Abstract
Background
BRCA1-associated protein 1 (BAP1) is a tumor suppressor gene that is altered in a variety of neoplasms as well as in BAP1 tumor predisposition syndrome. BAP1 alterations are associated with aggressive behavior in some malignancies and may have treatment implications in future. We present the first documented case of loss of BAP1 protein expression by immunohistochemistry in the salivary duct carcinoma (SDC) component of an intracapsular carcinoma ex pleomorphic adenoma (CXPA) in the context of molecular loss of function of BAP1 in the neoplasm.
Methods
A woman of approximately 55 years of age presented with a deep parotid lobe mass, which was resected and found to be CXPA. BAP1 immunohistochemistry and next-generation sequencing was performed to further characterize the neoplasm.
Results
The neoplasm showed loss of BAP1 protein expression in the SDC component but retention in the residual pleomorphic adenoma (PA). Next-generation sequencing confirmed a BAP1 loss of function alteration in the neoplasm.
Conclusion
This is the first documented case report of BAP1 protein expression loss in the SDC component of a CXPA. Future studies are needed to investigate the relevance of BAP1 alterations in SDC and CXPA, which may have prognostic and treatment implications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carcinoma ex pleomorphic adenoma (CXPA) represents the malignant transformation of a pleomorphic adenoma (PA), demonstrates predilection for the major salivary glands [1], and can further be classified as intracapsular, minimally invasive, or invasive based on the extent of invasion into surrounding tissues. Carcinomatous components most commonly include salivary duct carcinoma (SDC), myoepithelial carcinoma, and epithelial–myoepithelial carcinoma (EMC), among others [10, 25].
Reported molecular alterations in CXPA are varied. In addition to those alterations common to PA, such as rearrangements of PLAG1 and HMGA2, other molecular alterations include TP53, BRCA1, BRCA2, and EGFR [1, 5, 25]. However, to date there have been no reported cases of BRCA1-associated protein 1 (BAP1) in CXPA or SDC.
We present the first documented case of loss of BAP1 protein expression in a CXPA, which was limited to the SDC component of the neoplasm. A loss of function alteration of BAP1 was additionally demonstrated by next-generation sequencing, which has not been reported before in CXPA.
Case Report
The patient was a woman of approximately 55 years with no relevant past medical history who was found to have a rapidly enlarging mass of the deep parotid lobe. Resection of the lesion yielded a 4.5-cm, well-circumscribed, solid and cystic mass.
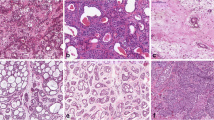
Histologic examination revealed an encapsulated, pleomorphic adenoma with a SDC that was positive for androgen receptor (AR, anti-androgen receptor, SP107, Rabbit monoclonal primary antibody, Cell Marque) (Fig. 1). No capsular, lymphovascular, or perineural invasion were present.
BAP1 immunohistochemistry (BAP1, anti-Bap1 mouse monoclonal antibody, sc-28283, Mayo Clinic Laboratories, Santa Cruz Biotechnology) showed BAP1 protein expression loss in the SDC portion of the neoplasm but retention in the residual PA (Fig. 2).
Next-generation sequencing (Tempus Laboratories, 648 gene panel) revealed a c.37+1G>A splice region variant loss of function alteration. Additionally present were the following alterations: PIK3CA gain of function, BRCA2 loss of function, NF1 loss of function, FANCA loss of function, androgen receptor overexpression, and FBXO32::PLAG1 chromosomal rearrangement. Material for germline testing was not available.
Due to the presence of intracapsular CXPA, a subsequent lymph node dissection was performed, and there were no lymph node metastases. The patient was referred to radiation oncology for additional treatment and has had no recurrence or disease progression at over one-year post-resection.
Discussion
BAP1 is a tumor suppressor gene located on chromosome 3p21.3 that functions as a deubiquitinating enzyme that interacts with the BRCA1 RING finger domain, among other proteins, and has roles in cell growth as well as genomic maintenance and stability [6, 7, 15, 17, 19, 22, 28]. BAP1 alterations are represented among many human neoplasms, including mesothelioma, cholangiocarcinoma, renal cell carcinoma, and melanoma [18]. A recent query of The Foundation Medicine database performed by Laitman and colleagues found BAP1 alterations in adenoid cystic carcinoma as well as 6.18% of salivary gland adenocarcinoma; however, the specific diagnostic type of salivary gland malignancy remained unspecified in the report [18]. One study found BAP1 alterations in 20.8% of mucoepidermoid carcinomas studied (n = 48) [26]; however, a second study of mucoepidermoid carcinomas found no such alterations (n = 40) [16].
The findings in the current case are unique because of the well-delineated loss of BAP1 protein expression by immunohistochemistry in the SDC component of the neoplasm with retention in the PA component of the neoplasm, a finding that suggests that BAP1 alterations may be relevant to SDCs arising in the setting of CXPA.
The identification of BAP1 alterations in other tumors has both prognostic and treatment implications. For example, somatic BAP1 inactivation has been implicated in metastatic potential in uveal melanoma [11] and is associated with an aggressive clinical course in high-grade meningiomas [24]. Germline BAP1 alterations cause BAP1 tumor predisposition syndrome, which predisposes patients to uveal and cutaneous melanomas, renal cell carcinoma, and mesothelioma [3, 20]; however, such a syndromic association with salivary gland neoplasms has not been reported. Finally, emerging studies suggest therapeutic strategies in BAP1-altered tumors, including platinum-based chemotherapies, such as cisplatin [13], and poly(ADP-ribose) polymerase (PARPI) inhibitors, such as niraparib and Olaparib [8, 12, 19].
Other alterations in this intracapsular CXPA are discussed as follows: PIK3CA alterations are reported in SDC [9, 23]. BRCA2 alterations are identified in a substantial number of PAs and CXPAs [14]. NF1 alterations are identified in SDC and adenocarcinoma, not otherwise specified, but not in CXPA in one study [27]. A FANCA mutation is reported in a SDC in a patient with a germline BRCA1 mutation [4]. AR expression is reported in many CXPA cases as well as approximately one-third of PAs in one limited study [21]. FBXO32::PLAG1 rearrangements are reported in both PA and CXPA [2].
Though the finding of immunohistochemical loss of BAP1 expression in the SDC component of a CXPA is novel and unique, it is limited by the nature of this being a single case report rather than a larger series. An additional limitation is that microdissection of different neoplastic components was not able to be performed to verify if the BAP1 alteration was limited to the SDC component. Though protein expression loss is well delineated by immunohistochemistry in the context of whole-tumor BAP1 loss of function, future studies will be needed to further parse the genetic landscape of SDC in CXPA in regard to BAP1.
In conclusion, we report the first documented case of BAP1 protein expression loss by immunohistochemistry in the SDC component of an intracapsular CXPA in the context of a BAP1 loss of function alteration by next-generation sequencing. Future studies will be needed to further investigate BAP1 alterations in CXPA, which may have prognostic and treatment implications.
References
Antony J, Gopalan V, Smith RA, Lam AK (2012) Carcinoma ex pleomorphic adenoma: a comprehensive review of clinical, pathological and molecular data. Head Neck Pathol 6(1):1–9. https://doi.org/10.1007/s12105-011-0281-z
Bubola J, MacMillan CM, Demicco EG et al (2021) Targeted RNA sequencing in the routine clinical detection of fusion genes in salivary gland tumors. Genes Chromosomes Cancer 60(10):695–708. https://doi.org/10.1002/gcc.22979
Chau C, van Doorn R, van Poppelen NM et al (2019) Families with BAP1-tumor predisposition syndrome in The Netherlands: path to identification and a proposal for genetic screening guidelines. Cancers. https://doi.org/10.3390/cancers11081114
Dogan S, Ng CKY, Xu B et al (2019) The repertoire of genetic alterations in salivary duct carcinoma including a novel HNRNPH3-ALK rearrangement. Hum Pathol 88:66–77. https://doi.org/10.1016/j.humpath.2019.03.004
El Hallani S, Udager AM, Bell D et al (2018) Epithelial-myoepithelial carcinoma: frequent morphologic and molecular evidence of preexisting pleomorphic adenoma, common HRAS mutations in PLAG1-intact and HMGA2-intact cases, and occasional TP53, FBXW7, and SMARCB1 alterations in high-grade cases. Am J Surg Pathol 42(1):18–27. https://doi.org/10.1097/pas.0000000000000933
Eletr ZM, Wilkinson KD (2011) An emerging model for BAP1’s role in regulating cell cycle progression. Cell Biochem Biophys 60(1–2):3–11. https://doi.org/10.1007/s12013-011-9184-6
Eletr ZM, Yin L, Wilkinson KD (2013) BAP1 is phosphorylated at serine 592 in S-phase following DNA damage. FEBS Lett 587(24):3906–3911. https://doi.org/10.1016/j.febslet.2013.10.035
George TJ, DeRemer DL, Parekh HD et al (2020) Phase II trial of the PARP inhibitor, niraparib, in BAP1 and other DNA damage response (DDR) pathway deficient neoplasms including cholangiocarcinoma. J Clin Oncol. https://doi.org/10.1200/JCO.2020.38.4_suppl.TPS591
Griffith CC, Seethala RR, Luvison A, Miller M, Chiosea SI (2013) PIK3CA mutations and PTEN loss in salivary duct carcinomas. Am J Surg Pathol 37(8):1201–1207. https://doi.org/10.1097/PAS.0b013e3182880d5a
Griffith CC, Thompson LDR, Assaad A et al (2014) Salivary duct carcinoma and the concept of early carcinoma ex pleomorphic adenoma. Histopathology 65(6):854–860. https://doi.org/10.1111/his.12454
Harbour JW, Onken MD, Roberson ED et al (2010) Frequent mutation of BAP1 in metastasizing uveal melanomas. Science 330(6009):1410–1413. https://doi.org/10.1126/science.1194472
Hassan R, Mian I, Wagner C et al (2020) Phase II study of olaparib in malignant mesothelioma (MM) to correlate efficacy with germline and somatic mutations in DNA repair genes. J Clin Oncol 38(15):9054–9054. https://doi.org/10.1200/JCO.2020.38.15_suppl.9054
Hassan R, Morrow B, Thomas A et al (2019) Inherited predisposition to malignant mesothelioma and overall survival following platinum chemotherapy. Proc Natl Acad Sci USA 116(18):9008–9013. https://doi.org/10.1073/pnas.1821510116
Irani S, Bidari-Zerehpoush F (2017) BRCA1/2 mutations in salivary pleomorphic adenoma and carcinoma-ex-pleomorphic adenoma. J Int Soc Prev Community Dent 7(Suppl 3):S155-s162. https://doi.org/10.4103/jispcd.JISPCD_184_17
Jensen DE, Proctor M, Marquis ST et al (1998) BAP1: a novel ubiquitin hydrolase which binds to the BRCA1 RING finger and enhances BRCA1-mediated cell growth suppression. Oncogene 16(9):1097–1112. https://doi.org/10.1038/sj.onc.1201861
Kakkar A, Guleria P, Madan K, Kumar R, Kumar S, Jain D (2019) Immunohistochemical assessment of BAP1 protein in mucoepidermoid carcinomas. Indian J Otolaryngol Head Neck Surg 71(1):33–37. https://doi.org/10.1007/s12070-018-1549-3
Kwon J, Lee D, Lee S-A (2023) BAP1 as a guardian of genome stability: implications in human cancer. Exp Mol Med. https://doi.org/10.1038/s12276-023-00979-1
Laitman Y, Newberg J, Molho RB, Jin DX, Friedman E (2021) The spectrum of tumors harboring BAP1 gene alterations. Cancer Genet 256–257:31–35. https://doi.org/10.1016/j.cancergen.2021.03.007
Louie BH, Kurzrock R (2020) BAP1: Not just a BRCA1-associated protein. Cancer Treat Rev 90:102091. https://doi.org/10.1016/j.ctrv.2020.102091
Masoomian B, Shields JA, Shields CL (2018) Overview of BAP1 cancer predisposition syndrome and the relationship to uveal melanoma. J Curr Ophthalmol 30(2):102–109. https://doi.org/10.1016/j.joco.2018.02.005
Nakajima Y, Kishimoto T, Nagai Y et al (2009) Expressions of androgen receptor and its co-regulators in carcinoma ex pleomorphic adenoma of salivary gland. Pathology 41(7):634–639. https://doi.org/10.3109/00313020903071595
Rai K, Pilarski R, Cebulla CM, Abdel-Rahman MH (2016) Comprehensive review of BAP1 tumor predisposition syndrome with report of two new cases. Clin Genet 89(3):285–294. https://doi.org/10.1111/cge.12630
Santana T, Pavel A, Martinek P et al (2019) Biomarker immunoprofile and molecular characteristics in salivary duct carcinoma: clinicopathological and prognostic implications. Hum Pathol 93:37–47. https://doi.org/10.1016/j.humpath.2019.08.009
Shankar GM, Santagata S (2017) BAP1 mutations in high-grade meningioma: implications for patient care. Neuro Oncol 19(11):1447–1456. https://doi.org/10.1093/neuonc/nox094
Tondi-Resta I, Hobday SB, Gubbiotti MA et al (2023) Carcinoma ex pleomorphic adenomas: an institutional experience and literature review. Am J Clin Pathol. https://doi.org/10.1093/ajcp/aqac181
Wang K, McDermott JD, Schrock AB et al (2017) Comprehensive genomic profiling of salivary mucoepidermoid carcinomas reveals frequent BAP1, PIK3CA, and other actionable genomic alterations. Ann Oncol 28(4):748–753. https://doi.org/10.1093/annonc/mdw689
Wang K, Russell JS, McDermott JD et al (2016) Profiling of 149 salivary duct carcinomas, carcinoma ex pleomorphic adenomas, and adenocarcinomas, not otherwise specified reveals actionable genomic alterations. Clin Cancer Res 22(24):6061–6068. https://doi.org/10.1158/1078-0432.CCR-15-2568
Yu H, Pak H, Hammond-Martel I et al (2014) Tumor suppressor and deubiquitinase BAP1 promotes DNA double-strand break repair. Proc Natl Acad Sci USA 111(1):285–290. https://doi.org/10.1073/pnas.1309085110
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
EFQ, PRC, and JSN contributed to the pathology diagnosis, concept, acquisition/analysis of clinical data, and interpretation as well as wrote and revised the manuscript. LR contributed to the pathology diagnosis, critically reviewed the intellectual content of the work, and contributed to manuscript revision. MAM acquired clinical data, critically reviewed the intellectual content of the work, and contributed to the manuscript revision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no competing interests or funding and declare that they have no conflicts of interest.
Research Involving Human Participants or Animals
This article does not contain any studies with human participants or animals performed by any of the authors as determined by the Institutional Review Board (UAMS).
Informed Consent
For this type of study (case report), informed consent is not required (IRB approved, UAMS).
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quiroga, E.F., Connor, P.R., Rooper, L. et al. Loss of BAP1 Protein Expression by Immunohistochemistry in the Salivary Duct Carcinoma Component of an Intracapsular Carcinoma ex Pleomorphic Adenoma of the Parotid Gland. Head and Neck Pathol 17, 851–854 (2023). https://doi.org/10.1007/s12105-023-01579-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-023-01579-1