Abstract
Background
Solitary fibrous tumor can exhibit a broad morphologic spectrum, such as presence of epithelioid tumor cells, adipose cells and multinucleated giant cells. This report describes an unusual morphologic variant characterized by adenofibromatous features, all occurring in the sinonasal region.
Methods
Four cases of the adenofibromatous variant of solitary fibrous tumor were retrieved from the surgical pathology and consultation files in Queen Elizabeth Hospital, Hong Kong. Histologic examination, immunohistochemical study and reverse-transcription polymerase chain reaction (RT-PCR) were performed.
Results
The patients were adults who presented with an obstructive mass of the nasal septum, nasal cavity or nasolacrimal sac. Histologic examination showed a circumscribed biphasic tumor with intermingling of glandular structures and spindle cells, reminiscent of mammary fibroadenoma. Bland-looking spindle cells formed short, irregularly oriented fascicles, admixed with variable amount of collagen fibers. The glandular component comprised ducts and seromucinous acini with a lobular architecture, indicating that it represented exuberant hyperplasia of indigenous glands rather than part of the neoplastic process. Demonstration of CD34 and STAT6 immunoreactivity in the spindle cells and NAB2::STAT6 gene fusion by polymerase chain reaction supports the diagnosis of solitary fibrous tumor.
Conclusion
This study reports four cases of sinonasal solitary fibrous tumor with adenofibromatous features, furthermore expanding the morphologic spectrum of this tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Solitary fibrous tumor is a mesenchymal tumor that has now been recognized in almost every anatomic site since its original description as a pleural tumor in 1931 by Klemperer and Rabin [1, 2]. Upon the theme of circumscribed growth, alternating hypercellular and hypocellular foci, patternless proliferation of spindle cells, collagenous stroma and pericytomatous blood vessels, the morphologic spectrum of this tumor type has expanded from the classical form (solitary fibrous tumor) and hypercellular form (so-called hemangiopericytoma) to encompass the epithelioid variant (with a component of epithelioid cells arranged in solid sheets) [3], fat-forming variant (with interspersed mature adipocytes) and giant cell-rich variant (formerly known as giant cell angiofibroma, with multinucleated cells which sometimes line pseudovascular spaces) [4, 5]. The distinctive genetic alteration of this tumor is inversion on chromosome 12q13 resulting in NAB2::STAT6 gene fusion, leading to overexpression of the C-terminal portion of STAT6 [6, 7]. We herein describe an unusual morphologic variant of solitary fibrous tumor occurring in the sinonasal tract, characterized by biphasic morphology due to presence of a prominent adenomatoid component.
Materials and Methods
Four cases of the adenofibromatous variant of solitary fibrous tumor were studied, including two (cases 1 and 3) retrieved from the surgical pathology files of Queen Elizabeth Hospital, Hong Kong and two from the consultation files of the authors. Clinical and follow-up information were obtained from the hospital records or the referring pathologists. Four-micron-thick sections were cut from formalin-fixed, paraffin-embedded blocks and stained with hematoxylin and eosin for light microscopic examination. Immunohistochemical study was performed using automated immunostainers (BOND III, Leica Microsystems, Nussloch, Germany; or VENTANA Benchmark, Roche Diagnostics, Tucson, Arizona, USA) and the antibodies used are listed in Table 1.
Reverse-transcription polymerase chain reaction (RT-PCR) was performed to detect NAB2::STAT6 fusion. Total RNA was extracted from paraffin sections and purified by standard method. RT-PCR was performed using NAB2 and STAT6 gene-specific primers. PCR product bands were purified and subjected to DNA sequencing analysis. NCBI sequence NM_005967.3 (mRNA, NAB2 gene) & NM_001178078.1 (mRNA, STAT6 gene) were used as reference for analyses.
Results
Clinical Features
The clinical features are summarized in Table 2. The patients included three women and one man, aged 34 to 69 years (mean 52 years). They presented with obstructive mass lesions arising from the nasal septum (n = 2), nasal cavity (n = 1) or lacrimal sac (n = 1), ranging from 1.5 to 4 cm in size. No recurrence was found after excision up to 7 years of follow up.
Pathologic Features
The tumors were firm, circumscribed, oval or bosselated with a smooth surface. The cut surfaces were whitish and homogeneous with scattered small cystic spaces.
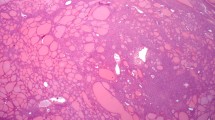
Histologically, the tumor was well circumscribed and showed a fibroadenomatous architecture (Figs. 1, 2). The glandular component, constituting a prominent (cases 1, 2 and 4) to multifocal component (case 3), was represented by dilated to cystic ducts and hyperplastic seromucinous acini (Figs. 1A, B, 2B) which were found throughout or predominantly at the peripheral zone of the tumor. Lined by cuboidal to columnar cells with bland-looking nuclei (Fig. 2C), the ducts contained eosinophilic secretion and were surrounded by fibrous stroma. The seromucinous acini were arranged in discrete lobules or sometimes merged into the fibrocellular stroma. Focally, connection between the acini and ducts was discernible (Fig. 2A). In case 2, some glandular structures were lined by respiratory-type epithelium. There was no cytologic atypia or mitotic activity.
Histological features of case 1 (Hematoxylin and eosin). A and B The biphasic tumor comprised variably dilated glands with preserved lobular architecture, intermingling with the spindle cell component. C and D The spindle cells were arranged in fascicles and intimately associated with collagen fibers. They displayed elongated nuclei with even chromatin as well as indistinct cytoplasm. Features of the spindle cell component were those of an otherwise typical solitary fibrous tumor
Histological features of cases 2, 3, and 4 (Hematoxylin and eosin). A The glandular component displayed preserved lobular architecture and maintenance of the ductal-acinar organization (case 4). B Occasional glands were dilated (case 3). C The glands, which included ducts and seromucinous acini, were lined by simple bland looking epithelium (case 2). D The spindle cells among the glands exhibited features of solitary fibrous tumor (case 2)
The mesenchymal component comprised spindle cells arranged in short, irregularly-oriented fascicles interspersed with collagenous to focally myxoid stroma. Keloid-like collagen was readily seen. The spindle cells possessed elongated nuclei, fine chromatin, indistinct nucleoli, and imperceptible or ill-defined eosinophilic cytoplasm that appeared to merge with the collagenous stroma (Figs. 1C, D, 2D). The mitotic count was less than 1 per 10 high power fields, and there was no necrosis. No staghorn-shaped blood vessels were found.
Immunostaining showed that the epithelial cells were positive for cytokeratin (Fig. 3A) and negative for p63, SMA, S100, CD34 and STAT6. The myoepithelial/ basal cells around the acini and ducts were highlighted by p63 (Fig. 3B), SMA, and S100. In case 3, some ducts rimmed by p63-positive, SMA-negative basal cells were discernible, suggesting that larger excretory ducts were also entrapped within the tumor. The spindle cells showed diffuse and strong staining for CD34 (Fig. 3C) and STAT6 (Fig. 3D). They were negative for cytokeratin, S100, SMA and calponin, and there was no nuclear staining for beta-catenin. The Ki67 proliferative index was less than 5%.
Immunohistochemical profile of case 1. A The glands were lined by pan-cytokeratin-positive epithelial cells. B The epithelial cells were rimmed by p63-positive myoepithelial/ basal cells. The spindle cells were negative for both cytokeratin and p63. C and D Staining for CD34 and STAT6 respectively, showing diffuse strong positivity in the spindle cells. The glandular component was negative for both markers
RT-PCR revealed NAB2::STAT6 gene fusion in all cases. The breakpoint was identified between exon 4 of NAB2 and exon 2 of STAT6 for cases 1 and 2, and between exon 3 of NAB2 and exon 18 of STAT6 for case 3. For case 4, in addition to a major fusion transcript between exon 6 of NAB2 and exon 17 of STAT6, there was a minor transcript joining exon 5 of NAB2 and exon 19 of STAT6, with breakpoint located within exons.
Discussion
Sinonasal solitary fibrous tumor is uncommon, accounting for less than 0.1% of all sinonasal neoplasms. About 6% of the solitary fibrous tumors occur in the head and neck region, among which ~ 30% originate in the sinonasal tract [8]. The reported morphologic features of sinonasal solitary fibrous tumor are similar to those found in other parts of the body [9, 10]. In this series, we describe an unusual morphologic variant occurring in the sinonasal region characterized by the presence of a prominent intermingled glandular component, giving rise to a fibroadenomatoid pattern. The epithelial component features dilated ducts and hyperplastic acini which do not appear to be neoplastic because of preserved lobular architecture, maintenance of the ductal-acinar organization and luminal-abluminal cellular architecture, and lack of nuclear STAT6 staining. They most likely represent a hyperplastic process in response to the tumor, similar to that seen in granular cell tumor, which is commonly accompanied by striking mucosal epithelial hyperplasia [11, 12]. The morphologic features of the spindle cells are otherwise typical for solitary fibrous tumor, and the diagnosis is confirmed by positive staining of CD34 and STAT6 and the presence of NAB2::STAT6 gene fusion.
When solitary fibrous tumor occurs in glandular or epithelial tissues, the indigenous epithelial structures may be incorporated among the neoplastic spindle cells, as has been reported in the parotid gland in the form of acini and ducts in the peripheral portion of the tumor [13] and in the lung in the form of attenuated epithelial structures giving rise to a peculiar biphasic morphology described as “pseudopapillary variant” [14] or “pulmonary adenofibroma” [15]. For solitary fibrous tumor occurring in the sinonasal tract, cystic dilatation of entrapped glands and ducts has been briefly described by Smith et al. [8], and a similar case is recently reported by Baneckova et al. as an example of “solitary fibrous tumor with deceptive morphologic features” [16]. In the current series, the indigenous minor salivary acini, ducts and surface respiratory epithelium of the sinonasal tract undergo exuberant hyperplasia within the solitary fibrous tumor, resulting in a biphasic appearance that can evoke wide differential diagnoses. Respiratory epithelial adenomatoid hamartoma comprises hamartomatous proliferation of glands in a hypocellular fibrous stroma which should lack STAT6 immunostaining. In contrast to seromucinous hamartoma in which myoepithelial/ basal cells around small glands are absent or at most focal, the hyperplastic acini and ducts entrapped within the solitary fibrous tumors in our case series are all rimmed by myoepithelial/ basal cells; seromucinous hamartoma also lacks a STAT6-positive cellular spindly cell component, unless it occurs in combination with a solitary fibrous tumor. Pleomorphic adenoma features proliferation of glandular structures comprising epithelial and myoepithelial cells, and the latter may appear as fascicles of spindle cells; however, the classic chondromyxoid stroma and immunopositivity of the spindle cells for myoepithelial markers are not seen in solitary fibrous tumor. While biphenotypic sinonasal sarcoma is commonly accompanied by proliferation and invagination of the covering epithelium [17], the collagen matrix accompanying the spindle cells is often less striking than that in solitary fibrous tumor; the spindle cells are characteristically positive for myogenic markers, S100 protein and PAX3 while being negative for STAT6. In biphasic synovial sarcoma, the epithelial component represents part of the neoplastic population which lacks ductal-acinar organization, and the tumor cells show immunoreactivity to SS18-SSX fusion-specific antibody while being negative for STAT6. The most important features suggesting the non-neoplastic nature of the glandular proliferation in adenofibromatous solitary fibrous tumor are the preserved lobular architecture and dual cell-layered composition. The adenofibromatous variant can be distinguished from the rare solitary fibrous tumors with transdifferentiation by the lack of malignant cytologic features in the glandular component [16].
The potential correlation between specific NAB2::STAT6 fusion variants and clinicopathological features has been explored by multiple previous studies. Most of the fusion variants belong to either STAT6-full or STAT6-△DBD type (i.e., fusion of any region of NAB2 with 5ʹ or 3ʹ site of STAT6 respectively), as proposed by Yuzawa et al. [18]. Many studies reported propensity for younger age, extra-thoracic location, smaller size, malignant histology and increased mitoses in STAT6-△DBD compared with STAT6-full tumors, yet data on prognostic implication have been conflicting [18,19,20,21,22,23,24,25]. In our series, the fusion variants in cases 1 and 2 were of STAT6-full type, while those in cases 3 and 4 belonged to STAT6-△DBD type. Thus the presence of adenofibromatoid features was common to tumors harboring both types of fusion variants.
In summary, we describe an unusual morphologic variant of solitary fibrous tumor in the sinonasal region characterized by intratumoral exuberant proliferation of indigenous glands. Awareness of this variant and use of appropriate immunostaining will aid in diagnosis. It is likely that solitary fibrous tumor occurring in other relatively enclosed anatomic sites with indigenous mucosal glands, such as the salivary glands, oral cavity, tracheobronchial mucosa or lacrimal gland, may potentially exhibit this variant morphology, as exemplified by a reported case in the lacrimal gland [26].
Data Availability
The data analyzed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
References
Klemperer P, Rabin CB. Primary neoplasms of the pleura. A report of five cases. Arch Pathol. 1931;11:385–412.
Chan JK. Solitary fibrous tumour–everywhere, and a diagnosis in vogue. Histopathology. 1997;31(6):568–76.
Warraich I, Dunn DM, Oliver JW. Solitary fibrous tumor of the orbit with epithelioid features. Arch Pathol Lab Med. 2006;130(7):1039–41.
Gengler C, Guillou L. Solitary fibrous tumour and haemangiopericytoma: evolution of a concept. Histopathology. 2006;48(1):63–74.
Demicco EG, Fritchie KH, Han A. Solitary fibrous tumour. In: Board WCoTE, editor. Soft tissue and bone tumours. Lyon: International Agency for Research on Cancer; 2020. p. 104–8.
Chmielecki J, et al. Whole-exome sequencing identifies a recurrent NAB2-STAT6 fusion in solitary fibrous tumors. Nat Genet. 2013;45(2):131–2.
Robinson DR, et al. Identification of recurrent NAB2-STAT6 gene fusions in solitary fibrous tumor by integrative sequencing. Nat Genet. 2013;45(2):180–5.
Smith SC, et al. Solitary fibrous tumors of the head and neck: a multi-institutional clinicopathologic study. Am J Surg Pathol. 2017;41:1642.
Batsakis JG, Hybels RD, El-Naggar AK. Solitary fibrous tumor. Ann Otol Rhinol Laryngol. 1993;102(1 Pt 1):74–6.
Flucke U, Thompson LDR, Wenig BM. Solitary fibrous tumor. In: El-Naggar AK, editor. WHO classification of head and neck tumors. Lyon: International Agency for Research on Cancer; 2017. p. 45.
Desimone RA, Ginter PS, Chen YT. Granular cell tumor of the breast eliciting exuberant pseudoepitheliomatous hyperplasia. Int J Surg Pathol. 2014;22(2):156–7.
Lack EE, et al. Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol. 1980;13(4):301–16.
Bauer JL, Miklos AZ, Thompson LD. Parotid gland solitary fibrous tumor: a case report and clinicopathologic review of 22 cases from the literature. Head Neck Pathol. 2012;6(1):21–31.
Cavazza A, et al. Solitary fibrous pseudopapillary tumor of the lung: pulmonary fibroadenoma and adenofibroma revisited. Pathologica. 2003;95(3):162–6.
Fusco N, et al. Recurrent NAB2-STAT6 gene fusions and oestrogen receptor-alpha expression in pulmonary adenofibromas. Histopathology. 2017;70(6):906–17.
Baneckova M, et al. Misleading morphologic and phenotypic features (transdifferentiation) in solitary fibrous tumor of the head and neck: report of 3 cases and review of the literature. Am J Surg Pathol. 2022;46:1084–94.
Lewis JE, Oliveira AM, et al. Biphenotypic sinonasal sarcoma. In: El-Naggar AK, et al., editors. WHO classification of head and neck tumors. Lyon: International Agency for Research on Cancer; 2017. p. 40–1.
Yuzawa S, et al. Analysis of NAB2-STAT6 gene fusion in 17 cases of meningeal solitary fibrous tumor/hemangiopericytoma: review of the literature. Am J Surg Pathol. 2016;40(8):1031–40.
Barthelmess S, et al. Solitary fibrous tumors/hemangiopericytomas with different variants of the NAB2-STAT6 gene fusion are characterized by specific histomorphology and distinct clinicopathological features. Am J Pathol. 2014;184(4):1209–18.
Baneckova M, et al. Solitary fibrous tumors of the head and neck region revisited: a single-institution study of 20 cases and review of the literature. Hum Pathol. 2020;99:1–12.
Nakada S, Minato H, Nojima T. Clinicopathological differences between variants of the NAB2-STAT6 fusion gene in solitary fibrous tumors of the meninges and extra-central nervous system. Brain Tumor Pathol. 2016;33(3):169–74.
Chuang IC, et al. NAB2-STAT6 gene fusion and STAT6 immunoexpression in extrathoracic solitary fibrous tumors: the association between fusion variants and locations. Pathol Int. 2016;66(5):288–96.
Huang SC, et al. The clinicopathological significance of NAB2-STAT6 gene fusions in 52 cases of intrathoracic solitary fibrous tumors. Cancer Med. 2016;5(2):159–68.
Tai HC, et al. NAB2-STAT6 fusion types account for clinicopathological variations in solitary fibrous tumors. Mod Pathol. 2015;28(10):1324–35.
Akaike K, et al. Distinct clinicopathological features of NAB2-STAT6 fusion gene variants in solitary fibrous tumor with emphasis on the acquisition of highly malignant potential. Hum Pathol. 2015;46(3):347–56.
Cho NH, et al. Solitary fibrous tumour with an unusual adenofibromatous feature in the lacrimal gland. Histopathology. 1998;33(3):289–90.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Results of Studies Involving Humans and/or Animals
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwok, A.L.M., Chan, J.K.C., Tang, A.H.N. et al. Adenofibromatous Solitary Fibrous Tumor: An Unusual Morphologic Variant Occurring in the Sinonasal Tract. Head and Neck Pathol 17, 165–171 (2023). https://doi.org/10.1007/s12105-022-01490-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-022-01490-1