an issue of contention [12,13,14,15].
In addition, ONM in prior studies were mainly defined according to the computed tomography modality. Positron emission tomography/computed tomography (PET/CT), which simultaneously provides the functional and anatomical information of tumours, has emerged as a more effective staging modality [16]. In the era of PET/CT, whether ONM defined by PET/CT represents a unique clinical subtype of NSCLC requires further investigation.
In such instances, this study aims to reveal the heterogeneity of prognosis between ONM and clinically evident nodal metastasis and tentatively explore the efficacy of adjuvant therapy in NSCLC with ONM.
Material and methods
Patients
We retrospectively reviewed 6737 consecutive patients with NSCLC who received surgical resection with hilar and mediastinal lymphadenectomy at Shanghai Pulmonary Hospital, Ningbo No. 2 Hospital, The First Hospital of Lanzhou University and Affiliated Hospital of Zunyi Medical College from January 2016 to September 2016. The approval of Institutional Review Board and waiver of written informed consent were obtained for this research.
Patients were excluded when meeting the following criteria: history of malignancy, sublobar resection, non-R0 resection, insufficient lymphadenectomy (numbers of resected lymph nodes < 6 or resected mediastinal stations < 3), carcinoma in situ or minimally invasive carcinoma, pathological N3 involvement, distant metastasis, pathological lymph node metastasis but without PET/CT and conduction of neoadjuvant therapy. Finally, a total of 3537 NSCLC patients were included (Fig. 1).
Preoperative evaluation and surgical treatment
Routine evaluation before surgery included chest X-ray and computed tomography (CT) scan, abdominal ultrasound, pulmonary function test, flexible bronchoscopy, assessment of cardiac function. Magnetic resonance imaging (MRI) of cerebrum and bone scintigraphy and were applied to rule out the distant metastasis. Considering PET/CT was not a routine administration in our institutions, we excluded patients with pathological lymph node metastasis but without preoperative PET/CT to confirm the reliability of the clinical staging in lymph node involved patients. ONM patients were defined as patients in whom there was no suspicion of lymph node involvement neither on CT (short-axis diameter < 1 cm), nor on PET (standardized uptake value < 2.5) [10]. The Parameters of The CT and PET Scanners were detailed in the supplementary material. The tumour stages were re-assessed according to eighth edition of the TNM staging system [1].
Adjuvant therapy and follow-up
Adjuvant chemotherapy was conducted for stage IB diseases with high-risk factors and stage IIA-IIIB tumours after surgery. Platinum-based doublet regimens were given for 4–6 cycles (3 weeks per cycle) after surgery. Adjuvant radiotherapy was administrated for stage III-N2 diseases. A radiotherapy dose of 50–60 Gy in 1.8–2.0 Gy per fraction was delivered for 5–6 weeks.
Follow-up was conducted at 3, 6, and 12 months within the first postoperative year and then at 1-year interval. Chest CT scan and abdominal ultrasound were routinely implemented. MRI scan for cerebrum and bone were adopted to excluded the distant metastasis. The PET/CT scan or/and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) were recommended when recurrence was suspected. Survival data were acquired from the outpatient visit and telephone follow-up. The overall survival (OS) was estimated as the duration since the day of surgery until the day of death or last follow-up visit. Patients alive would be censored at the last follow-up. Recurrence-free survival (RFS) was defined as the time elapsed between the date of surgery and the date of progress or death or last follow-up visit. Patients alive or without recurrence would be censored at the last follow-up. All patients completed follow-up survey up to September 2021.
Statistical analysis
Categorical data were presented as frequency (percentage) and compared by Pearson χ2 test or Fisher exact test. Normally distributed continuous parameters were exhibited as mean ± standard deviation and analysed using Student t-test, and continuous variables in skewed distribution were described as median (interquartile range [IQR]) and assessed by Mann–Whitney U test. The Kaplan–Meier method and Log-rank test were used to estimate the survival outcomes. Cox proportional hazards regression model was performed to identify the risk factors for the prognosis. All statistical analyses were conducted via SPSS 23.0 (IBM Corporation, Armonk, NY).
Results
Study population
The baseline characteristics were summarized in Table 1. The entire cohort of 3537 patients included 2220 (62.8%) men and 1317 (37.2%) women. There were 2110 (59.7%) adenocarcinomas and 999 (28.2%) squamous cell carcinomas. Most tumours (n = 3145, 88.9%) were treated with lobectomy. The median resected lymph node numbers and stations were 13 (range, 10–17) and 6 (range, 5–7), respectively. Postoperative adjuvant therapy was administered to 2132 (60.3%) patients. With respect to nodal status, most patients (n = 2762, 78%) were diagnosed as pathological N0 diseases, N1 and N2 metastasis were identified in 259 (7.23%) and 516 (14.63%) patients, respectively.
According to the preoperative staging outcome, 118 (3.36%) patients were categorized as occult N1 disease and 234 (6.62%) as occult N2 disease. No matter for N1 or N2 disease, ONM was significantly associated with less male (occult N1 versus evident N1: 60.2% versus 82.3%, p < 0.001; occult N2 versus evident N2: 53.8% versus 70.6%, p < 0.001), higher frequency of lobectomy (occult N1 versus evident N1: 83.05% versus 73.76%, p = 0.032; occult N2 versus evident N2: 86.32% versus 74.47%, p = 0.003), less resected lymph node numbers (occult N1 versus evident N1: 14 versus 15, p = 0.008; occult N2 versus evident N2: 13 versus 14, p = 0.002), more adenocarcinomas (occult N1 versus evident N1: 65.25% versus 34.04%, p < 0.001; occult N2 versus evident N2: 68.4% versus 56.4%, p = 0.020). In addition, as summarized in Table 2 station 11 (occult N1: 68.6%; evident N1: 64.5%) and station 4 (occult N2: 44%%; evident N2: 51.4%) were most frequently involved N1 station and N2 station, respectively.
Surgical prognosis of ONM
As displayed in Fig. 2 and Table 3, ONM was associated with significantly better prognosis than clinically evident lymph node metastasis whether for patients with N1 (5-year OS: 56.8% [47.8–67.6%] versus 52.3% [44.0–62.2%], adjusted p value = 0.267; 5-year RFS: 44.7% [35.8–55.8%] versus 33.2% [25.5–43.3%], adjusted p value = 0.031) or N2 metastasis (5-year OS: 42.8% [36.7–49.9%] versus 32.3% [27.0–38.5%], adjusted p value = 0.010; 5-year RFS: 31.3% [25.7–38.1%] versus 21.6% [17.1–27.4%], adjusted p value = 0.025). Subgroup analyses based on histology were illustrated in Fig. 3, for adenocarcinoma, ONM patients yielded significantly favourable prognosis than those with evident nodal metastasis no matter in N1 (5-year OS: 54.5% [43.3–68.3%] versus 49.4% [36.4–67.1%], adjusted p value = 0.342; 5-year RFS: 41.7% [31.1–56.0%] versus 35.9% [23.8–54.3%], adjusted p value = 0.049) or N2 disease (5-year OS: 44.8% [37.4–53.5%] versus 29.5% [23.0–37.9%], adjusted p value = 0.011; 5-year RFS: 30.4% [23.9–38.8%] versus 17.1% [12.0–24.6%], adjusted p value = 0.021). Similarly, for patients with squamous cell carcinoma, the occurrence of ONM was relevant to significantly improved prognosis compared with evident nodal metastasis in both N1 (5-year OS: 66.9% [48.2–92.9%] versus 65.3% [53.6–89.4%], adjusted p value = 0.768; 5-year RFS: 69.0% [51.1–93.3%] versus 32.5% [21.7–48.7%], adjusted p value = 0.035) and N2 involvement (5-year OS: 47.0% [32.7–67.4%] versus 39.4% [29.3–52.9%], adjusted p value = 0.471; 5-year RFS: 47.3% [33.1–67.6%] versus 28.4% [19.4–41.7%], adjusted p value = 0.047). However, in other histologies, ONM did not predict improved prognosis whether in N1 (5-year OS: 55.2% [35.9–85.0%] versus 34.1% [18.8–61.9%], adjusted p value = 0.240; 5-year RFS: 27.5% [11.6–65.3%] versus 29.8% [14.7–60.5%], adjusted p value = 0.839) or N2 disease (5-year OS: 31.0% [18.8–51.2%] versus 33.7% [22.0–51.5%], adjusted p value = 0.936; 5-year RFS: 18.9% [9.1–39.0%] versus 30.3% [19.4–47.4%], adjusted p value = 0.772).
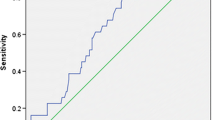
Adjuvant therapy benefits of ONM
In the ONM population (n = 352), adjuvant therapy was administrated to 292 (83%) patients, of them, 264 (75%) cases received adjuvant chemotherapy and 89 (25.3%) cases underwent adjuvant radiotherapy. The baseline between patients with and without adjuvant therapy did not differ significantly (Table 4). As illustrated in Fig. 4 & Table 5, patients receiving adjuvant therapy were associated with improved prognosis comparing to those without adjuvant therapy (5-year OS: 50.1% [44.4–56.6%] versus 33.5% [23.0–48.9%], adjusted p value < 0.001; 5-year RFS: 38.4% [32.9–44.8%] versus 22.1% [13.3–36.7%], adjusted p value < 0.001.
Discussion
ONM is a highly specialized group of lung cancer, in whom nodal metastasis evaded from the preoperative monitoring and only discovered during surgery. The current study raises two questions: does ONM defined by PET/CT yield better prognosis than evident nodal metastasis? If such is the case, should ONM population be considered as patients without histological nodal invasion, or as genuine positive nodal invasion?
Regarding the first question, it is presumed that compared to evident nodal metastasis, ONM may represent a lower extent of nodal involvement and tumour metastasis burden, which could be proved by results of this study that ONM patients tended to have a lower frequency of visceral pleural metastasis (42.6% versus 48.9%) and multi-station involvement (34.1% versus 42.8%). In addition, the occurrence of ONM may imply less aggressiveness and proliferation of the primary tumour, which was also indicated by the earlier T stage of ONM population in the current study (T3 and T4 stage: 10.5% versus 21.5%). Therefore, lower metastasis burden and less tumour aggressiveness of ONM jointly supported our hypothesis that ONM may be associated with better prognosis than evident nodal metastasis in patients with NSCLC.
In early studies, favourable prognostic impacts have been initially observed in ONM based on chest x-ray and bronchoscopy [11]. Thereafter, Andre et al. [12] claimed that occult N2 disease defined by CT and mediastinoscopy yielded better OS than evident N2 disease (evident N2 disease versus occult N2 disease: HR = 1.8, p < 0.001). In the era of modern staging modality, Cerfolio RJ, et al. [17] reported the first large PET/CT cohort in 2008. This study, however, did not directly compare the prognosis of occult N2 and evident N2, they found the 5-year survival of patients with occult N2 was 35%, better than the 5-year survival rate reported in previous publications. As such, they did not provide direct evidence regarding the difference between the prognosis of occult and evident N2 disease. A recent study conducted in 2018 [13] revealed that N2 metastasis negative on PET/CT achieved excellent surgical prognosis with 5-year OS of 48%, but despite better than N2 disease positive on PET/CT, the results did not differ significantly (p = 0.457). The current study included larger sample size of occult N2 disease and concurrently investigated the prognosis of occult N1 metastasis, revealing that ONM was associated with significantly better prognosis than evident lymph node metastasis whether for patients with N1 or N2 metastasis. These results proved that ONM and evident nodal metastasis were basically two distinct groups of NSCLC.
Answers of the second question would determine the optimal therapeutic strategy of NSCLC with ONM. If ONM population could be considered as patients without histological nodal invasion, postoperative monitoring is sufficient for those without high-risk components. According to our results, ONM was associated with significantly adverse prognosis compared to pathological N0 disease. Therefore, it would be more appropriate to classify ONM as genuine positive nodal invasion. In such instances, whether adjuvant therapy could confer additional survival benefits for ONM population becomes a crucial point. However, controversy continues on the role of postoperative adjuvant therapy in the ONM. In the study of Andre et al. [12] and Kim et al. [13], adjuvant therapy was not a significant prognostic predictor for the survival outcomes of occult N2 disease. In contrast, Kim et al. [15] analysed 115 pathological N2 disease negative on PET/CT, concluding that patients receiving adjuvant therapy were associated with better 5-year OS rate, but the difference did not reach statistical significance. Our results revealed that adjuvant chemotherapy did provide significant survival improvements whether for the occult N1 or N2 population, we speculated that it was attributable to the large sample size of our study, which enhanced the statistical efficacy of the results. Therefore, adjuvant therapy should be administrated as a routine procedure for ONM population.
There are several limitations of our study. Firstly, due to the retrospective nature, this study suffered from its inherent selection bias. Another limitation was represented by the heterogeneity in therapeutic regimens. The current study included the fact that not all patients received adjuvant therapy, and different drugs protocols and irradiation courses were administrated. Thirdly, in handing the lymph nodes in the N1 region, station 12–14 nodes were not routinely dissected, which potentially resulted in the underestimation of N1 metastasis. Finally, all included patients underwent PET/CT scans in four hospitals, the discrepancies in nuclear medicine physicians reporting, patient management and scan protocols, such as different resolution the equipment employed, different administration of a carbohydrate free diet before scanning and different time for uptake, were inevitable, which might result in heterogeneous results. In such instances, the generalization and robustness of our conclusion await validated by a randomized controlled trial.
In conclusion, our study demonstrated that ONM defined by PET/CT was a distinct group of NSCLC, which correlated to significantly better prognosis than clinically evident nodal metastasis. In treatment, adjuvant therapy could significantly improve the prognosis of ONM patients.
Data availability
Not applicable.
Code availability
Not applicable.
References
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol. 2016;11:39–51. https://doi.org/10.1016/j.jtho.2015.09.009.
National Comprehensive Cancer Network. (NCCN) Clinical Practice Guidelines in Oncology. Non-Small Cell Lung Cancer, Version 7. 2021. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed 29 Oct 2021.
Preoperative chemotherapy for non-small-cell lung cancer: a systematic review and meta-analysis of individual participant data. Lancet (London, England). 2014;383:1561-71. https://doi.org/10.1016/s0140-6736(13)62159-5.
Arriagada R, Bergman B, Dunant A, Le Chevalier T, Pignon JP, Vansteenkiste J. Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med. 2004;350:351–60. https://doi.org/10.1056/NEJMoa031644.
Pignon JP, Tribodet H, Scagliotti GV, Douillard JY, Shepherd FA, Stephens RJ, et al. Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE Collaborative Group. J Clin Oncol. 2008;26:3552–9. https://doi.org/10.1200/jco.2007.13.9030.
Scagliotti GV, Pastorino U, Vansteenkiste JF, Spaggiari L, Facciolo F, Orlowski TM, et al. Randomized phase III study of surgery alone or surgery plus preoperative cisplatin and gemcitabine in stages IB to IIIA non-small-cell lung cancer. J Clin Oncol. 2012;30:172–8. https://doi.org/10.1200/jco.2010.33.7089.
Song WA, Zhou NK, Wang W, Chu XY, Liang CY, Tian XD, et al. Survival benefit of neoadjuvant chemotherapy in non-small cell lung cancer: an updated meta-analysis of 13 randomized control trials. J Thorac Oncol. 2010;5:510–6. https://doi.org/10.1097/JTO.0b013e3181cd3345.
Uy KL, Darling G, Xu W, Yi QL, De Perrot M, Pierre AF, et al. Improved results of induction chemoradiation before surgical intervention for selected patients with stage IIIA-N2 non-small cell lung cancer. J Thorac Cardiovasc Surg. 2007;134:188–93. https://doi.org/10.1016/j.jtcvs.2007.01.078.
Chen Z, Xiong S, Li J, Ou L, Li C, Tao J, et al. DNA methylation markers that correlate with occult lymph node metastases of non-small cell lung cancer and a preliminary prediction model. Transl Lung Cancer Res. 2020;9:280–7. https://doi.org/10.21037/tlcr.2020.03.13.
Vaghjiani RG, Takahashi Y, Eguchi T, Lu S, Kameda K, Tano Z, et al. Tumor Spread Through Air Spaces Is a Predictor of Occult Lymph Node Metastasis in Clinical Stage IA Lung Adenocarcinoma. J Thorac Oncol. 2020;15:792–802. https://doi.org/10.1016/j.jtho.2020.01.008.
Martini N, Flehinger BJ, Zaman MB, Beattie EJ Jr. Results of resection in non-oat cell carcinoma of the lung with mediastinal lymph node metastases. Ann Surg. 1983;198:386–97. https://doi.org/10.1097/00000658-198309000-00015.
Andre F, Grunenwald D, Pignon JP, Dujon A, Pujol JL, Brichon PY, et al. Survival of patients with resected N2 non-small-cell lung cancer: evidence for a subclassification and implications. J Clin Oncol. 2000;18:2981–9. https://doi.org/10.1200/jco.2000.18.16.2981.
Kim MP, Correa AM, Hofstetter WL, Mehran RJ, Rice DC, Roth JA, et al. Occult stage IIIA-N2 patients have excellent overall survival with initial surgery. J Thorac Dis. 2018;10:6670–6. https://doi.org/10.21037/jtd.2018.10.94.
Yang CF, Kumar A, Gulack BC, Mulvihill MS, Hartwig MG, Wang X, et al. Long-term outcomes after lobectomy for non-small cell lung cancer when unsuspected pN2 disease is found: A National Cancer Data Base analysis. J Thorac Cardiovasc Surg. 2016;151:1380–8. https://doi.org/10.1016/j.jtcvs.2015.12.028.
Kim HK, Choi YS, Kim K, Shim YM, Park K, Ahn YC, et al. Outcomes of mediastinoscopy and surgery with or without neoadjuvant therapy in patients with non-small cell lung cancer who are N2 negative on positron emission tomography and computed tomography. J Thorac Oncol. 2011;6:336–42. https://doi.org/10.1097/JTO.0b013e318201212e.
Whitson BA, Groth SS, Maddaus MA. Recommendations for optimal use of imaging studies to clinically stage mediastinal lymph nodes in non-small-cell lung cancer patients. Lung cancer (Amsterdam, Netherlands). 2008;61:177–85. https://doi.org/10.1016/j.lungcan.2007.12.019.
Cerfolio RJ, Bryant AS. Survival of patients with unsuspected N2 (stage IIIA) nonsmall-cell lung cancer. Ann Thorac Surg. 2008;86:362–6; discussion 6–7. https://doi.org/10.1016/j.athoracsur.2008.04.042.
Funding
Supported by the National Natural Science Foundation of China (91959126, 8210071009), Science and Technology Commission of Shanghai Municipality (20XD1403000, 21YF1438200), Shanghai Municipal Health Commission (201940018), Shanghai Hospital Development Center (SHDC2020CR3047B), and Clinical Research Foundation of Shanghai Pulmonary Hospital (FK1943, FK1937).
Author information
Authors and Affiliations
Consortia
Contributions
Yifan Zhong, Jiajun Deng, Yunlang She and Chang Chen contributed to the concept and design of the study. Minglei Yang, Minjie Ma and Yongxiang Song were responsible for acquiring the data. Tingting Wang performed data analysis and statistical analysis. Yifan Zhong and Jiajun Deng drafted the manuscript. Yunlang She and Chang Chen critically reviewed and approved the manuscript. The authors are on behalf of the MultiomIcs claSSIfier for pulmOnary Nodules (MISSION) Collaborative Group.
Corresponding authors
Ethics declarations
Ethics approval
Institutional Review Board of Shanghai Pulmonary Hospital, Ningbo No. 2 Hospital, The First Hospital of Lanzhou University and Affiliated Hospital of Zunyi Medical College approved this research.
Consent to participate
Waiver of written informed consent was obtained for this retrospective research.
Consent for publication
All authors agreed publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology - Chest
J Deng and Y Zhong contributed equally to this work; Y She and C Chen are co-corresponding authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deng, J., Zhong, Y., Wang, T. et al. Lung cancer with PET/CT-defined occult nodal metastasis yields favourable prognosis and benefits from adjuvant therapy: a multicentre study. Eur J Nucl Med Mol Imaging 49, 2414–2424 (2022). https://doi.org/10.1007/s00259-022-05690-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05690-3