Abstract
Pleomorphic adenoma (PA) is the most common biphasic type of salivary gland tumour to arise in adults. It is a biphasic tumour composed of both luminal (ductal) cells and abluminal (basal and myoepithelial) cells. Other biphasic salivary gland type tumours, both benign and malignant, can mimic PA, especially on small biopsies. Previous studies have shown that glial fibrillary acidic protein (GFAP) is preferentially expressed in PA and can be useful in the distinction from other salivary gland tumours. However, most of these studies were performed on a small subset of tumour types at a time when the classification of salivary gland type tumours was less refined. The purpose of this study was to assess the expression of glial fibrillary acidic protein (GFAP) in a broad group of both benign and malignant salivary gland tumours. The expression of GFAP was assessed in 99 tumours including 54 PAs, 5 basal cell adenomas, 1 myoepitheliomas, 5 adenoid cystic carcinomas, 6 epithelial-myoepithelial carcinomas (EMCA), 6 mucoepidermoid carcinomas, 7 salivary duct carcinomas, 1 adenocarcinomas NOS, 2 myoepithelial carcinomas, 4 basal cell adenocarcinomas, 5 acinic cell carcinomas and 3 polymorphous adenocarcinomas. Of the malignant cases, 8 were classified as carcinomas ex PA. GFAP was also assessed in 19 concurrent biopsy specimens. GFAP was expressed in the resections of 51 PAs examined (94%). Expression was predominantly strong and diffusely seen in myoepithelial cells. Strong and diffuse GFAP expression was also seen in two EMCAs (33%) and one myoepithelial carcinoma (50%). On biopsy specimens, 100% of PAs and basal cell adenomas expressed GFAP. GFAP was also seen in 1 out of 3 carcinomas ex PAs on biopsies. Almost all PAs show strong and diffuse expression of GFAP. In contrast, most malignant neoplasms that can mimic PA on biopsies show only rare, focal expression. Other benign tumours composed of abluminal/myoepithelial cells also show focal expression of GFAP, highlighting the spectrum these tumours share with PA. Overall, the presence of strong and diffuse GFAP expression can favour a benign neoplasm, specifically a PA, on limited biopsy specimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pleomorphic adenoma (PA) is the most common type of salivary gland tumour. It is described as biphasic owing to the presence of both luminal (ductal) and abluminal (basal and myoepithelial cell) components [1]. PAs can arise in any anatomical site that contains salivary gland type tissue; however, the majority are found in the parotid gland. While most PAs behave as a benign tumour, a small proportion of PAs will undergo malignant transformation. This change is more commonly seen in older patients with longer standing disease [2,3,4].
PAs are well known to exhibit an almost endless variety of morphological and architectural patterns [5]. The variety arises both from the relative proportions of luminal and abluminal cells within a tumour and from the morphologic versatility inherent to myoepithelial cells. As a result, the histologic features of a PA frequently overlap with other benign and malignant salivary gland neoplasms [6]. This can present a diagnostic challenge for pathologists, especially when provided with small tissue samples.
Previous studies have shown that glial fibrillary acidic protein (GFAP) is preferentially expressed in PA and that this marker can be useful in the distinction from other salivary gland tumours [5, 7, 8]. However, most of these studies were performed on a smaller subset of tumour types at time when the classification of salivary gland type tumours was less refined. The purpose of this study was to assess the expression of GFAP in a broad group of both benign and malignant salivary gland tumours using the updated classification system and address the utility of GFAP in the diagnosis of PA.
Materials and Methods
Study Population
The pathology archive of the Eastern Ontario Regional Laboratory Association (EORLA) was searched for all salivary gland type tumours diagnosed between 2016 and 2020. Cases were excluded if glass slides were unavailable for review or if there was insufficient tissue to perform additional tests as required. Histological slides were reviewed to verify the diagnosis.
Immunohistochemistry
Immunohistochemical analysis was performed on 4-µm sections cut from paraffin blocks using a fully automated system (Benchmark XT, Ventana Medical Systems Inc, Tucson, Arizona, USA) according to the manufacturer guidelines using the following antibodies: GFAP (clone Ga5, prediluted, Leica), S100 (clone EP32, prediluted, Leica), p40 (clone BC28, dilution 1:100, Biocare), calponin (clone 26A11, prediluted, Leica), and SMA (clone 1A4, dilution 1:750, DAKO). Positive and negative controls were used throughout. A strong reaction in at least 10% of the tumour cells was considered positive.
Statistics
A Fisher exact test was performed to compare the difference in GFAP expression between PAs and non-PAs with a p-value of < 0.05 being considered significant.
Results
A total of 146 tumours were identified; 47 cases were excluded leaving 99 tumours in the final analysis. There were 36 males and 63 females and the average age at the time of diagnosis was 59 years (range 20–93 years). A biopsy was performed on 67 patients prior to surgical resection of the tumour. Most tumours involved the parotid gland (n = 59). Other head and neck sites involved were the oral cavity (n = 21), submandibular gland (n = 15), parapharyngeal space (n = 3), and middle ear (n = 1). The average tumour size was 29 millimeters (range 3–73 millimeters).
The tumours in this study included 54 PAs, 5 acinic cell carcinomas, 5 adenoid cystic carcinomas, 4 basal cell adenocarcinomas, 5 basal cell adenomas, 6 epithelial-myoepithelial carcinomas (EMCA), 6 mucoepidermoid carcinomas, 2 myoepithelial carcinomas, 1 myoepitheliomas, 3 polymorphous adenocarcinomas, 1 adenocarcinoma not otherwise specified (NOS), and 7 salivary duct carcinomas. Of these, 2 EMCAs and 2 salivary duct carcinomas arose from the background of a PA and were diagnosed as carcinoma ex PA.
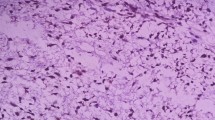
The immunohistochemical results for GFAP staining are summarized in Table 1. GFAP was expressed in 51 out of 54 PAs and in the majority of these tumours (96%) the expression was strong and diffuse (Fig. 1A, B). No GFAP expression was seen in 3 PAs (Fig. 1C, D). Microscopically, all three of these tumours were composed of a biphasic population of cells with no definitive features of malignancy. Of note, two of the three tumours were subclassified: one as a myoepithelial-rich PA and the other as a cellular PA. Despite showing non-reactivity for GFAP, the myoepithelial cells in all three cases were reactive for S100, calponin, SMA and p40.
GFAP expression in pleomorphic adenoma. The histologic appearance of a typical pleomorphic adenoma showing a well circumscribed biphasic tumour with focal chondromyxoid stroma (A). GFAP was strongly and diffusely expressed throughout the tumour (B) by abluminal cells consistent with myoepithelial cells (inset). Another biphasic tumour with abundant myoepithelial cells arranged in sheets around small ducts (C). This tumour was negative for GFAP (D)
Among the other tumour types assessed, strong and diffuse expression of GFAP was also seen in two EMCAs and one myoepithelial carcinoma. Focal GFAP expression was seen in one basal cell adenocarcinoma, three basal cell adenomas (Fig. 2A, B), and one salivary duct carcinoma. Despite a significant abluminal cell component, all five of the adenoid cystic carcinomas examined were negative for GFAP (Fig. 2C, D). Overall, strong, and diffuse expression of GFAP was more likely to be seen in PAs compared to all other tumour types assessed (p = 0.002).
GFAP expression in other types of salivary gland tumours. Basal cell adenoma with tumour cells arranged in a predominantly trabecular pattern (A). GFAP was focally expressed (B) by myoepithelial cells at the periphery of the trabeculae (inset). Adenoid cystic carcinoma showing a mixed cribriform and tubular pattern of growth with extensive perineural invasion (C). The tumour was negative for GFAP with nerves serving as an internal control (D, black arrows)
The other immunohistochemical markers assessed in this study are summarized in Table 2. Strong and diffuse S100 expression was seen in all 54 out of 54 PAs and most of the other tumour types tested. Interestingly, the other myoepithelial markers assessed were only expressed in a subset of PAs, with SMA, calponin, and p40 being strongly expressed in 40, 43, and 40 tumours, respectively. These markers were also variably expressed in the other tumour types assessed.
Carcinoma ex PA was identified in six cases including four salivary duct carcinomas and two EMCAs. In 5 out of 6 cases, strong and diffuse GFAP expression was seen in the residual benign PA. As previously described, the malignant cells in both EMCA ex PAs strongly expressed GFAP (Fig. 3A, B). In contrast, the malignant cells in all four salivary duct carcinomas were negative for GFAP. Interestingly, in one case, morphologically benign appearing GFAP positive cells were seen surrounding the morphologically malignant appearing GFAP negative ductal cells (Fig. 3C, D). Moreover, the GFAP positive cells tended to be large and physically separated from the GFAP negative ductal cells, unlike the myoepithelial cells that line normal ductal structures. Indeed, the overall appearance was more reminiscent of malignant ductal cells embedded in a benign stroma. The other myoepithelial markers assessed were also expressed both the benign and malignant components of these tumours with S100, SMA, calponin, and p40 being expressed in 5, 4, 4, and 4 tumours, respectively.
GFAP expression in carcinoma ex pleomorphic adenoma. Epithelial-myoepithelial carcinoma composed of small tubules infiltrating adipose tissue (A). A small focus of residual pleomorphic adenoma appears as a hyalinized nodule (A, black arrow). The malignant tumour and the residual pleomorphic adenoma are both strongly and diffusely positive for GFAP (B). Salivary duct carcinoma composed of apocrine cells arranged in large cystic structures (C, white arrow). The residual pleomorphic adenoma is composed primarily of myoepithelial cells embedded in a hyalinized stroma (C, black arrow). The residual pleomorphic adenoma is diffusely positive for GFAP while only scattered stromal cells are positive in the area of the malignant tumour (D)
Of the 99 tumours included in the study, 67 of them had a previous biopsy (n = 37) or cytology (n = 30) specimen. In sixty-four cases (95.5%) the biopsy or cytology diagnosis was concordant with the final resection diagnosis. Immunohistochemistry for GFAP was performed and available for review for 20 specimens and the results are summarized in Table 3. Of these cases, strong and diffuse GFAP was seen in all PAs. In contrast, only focal expression of GFAP was seen in one basal cell adenoma. The one salivary duct carcinoma that showed strong and diffuse expression of GFAP on biopsy analysis was later diagnosed as carcinoma ex PA and the GFAP expression was limited to the residual benign PA component in the resection specimen. Biopsies of remaining malignant tumours in our study, which included one EMCA, one polymorphous adenocarcinoma, and one salivary duct carcinoma were all negative for GFAP.
Discussion
This study confirms that neoplastic myoepithelial cells in PAs express GFAP and that this marker can be used to differentiate PA from histologically similar salivary gland type tumours. In contrast, the other immunohistochemical markers tested were expressed by a variety of tumour types and thus are not as helpful in this regard.
GFAP is an intermediate filament originally described in glial cells [9,10,11]. Acting primarily as a structural protein, GFAP serves a role in the maintenance of cell shape and structure [9, 10]. Subsequent studies found that GFAP is also expressed by myoepithelial cells in the normal salivary glands [7, 10, 11]. Consistent with prior studies, we found that GFAP was strongly and diffusely expressed by myoepithelial cells in the vast majority (96.1%) of PAs [5, 10,11,12]. The lack of GFAP expression in 3 out of 54 of our PAs may have represented variants that were limited or lacking in myoepithelial cells, were luminal cell-rich, or may have included myoepithelial cells at a stage of neoplastic development that were lacking GFAP-reactive intermediate filaments. The latter has been reported in an earlier study, describing the process of myoepithelial cell differentiation to be complex and accounting for differences in immunohistochemical marker reactivity based on stage of development [13]. Despite showing no reactivity for GFAP, the myoepithelial cells in all 3 cases were reactive for S100, calponin, SMA and p40.
In addition to GFAP, we also assessed the expression of the other widely available myoepithelial cell markers, S100 protein, actin, calponin and p40. In keeping with prior studies, we found that S100 is a highly sensitive marker for myoepithelial cells, with strong expression identified in all tumour types except salivary duct carcinoma [14, 15]. The other markers (actin, calponin, and p40), were less sensitive than both GFAP and S100 for PA and, like S100, were expressed in most of the other tumours assessed. Taken together, these results show that there is a differential expression of myoepithelial cell markers in salivary gland tumours. Specifically, the neoplastic myoepithelial cells in PA typically retain expression for GFAP and S100 while downregulating the expression of other makers such as actin, calponin, and p40. While S100 was consistently expressed in PA, its ubiquitous expression in the other tumour types assessed limits its utility as a differentiating marker.
While GFAP was consistently expressed by myoepithelial cells in PA, the expression of this marker in other myoepithelial-rich tumours was highly variable. For example, adenoid cystic carcinoma includes a significant myoepithelial cell component and yet none of the tumours in this study demonstrated any expression of GFAP. In contrast, a subset of myoepitheliomas and EMCAs in this study showed strong and diffuse staining for GFAP while other tumours were completely negative. These results suggest that GFAP is preferentially expressed by myoepithelial cells in PA.
A wide variety of both benign and malignant salivary gland tumours demonstrate a biphasic phenotype and tumours rich in myoepithelial and basal cells can closely resemble the cellular composition of PAs [16, 17]. Depending on the size of the sample, the differential diagnosis typically includes basal cell adenoma, basal cell adenocarcinoma, myoepithelioma, myoepithelial carcinoma, epithelial-myoepithelial carcinoma, and adenoid cystic carcinoma.
Of these, basal cell adenoma and its malignant counterpart basal cell adenocarcinoma are both composed predominantly of basal and myoepithelial cells and both can easily mimic an abluminal-cell rich PA [18]. One of the most helpful distinguishing traits is the absence of chondromyxoid stroma in basal cell adenoma and basal cell adenocarcinoma [6, 19, 20]. Necrosis and abundant mitoses are also typically identified in basal cell adenocarcinoma and should not be seen in PAs [18, 19]. Our results suggest that GFAP can aid in this setting as both tumour types show only focal expression in contrast to the diffuse expression seen in PA.
Similarly, myoepithelioma and its malignant counterpart myoepithelial carcinoma are both composed almost entirely of myoepithelial cells and, like PA, they often demonstrate a wide variety of architectural patterns. In contrast, they lack the chondromyxoid stroma that is so commonly observed in PA. However, this feature is not always identified on small biopsy samples [21, 22]. The one myoepithelioma in our study was negative for GFAP. In contrast, one myoepithelial carcinoma was positive for GFAP. Fortunately, the distinction between PA and myoepithelial carcinoma can be made based on the presence of necrosis, pleomorphism, and mitotic activity in the malignant tumour [21, 23]. That said, cellular PAs have previously shown higher false positive rates for malignant diagnoses on fine needle aspiration biopsies [10]. Within the current study 1 out of 3 GFAP-negative PAs was classified as a cellular variant, however, there were no microscopic features of malignancy seen in this particular case.
In small tissue samples, foci of cytological atypia and mucinous metaplasia may raise malignant diagnostic considerations including carcinoma ex PA and mucoepidermoid carcinoma [24]. Distinguishing between PA and adenoid cystic carcinoma can be even more challenging. In particular, PAs with basaloid morphology and extensive cylindromatous change are commonly mistaken for adenoid cystic carcinoma. [24]. In addition, characteristic morphological features of the two entities cannot always be relied on, particularity if a PA either lacks its unique chondromyxoid stroma or contains eosinophilic hyaline globules, the latter often found in adenoid cystic carcinoma [6, 25]. In keeping with previously published studies, we found that PA and adenoid cystic carcinoma also share many immunohistochemical features including diffuse expression of S100, SMA, and p40. While not assessed in this study, even the somewhat unique c-KIT staining seen in adenoid cystic carcinoma can occasionally be seen in PA [6, 26]. In contrast, we found that GFAP was strongly and diffusely expressed in PA and only focally expressed in adenoid cystic carcinoma. This distinction is important as these two entities have vastly different clinical outcomes.
The present study included six carcinoma ex PAs including two EMCAs and four salivary duct carcinomas. Not surprisingly, 5 out of 6 tumours expressed GFAP in the residual PA. However, strong GFAP expression was also observed in malignant myoepithelial cells in both EMCAs. Fortunately, the histologic features typically seen in EMCA help distinguish between these two tumours. In particular, EMCA commonly demonstrates a biphasic pattern of small inner ductal cells with dense eosinophilic cytoplasm and outer polygonal myoepithelial cells with clear cytoplasm, often arranged in tubules or cribriform structures [27,28,29]. This contrasts with the much less orderly arrangement of ductal cells, basal cells, myoepithelial cells, and stromal elements typically seen in a PA [25].
The expression of GFAP in benign myoepithelial cells adjacent to the malignant cells in one salivary duct carcinoma is interesting as these myoepithelial cells were clearly outside of the residual PA and appeared to be a bonafide component of the emergent malignant tumour. In contrast to the myoepithelial cells in the recently described intraductal carcinoma, the myoepithelial cells in this tumour were not associated with ductal structures and did not form a continuous layer below the malignant ductal cells [30, 31]. Despite the expression of GFAP in the myoepithelial cells, this tumour could easily be distinguished from PA by the presence of large, highly atypical, and pleomorphic tumour cells with abundant mitotic figures and an invasive pattern of growth. These features are characteristic of salivary duct carcinoma and can even be seen on small biopsy samples [4, 32].
Our study has several limitations. First, the expression of GFAP could only be assessed on 20 of 67 biopsy specimens. In most cases these biopsies were fine needle aspiration biopsies with inadequate tissue to perform a cell blocks for ancillary studies. However, in some cases, the biopsy was performed at an outside institution and the slides were not available for review. In 32 cases, no biopsy was performed prior to surgical resection. Although the immunohistochemical results were concordant in all of the cases with available biopsy specimens, not all tumour types were represented in the biopsy group. Despite the small number of cases, our results show that the presence of strong and diffuse GFAP expression can be used to favor pleomorphic adenoma, even when only limited biopsy material is available for microscopic examination. In our experience, this is particularly useful when assessing a tumour with morphologic features of a low-grade biphasic salivary gland neoplasm. The diagnostic entities in this category include polymorphous adenocarcinoma, basal cell adenocarcinoma, and adenoid cystic carcinoma, which in this study were largely negative for GFAP. Second, only one myoepithelioma was included in this study. This is important because some authors consider PA to be a spectrum of tumours with myoepithelioma on the myoepithelial-rich side of the spectrum. If such a theory is true, one would expect myoepithelioma to be positive for GFAP. However, in our study, the only myoepithelioma assessed did not show any expression of GFAP. This result suggests that myoepithelioma may in fact be a distinct entity, however, this result needs to be confirmed in larger studies.
This study confirms that PA can be distinguished from other salivary gland type tumours by its strong and diffuse expression of GFAP. Importantly, most malignant salivary gland type tumours that can mimic PA were either negative for GFAP or expressed the marker focally. These findings may be particularly useful in limited tissue biopsies which may not have all of the classic features of PA. A notable exception is EMCA, which shares overlapping features and may be derived from a PA. However, staining in EMCA may be confined to the myoepithelial component only, in contrast to the more diffuse staining seen in PA. Carcinomas ex PA may also demonstrate GFAP staining in the residual PA component, which may be strong and diffuse. The results of this study support including GFAP in the routine workup of salivary gland tumours.
Data Availability
Not applicable.
Code Availability
Data not available.
References
Nagao T, Sato E, Inoue R, et al. Immunohistochemical analysis of salivary gland tumors: application for surgical pathology practice. Acta Histochem Cytochem. 2012;45(5):269–82. https://doi.org/10.1267/ahc.12019.
Tarakji B, Baroudi K, Hanouneh S, Kharma MY, Nassani MZ, Azzeghaiby SN. Extensive review in the detection of the malignant transformation of pleomorphic adenoma. Gulf J Oncolog. 2013;1(13):67–82.
Francesco G, Emanuele C, Gabriele M, Valeria M, Angelo S, Antonio T. Myoepithelial carcinoma ex pleomorphic adenoma of the maxillary sinus: a case report and review of literature. Head Neck Pathol. 2021;15(4):1345–9. https://doi.org/10.1007/s12105-020-01282-5.
Toluie S, Thompson LD. Sinonasal tract adenoid cystic carcinoma ex-pleomorphic adenoma: a clinicopathologic and immunophenotypic study of 9 cases combined with a comprehensive review of the literature. Head Neck Pathol. 2012;6(4):409–21. https://doi.org/10.1007/s12105-012-0381-4.
Altunpulluk MD, Karabulut MH, Kır G, Şahin Ş. Pleomorphic adenoma of the larynx. North Clin Istanb. 2016;3(1):67–70. https://doi.org/10.14744/nci.2015.47965.
Cantley RL. Fine-needle aspiration cytology of cellular basaloid neoplasms of the salivary gland. Arch Pathol Lab Med. 2019;143(11):1338–45. https://doi.org/10.5858/arpa.2019-0327-RA.
Zaib N, Mushtaq S, Mamoon N, Akhter N, Ayaz B. Immunohistochemical pattern of pleomorphic adenoma, polymorphous low grade adenocarcinoma and adenoid cystic carcinoma in minor salivary glands. J Dent (Tehran). 2014;11(1):38–46.
Curran AE, Allen CM, Beck FM, Damm DD, Murrah VA. Distinctive pattern of glial fibrillary acidic protein immunoreactivity useful in distinguishing fragmented pleomorphic adenoma, canalicular adenoma and polymorphous low grade adenocarcinoma of minor salivary glands. Head Neck Pathol. 2007;1(1):27–32. https://doi.org/10.1007/s12105-007-0003-8.
Yang Z, Wang KK. Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trends Neurosci. 2015;38(6):364–74. https://doi.org/10.1016/j.tins.2015.04.003.
Ostrzega N, Cheng L, Layfield L. Glial fibrillary acid protein immunoreactivity in fine-needle aspiration of salivary gland lesions: a useful adjunct for the differential diagnosis of salivary gland neoplasms. Diagn Cytopathol. 1989;5(2):145–9. https://doi.org/10.1002/dc.2840050207.
Stead RH, Qizilbash AH, Kontozoglou T, Daya AD, Riddell RH. An immunohistochemical study of pleomorphic adenomas of the salivary gland: glial fibrillary acidic protein-like immunoreactivity identifies a major myoepithelial component. Hum Pathol. 1988;19(1):32–40. https://doi.org/10.1016/s0046-8177(88)80313-7.
Nishimura T, Furukawa M, Kawahara E, Miwa A. Differential diagnosis of pleomorphic adenoma by immunohistochemical means. J Laryngol Otol. 1991;105(12):1057–60. https://doi.org/10.1017/s0022215100118183.
Ianez RF, Buim ME, Coutinho-Camillo CM, Schultz R, Soares FA, Lourenço SV. Human salivary gland morphogenesis: myoepithelial cell maturation assessed by immunohistochemical markers. Histopathology. 2010;57(3):410–7. https://doi.org/10.1111/j.1365-2559.2010.03645.x.
Acharya S, Padmini S, Koneru A, Krishnapillai R. Intraoral salivary duct carcinoma: a case report and a brief review. J Oral Maxillofac Pathol. 2014;18(Suppl 1):121–7. https://doi.org/10.4103/0973-029X.141353.
Xie S, Yang H, Bredell M, et al. Salivary duct carcinoma of the parotid gland: a case report and review of the literature. Oncol Lett. 2015;9(1):371–4. https://doi.org/10.3892/ol.2014.2655.
Seethala RR. Basaloid/blue salivary gland tumors. Mod Pathol. 2017;30(s1):84–95. https://doi.org/10.1038/modpathol.2016.190.
Seethala RR, Stenman G. Update from the 4th edition of the world health organization classification of head and neck tumours: tumors of the salivary gland. Head Neck Pathol. 2017;11(1):55–67. https://doi.org/10.1007/s12105-017-0795-0.
Wilson TC, Robinson RA. Basal cell adenocarcinoma and basal cell adenoma of the salivary glands: a clinicopathological review of seventy tumors with comparison of morphologic features and growth control indices. Head Neck Pathol. 2015;9(2):205–13. https://doi.org/10.1007/s12105-014-0562-4.
Griffith CC, Siddiqui MT, Schmitt AC. Ancillary testing strategies in salivary gland aspiration cytology: a practical pattern-based approach. Diagn Cytopathol. 2017;45(9):808–19. https://doi.org/10.1002/dc.23715.
Griffith CC, Pai RK, Schneider F, et al. Salivary gland tumor fine-needle aspiration cytology: a proposal for a risk stratification classification. Am J Clin Pathol. 2015;143(6):839–53. https://doi.org/10.1309/AJCPMII6OSD2HSJA.
Xu B, Mneimneh W, Torrence DE, et al. Misinterpreted myoepithelial carcinoma of salivary gland: a challenging and potentially significant pitfall. Am J Surg Pathol. 2019;43(5):601–9. https://doi.org/10.1097/PAS.0000000000001218.
Wang C, Zhang Z, Ge Y, et al. Myoepithelial carcinoma of the salivary glands: a clinicopathologic study of 29 patients. J Oral Maxillofac Surg. 2015;73(10):1938–45. https://doi.org/10.1016/j.joms.2015.03.054.
Xu B, Katabi N. Myoepithelial carcinoma. Surg Pathol Clin. 2021;14(1):67–73. https://doi.org/10.1016/j.path.2020.09.008.
Chowsilpa S, An D, Maleki Z. Adenoid cystic carcinoma cytology: salivary gland and nonsalivary gland. Diagn Cytopathol. 2020;48(12):1282–9. https://doi.org/10.1002/dc.24573.
Jain R, Gupta R, Kudesia M, Singh S. Fine needle aspiration cytology in diagnosis of salivary gland lesions: a study with histologic comparison. Cytojournal. 2013;10:5. https://doi.org/10.4103/1742-6413.109547.
Zhu S, Schuerch C, Hunt J. Review and updates of immunohistochemistry in selected salivary gland and head and neck tumors. Arch Pathol Lab Med. 2015;139(1):55–66. https://doi.org/10.5858/arpa.2014-0167-RA.
Vázquez A, Patel TD, D’Aguillo CM, et al. Epithelial-myoepithelial carcinoma of the salivary glands: an analysis of 246 cases. Otolaryngol Head Neck Surg. 2015;153(4):569–74. https://doi.org/10.1177/0194599815594788.
El Hallani S, Udager AM, Bell D, et al. Epithelial-myoepithelial carcinoma: frequent morphologic and molecular evidence of preexisting pleomorphic adenoma, common HRAS mutations in PLAG1-intact and HMGA2-intact cases, and occasional TP53, FBXW7, and SMARCB1 alterations in high-grade cases. Am J Surg Pathol. 2018;42(1):18–27. https://doi.org/10.1097/PAS.0000000000000933.
Kusafuka K, Yamashita M, Muramatsu A, Arai K, Suzuki M. Epithelial-myoepithelial carcinoma ex-pleomorphic adenoma of the parotid gland: report of a rare case with immunohistochemical and genetic analyses. Med Mol Morphol. 2021;54(2):173–80. https://doi.org/10.1007/s00795-020-00262-6.
Russo D, Di Crescenzo RM, Varricchio S, et al. Low-grade intraductal carcinoma of the parotid gland: a case report and literature review. Head Neck Pathol. 2021;15(4):1359–71. https://doi.org/10.1007/s12105-021-01290-z.
Kuo YJ, Weinreb I, Perez-Ordonez B. Low-grade salivary duct carcinoma or low-grade intraductal carcinoma? Review of the literature. Head Neck Pathol. 2013;7(Suppl 1):59–67. https://doi.org/10.1007/s12105-013-0460-1.
Okano K, Ishida M, Sandoh K, Fujisawa T, Iwai H, Tsuta K. Cytological features of carcinoma ex pleomorphic adenoma of the salivary glands: a diagnostic challenge. Diagn Cytopathol. 2020;48(2):149–53. https://doi.org/10.1002/dc.24333.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work; acquisition, analysis, and interpretation of data; drafted the manuscript; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts or competing interests.
Ethical Approval
This study was conducted as part of a quality assurance program and was not subject to ethics approval.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gorski, Z., Purgina, B. & Wasserman, J.K. Glial Fibrillary Acidic Protein Expression Helps Distinguish Pleomorphic Adenoma from Histologic Mimics. Head and Neck Pathol 16, 695–702 (2022). https://doi.org/10.1007/s12105-021-01409-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-021-01409-2