Abstract
Primary myoepithelial neoplasms of soft tissue have been shown to be related to their salivary gland counterparts, with which they often share morphologic, immunophenotypic, and molecular genetic features, such as the presence of PLAG1 rearrangement in both soft tissue mixed tumor and salivary pleomorphic adenoma. However, important distinctions remain between soft tissue and salivary myoepithelial neoplasms, namely differing criteria for malignancy. This review provides an overview of the current understanding of the clinicopathologic and molecular features of soft tissue myoepithelial neoplasms, including discussion of the similarities and differences between soft tissue and salivary counterparts and relevant diagnostic issues specific to head and neck pathology practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumors of myoepithelial differentiation have been long recognized to arise in the salivary glands. Over the past two decades, primary myoepithelial neoplasms of soft tissue (as well as skin and bone) have been characterized on clinicopathologic, morphologic, and molecular grounds. While soft tissue myoepithelial neoplasms share many features with salivary myoepithelial tumors, there remain important distinctions that occasionally pose diagnostic challenges. In contrast to the salivary gland, primary myoepithelial tumors in soft tissue, bone, and skin (with the exception of some cutaneous lesions) lack any known normal cellular counterpart, accounting largely for initial skepticism as to the existence and myoepithelial phenotype of this group of tumors when they were first described. Myoepithelial tumors of soft tissue are classified as benign (myoepithelioma and mixed tumor/chondroid syringoma) and malignant (myoepithelial carcinoma). This review discusses our current understanding of soft tissue myoepithelial neoplasms, as well as outlining important similarities with, and distinctions from their salivary counterparts.
Clinical Features
Soft tissue myoepithelial tumors arise in men and women with equal frequency; patients are affected over a wide age range, with peak incidence during the third through fifth decades [1,2,3,4,5]. Approximately one-fifth of cases occur in the pediatric population; most of these are myoepithelial carcinomas [2, 3, 6]. Myoepithelial neoplasms most commonly arise in the subcutaneous tissues of the extremities and proximal limb girdles, with tumors more frequently presenting in the lower limbs than in the upper limbs. However, a broad anatomic range can be observed, including deep-seated tumors and primary sites in the trunk, head and neck, and visceral organs [5, 7,8,9]. Cutaneous lesions are confined to the dermis, and are most common in the limbs, trunk, and head and neck [4, 10, 11]. Most patients present with a palpable, slow-growing, and painless superficial mass. Pain and local mass effects may occur secondary to larger lesions, which are more likely to be malignant.
Gross Features
Macroscopically, most tumors are well-circumscribed and nodular. Malignant tumors are likely to appear grossly infiltrative and are often larger in size. Benign myoepithelial tumors range in size from 0.7 to 12 cm (mean 3.8 cm) in soft tissue [2]; dermal lesions tend to be smaller, ranging from 0.5 to 2.5 cm (mean, 0.7 cm) [4]. Myoepithelial carcinomas range in size from 1.3 to 20 cm (mean ~ 5.3 cm) [2, 3]. Tumors are tan/white, or yellow, with a cut surface that can appear gelatinous or firm and fleshy, as well as occasionally gritty or calcified. Malignant tumors may show hemorrhage and necrosis.
Histologic Features and Malignant Criterion
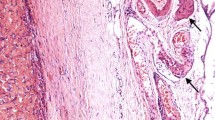
Myoepithelial neoplasms are morphologically diverse and are characterized by a wide range of architectural and cytologic features both within a tumor and between different lesions, similar to salivary myoepithelial tumors. Myoepithelial tumors appear multinodular or lobulated with a variably myxoid, chondroid, or hyalinized stroma (Fig. 1); tumors are well-circumscribed but unencapsulated, and infiltrative growth is common even for benign lesions. Tumors frequently show reticular or trabecular growth patterns, though nested and solid growth are also common (Fig. 1). Tumor cells are variably spindled, ovoid, or epithelioid, with uniform ovoid or round nuclei and eosinophilic to clear cytoplasm (Fig. 2). Occasionally, tumors may show a dominant single growth pattern or uniform morphologic appearance. For instance, the distinctive variant “cutaneous syncytial myoepithelioma” shows solid, sheet-like and syncytial growth of bland and uniform ovoid, spindled, or histiocytoid cells with palely eosinophilic cytoplasm [12] (Fig. 3). In many pediatric myoepithelial tumors, an epithelioid morphology predominates [3]. Studies have suggested some associations between genotype and specific phenotypes (see “Molecular Features”).
Similarly to salivary myoepithelial tumors (particularly pleomorphic adenoma), both benign and malignant soft tissue myoepithelial neoplasms can show occasional features of plasmacytoid “hyaline” cells with eccentrically placed nuclei and densely eosinophilic cytoplasm (Fig. 4a), tumor cells having clear vacuolated cytoplasm (previously classified as “parachordoma”) (Fig. 4b), and rhabdoid morphology. Heterologous differentiation is observed in up to 15% of cases, and is most commonly chondroosseous (Fig. 5a) and more rarely adipocytic or squamous (Fig. 5b) [1,2,3,4, 12].
Tumors are classified as “mixed tumors” when there is tubuloductal differentiation (which may be very focal in some cases) (Fig. 6a); these constitute approximately 10% of all myoepithelial tumors and nearly all are benign. Mixed tumors are essentially morphologically identical to pleomorphic adenoma of the salivary gland, but differ in that they may show infiltrative growth. In the skin, such tumors are known as chondroid syringomas, and are morphologically subclassified as apocrine-type and eccrine-type, the former being identical to mixed tumors and the latter likely pathogenetically distinct from soft tissue and salivary myoepithelial neoplasms [10, 13, 14].
Currently, cytologic atypia is the only known predictor of aggressive behavior in soft tissue myoepithelial tumors [2, 3], in contrast to salivary tumors for which malignancy is designated by the presence of capsular invasion and infiltrative growth. Benign tumors are designated as “myoepitheliomas,” which overall lack cytologic atypia (but if present, is at most mild) (Fig. 7a). Nucleoli are small or inconspicuous and lack hyperchromasia. While myoepithelioma may show some mitotic activity, atypical mitotic figures are absent. While rare cases may show perineural invasion, tumor necrosis is not observed. “Myoepithelial carcinomas”of soft tissue are defined as having moderate to severe nuclear atypia, and nuclei appear vesicular with coarse chromatin and prominent nucleoli. No standard criteria exist for grading, though in soft tissue pathology practice myoepithelial carcinomas are graded (somewhat) subjectively as low (Fig. 7b), intermediate, and high based on the degree of nuclear atypia; high-grade myoepithelial carcinomas typically show increased mitotic activity, atypical mitotic figures, and necrosis (Fig. 7c, d). However, the histologic grade does not appear to affect prognosis, and neither high mitotic rates and necrosis are predictive of behavior [2, 3]. Based on available data, it appears that nearly all soft tissue myoepithelial carcinomas arise de novo rather than from a benign precursor and only rarely show areas of morphologically benign mixed tumor or myoepithelioma [2, 3]. In contrast, at least half of all salivary myoepithelial carcinomas show preexisting pleomorphic adenoma [15], including a diagnostically challenging subset of intracapsular and minimally invasive tumors [16]. Approximately 30% of soft tissue myoepithelial carcinomas in pediatric patients exhibit an undifferentiated round cell component (Fig. 8), in addition to the prominent epithelioid morphology common in tumors in this age group [3].
Immunohistochemical Features
Myoepithelial neoplasms typically show co-expression of epithelial markers and S-100 [1,2,3,4,5, 10] (Fig. 9a, b), though many tumors show variability in immunophenotypes. Most cases show positivity for broad-spectrum keratins (93–100%), though some cases may require using multiple cocktails (pan-keratin, AE1/AE3, and Cam5.2). EMA positivity is more variable (19–79%), though reliably highlights ductal cells in soft tissue mixed tumors [1, 4, 10, 11, 17.]. S-100 protein is frequently positive (72–100%), while staining for GFAP is only seen in up 27–54% of cases. SOX10 staining occurs in up to 80% of myoepithelial neoplasms, although expression is much less frequent in myoepithelial carcinomas (30%) [18]. p63 staining ranges from 23 to 70% in myoepithelioma and 7–40% in myoepithelial carcinomas [2, 4, 19, 20], in contrast to more consistent p63 expression in most salivary myoepithelial neoplasms [21, 22]. Myogenic markers show more variable staining and are overall of limited diagnostic value; calponin is most frequently positive (90%), followed by SMA (34–64%), HHG-35 (20–60%), and desmin (0–20%) [1, 2].
Among myoepithelial neoplasms, there are several immunophenotypic associations with certain morphologic or molecular features. PLAG1 is frequently positive in mixed tumors (58–100%), correlating with PLAG1 gene rearrangement [17, 23] (Fig. 6b), but is negative in soft tissue myoepitheliomas [23, 24]. Among cutaneous mixed tumors, PLAG1 expression appears to be characteristic of apocrine type tumors, but is consistently negative in eccrine-type mixed tumors [14]. The variant of cutaneous syncytial myoepithelioma has the distinctive immunophenotype of consistent positivity for EMA and S-100 protein, but overall negative for keratin with rare staining in only up to 12% [4, 12]. SMARCB1 loss of expression is observed in a subset of myoepithelial carcinomas [3, 25, 26] (Fig. 9c), corresponding to genomic SMARCB1 inactivation, as well as likely functional loss of material on chromosome 22q11.2 secondary to EWSR1 rearrangement in some cases.
Molecular Features
In the past decade, molecular studies have suggested that some soft tissue and salivary myoepithelial neoplasms are genetically related. Soft tissue mixed tumors (with ductal differentiation) and cutaneous chondroid syringomas (specifically apocrine-type) have rearrangements of PLAG1 (encoded on chromosome 8q12) [17, 23], which are characteristic of salivary pleomorphic adenoma [27,28,29,30] and carcinoma ex pleomorphic adenoma [31, 32.] LIFR is an occasional fusion partner to PLAG1 in both soft tissue and salivary tumors [17, 30]. While HMGA2 rearrangement occurs in a subset of salivary pleomorphic adenoma and carcinoma ex pleomorphic adenoma [33, 34], to date this alteration has not been identified in soft tissue mixed tumors [17], although a single case of apocrine-type chondroid syringoma has been reported to overexpress HMGA2 by immunohistochemistry [14].
Rearrangement of the EWSR1 gene (encoded on chromosome 22q) occurs in nearly half of all myoepithelial tumors of soft tissue [7, 20, 35,36,37,38,39], as well as skin [11, 12, 40] and bone [7,8,9, 35, 41]. A small subset of cases have alternate FUS rearrangements in lieu of EWSR1 [9, 42]. In the largest study to date, POU5F1 and PBX1 were identified as the most common fusion partners, each reported to occur in up to 16% cases [7]. Other documented fusion partners thus far are ZNF444, KLF17, ATF1, and PBX3 [7, 35, 36, 40,41,42].
EWSR1 rearrangement has also been reported in up to 39% of primary salivary myoepithelial carcinomas having clear cell morphology, though the fusion partners are currently unknown [43]. Rearrangements involving PLAG1 are most common overall in salivary myoepithelial carcinomas (at least 50%), in both that arise de novo and ex pleomorphic adenoma; HMGA2 fusions are much rarer [44]. The most frequent fusion partners are FGFR1 (18%) and TGFBR3 (15%) [44]. PLAG1 rearrangements have not been identified in soft tissue myoepitheliomas and myoepithelial carcinomas that lack tubuloductal differentiation [45, 46]. Despite EWSR1 rearrangements being shared by soft tissue myoepithelial tumors and a subset of salivary myoepithelial carcinomas, the prevalence of PLAG1 fusion in the latter highlight that there are likely differences in initiating pathogenetic events between the two.
These molecular insights have raised some suggestions of genotype–phenotype correlations for subsets of soft tissue myoepithelial neoplasms, although data is still limited. Tumors with EWSR1-POU5F1 fusions tend to present in deep soft tissues of the extremities in young patients, and show nested growth of epithelioid cells with clear cytoplasm [7]. Myoepithelial tumors with EWSR1-PBX1 show a deceptively bland spindle cell appearance within a prominent sclerotic stroma [7]. A small number of tumors with EWSR1-PBX3 have been described to show fascicular or nested arrangement of spindled or epithelioid cells within a collagenous or myxoid stroma, often in osseous sites [35]. Additionally, cutaneous syncytial myoepitheliomas have consistent EWSR1-PBX3 fusions [40].
Among myoepithelial carcinomas lacking EWSR1 rearrangements, a subset (60%) of tumors that show immunohistochemical loss of SMARCB1 are characterized by homozygous deletions of SMARCB1 [26].
Prognosis
There are many similarities, but also some differences in the biologic behavior and prognostication of soft tissue and salivary myoepithelial neoplasms. Overall, soft tissue and cutaneous myoepitheliomas and mixed tumors typically follow a benign clinical course with complete resection [1, 2, 4, 5, 10,11,12]. The overall recurrence risk is 18%, and is increased with incomplete resection; distant metastasis is exceptionally rare [2, 4]. Salivary pleomorphic adenoma also shows low recurrence rates with complete resection, although tumor disruption and spillage of salivary pleomorphic adenomas are associated with recurrence risks of up to 80% [47] which has not been observed for benign soft tissue myoepithelial neoplasms. While some cases of salivary pleomorphic adenoma and myoepithelioma may show malignant transformation [48], and metastasis of tumors lacking malignant morphology [49], these phenomena are not appreciably described in primary soft tissue myoepithelial tumors.
Myoepithelial carcinoma of soft tissue show overall aggressive behavior and show recurrence rates of up to 42% and distant metastases in up to 52% of patients [2, 3]. Based on the largest series to date, the presence of cytologic atypia is the single most reliable predictor of malignant behavior, and risks of recurrence and metastasis appear irrespective of histologic grade or margin status. Reported sites of distant metastasis include lung, liver, lymph node, bone, brain, and soft tissue, with disease-related death occurring in 13–43% of patients [2, 3]. Malignant progression of benign skin and soft tissue myoepithelial tumors has not been well characterized and areas of morphologically benign precursors are rare within myoepithelial carcinoma of soft tissue. In contrast, at least half of all salivary myoepithelial carcinomas are recognized to arise ex pleomorphic adenoma [15] (though progression of intracapsular carcinoma to minimally invasive and then widely invasive carcinoma), and comprise the second most common morphology of carcinoma ex pleomorphic adenoma after salivary duct carcinoma. The behavior of salivary myoepithelial carcinoma is overall aggressive, with risks of recurrence and distant metastases of 27% and 33%, respectively [15]. The presence of necrosis correlates with more aggressive behavior, and worse clinical outcomes are associated with myoepithelial carcinoma ex pleomorphic adenoma compared to tumors arising de novo [15].
Differential Diagnosis
The differential diagnosis for myoepithelial neoplasms is broad due to the wide morphologic spectrum of myoepithelial tumors, and this review focuses on entities more common in the head and neck and specific considerations in distinguishing soft tissue and salivary primary sites. Although the characteristic architectural and cytologic heterogeneity (particularly within a tumor) may be a distinctive feature, the diagnosis of soft tissue myoepithelioma, mixed tumor, and myoepithelial carcinoma often requires an inclusive immunohistochemical panel and correlation with clinical data; molecular testing may be helpful in specific scenarios.
The presence of tubuloductal differentiation clearly distinguishes soft tissue mixed tumor from soft tissue myoepithelioma, although diagnostic areas of tubuloductal differentiation may be very focal. Given the similarities in biologic behavior, distinction between the two is not crucial. However, in head and neck practice, the diagnosis of soft tissue myoepithelioma and mixed tumor should not be made before excluding the possibility of a primary or recurrent salivary tumor, and in non-salivary sites the rare occurrence of “metastasizing pleomorphic adenoma.” Most reported cases of metastasizing pleomorphic adenoma are characterized by a clinical course of repeated local recurrences of an otherwise “benign” appearing pleomorphic adenoma; the most common sites of distant metastases are bone, head and neck, and lung [49, 50]. Given the shared morphologic, immunohistochemical, and genetic features of soft tissue and salivary counterparts, distinction may rely solely on clinical correlation.
In some scenarios, it may be difficult to distinguish between salivary myoepithelial carcinoma and soft tissue myoepithelial carcinoma; similarly, a prior history of a salivary primary should always favor the former. Myoepithelial carcinoma is the second-most common histologic type of carcinoma ex pleomorphic adenoma, and a subset can be identified by positive PLAG1 and HMGA2 immunohistochemical staining or identification of corresponding fusion genes. EWSR1 rearrangements may occur in both soft tissue and salivary lesions, although more rarely in the latter and tend to be associated with clear cell morphology [43]. Aside from detection of cases with PLAG1 and HMGA2 rearrangements, the presence of residual areas of precursor pleomorphic adenoma is the single most useful feature in recognizing salivary myoepithelial carcinoma ex pleomorphic adenoma. Thorough sampling and histologic examination for residual areas of precursor pleomorphic adenoma is recommended for tumors arising in the cheek or neck, especially because residual foci of pleomorphic adenomas may appear extremely subtle with near-complete hyalinization.
Outside of the salivary gland, both soft tissue myoepithelioma and myoepithelial carcinoma overlap with a broad range of mesenchymal neoplasms. The chief considerations are extraskeletal myxoid chondrosarcoma, ossifying fibromyxoid tumor, and proximal-type epithelioid sarcoma, as well as some primary bone tumors. In adults, carcinoma and melanoma often must be excluded. There are also specific diagnostic considerations for pediatric myoepithelial carcinomas, especially those having prominent round cell morphology. Inclusive immunohistochemical panels are helpful in resolving most diagnostic scenarios, and molecular testing may be useful in some contexts (see Table 1).
Extraskeletal myxoid chondrosarcoma (EMC) is very rare in the head and neck, and is characterized by a reticular growth pattern of uniform ovoid-to-round cells that appear to interconnect by their elongated bipolar and stellate cytoplasmic processes. EMC shows an overall lobular architecture, and the tumor cells are embedded in a predominantly myxoid stroma. Most cases show uniform cytomorphology, although rare high-grade variants of EMC may show hypercellularity, epithelioid morphology, and increased nuclear atypia, which are much harder to distinguish from myoepithelial carcinoma. While most myoepithelial neoplasms show cytologic and architectural heterogeneity, a predominant reticular architecture may be present in some cases. Differences in the immunophenotypes of EMC and myoepithelial carcinoma are helpful. While EMC can show rare S-100 and EMA staining, EMC is consistently negative for keratin, GFAP, and p63 [19]. EMC harbors NR4A3-EWSR1 fusions; while EWSR1 FISH cannot distinguish between EMC and myoepithelial neoplasms, detection of NR4A3 rearrangement is diagnostic of EMC [51].
OFMT shows a multilobular growth of predominantly ovoid tumor cells arranged in cords and trabeculae within a fibromyxoid stroma. Most tumors are surrounded by a peripheral but incomplete shell of lamellar bone, however the bony shell is absent in some cases and 15% of myoepithelial neoplasms can show heterologous osseous differentiation. OFMTs that are designated as “atypical” and “malignant” show hypercellularity, solid growth, and cytologic atypia, as well as irregularly distributed of bone within tumor lobules and between tumor cells [52]. While OFMT shows some overlapping immunohistochemical features with myoepithelial tumors, being also positive for S-100 with variable expression for keratin and GFAP, desmin is frequently positive (50%) in OFMT but absent in most myoepithelial neoplasms. Challenging cases can be resolved by molecular studies; OFMT harbors PHF1 rearrangements [53, 54], including a subset of cases with PHF1-TFE3 fusion [55]. Rare variant fusions, including ZC3H7B-BCOR, CREBBP-BCORL1 and KDM2A-WWTR1 have also been reported [56, 57].
The proximal-type variant of epithelioid sarcoma may arise in the differential diagnosis of soft tissue myoepithelial carcinomas. Proximal-type epithelioid sarcoma appears as a sheetlike or multinodular growth of uniform but atypical large epithelioid cells having vesicular nuclei, prominent nucleoli, and abundant eosinophilic cytoplasm. Some examples may show prominent rhabdoid morphology and myxoid stroma, which that especially resemble myoepithelial carcinoma. Epithelioid sarcoma is positive for keratin and EMA, however in contrast to myoepithelial carcinoma, it is negative for S-100, GFAP, and SOX10 [18] and only rarely shows weak p63 staining [19]. Approximately half of all epithelioid sarcomas are positive for CD34. Loss of expression of SMARCB1 is characteristic of epithelioid sarcoma [25], secondary to homozygous SMARCB1 deletions [26]. While most cases can be resolved by immunohistochemistry, a subset of EWSR1 non-rearranged myoepithelial carcinomas have identical SMARCB1 deletions as epithelioid sarcoma and show SMARCB1 expression [26]. Molecular testing is helpful for detecting cases with EWSR1 rearrangement.
Carcinoma and melanoma may need to be excluded, especially in older patients. Keratin expression in myoepithelial carcinoma can be misleading, especially if other myoepithelial markers have not been performed. Clinical correlation is required and differentiation-specific immunohistochemical markers are helpful in most cases (e.g. TTF1 for lung). The presence of myxoid stroma and multinodular growth should favor myoepithelial carcinoma, and S-100, GFAP, and SOX10 should be included in the work-up. In the head and neck, SMARCB1-deficient sinonasal carcinoma may enter the differential diagnosis, particularly those showing predominantly plasmacytoid or rhabdoid morphology, nested or solid growth, or glandular differentiation [58]. SMARCB1-deficient sinonasal carcinoma is keratin-positive and can show variable p63 staining, but are negative for S-100 and SOX10. SMARCB1 is definitionally lost in SMARCB1-deficient sinonasal carcinoma, but is only lost in a small subset of myoepithelial carcinoma. NUT carcinoma may also be considered, and its characteristic foci of abrupt squamous keratinization may resemble heterologous squamous differentiation in myoepithelial neoplasms. Diffuse nuclear staining for NUT by immunohistochemistry, particularly in a speckled chromatin pattern, is diagnostic; identification of NUTM1 rearrangement can also confirm the diagnosis. While malignant melanoma may resemble myoepithelial carcinoma, most cases show expression of melanocytic-specific markers HMB-45 and Melan A and are negative for keratin and EMA; furthermore, myxoid stroma is also rare.
Some primary bone tumors may show overlapping features with myoepithelial neoplasms, especially in the head and neck. Chondromyxoid fibroma may arise in craniofacial sites, though they most commonly present as metaphyseal tumors in the long bones [59]. Tumors are multilobulated with reticular growth of uniform spindle or stellate cells set in a myxoid matrix. While chondromyxoid fibromas are positive for S-100, they are generally negative for keratin, EMA, and GFAP. Chordomas arising in the cervical spine may be sampled as a “neck mass,” and are characterized by a heterogeneous population of tumor cells ranging from epithelioid cells with small round nuclei and abundant eosinophilic cytoplasm and “physaliferous” cells having abundant vacuolated cytoplasm, with a prominent myxoid stroma. Moreover, poorly differentiated chordomas show increased atypia and solid growth, closely resembling myoepithelial carcinoma. While chordoma is also positive for keratin, EMA, and S-100, brachyury is a sensitive and specific marker for chordoma [60].
In pediatric patients, myoepithelial carcinomas raise a broader differential diagnosis. Extrarenal malignant rhabdoid tumor may rarely be considered in very young patients (3 years or younger), which shows sheets of large epithelioid and polygonal cells with round nuclei, prominent nucleoli, and abundant eosinophilic cytoplasm with frequent hyaline inclusions. Similarly to myoepithelial carcinoma, malignant rhabdoid tumors show variable expression of epithelial markers and S-100. While SMARCB1 loss of expression secondary to SMARCB1 alterations are present in malignant rhabdoid tumor [61], these changes are infrequent in myoepithelial carcinoma and most cases can be distinguished by the presence of cytologic and architectural heterogeneity and identification of EWSR1 rearrangement, when present. Since round cell morphology is present in a subset of myoepithelial carcinomas in pediatric patients, a range of round cell sarcomas may need to be excluded, especially those that show keratin expression with some frequency. Most round cell sarcomas are translocation-associated and show overall cytologic uniformity, which is not a feature of most myoepithelial carcinomas. Immunohistochemistry and molecular testing can resolve the most common alternate diagnoses of Ewing sarcoma (diffuse membranous CD99 staining, NKX2.2 and FLI1 positivity; EWSR1-FLI1 fusion), alveolar rhabdomyosarcoma (diffuse desmin and myogenin positivity; FOXO1 rearrangement); poorly differentiated synovial sarcoma (diffuse nuclear TLE1 positivity; SS18 rearrangement); and CIC-rearranged sarcoma (WT1 and ETV4 staining; CIC rearrangement).
Summary
Primary soft tissue and salivary myoepithelial neoplasms share clinicopathologic features and molecular studies have established that the two groups are clearly related. Some differences remain between soft tissue and salivary counterparts, including pathogenesis (given that most soft tissue myoepithelial carcinomas appear to arise de novo) and criteria for malignancy. The differential diagnosis for soft tissue myoepithelial neoplasms is broad, including a wide range of other mesenchymal tumors, as well as specific considerations in head and neck pathology. While the presence of rearrangements of PLAG1 and EWSR1 in soft tissue mixed tumor and myoepithelioma/myoepithelial carcinoma are helpful in many contexts, these alterations are not entirely specific in the differential diagnosis. Clinical correlation and a broad immunohistochemical panel to identify co-expression of epithelial markers and S-100/GFAP/SOX10 is important for accurate identification of soft tissue myoepithelial tumors.
References
Kilpatrick SE, Hitchcock MG, Kraus MD, et al. Mixed tumors and myoepitheliomas of soft tissue: a clinicopathologic study of 19 cases with a unifying concept. Am J Surg Pathol. 1997;21:13–22.
Hornick JL, Fletcher CD. Myoepithelial tumors of soft tissue: a clinicopathologic and immunohistochemical study of 101 cases with evaluation of prognostic parameters. Am J Surg Pathol. 2003;27:1183–96.
Gleason BC, Fletcher CD. Myoepithelial carcinoma of soft tissue in children: an aggressive neoplasm analyzed in a series of 29 cases. Am J Surg Pathol. 2007;31:1813–24.
Hornick JL, Fletcher CD. Cutaneous myoepithelioma: a clinicopathologic and immunohistochemical study of 14 cases. Hum Pathol. 2004;35:14–24.
Michal M, Miettinen M. Myoepitheliomas of the skin and soft tissues. Report of 12 cases. Virchows Arch. 1999;434:393–400.
Bisogno G, Tagarelli A, Schiavetti A, et al. Myoepithelial carcinoma treatment in children: a report from the TREP project. Pediatr Blood Cancer. 2014;61:643–6.
Antonescu CR, Zhang L, Chang NE, et al. EWSR1-POU5F1 fusion in soft tissue myoepithelial tumors. A molecular analysis of sixty-six cases, including soft tissue, bone, and visceral lesions, showing common involvement of the EWSR1 gene. Genes Chromosomes Cancer. 2010;49:1114–24.
Kurzawa P, Kattapuram S, Hornicek FJ, et al. Primary myoepithelioma of bone: a report of 8 cases. Am J Surg Pathol. 2013;37:960–8.
Puls F, Arbajian E, Magnusson L, et al. Myoepithelioma of bone with a novel FUS-POU5F1 fusion gene. Histopathology. 2014;65:917–22.
Mentzel T, Requena L, Kaddu S, et al. Cutaneous myoepithelial neoplasms: clinicopathologic and immunohistochemical study of 20 cases suggesting a continuous spectrum ranging from benign mixed tumor of the skin to cutaneous myoepithelioma and myoepithelial carcinoma. J Cutan Pathol. 2003;30:294–302.
Flucke U, Palmedo G, Blankenhorn N, et al. EWSR1 gene rearrangement occurs in a subset of cutaneous myoepithelial tumors: a study of 18 cases. Mod Pathol. 2011;24:1444–50.
Jo VY, Antonescu CR, Zhang L, et al. Cutaneous syncytial myoepithelioma: clinicopathologic characterization in a series of 38 cases. Am J Surg Pathol. 2013;37:710–8.
Hassab-el-Naby HM, Tam S, White WL, et al. Mixed tumors of the skin. A histological and immunohistochemical study. Am J Dermatopathol. 1989;11:413–28.
Russell-Goldman E, Dubuc A, Hanna J. Differential expression of PLAG1 in apocrine and eccrine cutaneous mixed tumors: evidence for distinct molecular pathogenesis. Am J Dermatopathol. 2019. https://doi.org/10.1097/dad.0000000000001393.
Kong M, Drill EN, Morris L, et al. Prognostic factors in myoepithelial carcinoma of salivary glands: a clinicopathologic study of 48 cases. Am J Surg Pathol. 2015;39:931–8.
Xu B, Mneimneh W, Torrence DE, et al. Misinterpreted Myoepithelial Carcinoma of Salivary Gland: A Challenging and Potentially Significant Pitfall. Am J Surg Pathol. 2019;43:601–9.
Antonescu CR, Zhang L, Shao SY, et al. Frequent PLAG1 gene rearrangements in skin and soft tissue myoepithelioma with ductal differentiation. Genes Chromosomes Cancer. 2013;52:675–82.
Miettinen M, McCue PA, Sarlomo-Rikala M, et al. Sox10-A marker for not only schwannian and melanocytic neoplasms but also myoepithelial cell tumors of soft tissue: a systematic analysis of 5134 Tumors. Am J Surg Pathol. 2015;39:826.
Jo VY, Fletcher CD. p63 immunohistochemical staining is limited in soft tissue tumors. Am J Clin Pathol. 2011;136:762–6.
Rekhi B, Sable M, Jambhekar NA. Histopathological, immunohistochemical and molecular spectrum of myoepithelial tumours of soft tissues. Virchows Arch. 2012;461:687–97.
Bilal H, Handra-Luca A, Bertrand JC, et al. P63 is expressed in basal and myoepithelial cells of human normal and tumor salivary gland tissues. J Histochem Cytochem. 2003;51:133–9.
Genelhu MC, Gobbi H, Soares FA, et al. Immunohistochemical expression of p63 in pleomorphic adenomas and carcinomas ex-pleomorphic adenomas of salivary glands. Oral Oncol. 2006;42:154–60.
Bahrami A, Dalton JD, Krane JF, et al. A subset of cutaneous and soft tissue mixed tumors are genetically linked to their salivary gland counterpart. Genes Chromosomes Cancer. 2012;51:140–8.
Matsuyama A, Hisaoka M, Hashimoto H. PLAG1 expression in cutaneous mixed tumors: an immunohistochemical and molecular genetic study. Virchows Arch. 2011;459:539–45.
Hornick JL, Dal Cin P, Fletcher CD. Loss of INI1 expression is characteristic of both conventional and proximal-type epithelioid sarcoma. Am J Surg Pathol. 2009;33:542–50.
Le Loarer F, Zhang L, Fletcher CD, et al. Consistent SMARCB1 homozygous deletions in epithelioid sarcoma and in a subset of myoepithelial carcinomas can be reliably detected by FISH in archival material. Genes Chromosomes Cancer. 2014;53:475–86.
Astrom AK, Voz ML, Kas K, et al. Conserved mechanism of PLAG1 activation in salivary gland tumors with and without chromosome 8q12 abnormalities: identification of SII as a new fusion partner gene. Cancer Res. 1999;59:918–23.
Debiec-Rychter M, Van Valckenborgh I, Van den Broeck C, et al. Histologic localization of PLAG1 (pleomorphic adenoma gene 1) in pleomorphic adenoma of the salivary gland: cytogenetic evidence of common origin of phenotypically diverse cells. Lab Invest. 2001;81:1289–97.
Kas K, Voz ML, Roijer E, et al. Promoter swapping between the genes for a novel zinc finger protein and beta-catenin in pleiomorphic adenomas with t(3;8)(p21;q12) translocations. Nat Genet. 1997;15:170–4.
Voz ML, Astrom AK, Kas K, et al. The recurrent translocation t(5;8)(p13;q12) in pleomorphic adenomas results in upregulation of PLAG1 gene expression under control of the LIFR promoter. Oncogene. 1998;16:1409–16.
Martins C, Fonseca I, Roque L, et al. PLAG1 gene alterations in salivary gland pleomorphic adenoma and carcinoma ex-pleomorphic adenoma: a combined study using chromosome banding, in situ hybridization and immunocytochemistry. Mod Pathol. 2005;18:1048–55.
Bahrami A, Dalton JD, Shivakumar B, et al. PLAG1 alteration in carcinoma ex pleomorphic adenoma: immunohistochemical and fluorescence in situ hybridization studies of 22 cases. Head Neck Pathol. 2012;6:328–35.
Geurts JM, Schoenmakers EF, Roijer E, et al. Expression of reciprocal hybrid transcripts of HMGIC and FHIT in a pleomorphic adenoma of the parotid gland. Cancer Res. 1997;57:13–7.
Katabi N, Ghossein R, Ho A, et al. Consistent PLAG1 and HMGA2 abnormalities distinguish carcinoma ex-pleomorphic adenoma from its de novo counterparts. Hum Pathol. 2015;46:26–33.
Agaram NP, Chen HW, Zhang L, et al. EWSR1-PBX3: a novel gene fusion in myoepithelial tumors. Genes Chromosomes Cancer. 2015;54:63–71.
Flucke U, Mentzel T, Verdijk MA, et al. EWSR1-ATF1 chimeric transcript in a myoepithelial tumor of soft tissue: a case report. Hum Pathol. 2012;43:764–8.
Thway K, Bown N, Miah A, et al. Rhabdoid variant of myoepithelial carcinoma, with EWSR1 rearrangement: expanding the spectrum of EWSR1-rearranged myoepithelial tumors. Head Neck Pathol. 2015;9:273–9.
Brandal P, Panagopoulos I, Bjerkehagen B, et al. Detection of a t(1;22)(q23;q12) translocation leading to an EWSR1-PBX1 fusion gene in a myoepithelioma. Genes Chromosomes Cancer. 2008;47:558–64.
Brandal P, Panagopoulos I, Bjerkehagen B, et al. t(19;22)(q13;q12) Translocation leading to the novel fusion gene EWSR1-ZNF444 in soft tissue myoepithelial carcinoma. Genes Chromosomes Cancer. 2009;48:1051–6.
Jo VY, Antonescu CR, Dickson BC, et al. Cutaneous syncytial myoepithelioma is characterized by recurrent EWSR1-PBX3 fusions. Am J Surg Pathol. 2019;43:1349–54.
Yun S, Kim SH, Cho HS, et al. EWSR1-PBX3 fused myoepithelioma arising in metatarsal bone: case report and review of the literature. Pathol Int. 2019;69:42–7.
Huang SC, Chen HW, Zhang L, et al. Novel FUS-KLF17 and EWSR1-KLF17 fusions in myoepithelial tumors. Genes Chromosomes Cancer. 2015;54:267–75.
Skalova A, Weinreb I, Hyrcza M, et al. Clear cell myoepithelial carcinoma of salivary glands showing EWSR1 rearrangement: molecular analysis of 94 salivary gland carcinomas with prominent clear cell component. Am J Surg Pathol. 2015;39:338–48.
Dalin MG, Katabi N, Persson M, et al. Multi-dimensional genomic analysis of myoepithelial carcinoma identifies prevalent oncogenic gene fusions. Nat Commun. 2017;8:1197.
Hallor KH, Teixeira MR, Fletcher CD, et al. Heterogeneous genetic profiles in soft tissue myoepitheliomas. Mod Pathol. 2008;21:1311–9.
Matsuyama A, Hisaoka M, Hashimoto H. PLAG1 expression in mesenchymal tumors: an immunohistochemical study with special emphasis on the pathogenetical distinction between soft tissue myoepithelioma and pleomorphic adenoma of the salivary gland. Pathol Int. 2012;62:1–7.
Riad MA, Abdel-Rahman H, Ezzat WF, et al. Variables related to recurrence of pleomorphic adenomas: outcome of parotid surgery in 182 cases. Laryngoscope. 2011;121:1467–72.
Gnepp DR. Malignant mixed tumors of the salivary glands: a review. Pathol Annu. 1993;28(Pt 1):279–328.
Knight J, Ratnasingham K. Metastasising pleomorphic adenoma: systematic review. Int J Surg. 2015;19:137–45.
Manucha V, Ioffe OB. Metastasizing pleomorphic adenoma of the salivary gland. Arch Pathol Lab Med. 2008;132:1445–7.
Flucke U, Tops BB, Verdijk MA, et al. NR4A3 rearrangement reliably distinguishes between the clinicopathologically overlapping entities myoepithelial carcinoma of soft tissue and cellular extraskeletal myxoid chondrosarcoma. Virchows Arch. 2012;460:621–8.
Folpe AL, Weiss SW. Ossifying fibromyxoid tumor of soft parts: a clinicopathologic study of 70 cases with emphasis on atypical and malignant variants. Am J Surg Pathol. 2003;27:421–31.
Gebre-Medhin S, Nord KH, Moller E, et al. Recurrent rearrangement of the PHF1 gene in ossifying fibromyxoid tumors. Am J Pathol. 2012;181:1069–77.
Graham RP, Weiss SW, Sukov WR, et al. PHF1 rearrangements in ossifying fibromyxoid tumors of soft parts: a fluorescence in situ hybridization study of 41 cases with emphasis on the malignant variant. Am J Surg Pathol. 2013;37:1751–5.
Suurmeijer AJH, Song W, Sung YS, et al. Novel recurrent PHF1-TFE3 fusions in ossifying fibromyxoid tumors. Genes Chromosomes Cancer. 2019;58:643–9.
Antonescu CR, Sung YS, Chen CL, et al. Novel ZC3H7B-BCOR, MEAF6-PHF1, and EPC1-PHF1 fusions in ossifying fibromyxoid tumors–molecular characterization shows genetic overlap with endometrial stromal sarcoma. Genes Chromosomes Cancer. 2014;53:183–93.
Kao YC, Sung YS, Zhang L, et al. Expanding the molecular signature of ossifying fibromyxoid tumors with two novel gene fusions: cREBBP-BCORL1 and KDM2A-WWTR1. Genes Chromosomes Cancer. 2017;56:42–50.
Agaimy A, Hartmann A, Antonescu CR, et al. SMARCB1 (INI-1)-deficient sinonasal carcinoma: a series of 39 cases expanding the morphologic and clinicopathologic spectrum of a recently described entity. Am J Surg Pathol. 2017;41:458–71.
Meredith DM, Fletcher CDM, Jo VY. Chondromyxoid fibroma arising in craniofacial sites: a clinicopathologic analysis of 25 cases. Am J Surg Pathol. 2018;42:392–400.
Tirabosco R, Mangham DC, Rosenberg AE, et al. Brachyury expression in extra-axial skeletal and soft tissue chordomas: a marker that distinguishes chordoma from mixed tumor/myoepithelioma/parachordoma in soft tissue. Am J Surg Pathol. 2008;32:572–80.
Biegel JA, Tan L, Zhang F, et al. Alterations of the hSNF5/INI1 gene in central nervous system atypical teratoid/rhabdoid tumors and renal and extrarenal rhabdoid tumors. Clin Cancer Res. 2002;8:3461–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Vickie Y. Jo declares that she has no conflicts of interest to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jo, V.Y. Soft Tissue Special Issue: Myoepithelial Neoplasms of Soft Tissue: An Updated Review with Emphasis on Diagnostic Considerations in the Head and Neck. Head and Neck Pathol 14, 121–131 (2020). https://doi.org/10.1007/s12105-019-01109-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-019-01109-y