Abstract
We examined the association between depression symptoms and job stress based on the Demand–Control–Support model among workers employed in Japanese eldercare institutions. We randomly selected 197 eldercare institutions and invited workers to participate in a questionnaire survey. Depression symptom prevalence and severity were evaluated using the Center for Epidemiologic Studies Depression (CES-D) Scale (≥ 16 = high score). Job stress was assessed using the Job Content Questionnaire based on job Demand–Control–Support. A total of 2,727 workers agreed to participate. In total, 1,740 valid responses were obtained from 434 males and 1,306 females. Approximately 44.9% had high CES-D scores. Workers with long working hours had high and low scores of psychological job demand and social support, respectively. Those who exhibited high CES-D scores had significantly higher psychological job demand scores and lower decision latitude and social support scores. A positive correlation was found between psychological job demand and CES-D scores. By contrast, a negative correlation was found between decision latitude and CES-D scores and between the social support scores and CES-D scores. Employers and employees should be mindful of the risks associated with prolonged work hours to prevent depression. Moreover, special attention should be paid to workers with substantial psychological job demands, low decision latitude, and low social support, as these workers constitute a high-risk group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent years have seen rapid increases in work complexity (Jalilian et al., 2019; Karasek & Theorell, 1992), with workers across myriad settings—particularly healthcare—having to learn numerous complex procedures, resulting in increased job demands and strain. This rapid increase in job demands and strain, particularly among healthcare workers, can cause health issues; reduced productivity; and increased errors (e.g., medical errors), costs, and job turnover (Hayes et al., 2012; Jalilian et al., 2019; Saremi & Fallah, 2013; Thirumakkal, 2015). Stress-related problems in care-service workers have increased (Fushimi, 2019; Suzumura et al., 2013; Tanaka et al., 2017; Yiengprugsawan et al., 2016); these workers tend to experience greater mental and physical burdens than those in other industries (Fushimi, 2019; Honda et al., 2014; Suzumura et al., 2013). Providing care is stressful as these jobs require teamwork; prolonged social contact; and maintaining relationships with patients, their families, and other medical and social workers (Fushimi, 2019; Margallo-Lana et al., 2001; Teraoka & Kyougoku, 2015). Job turnover rates are generally high, and care provider workplaces are usually understaffed (Fushimi, 2019; Suzumura et al., 2013; Tanaka et al., 2017; Varela et al., 2011), leading to various workplace issues in care-service facilities (Fushimi, 2019; Schneider et al., 2013; Teraoka & Kyougoku, 2015; Yiengprugsawan et al., 2016). Care providers, therefore, often experience physical and mental health problems (Fushimi, 2019; Honda et al., 2014; Joling et al., 2012; Suzumura et al., 2013; Varela et al., 2011; Ying et al., 2018).
Care providers should be aware of these work-related health issues and practice stress-relief techniques when possible. These providers should also receive guidance and training to improve long-term retention rates (Fushimi, 2019; Honda et al., 2014; Li et al., 2015; Varela et al., 2011; Yiengprugsawan et al., 2016).
Job stress is a crucial health and safety issue for workers in many work environments (Jalilian et al., 2019; Moustaka & Constantinidis, 2010; Peltzer et al., 2009). Factors like social support, psychological job demands, and decision control are related to job stress (Jalilian et al., 2019; Nieuwenhuijsen et al., 2010) and are considered vital in Karasek’s job Demand–Control–Support model, which hypothesizes that the combination of high job demands and low social support and decision latitude causes job stress (Häusser et al., 2010; Jalilian et al., 2019; Karasek et al., 1998). Job stress due to increased job demands can cause physical and mental health problems (Jalilian et al., 2019; Moustaka & Constantinidis, 2010) and can be created and exacerbated by a substandard working environment. This stress adversely affects workers’ health and lives (Arsalani et al., 2014; Jalilian et al., 2019; Menzel, 2007). Previous studies have attempted to measure worker stress levels (Jalilian et al., 2019; Johnson et al., 2005).
Depression, a common mental disorder, is a significant public health concern (Eaton et al., 2008; Fushimi, 2019; Virtanen et al., 2012). Few studies have evaluated the association of job stress with depressive symptoms among workers employed in Japanese eldercare institutions. By contrast, studies on healthcare staff in other countries and in-home care providers have been conducted.
In developed nations such as Japan, population aging and increased life expectancy have similarly increased the demand for elderly care workers, who are presently in short supply (Damiani et al., 2011; Fujisawa & Colombo, 2009; Ikeda-Sonoda et al., 2020). In Japan, there are long wait lists for special nursing homes, partly due to labor shortages (Ikeda-Sonoda et al., 2020; Squires et al., 2015). In 2018, the effective ratio of care worker job vacancies to job applicants was more than 3.95 nationwide; 62.6% of care workers are employed full-time (Gospel, 2015; Ikeda-Sonoda et al., 2020). Changes to the social welfare system in Japan have led to new facility service estimates for the year 2025 (Nishino, 2017; Tsuno & Honma, 2009). We estimate that, by 2025, an additional 550,000 workers will be needed to ensure quality care and contain costs (Ikeda-Sonoda et al., 2020). Japan expects to see net increases in its elderly population (> 65 years) until 2042 (Nishino, 2017). Therefore, the Japanese government, nursing home administrators, and service providers must recruit and retain additional care workers.
The present study evaluated the factors that affected workers’ mental health in Japanese eldercare institutions. It investigated the association of job stress dimensions with depressive symptoms in these workers based on Karasek’s job Demand–Control–Support model. The Job Content Questionnaire (JCQ) was used to assess job stress, whereas the Center for Epidemiologic Studies Depression (CES-D) Scale was used to evaluate depressive symptoms. The present study results may help identify workers at a high risk of depression and detect the involvement of sociodemographic characteristics and work environment-associated factors concerning depressive symptoms.
Materials and methods
Participants
The data used in this study were generated partly for an occupational health study conducted by the Akita Occupational Health Promotion Center (Fushimi, 2019). The study survey was conducted among workers employed in eldercare institutions in the Akita Prefecture, Japan, from September–November 2015.
Institutions were selected using random sampling. All survey respondents were non-compensated volunteers who independently consented to participate. The Akita Occupational Health Comprehensive Support Center maintains a list of offices in the Akita Prefecture. The center staff carried out random sampling using this list. This study used the “systematic sampling (equal sampling interval method).” Here, the population is assigned a serial number, and the first sample is randomly selected from populations with lower serial numbers. We adopted a method of equal sampling intervals from that point. The included facilities support elderly people who live at home, receive daily care, and require long-term care and assistance, including excretion, feeding, bathing, managing their health and medical needs, and functional training. These facilities include group homes that support elderly people with dementia, assigned care workers and managers, and rehabilitation and recreational staff. The group homes include long- and short-term stay options, partial-day services, and visiting nurses. Information was collected regarding the employees’ sociodemographic and occupational characteristics, including sex, full-time vs. part-time work status, managerial vs. nonmanagerial work, and mean hours worked per week. The board of research ethics of the Japan Labor Health and Welfare Organization approved the study protocol. Before obtaining consent, the study protocol was explained to the participants. All survey responses were anonymized.
Instruments
To determine depression symptom prevalence and severity, the CES-D, a self-reported depression scale (Vilagut et al., 2016; Ying et al., 2019) with good reliability and validity in varied populations, was used (Fushimi et al., 2013; Radloff, 1977; Vilagut et al., 2016; Ying et al., 2019). The Japanese version of CES-D has satisfactory reliability and validity in the general Japanese population (Fushimi, 2019; Iwata et al., 1989) for measuring depressive symptoms experienced over the preceding week. There are 20 items in CES-D, which are answered using a 4-point scale (range: 0, rarely or none of the time to 3, most or all of the time). CES-D scores ≥ 16 represent “probable” depression (Fushimi, 2015; Fushimi et al., 2013; Ying et al., 2018). Thus, 16 was used as a cutoff for depression in this study.
Based on the job Demand-Control–Support Model (shortened JCQ version, adapted from the full JCQ, including 22 items across three separate dimensions), was used to evaluate job stress (Karasek et al., 1998; Kataoka et al., 2021; Kawakami et al., 1995). The following dimensions were included in the study: psychological job demands (5 items), decision latitude or control (9 items), and social support (8 items; Table 1). A 4-point scale (range 1, strongly disagree to 4, strongly agree) was used for JCQ. The “JCQ User’s Guide” was used to calculate JCQ subcategory scores, i.e., psychological demands, decision latitude = skill discretion + decision authority, and social support = supervisor support + coworker support (Table 2; Karasek, 1985). The Japanese version of JCQ is considered reliable and valid (Kataoka et al., 2021; Kawakami et al., 1995).
Statistical analyses
All data were analyzed using SPSS version 11.0 J for Windows (SPSS, Tokyo, Japan). The Mann–Whitney U test was used to evaluate differences in the JCQ scores according to sociodemographic characteristics, work hours per week, and CES-D scores. The JCQ subcategory and CES-D scores were compared using Spearman’s correlation coefficients.
Results
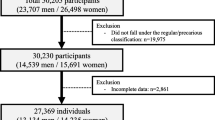
There were 197 public and private care institutions that participated in the study. The survey was voluntary, paper-based, and included only de-identified personal information. In total, 2,727 workers were encouraged to participate; of these, 2,404 completed the survey (response rate = 88.2%) and valid responses were 1,740 (males, 434; females, 1,306). Table 3 shows the participant demographics (n = 1,740). Of the 236 workers who worked more than 45 h per week, 33 were considered managerial class, accounting for 14.0% of the total. Of the 1,504 employees who worked fewer than 45 h per week, 138 (9.2%) were in the managerial class. This result was added to the table’s explanation. Table 4 shows the mean and standard deviation of the JCQ scores for each category and the differences among each JCQ category. Male workers scored significantly higher on the decision latitude (P ≤ 0.05), particularly in the skill discretion subscore (P ≤ 0.01), than female workers. Full-time workers scored significantly higher on psychological demands (P ≤ 0.01) and decision latitudes (P ≤ 0.01) than part-time workers. Part-time workers scored significantly higher on social support (P ≤ 0.01), particularly supervisor support (P ≤ 0.01), than full-time workers. The managerial class scored significantly higher on the decision latitude (P ≤ 0.01) than the nonmanagerial class. Workers with long working hours had significantly higher psychological demands (P ≤ 0.01) and lower social support scores (P ≤ 0.01), whereas those with high CES-D scores had significantly higher psychological demands (P ≤ 0.01) and lower decision latitude (P ≤ 0.01) and social support scores (P ≤ 0.01).
Table 5 shows the correlation between the JCQ and CES-D scores. A significant positive correlation was observed between the JCQ psychological job demands score and the CES-D score (P ≤ 0.01). A significant negative correlation was observed between decision latitude and the CES-D score (P ≤ 0.01). Moreover, social support and the CES-D score were negatively correlated (P ≤ 0.01).
Discussion
The present study results support the development of techniques to improve mental health in eldercare workers. Our results are consistent with previous studies' results (Fushimi, 2019; Tanaka et al., 2017). The significantly higher scores of the full-time workers on social support—particularly supervisor support— indicate that full-time workers (often supervisors) often instruct part-time subordinates in actual care provider settings. The managerial class scored significantly higher on decision latitude than the nonmanagerial class, which appears to reflect the general character of work in the managerial class. Managers exhibit lower depression scores and appear better able to adjust to social and environmental changes and control work-related stress than non-managers (Fushimi, 2015; Fushimi et al., 2013). Furthermore, managerial positions are not associated with psychological stress (Fushimi, 2019; Fushimi et al., 2010; Fushimi et al., 2012).
Workers with long working hours had significantly higher psychological demands and lower social support scores, consistent with previous studies’ results (Fushimi, 2019; Kataoka et al., 2021). An important indicator of psychological stress is the time spent at work (Fushimi, 2019; Virtanen et al., 2012). High work demands and overtime pressure adversely impact mental well-being, and longer working hours cause negative work-to-family spillover, increasing depression risk (D’Souza et al., 2006; Fushimi et al., 2013; Iwata et al., 1989). However, to manage excessive workloads, some employees must work longer hours (Hilton et al., 2008). Long work hours are associated with overwork and increase the risk of depression in workers (Virtanen et al., 2012). The present study results revealed that the increased risk of depression is also applicable to care providers.
In the present study, significantly higher psychological demands, as well as lower decision latitude and social support, were observed in workers with high CES-D scores, which was similar to the results of previous studies (Fushimi, 2019; Jalilian et al., 2019; Kataoka et al., 2021; Tanaka et al., 2017).
Workers with high depression scores on the CES-D had low decision latitude (control). To improve mental health, we must expand decision latitude (i.e., increase control), decrease work demand, decrease overtime, and enhance social support to promote mental health.
The significant positive correlation between the JCQ psychological job demand and CES-D scores, in addition to the negative correlation between the decision latitude (control) score and CES-D scores and between the social support and CES-D scores, is also consistent with previous results (Fushimi, 2019; Jalilian et al., 2019; Kataoka et al., 2021; Tanaka et al., 2017). These variables are, therefore, highly reproducible.
Research has shown fatigue is caused by high job demand and low decision latitude (Jalilian et al., 2019; Van Yperen & Hagedoorn, 2003). In jobs with increased stress and demands along with low decision latitude, depression can be more apparent compared with jobs with both high demands and decision latitude. Moreover, job stress effects can be more obvious when social support is low. In this case, care providers are no exception, given their major responsibility for the lives of their customers. By contrast, if care workers are given more decision-making control and social support, they will be more motivated to perform their duties, thereby increasing their physical activity at work and improving their morale. Based on these results, preventing the onset of depressive symptoms might be possible; however, further studies are required for clarification.
Hospital populations also age in an aging society. Thus, by reducing stays or preventing readmissions, the additional need for hospital capacity can be reduced (Van den Heede et al., 2019; Holst Pedersen et al., 2018). To achieve this, the demand for care services is expected to increase, thereby increasing the difficulty of securing qualified workers and subsequently increasing the burden on existing workers (Suzumura et al., 2013; Yiengprugsawan et al., 2016). This increased burden may cause physical and mental problems. Japan’s population is aging, and the number of people requiring care is increasing, thereby increasing the demand for care workers (Fushimi, 2019), resulting in increased health problems for care providers (Fushimi, 2019; Kaneko et al., 2008).
Various factors increase job stress: customer safety, substantial workload, poor working conditions, low pay, and minimal experience in providing care. The undesirable effects on care workers’ physical and psychological health due to job stress can subsequently affect their efficiency and customer safety (e.g., medical errors caused by healthcare workers) (Jalilian et al., 2019; Saremi & Fallah, 2013).
Although numerous studies have focused on these health problems arising from home-based health support (Chan et al., 2013; Honda et al., 2014; Oshio, 2014; Schneider et al., 2013; Yiengprugsawan et al., 2016), few have examined this relationship in workers employed in care-service facilities (Fushimi, 2019; Margallo-Lana et al., 2001). Numerous surveys have been conducted among in-home caregivers; however, few have evaluated caregivers in facilities, as in our study (Fushimi, 2019), which surveyed many workers. As country-specific legal systems for care services and work environments vary, care providers’ mental and physical health status cannot be easily compared internationally. However, this issue must be compared and examined using numerous reports published worldwide. Moreover, additional studies are needed to elucidate the work-related conditions of workers in care facilities in addition to the factors that affect these conditions.
There is a need to hire care workers and retain current providers. Therefore, workplace health management for care workers is important, as is mental healthcare. Considering the effects of job stress on such workers, a suitable interventional program must be developed to decrease job stress. The present study results can provide a starting point for measures designed to reduce care providers’ physical and mental burdens. Moreover, we believe that the present study data can act as a solution to address these issues in Japanese care-service facilities.
The cross-sectional design is a study limitation as we could not determine whether the associations of sociodemographic characteristics with the symptoms of depression were antecedents or consequences of depression. In addition, we restricted our study to only care-service workers and did not include all workers. The study’s results should be interpreted with caution owing to the self-reported method of data collection and cross-sectional design of the study, as such a study has several drawbacks, including recall bias, denial, and deception. However, we attempted to compensate for these shortcomings by including a large sample.
Conclusion
This study examined the association of depressive symptoms with job Demand–Control–Support among workers employed in Japanese eldercare institutions. The results suggest that higher psychological job demands are correlated with lower decision latitude. A lack of social support is correlated with a greater risk of depression. The observed impact of job stress based on the job Demand–Control–Support model highlights the need to identify workers at a high risk of depression and reduce their risk within each aspect of psychological job demands, decision latitude, and social support.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Arsalani, N., Fallahi-Khoshknab, M., Josephson, M., & Lagerström, M. (2014). Musculoskeletal disorders and working conditions among Iranian nursing personnel. International Journal of Occupational Safety and Ergonomics, 20(4), 671–680. https://doi.org/10.1080/10803548.2014.11077073
Chan, A., Malhotra, C., Malhotra, R., Rush, A. J., & Østbye, T. (2013). Health impacts of caregiving for older adults with functional limitations: Results from the Singapore survey on informal caregiving. Journal of Aging and Health, 25(6), 998–1012. https://doi.org/10.1177/0898264313494801
Damiani, G., Farelli, V., Anselmi, A., Sicuro, L., Solipaca, A., Burgio, A., Iezzi, D. F., & Ricciardi, W. (2011). Patterns of long term care in 29 European countries: Evidence from an exploratory study. BMC Health Services Research, 11, 316. https://doi.org/10.1186/1472-6963-11-316
D’Souza, R. M., Strazdins, L., Broom, D. H., Rodgers, B., & Berry, H. L. (2006). Work demands, job insecurity and sickness absence from work. How productive is the new, flexible labour force? Australian and New Zealand Journal of Public Health, 30(3), 205–212. https://doi.org/10.1111/j.1467-842x.2006.tb00859.x
Eaton, W. W., Martins, S. S., Nestadt, G., Bienvenu, O. J., Clarke, D., & Alexandre, P. (2008). The burden of mental disorders. Epidemiologic Reviews, 30, 1–14. https://doi.org/10.1093/epirev/mxn011
Fujisawa, R., & Colombo, F. (2009). The long-term care workforce: overview and strategies to adapt supply to a growing demand. OECD Health Working Papers No.44. https://doi.org/10.1787/225350638472
Fushimi, M. (2015). Prevalence of depressive symptoms and related factors in Japanese employees: A comparative study between surveys from 2007 and 2010. Psychiatry Journal, 2015, 537073. https://doi.org/10.1155/2015/537073
Fushimi, M. (2019). Depressive symptoms and related factors among workers in care institutions for older persons in Japan: A cross-sectional study. European Geriatric Medicine, 10(6), 957–964. https://doi.org/10.1007/s41999-019-00241-w
Fushimi, M., Shimizu, T., Saito, S., Kudo, Y., Seki, M., & Murata, K. (2010). Prevalence of and risk factors for psychological distress among employees in Japan. Public Health, 124(12), 713–715. https://doi.org/10.1016/j.puhe.2010.07.010
Fushimi, M., Saito, S., Shimizu, T., Kudo, Y., Seki, M., & Murata, K. (2012). Prevalence of psychological distress, as measured by the Kessler 6 (K6), and related factors in Japanese employees. Community Mental Health Journal, 48(3), 328–335. https://doi.org/10.1007/s10597-011-9416-7
Fushimi, M., Saito, S., & Shimizu, T. (2013). Prevalence of depressive symptoms and related factors in Japanese employees as measured by the Center for Epidemiologic Studies Depression Scale (CES-D). Community Mental Health Journal, 49(2), 236–242. https://doi.org/10.1007/s10597-012-9542-x
Gospel, H. (2015). Varieties of qualifications, training, and skills in long-term care: A German, Japanese, and UK comparison. Human Resource Management, 54(5), 833–850. https://doi.org/10.1002/hrm.21714
Häusser, J. A., Mojzisch, A., Niesel, M., & Schulz-Hardt, S. (2010). Ten years on: A review of recent research on the job demand—Control (-Support) model and psychological well-being. Work and Stress, 24(1), 1–35. https://doi.org/10.1080/02678371003683747
Hayes, L. J., O’Brien-Pallas, L., Duffield, C., Shamian, J., Buchan, J., Hughes, F., Laschinger, H. K., & North, N. (2012). Nurse turnover: A literature review—An update. International Journal of Nursing Studies, 49(7), 887–905. https://doi.org/10.1016/j.ijnurstu.2011.10.001
Hilton, M. F., Whiteford, H. A., Sheridan, J. S., Cleary, C. M., Chant, D. C., Wang, P. S., & Kessler, R. C. (2008). The prevalence of psychological distress in employees and associated occupational risk factors. Journal of Occupational and Environmental Medicine, 50(7), 746–757. https://doi.org/10.1097/JOM.0b013e31817e9171
Holst Pedersen, L. H., Brynningsen, P., Foss, C. H., Gregersen, M., Barat, I., & Damsgaard, E. M. (2018). Avoidable readmissions seem to be reduced by early follow-up visits for geriatric patients discharged from hospital. European Geriatric Medicine, 9(5), 613–621. https://doi.org/10.1007/s41999-018-0078-7
Honda, A., Date, Y., Abe, Y., Aoyagi, K., & Honda, S. (2014). Work-related stress, caregiver role, and depressive symptoms among Japanese workers. Safety and Health at Work, 5(1), 7–12. https://doi.org/10.1016/j.shaw.2013.11.002
Ikeda-Sonoda, S., Ichihara, N., Okochi, J., Takahashi, A., & Miyata, H. (2020). Association of care workers’ job satisfaction and global happiness with change of functional performance of severely disabled elderly residents in nursing homes: A cohort and questionnaire study in Japan. British Medical Journal Open, 10(10), e033937. https://doi.org/10.1136/bmjopen-2019-033937
Iwata, N., Okuyama, Y., Kawakami, Y., & Saito, K. (1989). Prevalence of depressive symptoms in a Japanese occupational setting: A preliminary study. American Journal of Public Health, 79(11), 1486–1489. https://doi.org/10.2105/ajph.79.11.1486
Jalilian, H., Shouroki, F. K., Azmoon, H., Rostamabadi, A., & Choobineh, A. (2019). Relationship between job stress and fatigue based on job demand-control-support model in hospital nurses. International Journal of Preventive Medicine, 10, 56. https://doi.org/10.4103/ijpvm.IJPVM_178_17
Johnson, S., Cooper, C., Cartwright, S., Donald, I., Taylor, P., & Millet, C. (2005). The experience of work-related stress across occupations. Journal of Managerial Psychology, 20(2), 178–187. https://doi.org/10.1108/02683940510579803
Joling, K. J., Smit, F., van Marwijk, H. W., van der Horst, H. E., Scheltens, P., Schulz, R., & van Hout, H. P. (2012). Identifying target groups for the prevention of depression among caregivers of dementia patients. International Psychogeriatrics, 24(2), 298–306. https://doi.org/10.1017/S1041610211001633
Kaneko, R., Ishikawa, A., Ishii, F., Sasai, T., Iwasawa, M., Mita, F., & Moriizumi, R. (2008). Population projections for Japan: 2006–2055 Outline of results, methods, and assumptions. The Japanese Journal of Population, 6(1), 76–114.
Karasek, R. A. (1985). Job content questionnaire and User’s guide. University of Massachusetts.
Karasek, R., & Theorell, T. (1992). Healthy work: Stress, productivity, and the reconstruction of working life. Basic Books.
Karasek, R., Brisson, C., Kawakami, N., Houtman, I., Bongers, P., & Amick, B. (1998). The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. Journal of Occupational Health Psychology, 3(4), 322–355. https://doi.org/10.1037//1076-8998.3.4.322
Kataoka, S., Kitamura, K., Kataoka, Y., & Yamamoto, Y. (2021). Depressive symptoms and their associated factors in nursery school teachers: A multicenter cross-sectional study. Cureus, 13(7), e16545. https://doi.org/10.7759/cureus.16545
Kawakami, N., Kobayashi, F., Araki, S., Haratani, T., & Furui, H. (1995). Assessment of job stress dimensions based on the job demands- control model of employees of telecommunication and electric power companies in Japan: Reliability and validity of the Japanese version of the Job Content Questionnaire. International Journal of Behavioral Medicine, 2(4), 358–375. https://doi.org/10.1207/s15327558ijbm0204_5
Li, A., Shaffer, J., & Bagger, J. (2015). The psychological well-being of disability caregivers: Examining the roles of family strain, family-to-work conflict, and perceived supervisor support. Journal of Occupational Health Psychology, 20(1), 40–49. https://doi.org/10.1037/a0037878
Margallo-Lana, M., Reichelt, K., Hayes, P., Lee, L., Fossey, J., O’Brien, J., & Ballard, C. (2001). Longitudinal comparison of depression, coping, and turnover among NHS and private sector staff caring for people with dementia. BMJ, 322(7289), 769–770. https://doi.org/10.1136/bmj.322.7289.769
Menzel, N. N. (2007). Psychosocial factors in musculoskeletal disorders. Critical Care Nursing Clinics of North America, 19(2), 145–153. https://doi.org/10.1016/j.ccell.2007.02.006
Moustaka, A., & Constantinidis, T. C. (2010). Sources and effects of work-related stress in nursing. Health Science Journal, 4, 210–216.
Nieuwenhuijsen, K., Bruinvels, D., & Frings-Dresen, M. (2010). Psychosocial work environment and stress-related disorders, a systematic review. Occupational Medicine, 60(4), 277–286. https://doi.org/10.1093/occmed/kqq081
Nishino, T. (2017). Quantitative properties of the macro supply and demand structure for care facilities for elderly in Japan. International Journal of Environmental Research and Public Health, 14(12), 1489. https://doi.org/10.3390/ijerph14121489
Oshio, T. (2014). The association between involvement in family caregiving and mental health among middle-aged adults in Japan. Social Science and Medicine, 115, 121–129. https://doi.org/10.1016/j.socscimed.2014.06.016
Peltzer, K., Shisana, O., Zuma, K., Van Wyk, B., & Zungu-Dirwayi, N. (2009). Job stress, job satisfaction and stress-related illnesses among South African educators. Stress and Health, 25(3), 247–257. https://doi.org/10.1002/smi.1244
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
Saremi, M., & Fallah, M. R. (2013). Subjective fatigue and medical errors among nurses in an educational hospital. Iran Occupational Health, 10, 1–8.
Schneider, U., Trukeschitz, B., Mühlmann, R., & Ponocny, I. (2013). ‘Do I stay or do I go?’—Job change and labor market exit intentions of employees providing informal care to older adults. Health Economics, 22(10), 1230–1249. https://doi.org/10.1002/hec.2880
Squires, J. E., Hoben, M., Linklater, S., Carleton, H. L., Graham, N., & Estabrooks, C. A. (2015). Job satisfaction among care aides in residential long-term care: A systematic review of contributing factors, both individual and organizational. Nursing Research and Practice, 1–24. https://doi.org/10.1155/2015/157924
Suzumura, M., Fushiki, Y., Kobayashi, K., Oura, A., Suzumura, S., Yamashita, M., & Mori, M. (2013). A cross-sectional study on association of work environment, coping style, and other risk factors with depression among caregivers in group homes in Japan. Industrial Health, 51(4), 417–423. https://doi.org/10.2486/indhealth.2012-0204
Tanaka, O., Maeda, E., Fushimi, M., Iwata, T., Shimizu, T., Saito, S., & Murata, K. (2017). Precarious employment is not associated with increased depressive symptoms: A cross-sectional study in care service workers of Japan. Tohoku Journal of Experimental Medicine, 243(1), 19–26. https://doi.org/10.1620/tjem.243.19
Teraoka, M., & Kyougoku, M. (2015). Analysis of structural relationship among the occupational dysfunction on the psychological problem in healthcare workers: A study using structural equation modeling. PeerJ, 3(3), e1389. https://doi.org/10.7717/peerj.1389
Thirumakkal, M. (2015). A study on role of occupational stress on employees productivity. International Journal of Management, 6, 560–572.
Tsuno, N., & Honma, A. (2009). Ageing in Asia—the Japan experience. Ageing International, 34, 1–14. https://doi.org/10.1007/s12126-009-9032-9
Van den Heede, K., Bouckaert, N., & Van de Voorde, C. (2019). The impact of an ageing population on the required hospital capacity: Results from forecast analysis on administrative data. European Geriatric Medicine, 10(5), 697–705. https://doi.org/10.1007/s41999-019-00219-8
Van Yperen, N. W., & Hagedoorn, M. (2003). Do high job demands increase intrinsic motivation or fatigue or both? The role of job control and job social support. Academy of Management Journal, 46, 339–348.
Varela, G., Varona, L., Anderson, K., & Sansoni, J. (2011). Alzheimer’s care at home: A focus on caregivers strain. Professioni Infermieristiche, 64(2), 113–117.
Vilagut, G., Forero, C. G., Barbaglia, G., & Alonso, J. (2016). Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): A systematic review with meta-analysis. PLoS ONE, 11(5), e0155431. https://doi.org/10.1371/journal.pone.0155431
Virtanen, M., Stansfeld, S. A., Fuhrer, R., Ferrie, J. E., & Kivimäki, M. (2012). Overtime work as a predictor of major depressive episode: A 5-year follow-up of the Whitehall II study. PLoS ONE, 7(1), e30719. https://doi.org/10.1371/journal.pone.0030719
Yiengprugsawan, V., Leach, L., Berecki-Gisolf, J., Kendig, H., Harley, D., Seubsman, S. A., & Sleigh, A. C. (2016). Caregiving and mental health among workers: Longitudinal evidence from a large cohort of adults in Thailand. SSM – Population Health, 2, 149–154. https://doi.org/10.1016/j.ssmph.2016.01.004
Ying, J., Yap, P., Gandhi, M., & Liew, T. M. (2018). Iterating a framework for the prevention of caregiver depression in dementia: A multi-method approach. International Psychogeriatrics, 30(8), 1119–1130. https://doi.org/10.1017/S1041610217002629
Ying, J., Yap, P., Gandhi, M., & Liew, T. M. (2019). Validity and utility of the Center for Epidemiological Studies Depression Scale for detecting depression in family caregivers of persons with dementia. Dementia and Geriatric Cognitive Disorders, 15, 1–12.
Acknowledgements
The author would like to thank the participants for their contribution to the study, as well as Seiji Saito, Tetsuo Shimizu, Katsuyuki Murata, Yasutsugu Kudo, Tomokazu Asanuma, Masayuki Seki, and all the occupational physicians and their assistants from the Akita Occupational Health Promotion Centers for their help during the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Board at the Japan Labor Health and Welfare Organization.
Consent to participate
All individual participants provided consent after they were informed that participation in the paper-based survey was voluntary and confidential.
Conflicts of interest
The author has no conflicts of interest to declare regarding the publication of this paper.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fushimi, M. Factors associated with depressive symptoms among workers employed in Japanese eldercare institutions: a cross-sectional study based on the Job Demand–Control–Support Model. Curr Psychol 42, 28953–28960 (2023). https://doi.org/10.1007/s12144-022-03971-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03971-6