Abstract
Perinatal anxiety is a prevalent mental health issue associated with deleterious effects; however, factors that affect treatment outcomes have yet to be identified. We examined predictors of treatment completion and moderators of treatment outcome among individuals receiving six weeks of group Cognitive-Behavioral Therapy for Perinatal Anxiety (CBT-PA) via retrospective chart review. Among 98 women (Mean age = 32.36, SD = 4.79; 87% postpartum), pregnancy (versus postpartum), comorbid depression, and greater pre-treatment anxiety symptoms, as measured by the Perinatal Anxiety Screening Scale, were predictive of treatment attrition. Among treatment completers, older maternal age was associated with greater number of sessions completed. Overall, anxiety symptom scores significantly reduced from pre- to post-treatment. Obsessive-compulsive symptoms, comorbid depression, and two or more comorbid diagnoses at pre-treatment were each significantly associated with higher overall anxiety scores across both time points. Further, women with versus without health anxiety at pre-treatment showed a greater reduction in anxiety from pre- to post-treatment. These results are important for informing clinicians of factors that may enhance overall treatment completion and effectiveness for perinatal populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The perinatal period, including pregnancy through the first 12-months postpartum, represents a period of increased vulnerability to maternal mental health difficulties (O’Hara & Wisner, 2014). Perinatal anxiety affects between 9 and 23% of women (Dennis et al., 2017; Fawcett et al., 2019) and is associated with adverse effects for both mother and infant, including increased risk of pregnancy and obstetrical complications, impaired mother-infant bonding, reduced breastfeeding duration, and increased infant illness (Beijers et al., 2010; Glasheen et al., 2010; Paul et al., 2013). Cognitive-Behavioral Therapy (CBT) is considered the first line treatment for anxiety disorders (Otte, 2011) and has recently been adapted specifically for the treatment of perinatal anxiety (CBT-PA; Furer et al., 2021; Green et al., 2015, 2020). Research to date suggests that CBT-PA is effective in reducing symptoms of anxiety both in the short-term (i.e., immediately post-treatment), as well as in the long-term (i.e., up to 12 months post-treatment (Li et al., 2022). CBT-PA can be delivered in group format, making it cost effective within the public health system, and offers additional therapeutic benefits of social support and interpersonal learning (Bieling et al., 2006). Further, CBT offers additional advantages compared with pharmacological treatment such as avoiding maternal and infant exposure to potential adverse effects associated with psychiatric medication, as well as lower relapse rates following CBT compared with pharmacological treatment (Clark et al., 2003).
Treatment attrition represents a considerable problem for the delivery of effective psychotherapy in community settings, with average attrition rates of 26% in the general population (Fernandez et al., 2015) and 16% in perinatal populations (Sockol, 2018). Understanding predictors of treatment attrition is important in developing mitigation strategies. In terms of sociodemographic variables, older age, higher education, and greater social support are associated with lower rates of attrition and greater number of completed CBT sessions in the general population (Edmonds et al., 2018; Hadjistavropoulos et al., 2016) and in perinatal women seeking treatment for depression (Bowen et al., 2012; Haga et al., 2019). Further, having children at home has been associated with fewer mindfulness-based cognitive therapy sessions attended among pregnant women (Evans et al., 2021), suggesting that primiparous status may affect the likelihood of attrition for women enrolled in CBT-PA. In terms of clinical variables, comorbid depression is associated with increased attrition among anxiety disorder populations in general (Fernandez et al., 2015) and severity of mental health symptoms has been associated with increased attrition among perinatal women seeking treatment for depression (Haga et al., 2019; Freeman & Davis, 2010). To our knowledge, such predictors have not been well-studied in perinatal anxiety disorder populations to-date.
In addition to understanding predictors of treatment completion and engagement, it is important to understand moderators of treatment effectiveness. CBT for anxiety disorders appears to be effective across socio-demographic variables (Piacentini et al., 2002; Schuurmans et al., 2009; Watanabe et al., 2010). With respect to clinical variables, however, the outcomes are mixed. CBT-PA is a transdiagnostic treatment in which the same protocol is applied across anxiety disorders (Furer et al., 2021). Although disorder-specific and transdiagnostic interventions have been found to result in equivalent outcomes (Dear et al., 2016; Titov et al., 2015), there is some evidence that disorder-specific interventions may produce larger effect sizes for women with perinatal anxiety than transdiagnostic interventions (Maguire et al., 2018). Further, several studies have found that comorbid depression predicts a lower anxiety treatment response to CBT (Chambless et al., 1997, 2000; Steketee et al., 2001; van Balkom et al., 2008; Watanabe et al., 2010), whereas other studies have found no predictive effect of comorbid depression (Kampman et al., 2008; Rief et al., 2000; Schuurmans et al., 2009). Such moderating factors have not yet been studied in the emerging literature on CBT-PA.
Current study
To examine predictors and moderators of group CBT-PA treatment outcome, we conducted a retrospective chart review of women who participated in CBT-PA through a public hospital Anxiety Disorders Service in central Canada. Aim 1 was to examine sociodemographic and clinical characteristics associated with CBT-PA completion (Aim 1a) as well as engagement in the treatment (Aim 1b), defined as the number of sessions attended. We hypothesized that older maternal age, higher education, having a partner, and being primiparous (i.e., pregnant with or given birth to first child) would be positively associated with treatment completion and greater engagement in treatment. Further, we hypothesized that comorbid depression as well as anxiety severity, as assessed by both self-reported anxiety symptoms as well as psychotropic medication use, would be negatively associated with completion and engagement in treatment. Given that CBT-PA is offered to both pregnant and postpartum women, we also explored whether pregnancy status predicted treatment completion and engagement.
Aim 2 of the current study was to examine clinical moderators of CBT-PA effectiveness in individuals who completed treatment to understand whether treatment effectiveness, operationalized as the reduction of self-reported anxiety disorder symptoms from pre- to post-treatment, was moderated by: (a) primary anxiety disorder, (b) depression comorbidity, and (c) number of comorbid disorders. We hypothesized that the presence of comorbid depression and/or other comorbid anxiety disorders would decrease treatment effectiveness.
Method
Participants
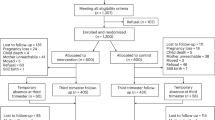
Participants were 98 adult women (Mean age = 32.36, SD = 4.79; 87% postpartum) who participated in a 6-session CBT-PA group through a community hospital. Inclusion criteria for the group included the presence of a clinically significant anxiety disorder during the perinatal period, English-speaking, and over 18 years of age. Individuals were excluded from participating in the group if they reported active mania or psychosis, uncontrolled substance use, active suicidality or self-harm, or if they declined to participate in the group treatment.
Measures and procedure
The current study retrospectively reviewed chart data from a group CBT program for perinatal anxiety disorders. Patients were referred to the program by a healthcare provider, including but not limited to, family physician, medical specialist, psychiatrist, and psychologist. All participants who were referred and met inclusion criteria were included in the study. All participants completed an intake assessment prior to engagement in the group in which demographic information on age (continuous), education (0 = less than college/university degree; 1 = at least college/university degree), perinatal status (0 = pregnant; 1 = postpartum), primiparous status (0 = no; 1 = yes), relationship status (0 = single; 1 = currently in a relationship), and current psychiatric medication (0 = no current medication; 1 = currently taking medication) was collected. Information on race/ethnicity and other socioeconomic variables were not collected and thus not available for the current analyses. Participants also completed a diagnostic interview with either a registered clinical psychologist or doctoral-level clinical psychology student or resident under the supervision of a registered clinical psychologist. Participants were given a specific anxiety diagnosis if they met criteria for a clinically significant anxiety disorder based on criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders- Fifth Edition (DSM-5; American Psychiatric Association, 2013).
Participants completed a 6-session CBT in-person group program for perinatal anxiety disorders (Furer & Reynolds, 2015). Data from a total of 16 groups (4 to 10 participants in each) offered between 2015 and 2019 were included in the current report. A brief overview of CBT-PA is provided in Table 1 (full details of the treatment are described in Furer et al., 2021). Groups were facilitated by a registered clinical psychologist and a clinical psychology graduate student. Participants were administered the Perinatal Anxiety Screening Scale (PASS; Somerville et al., 2014), at sessions 1 (baseline) and 6 (post-treatment). The PASS is a 31-item self-report scale used to measure anxiety symptoms during the perinatal period. Items are rated on a 4-point Likert-type scale from 0 (“not at all”) to 3 (“almost always”) with higher scores reflecting greater anxiety symptoms. Internal consistency in the current study was α = 0.93 at baseline and α = 0.94 at follow-up. Consistent with previous research using the same protocol (Furer et al., 2021), treatment completion was defined as attending at least three treatment sessions and treatment engagement was coded as 0 = moderate (3–4 sessions), 1 = high (5 sessions), and 2 = full (6 sessions).
Data analysis
To ensure the validity of the data, two research assistants independently coded the data and any discrepancies between coders were reviewed by the third author in a rating meeting and discussed until consensus was achieved. To examine individual predictors of treatment non-completion (Aim 1a) and treatment engagement (Aim 1b), we conducted chi-square tests for categorical predictors (education, pregnancy status, primiparous, postpartum, psychiatric medication, and depression status) and one-way analyses of variance (ANOVAs) for continuous predictors (age and baseline PASS). Further, to examine robust predictors of treatment non-completion, we conducted a binary logistic regression, and to examine robust predictors of treatment engagement, we conducted an ordinal logistic regression including all potential predictors. To examine the moderating effect of specific anxiety disorder diagnoses on PASS scores from pre- to post-treatment (Aim 2), we conducted eight longitudinal models using R (R Core Team, 2017) and the nlme package 3.1–131. PASS scores were entered as within-subject variables (Level 1) and moderators were entered as between-subject variables (Level 2). Level 1 allows for the estimation of within-subject change described by two parameters: an intercept (initial level of the variable) and a slope (rate of change over time). Level 2 allows for the examination of between-subject differences in these parameters. Time was uncentered so that the intercept could be interpreted as the value at the first assessment (pre-treatment). In all analyses, we allowed the intercept to vary across individuals. As described, moderators were coded such that the absence of the diagnosis was the reference point. We present the baseline linear model first (Model 1) and then the moderator analyses (Models 2 through 8). For Model 8, number of comorbid diagnoses was dummy coded such that the presence of one comorbid diagnosis and two or more comorbid diagnoses were compared to no comorbid diagnoses (reference group). To follow-up significant interactions, we examined symptom scores at each level of the moderator (i.e., presence or absence of the specific mental disorder) over time and then examined the simple main effects at each time point by calculating t-tests.
Results
Preliminary analyses
Regarding Aim 1, a total of 82 women completed the treatment program—defined as attending at least three sessions—with 16 non-completers (16% attrition rate). In the completer group, one participant was missing data on psychiatric medication use and seven were missing the pre-treatment PASS. In the non-completer group, three participants were missing the pre-treatment PASS data.
Regarding Aim 2, seven women did not complete the pre-treatment PASS and an additional 12 did not complete the post-treatment PASS, resulting in a final sample of 63 treatment completers for the moderation analyses. Those who completed the PASS (n = 63) did not differ significantly from those who did not (n = 19) on age, pregnancy status, primiparous, medication status, or number of diagnoses (all ps > 0.134). Further, pre-treatment PASS scores did not differ for women who did (n = 63) versus did not (n = 12) complete the post-treatment PASS, t(73) = 0.82, p = .413.
See Table 2 for the diagnostic composition of the full sample (N = 98) and the sub-sample used in Aim 2 (n = 63). A total of 31 participants met criteria for one disorder, 39 for two disorders, 21 for three disorders, 5 for four disorders, and 1 for five disorders.
Aim 1: predictors of Treatment Completion and Engagement
Treatment completion. Results are presented in Table 3. Postpartum women were more likely to complete treatment compared to pregnant women. As predicted, women with comorbid depression were less likely to complete treatment compared to women without comorbid depression. Similarly, women who did not complete treatment had significantly greater pre-treatment PASS scores compared to women who completed treatment. As 94% of participants were in a relationship, we were unable to examine relationship status as a predictor of treatment completion. When all predictors were entered into the regression analysis (n = 87), only comorbid depression remained a significant predictor of treatment non-completion, χ2(1) = 4.546, p = .033.
Engagement. Of treatment completers (n = 82), 36 participants (44%) attended all 6 sessions, 29 (35%) attended 5 sessions, and 17 (21%) attended 3–4 sessions. Age was a significant predictor of session engagement, F(2, 79) = 4.98, p = .009, ηp2 = 0.015. Follow-up simple main effects analyses revealed that participants who attended 3–4 sessions (M = 29.80, SD = 5.35) were significantly younger than participants who attended all 6 sessions (M = 34.03, SD = 4.39), p = .002, and younger at trend level from those who attended 5 sessions (M = 32.48, SD = 4.30), p = .058. There was no significant difference in age between participants who attended 5 versus 6 sessions, p = .177. No other demographic variables, nor baseline PASS scores, predicted session engagement, ps > 0.106. When all predictors were entered into the regression analyses (n = 74), age remained a significant predictor of treatment engagement, χ2(1) = 8.004, p = .005, 95% CI, 0.051 to 0.279.
Aim 2: moderation of treatment outcome by Symptom Profiles
Results of the moderator analyses are presented in Table 4. As expected, PASS scores significantly reduced from pre- to post-treatment (Model 1). We found evidence for a significant two-way interaction between time and health anxiety (Model 3). Although all participants showed significant reductions in PASS scores from pre- to post-treatment, women with health anxiety showed a greater reduction in PASS scores across time, b= -23.86, t(61)= -6.18, p < .001, compared to women without health anxiety, b= -14.73, t(61)= -9.35, p < .001. Simple main effects comparisons revealed no significant differences for women with versus without health anxiety at pre-treatment (M = 52.36, SD = 17.42; M = 45.15, SD = 14.51, respectively), t(61)= -1.34, p = .185, or post-treatment (M = 28.50, SD = 9.02; M = 30.41, SD = 16.35, respectively), t(61) = 0.34, p = .734. We did not find evidence of significant moderation by any of the other anxiety disorders, depression, or number of comorbid diagnoses. However, women with obsessive-compulsive disorder (Model 4) and comorbid depression (Model 7) at pre-treatment showed significantly higher overall PASS scores compared to women without these disorders. Similarly, women with two or more comorbid diagnoses showed significantly higher overall PASS scores compared to women with no comorbid diagnoses (Model 8).
Discussion
Perinatal anxiety affects close to a quarter of women and is associated with a number of negative health sequalae (Goodman et al., 2016). This study is among the first to examine predictors of completion and moderators of CBT-PA. Taken together with previous findings (Furer et al., 2021; Green et al., 2015, 2020), a brief group intervention involving transdiagnostic CBT is appropriate for women in the perinatal period across anxiety disorders. Our results are important for informing clinicians of factors that may enhance overall treatment completion, engagement, and effectiveness for perinatal populations. Importantly, our study was based on chart data from patients enrolled in CBT-PA at a tertiary care hospital, and thus, are applicable to clinicians working in similar real-world settings.
Postpartum status was associated with significantly reduced treatment attrition. Although the perinatal period encompasses both pregnancy and postpartum periods, a greater proportion of women in the current study were postpartum, which is consistent with previous research (Green et al., 2020). Cohesion and group belongingness are some of the core and necessary components of CBT group therapies (Bieling et al., 2006) and have been found to predict treatment outcomes (Paulus et al., 2015). It is possible that the pregnant participants felt less connected to the postpartum groups members or that group discussions were less applicable to pregnant participants. It is also possible that some of the pregnant participants withdrew from treatment because they gave birth during the course of treatment. We are now tracking this variable in our ongoing research. Future research should thoroughly assess factors that may contribute to premature termination among pregnant participants.
Consistent with the hypotheses, comorbid depression predicted treatment attrition from group CBT-PA. There is strong and convincing evidence that depression is associated with significant dropout from traditional CBTs (e.g., Fernandez et al., 2015; Issakidis & Andrews, 2004). In addition to symptoms of depression that might interfere with treatment adherence, including low energy, decreased motivation, and anhedonia (APA, 2013), depression severity is associated with reduced perceived value of treatment (Morey et al., 2007), which might also reduce adherence to CBT-PA. This finding is interesting, especially in light of previous findings that depression symptoms improve throughout the course of CBT-PA (Furer et al., 2021). It may be that this benefit is only conferred for those who have lower depression scores, or who are able to continue with the treatment despite their depressive symptoms. Further exploration of mechanisms through which comorbid depression influences treatment attrition is warranted.
Higher pre-treatment anxiety symptom scores were also a significant predictor of treatment attrition. Distress and avoidant tendencies are common components to anxiety presentations (American Psychiatric Association, 2013), which when elevated at baseline, may have been driving the decision to withdraw from treatment. For example, Edelman and Chambless (1995) found that participants with avoidant traits were more likely to withdraw from a CBT group than those without these traits. Brief motivational sessions prior to group therapy have been effective at reducing dropout with other anxiety presentations (Poulin et al., 2018). In light of the current findings, it may be necessary to further engage with women who present with comorbid depression or elevated pre-treatment anxiety to ensure they are adequately supported. Future research should assess whether one or two pre-treatment sessions or group sessions focused on behavioral activation or motivation enhance treatment engagement. With regards to Aim 2, we found a significant reduction in anxiety symptom scores at the completion of the 6-week CBT-PA program. Further, the reduction in anxiety symptom scores was not dependent on the specific anxiety disorder diagnosis at pre-treatment. Transdiagnostic approaches for emotional disorders (e.g., Unified Protocol; Barlow et al., 2011) have empirical support for effectiveness (Newby et al., 2015) and burgeoning research supports the use of a transdiagnostic treatment protocol for perinatal anxiety (Furer et al., 2021; Green et al., 2015, 2020). Given that CBT-PA seems to be effective without needing to be disorder-specific may mean that the program can be offered more readily, which is critical given the increasing prevalence of perinatal anxiety (Goodman et al., 2016) and lack of adequate resources (Harison et al., 2020). Although the findings from the current study are promising, future research is needed to directly compare this transdiagnostic approach to single disorder protocols to provide greater empirical support for transdiagnostic approaches.
Participants with a health anxiety diagnosis experienced the greatest anxiety symptom improvement from pre- to post-treatment. This result is consistent with previous research that has found higher health anxiety pre-treatment scores predict greater improvement in symptoms following CBT (Olatunji et al., 2014). Future researchers should explore if modifying CBT-PA protocol to uniquely target health anxiety impacts treatment outcomes. Further, obsessive-compulsive disorder, comorbid depression, and having two or more comorbid diagnoses were associated with higher overall anxiety symptom scores at both time points; however, CPT-PA appeared to reduce anxiety symptoms at a similar rate compared to other disorders. This finding is interesting in the context of our Aim 1 findings that higher pre-treatment anxiety symptom scores were associated with greater treatment dropout. Patient perceptions of skills and mastery have been found to predict treatment engagement in CBT for anxiety in the context of physical health (Cully et al., 2007). Together, our findings highlight the need for preliminary sessions to instill hope and motivation, because once engaged in the group, significant symptom improvement can be achieved.
Results of the current study should be viewed in light of the following limitations. First, although our attrition rate is consistent with previous research (see Sockol 2018 for a review), the sample size for non-completers was relatively small. It would be important to determine whether our Aim 1 results hold in a larger sample. Second, we did not have post-treatment PASS data for non-completers which prevented us from assessing treatment completion as a predictor of effectiveness. Future research would benefit from obtaining comprehensive data from both completers and non-completers to clarify the differential clinical outcomes based on competition status. Third, we did not have data on race/ethnicity or other possibly relevant sociodemographic variables, such as income, working status, relationship status, exposure to intimate partner violence, the presence of prenatal or postnatal complications, childcare, social support, etc. that may be important variables in predicting treatment attrition. Future research examining a broader set of predictors is warranted. Fourth, consistent with many psychotherapy studies, this study has a small sample size (N = 98). Future research should be conducted on a larger sample of perinatal women.
In conclusion, our study examined predictors of treatment completion and engagement, and moderators of treatment effectiveness of a transdiagnostic group CBT-PA treatment program. By first identifying the efficacy of this treatment (Furer at al., 2021; Green et al., 2015; 2020) and now clarifying who it is most effective and engaging for, clinicians can be better equipped to help women during this vulnerable time. Given the prevalence of perinatal anxiety, this work is an essential step in being able to provide an accessible and brief intervention to women in need, particularly in the context of anxiety.
References
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders, 5th ed.
Barlow, D. H., Farchione, T. J., Fairholme, C. P., Ellard, K. K., Boisseau, C. L., Allen, L. B., & Ehrenreich-May, J. (2011). Treatments that work. Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. Oxford University Press.
Beijers, R., Jansen, J., Riksen-Walraven, M., & de Weerth, C. (2010). Maternal prenatal anxiety and stress predict infant illness and health complaints. Pediatrics, 126, e401–409. https://doi.org/10.1542/peds.2009-3226
Bieling, P. J., McCabe, R. E., & Antony, M. M. (2006). Cognitive-behavioral therapy in groups. Guilford Press.
Bowen, A., Bowen, R., Butt, P., Rahman, K., & Muhajarine, N. (2012). Patterns of depression and treatment in pregnant and postpartum women. The Canadian Journal of Psychiatry, 57(3), 161–167.
Chambless, D. L., Tran, G. Q., & Glass, C. R. (1997). Predictors of response to cognitive-behavioral group therapy for social phobia. Journal of Anxiety Disorders, 11, 221–240. https://doi.org/10.1016/S0887-6185(97)00008-X
Chambless, D. L., Beck, A. T., Gracely, E. J., & Grisham, J. R. (2000). Relationship of cognitions to fear of somatic symptoms: A test of the cognitive theory of panic. Depression and Anxiety, 11, 1–9. https://doi.org/10.1002/(SICI)1520-6394(2000)11:1_1::AID-DA1_3.0.CO;2-X.
Clark, D. M., Ehlers, A., McManus, F., Hackmann, A., Fennell, M., Campbell, H., Flower, T., Davenport, C., & Louis, B. (2003). Cognitive therapy Versus Fluoxetine in Generalized Social Phobia: A randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology, 71(6), 1058–1067. https://doi.org/10.1037/0022-006X.71.6.1058
Cully, J. A., Graham, D. P., Stanley, M. A., & Kunik, M. E. (2007). Depressed and anxious COPD patients: Predictors of psychotherapy engagement from a clinical trial. Journal of Clinical Psychology in Medical Settings, 14, 160–164. https://doi.org/10.1007/s10880-007-9060-0
Dear, B., Staples, L., Terides, M., Fogliati, V. J., Johnston, L., & Titov, N. (2016). Transdiagnostic versus disorder-specific and clinician-guided versus self-guided internet- delivered treatment for social anxiety disorder and comorbid disorders: A randomized controlled trial. Journal of Anxiety Disorders, 42, 30–44. https://doi.org/10.1016/j.janxdis.2016.05.004
Dennis, C. L., Falah-Hassani, K., & Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. British Journal of Psychiatry, 210, 315–323. https://doi.org/10.1192/bjp.bp.116.187179
Edelman, R. E., & Chambless, D. L. (1995). Adherence during sessions and homework in cognitive-behavioral group treatment of social phobia. Behaviour Research and Therapy, 33, 573–577. https://doi.org/10.1016/0005-7967(94)00068-u
Edmonds, M., Hadjistavropoulos, H. D., Schneider, L. H., Dear, B. F., & Titov, N. (2018). Who benefits most from therapist-assisted internet-delivered cognitive behaviour therapy in clinical practice? Predictors of symptom change and dropout. Journal of Anxiety Disorders, 54, 24–32. https://doi.org/10.1016/j.janxdis.2018.01.003
Evans, A. P. B., Goodman, S. H., Dimidjian, S., & Gallop, R. (2021). The role of engagement in Mindfulness-Based Cognitive Therapy for the prevention of depressive relapse/recurrence in perinatal women. Mindfulness 12, 61–67. doi: https://doi.org/10.1007/s12671-019-01160-4
Fawcett, E. J., Fairbrother, N., Cox, M. L., White, I. R., & Fawcett, J. M. (2019). The prevalence of anxiety disorders during pregnancy and the postpartum period: A multivariate bayesian meta-analysis. The Journal of Clinical Psychiatry, 80, 18r12527.
Fernandez, E., Salem, D., Swift, J. K., & Ramtahal, N. (2015). Meta-analysis of dropout from cognitive behavioral therapy: Magnitude, timing, and moderators. Journal of Consulting and Clinical Psychology, 83(6), 1108–1122. https://doi.org/10.1037/ccp0000044
Freeman, M. P., & Davis, M. F. (2010). Supportive psychotherapy for perinatal depression: Preliminary data for adherence and response. Depression & Anxiety (1091–4269), 27(1), 39–45. https://doi.org/10.1002/da.20596
Furer, P., & Reynolds, K. (2015). Overcoming anxiety in pregnancy and Postpartum. Unpublished treatment manual. Winnipeg, MB: University of Manitoba.
Furer, P., Alcolado, G., Reynolds, K. & Hebert, E. A. (2021). Group cognitive-behavioural therapy for perinatal anxiety disorders: Treatment development, content, and pilot results. Journal of Affective Disorder Reports, 6, 100195. https://doi.org/10.1016/j.jadr.2021.100195
Glasheen, C., Richardson, G. A., & Fabio, A. (2010). A systematic review of the effects of postnatal maternal anxiety on children. Archives of Women’s Mental Health, 13(1), 61–74. https://doi.org/10.1007/s00737-009-0109-y
Goodman, J. H., Watson, G. R., & Stubbs, B. (2016). Anxiety disorders in postpartum women: A systematic review and meta-analysis. Journal of Affective Disorders, 203, 292–331. https://doi.org/10.1016/j.jad.2016.05.033
Green, S. M., Harber, E., Frey, B. N., & McCabe, R. E. (2015). Cognitive-behavioral group treatment for perinatal anxiety: A pilot study. Archives of Women’s Health, 18, 631–638. https://doi.org/10.1007/s00737-015-0498
Green, S., Donegan, E., Mccabe, R., Streiner, D., Agako, A., & Frey, B. (2020). Cognitive behavioral therapy for perinatal anxiety: A randomized controlled trial. The Australian and New Zealand Journal of Psychiatry, 54, 423–432. https://doi.org/10.1177/0004867419898528
Hadjistavropoulos, H. D., Pugh, N. E., Hesser, H., & Andersson, G. (2016). Predicting response to therapist-assisted internet-delivered cognitive behavior therapy for depression and anxiety within an open dissemination trial. Behavior Therapy, 47, 155–165.
Haga, S. M., Drozd, F., Lisoy, C., Wentzel-Larsen, T., & Slinning, K. (2019). Mamma Mia – A randomized controlled trial of an internet-based intervention for perinatal depression. Psychological Medicine, 49, 1850–1858. https://doi.org/10.1017/S0033291718002544
Harison, V., Moore, D., & Lazard, L. (2020). Supporting perinatal anxiety in the digital age: A qualitative exploration of stressors and support strategies. BMC Pregnancy and Childbirth, 20, 363. https://doi.org/10.1186/s12884-020-02990-0
Issakidis, C., & Andrews, G. (2004). Pretreatment attrition and dropout in an outpatient clinic for anxiety disorders. Acta Psychiatrica Scandinavica, 109, 426–433.
Kampman, M., Keijsers, G. P. J., Hoogduin, C. A. L., & Hendriks, G. (2008). Outcome prediction of cognitive behaviour therapy for panic disorder: Initial symptom severity is predictive for treatment outcome, comorbid anxiety or depressive disorder, cluster C personality disorders and initial motivation are not. Behavioural and Cognitive Psychotherapy, 36, 99–112. https://doi.org/10.1017/S1352465807004018
Li, X., Laplante, D. P., Paquin, V., Lafortune, S., Elgbeili, G., & King, S. (2022). Effectiveness of cognitive behavioral therapy for perinatal maternal depression, anxiety and stress: A systematic review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 92, 102129–102129. https://doi.org/10.1016/j.cpr.2022.102129
Maguire, P. N., Clark, G. I., & Wootton, B. M. (2018). The efficacy of cognitive behavior therapy for the treatment of perinatal anxiety symptoms: A preliminary meta-analysis. Journal of Anxiety Disorders, 60, 26–34. https://doi.org/10.1016/j.janxdis.2018.10.002
Morey, E., Thacher, J. A., & Craighead, W. E. (2007). Patient preferences for depression treatment programs and willingness to pay for treatment. Journal of Mental Health Policy and Economics, 10, 73–85.
Newby, J. M., McKinnon, A., Kuyken, W., Gilbody, S., & Dalgleish, T. (2015). Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clinical Psychology Review, 40, 91–110. https://doi.org/10.1016/j.cpr.2015.06.002
O’Hara, M. W., & Wisner, K. L. (2014). Perinatal mental illness: Definition, description and aetiology. Best Practice & Research Clinical Obstetrics & Gynaecology, 28, 3–12. https://doi.org/10.1016/j.bpobgyn.2013.09.002
Olatunji, B. O., Kauffman, B. Y., Meltzer, S., Davis, M. L., Smits, J. A. J., & Powers, M. B. (2014). Cognitive-behavioral therapy for hypochondriasis/health anxiety: A meta-analysis of treatment outcomes and moderators. Behaviour Research and Therapy, 58, 65–74. https://doi.org/10.1016/j.brat.2014.05.002
Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues in Clinical Neuroscience, 13(4), 413.
Paul, I. M., Downs, D. S., Schaefer, E. W., Beiler, J. S., & Weisman, C. S. (2013). Postpartum anxiety and maternal-infant health outcomes. Pediatrics, 131, e1218–e1224.
Paulus, D. J., Hayes-Skelton, & Norton, P. J. (2015). There’s no “I” in GCBT: Identifying predictors of a group-level outcome in transdiagnostic group cognitive-behavioral therapy for anxiety. Group Dynamics: Theory Research and Practice, 19(2), 63–76. https://doi.org/10.1037/gdn0000023
Piacentini, J., Bergman, R. L., Jacobs, C., McCracken, J. T., & Kretchman, J. (2002). Open trial of cognitive behavior therapy for childhood obsessive-compulsive disorder. Journal of Anxiety Disorders, 16, 207–219. https://doi.org/10.1016/S0887-6185(02)00096-8
Poulin, L. E., Button, M. L., Westra, H. A., Constantino, M. J., & Antony, M. M. (2018). The predictive capacity of self-reported motivation vs. early observed motivational language in cognitive behavioural therapy group for generalized anxiety disorder. Cognitive Behaviour Therapy, 48(5), 369–384. https://doi.org/10.1080/16506073.2018.1517390
R Core Team (2007). R: A Language and Environment for Statistical Computing.
Rief, W., Trenkamp, S., Auer, C., & Ficther, M. M. (2000). Cognitive behavior therapy in panic disorder and comorbid major depression. Psychotherapy and Psychosomatics, 69, 70–78. https://doi.org/10.1159/000012369
Schuurmans, J., Comijs, H., Emmelkamp, P. M., Weijnen, I. J., van den Hout, M., & van Dyck, R. (2009). Long-term effectiveness and prediction of treatment outcome in cognitive behavioral therapy and sertraline for late-life anxiety disorders. International Psychogeriatrics, 21, 1148–1159. https://doi.org/10.1017/S1041610209990536
Sockol, L. E. (2018). A systematic review and meta-analysis of interpersonal psychotherapy for perinatal women. Journal of Affective Disorders, 232, 316–328. https://doi.org/10.1016/j.jad.2018.01.018
Somerville, S., Dedman, K., Hagan, R., Oxnam, E., Wettinger, M., Byrne, S., Coo, S., Doherty, D., & Page, A. C. (2014). The perinatal anxiety screening scale: Development and preliminary validation. Archives of Women’s Mental Health, 17, 443–454. https://doi.org/10.1007/s00737-014-0425-8
Steketee, G., Chambless, D. L., & Tran, G. Q. (2001). Effects of Axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Comprehensive Psychiatry, 42, 76–86. https://doi.org/10.1053/comp.2001.19746
Titov, N., Dear, B., Staples, L., Terides, M., Karin, E., Sheehan, J., & McEvoy, P. (2015). Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: A randomized controlled trial. Journal of Anxiety Disorders, 35, 88–102. https://doi.org/10.1016/j.janxdis.2015.08.002
van Balkom, A. J., van Boeijen, C. A., Boeke, A. J. P., van Oppen, P., Kempe, P. T., & van Dyck, R. (2008). Comorbid depression, but not comorbid anxiety disorders, predicts poor outcome in anxiety disorders. Depression and Anxiety, 25, 408–415. https://doi.org/10.1002/da.20386
Watanabe, N., Furukawa, T. A., Chen, J., Kinoshita, Y., Nakano, Y., Ogawa, S., & Noda, Y. (2010). Change in quality of life and their predictors in the long-term follow-up after group cognitive behavioral therapy for social anxiety disorder: A prospective cohort study. Bmc Psychiatry, 10, 81–91. https://doi.org/10.1186/1471-244X-10-81
Author information
Authors and Affiliations
Contributions
All authors have contributed to multiple aspects of the study and approved the final manuscript.
All authors certify responsibility for this study and that neither the whole article or any essential part thereof will be published or submitted anywhere else prior to appearing in Current Psychology.
Corresponding author
Ethics declarations
Ethical approval
for this study was obtained from our local university and hospital Human Research Ethics Boards of the University of Manitoba (#HS20183) and the Research Review Committee of St. Boniface Hospital (#RRC/2016/1624). The study was based entirely on analyses of retrospective data obtained from medical records. As such, the boards waived the need to obtain informed consent.
Conflicts of interest
There are no known conflicts of interest related to this study. There was no funding received for this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kinsman, L., Bilevicius, E., Shamblaw, A.L. et al. Group cognitive-behavioral therapy for perinatal anxiety: predictors of completion and response. Curr Psychol 43, 5419–5427 (2024). https://doi.org/10.1007/s12144-023-04723-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-04723-w