Abstract
Microcystic adnexal carcinoma (MAC) occurs predominantly in the centrofacial skin and has been only rarely reported in mucosal surfaces. We here present a 5 case series of tumors closely resembling MAC occurring in the mucosal surfaces of the head and neck, which we have termed sclerosing microcystic adenocarcinomas. These tumors showed a predilection for women (4:1) with an average patient age of 52.6 years (range 41–73 years). Location included the tongue (n = 2), the floor of the mouth (n = 2), and the nasopharynx/clivus (n = 1). One occurred after radiation therapy and another occurred in the setting of immune compromise. Immunohistochemistry highlighted a dual cell population with luminal cells showing positivity for high and low-molecular weight keratins and surrounding myoepithelial cells showing S100 and smooth muscle actin staining. No cases had nodal involvement, and the single patient with clinical follow-up was alive and free of disease 34 months after diagnosis and definitive radiochemotherapy. Differential diagnoses for all cases diverged from those provoked by MAC in the skin and included a variety of salivary gland neoplasms such as adenoid cystic carcinoma, polymorphous low grade adenocarcinoma, and mucoepidermoid carcinoma. Recognition of sclerosing microcystic adenocarcinoma in the head and neck mucosa is critical given its bland appearance and subtle infiltration pattern, infrequency of nodal involvement, and behavioral differences from the other entities on the differential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microcystic adnexal carcinoma (MAC) is a rare neoplasm that most often arises in the central facial skin of middle-aged and older adults [1–6]. It is most common among Caucasians and shows a slight female predominance. These tumors are histologically characterized by minimally atypical cells arranged in thin strands and angulated ducts, many of which contain intraluminal eosinophilic secretions. MACs show a relative paucity of neoplastic cells with scattered invasive cords and ducts percolating through a background of densely sclerotic stroma. This infiltrative pattern corresponds with their clinical behavior: MACs characteristically show extensive invasion and local destruction and are prone to recurrence. This insidious, locally-aggressive course necessitates lifetime monitoring for and management of recurrence even after resection and therapy [1–6].
In the skin, the bland morphology and very subtle infiltration pattern of MACs may lead to diagnostic confusion with benign entities such as syringoma, desmoplastic trichoepithelioma, and trichoadenoma [2, 3, 6]. This morphologic overlap can be particularly problematic in superficial biopsies that fail to fully demonstrate the deeply infiltrative nature of the tumor. Diagnostic difficulties are compounded when MAC arises in alternate locations where it may not come to mind as a consideration. For instance, MAC has been documented in the breast and the vulva, where it can be mistaken for more conventional adenocarcinomas of these locales [7, 8]. Other potentially problematic primary sites include head and neck locations outside the skin. There are rare reports of MAC occurring in the extracutaneous head and neck including a single report of MAC occurring in the tongue and another from the parotid gland [9, 10]. We here report a 5-case series of MAC-like tumors arising in the mucosal surfaces of the head and neck. To our knowledge, this is the first case series of MAC-like carcinomas arising in the mucosal head and neck and the first report occurring in the nasopharynx. Because these tumors are not thought to be adnexal in derivation, we have proposed the name “sclerosing microcystic adenocarcinoma.” In addition, we review prior reports of MAC-like tumors involving the head and neck mucosa and salivary glands and discuss the differential diagnosis for this entity in this region.
Materials and Methods
A retrospective computerized search of the University of Virginia Health System Surgical Pathology internal and consultative files was conducted to identify all diagnosed cases of mucosal MAC-like tumors occurring in the head and neck between 12/2003 and 1/2016. An additional case was contributed from the Department of Pathology, University of Erlangen, Germany following presentation of this work at the 2013 United States and Canadian Academy of Pathology. The diagnosis was confirmed primarily based on the presence of morphologic features identical to those of cutaneous MAC as interpreted by expert reviewers (S.E.M. and M.W.W.): chiefly, bland and mitotically inactive cells arranged in infiltrative cords, ducts, and microcystic structures (often with eosinophilic intraluminal secretions) and set in a background of abundant densely collagenized to focally desmoplastic stroma. This work was approved by the Institutional Review Board of the University of Virginia.
Results
A total of 5 cases were identified (Table 1). Two were biopsies from the tongue, 2 were from the floor-of-the mouth, and a single case was from the nasopharynx and clivus. Four cases occurred in women and 1 occurred in a man. Patient age in our series ranged from 41 to 73 years (mean 52.6 years). Because all specimens were derived from consultative material, clinical follow-up was not available for the majority of cases although one patient (Case 5) was alive and well without evidence of recurrence 34 months status-post resection and chemoradiation. Furthermore, available immunohistochemical stains were somewhat variable due to the consultative nature of the material. Additional case details are as follows:
Case 1
A 41-year-old woman presented with a mass at the base of her tongue. The patient had undergone resection and radiotherapy for adenoid cystic carcinoma involving the soft palate 7 years previously. Histologic sections of the tongue base biopsy demonstrated diffuse involvement of the normal lingual submucosa by a proliferation of bland cuboidal cells arranged in nests and tubules, a few of which contained dense, globular eosinophilic material (Fig. 1). The tubules were lined by cuboidal cells with round to oval nuclei, evenly dispersed chromatin, and occasional prominent nucleoli with a surrounding myoepithelial layer. Mitotic figures were rare. Perineural and skeletal muscle invasion was present (Fig. 2). Given the history of adenoid cystic carcinoma, an immunohistochemical stain with CD117 was performed, which was non-immunoreactive. No lymph nodes were involved.
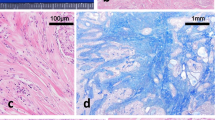
The morphologic features of sclerosing microcystic adenocarcinoma. a Case 1; b Case 3; c Case 4; d Case 5. All cases showed a proliferation of bland cells arranged in infiltrating strands and ducts, often with associated microcystic spaces filled with intraluminal secretions. Mitotic figures were very rare, with the figure identified near the center of image (a) representing one of the only ones identified in this series. All cases showed abundant dense stroma which ranged from the paler, basophilic desmoplasia that predominates in image (a) to the more densely collagenized stroma in image (b). Images (c, d) illustrate an admixture of these two stromal types, with paler desmoplastic halos immediately surrounding the tumor infiltrates and a denser, more collagenized background. All cases included areas of extensive but remarkably subtle infiltration—well illustrated in image (b)—wherein the neoplastic ducts could easily be mistaken for vessels
The infiltrative patterns of sclerosing microcystic adenocarcinoma. a Several sclerosing microcystic adenocarcinomas showed close association with minor salivary glands (Case 4 pictured). b All cases showed percolation of neoplastic ducts deep within the submucosa, in some cases frankly abutting or invading the skeletal muscle (Case 4 pictured). c Perineural invasion was focally present in some cases (Case 1 pictured)
Case 2
A 47-year-old woman presented with a tongue lesion. Microscopically, the tumor was embedded among normal salivary glands and was comprised of an invasive proliferation of epithelial tubules lined by cuboidal cells with evenly dispersed chromatin and occasional prominent nucleoli. An attenuated myoepithelial layer was appreciable around most of the invasive ducts. Rare mitotic figures were identified. Although perineural invasion was not appreciated in this limited sample, extensive invasion into the underlying skeletal muscle was identified. Nodal involvement was not identified.
Case 3
A 73-year-old man presented with an 8 month history of diplopia. An MRI scan showed a 3.9 × 3.8 × 2.9 cm gadolinium-enhancing mass of the clivus/sphenoid body with involvement of the cavernous sinus and nasopharynx, as well as intracranial extension. Histologic sections of biopsies from the nasopharynx and clivus revealed invasive strands, nests, and microcysts comprised of bland cuboidal cells with surrounding myoepithelial cells admixed with normal mucosal tissue. The microcystic spaces focally contained eosinophilic luminal secretory material. This neoplastic proliferation was embedded in a densely hyalinized to desmoplastic stroma (Fig. 1). Mitotic figures were not readily identified. Immunohistochemical staining revealed positivity for cytokeratin cocktail and BerEP4 with negative immunoreactivity with antibodies to KIT (CD117), CK20, and CEA. S100 focally marked the myoepithelial layer. There was no evidence of nodal involvement.
Case 4
A 54-year-old woman presented with a floor-of-mouth lesion. Histologic sections showed predominantly benign salivary tissue with a subtle infiltrate of neoplastic cords and ducts which focally contained eosinophilic secretions (Fig. 2). The background stroma was densely sclerotic with halos of desmoplasia surrounding the infiltrative cells. Immunohistochemistry revealed positivity for keratin cocktail within the central ductal and nested cells with a thin rim of smooth muscle actin (SMA) positivity in the surrounding myoepithelial layer (Fig. 3). No lymph nodes were involved.
Immunohistochemical staining of sclerosing microcystic adenocarcinoma. a 40 × view of a neoplastic duct bearing a two cell layer and prominent intraluminal secretions. b The tumor cells show strong diffuse positivity for cytokeratin cocktail. c Smooth muscle actin (SMA) highlights the peripheral myoepithelial cell layer
Case 5
A 48-year-old woman presented with diffuse swelling of the floor of the mouth after stem cell transplant for acute myeloid leukemia (AML) at age 25. Biopsy specimens consisted predominantly of benign minor salivary gland tissue with an admixed proliferation of bland cords, microtrabeculae, and microcysts lined by myoepithelial cells (Fig. 1). Mitotic figures were not readily identified. Immunohistochemistry showed strong CK5/6 expression, while CK7 was negative. Ki67 highlighted approximately 5 % of cells. No lymph nodes were involved. This patient was alive and free of disease 34 months following biopsy and radiochemotherapy.
Discussion
MAC is a rare, primarily cutaneous neoplasm that usually occurs in the face with a predilection for the nasolabial area and periorbital skin [1–6]. MAC has historically gone by a variety of names including malignant syringoma, anaplastic syringoma/syringoid carcinoma, sweat gland carcinoma with syringomatous features, and sclerosing sweat duct carcinoma [1–4]. This entity was first described by Goldstein et al. [2] as a potential mimicker of benign adnexal neoplasms such as desmoplastic trichoepithelioma, trichoadenoma, and syringoma. In this original description, Goldstein and colleagues described 6 cases of facial papules which were comprised of islands of basaloid keratinocytes percolating through dense desmoplastic stroma. Some showed overt ductal differentiation with a two discrete cell layers and gland-like spaces filled with eosinophilic material. Within the deeper dermis, the tumor cells assumed a more infiltrative appearance with invasion as single cells and thin strands, often dissecting through skeletal muscle and invading perineural spaces.
Subsequent reports of MAC invested a great deal of energy into delineating a possible anatomic origin for the tumor with dual follicular and eccrine, single eccrine, and mixed follicular and apocrine derivation proposed by a variety of investigators [2, 3, 11–14]. These discussions ultimately provide more information about where the tumor is going (line of differentiation) than where it is coming from (cell of origin), but bring an important point to light regarding MAC-like tumors in the head-and-neck: Is there sufficient homology between the cutaneous and mucosal sites of the head and neck to explain the occurrence of MAC in the latter locale? In the oral cavity, Ebner’s glands of the tongue closely resemble the eccrine sweat glands of the skin and Schipper et al. [9] have demonstrated shared histologic and immunohistochemical features between a MAC-like tumor arising in the tongue with MAC of the skin. The floor of the mouth is also invested with minor salivary glands which have some morphologic and functional overlap with adnexal and eccrine structures of the skin. Tissue of origin in the nasopharynx is less clear. The nasopharyx is lined by non-keratinizing squamous and respiratory-type mucosa that does not closely resemble the skin, although seromucinous glands can be found in the posterior pharynx. Ultimately, even in the absence of perfect homology across anatomic locales, the existence of a mucosal head and neck tumor which is analogous to MAC can likely be explained by a multipotent stem cell capable of a variety of lines of differentiation [15]. However, because adnexal structures do not reside in the mucosal head and neck, we prefer the term sclerosing microcystic adenocarcinoma for the tumors arising in these mucosal locales.
Another point of discussion regarding MAC-like carcinomas in the mucosal surfaces of the head and neck is the absence of significant solar exposure. Solar radiation has previously been implicated in MACs due to their predilection for the skin of the face, a highly sun-exposed locale [1, 4, 6, 16]. Therapeutic ionizing radiation for other causes, such as acne and carcinoma, has also been suggested as causal in MAC, with reports of MACs arising three to four decades after radiation treatment [17]. Of the 5 cases of sclerosing microcystic adenocarcinoma assessed here, only one (Case 1) was associated with prior radiotherapy. Interestingly, 1 of the other patients in our series had a history of chemotherapy and stem cell transplantation for AML (Case 5), and other authors have associated MACs with immunocompromise secondary to hematopoietic malignancies as well as solid organ transplantation [18, 19]. Immunosuppression is known to predispose patients to cutaneous squamous cell carcinomas in addition to a variety of virally-associated cancers, and may play a role in this malignancy as well.
MAC-like tumors are extremely rare in the extracutaneous head and neck. To our knowledge, this collection of 5 cases represents the first such series and adds to contributions by Schipper et al. and Hunt et al. [9, 10]. Notably, the case reported by Hunt et al. [10] was presumed to arise within the external auditory canal and is therefore thought to be of conventional adnexal derivation. Furthermore, all cases reviewed here were accrued on a busy consultative service with a focus on head and neck malignancies, contributing to the relative enrichment of this lesion at our institution. Despite that enrichment we only identified as small number of cases over a 12-year period. That said sclerosing microcystic adenocarcinomas may be more common than these numbers imply as it is prone to under recognition and misclassification as other more well-known head and neck tumors including squamous cell carcinoma and a variety of salivary gland malignancies. Confusion with benign processes is somewhat less problematic for sclerosing microcystic adenocarcinomas of the mucosal head and neck than it is in the skin, where MAC can mimic a host of benign adnexal tumors; however care must also be taken not to miss the subtly infiltrative cells of sclerosing microcystic adenocarcinomas and erroneously call a sampling benign. This is particularly true in marginal assessments on both permanent and frozen section, where the paucicellularity of the tumor and abundant associated stroma could easily lead to missed marginal involvement.
Squamous cell carcinoma is the most common among the malignancies on the differential diagnosis for sclerosing microcystic adenocarcinoma. Squamous cell carcinomas generally show significantly more atypia and mitotic activity than sclerosing microcystic adenocarcinoma and those that are well-differentiated are typically associated with abundant keratin. While the intraluminal eosinophilic secretions of sclerosing microcystic adenocarcinoma might focally evoke keratinization, their smooth, even texture and placement within uniform spaces excludes this possibility. Furthermore, although sclerosing microcystic adenocarcinoma, like MAC, can intermingle with the squamous mucosa and may elicit a pseudoepitheliomatous response, it should not be associated with overlying dysplasia.
Adenoid cystic carcinoma is also high on the differential as its tubular iteration can closely mirror the blandly infiltrative appearance of sclerosing microcystic adenocarcinoma. Indeed, 2 cases in our series (Case 1 and Case 3) were originally diagnosed as adenoid cystic carcinoma prior to review in consultation. While there is some morphologic overlap between the tubular pattern of adenoid cystic carcinoma and sclerosing microcystic adenocarcinoma, adenoid cystic carcinomas typically bear more angulated and hyperchromatic nuclei and contain more basophilic (rather than eosinophilic) luminal secretions [20, 21]. CD117 (CKIT) immunohistochemistry is also of utility in this differential as it is positive in adenoid cystic carcinoma but negative in MACs and in the cases of sclerosing microcystic adenocarcinoma tested here [20, 21].
Sclerosing microcystic adenocarcinoma may also mimic polymorphous low-grade adenocarcinoma (PLGA). PLGA arises in the seromucinous glands of the upper aerodigestive tract and may assume tubular, trabecular, glandular, cystic, and cribriform growth patterns with a tendency towards local infiltration and perineural invasion [22, 23]. As with MAC-like tumors, PLGAs show bland cytology, frequent perineural invasion, and a paucity of mitotic figures. However, PLGA usually shows a very minimal contribution of stroma, whereas the background of abundant densely sclerotic stroma is typical of sclerosing microcystic adenocarcinoma. Furthermore, PLGA by definition shows great variability in architectural pattern within a single tumor whereas sclerosing microcystic adenocarcinoma shares an architectural pattern with MAC and is typically limited to tubules, nests, and microcystic/ductal structures.
Low-grade mucoepidermoid carcinoma also warrants consideration on the differential for sclerosing microcystic adenocarcinoma as it can manifest as a minimally atypical infiltration of small glands [24]. However, it can be excluded by the presence of intracytoplasmic mucin and mucinous, rather than eosinophilic, intraluminal secretions. Abundant dense stroma is also not typically a feature.
Secretory carcinoma (formerly known as mammary analog secretory carcinoma or MASC) is another bland salivary gland tumor that may appear on the differential for sclerosing microcystic adenocarcinoma. Like MAC-like tumors, secretory carcinomas often show microcystic architecture with intraluminal secretions [25]. However, the constituent cells of these microcysts are dramatically different from those of MAC and sclerosing microcystic adenocarcinoma, showing abundant foamy cytoplasm. Furthermore, as with the previously discussed salivary gland tumors, they are much more richly cellular than sclerosing microcystic adenocarcinomas without a considerable stromal contribution.
The final entity on the differential for sclerosing microcystic adenocarcinoma of the oropharynx is low grade adenocarcinoma, non-intestinal type. These tumors are composed of tubules lined by bland cuboidal to columnar cells. Like sclerosing microcystic adenocarcinoma, they can be fairly mitotically quiescent however unlike sclerosing microcystic adenocarcinoma their cytoplasm often contains pale basophilic mucinous material. They also lack the dense hyalinized stroma characteristic of sclerosing microcystic adenocarcinoma, instead showing more crowded glandular configurations. Perineural invasion is rare.
With the possible exception of adenoid cystic carcinoma, the entities discussed in the above differential can be excluded primarily on the basis of careful morphologic assessment. Indeed, immunohistochemistry is of limited value in the diagnosis of mucosal sclerosing microcystic adenocarcinoma, but may be useful for addressing specific differentials. The immunohistochemical profile of MACs includes reactivity with broad-spectrum and high-molecular weight cytokeratins [11]. Myoepithelial markers such as p63, S100, and SMA are known to often highlight a small cell layer surrounding infiltrative nests and ducts of MAC and showed a similar staining pattern in the sclerosing microcystic adenocarcinoma in our series. CD117 (KIT) is also negative in MAC and in the sclerosing microcystic adenocarcinoma tested here, aiding in the exclusion of adenoid cystic carcinoma [21]. BerEP4, which has previously been presented as a valuable tool in cutaneous sites for the distinction of basal cell carcinoma from MAC, has subsequently proven an unreliable stratifier, highlighting over a third of MACs [26]. BerEP4 was not evaluated in the sclerosing microcystic adenocarcinoma in this series but may be an area of future interest.
The low-grade nature and morphologic homogeneity (both within and across tumors) of sclerosing microcystic adenocarcinomas raises interesting questions about the potential for an underlying translocation as many similarly bland tumors in the head and neck have been found to be translocation-associated (e.g. adenoid cystic carcinoma: MYB-NFID; low-grade mucoepidermoid carcinoma: MECT/MAML; mammary analogue secretory carcinoma: ETV6/NTRK3; benign mixed tumor/pleomorphic adenoma: PLAG1/LIFR) [25, 27, 28]. Indeed, these translocations may be of some utility in addressing the diagnostic differential for sclerosing microcystic adenocarcinoma when morphology remains ambiguous. It will be interesting to see whether a similarly reproducible genetic anomaly is ever identified in sclerosing microcystic adenocarcinoma or in conventional MACs, either in the mucosal head and neck or elsewhere.
Given the rarity of this diagnosis, the optimal therapeutic approach for sclerosing microcystic adenocarcinoma may be difficult to establish, but could be informed by treatment practices for MAC. Various modalities have been enlisted for the management of MAC occurring in the skin and include Mohs micrographic surgery, electrodessication and curettage, and simple to wide excision. As with MACs of cutaneous sites, treatment approach for sclerosing microcystic adenocarcinomas is likely to be heavily informed by anatomic location and extent of disease [1, 3]. It is reasonable to speculate that sclerosing microcystic adenocarcinomas may warrant different management when compared to some of the other tumors in the diagnostic differential, given their cutaneous counterparts’ relative propensity for late local recurrences and infrequent nodal and distant metastases. Furthermore, assessment of surgical margins on both frozen and permanent sections may be complicated by the relatively low epithelial contribution of the infiltrative edge of sclerosing microcystic adenocarcinoma. It will be valuable for pathologists and surgeons alike to be aware of this potential confounding problem to ensure adequate marginal assessment while recognizing its limitations in this setting. Although managerial uncertainty remains, inclusion of sclerosing microcystic adenocarcinoma on the diagnostic differential for cytologically bland, duct-forming infiltrative lesions identified in the head and neck mucosa, particularly in the region of the tongue and floor of mouth, will permit early recognition of this entity and ensure that therapeutic and monitoring approaches can be calibrated accordingly.
References
Abbate M, Zeitouni NC, Seyler M, Hicks W, Loree T, Cheney RT. Clinical course, risk factors, and treatment of microcystic adnexal carcinoma: a short series report. Dermatol Surg. 2003;29(10):1035–8.
Goldstein DJ, Barr RJ, Santa Cruz DJ. Microcystic adnexal carcinoma: a distinct clinicopathologic entity. Cancer. 1982;50(3):566–72.
LeBoit PE, Sexton M. Microcystic adnexal carcinoma of the skin. A reappraisal of the differentiation and differential diagnosis of an underrecognized neoplasm. J Am Acad Dermatol. 1993;29(4):609–18.
Friedman PM, Friedman RH, Jiang SB, Nouri K, Amonette R, Robins P. Microcystic adnexal carcinoma: collaborative series review and update. J Am Acad Dermatol. 1999;41(2 Pt 1):225–31.
Kato H, Mizuno N, Nakagawa K, Furukawa M, Hamada T. Microcystic adnexal carcinoma: a light microscopic, immunohistochemical and ultrastructural study. J Cutan Pathol. 1990;17(2):87–95.
Cooper PH. Sclerosing carcinomas of sweat ducts (microcystic adnexal carcinoma). Arch Dermatol. 1986;122(3):261–4.
Buhl A, Landow S, Lee YC, Holcomb K, Heilman E, Abulafia O. Microcystic adnexal carcinoma of the vulva. Gynecol Oncol. 2001;82(3):571–4. doi:10.1006/gyno.2001.6300.
Yavuzer R, Boyaci M, Sari A, Ataoglu O. Microcystic adnexal carcinoma of the breast: a very rare breast skin tumor. Dermatol Surg. 2002;28(11):1092–4.
Schipper JH, Holecek BU, Sievers KW. A tumour derived from ebner’s glands: microcystic adnexal carcinoma of the tongue. J Laryngol Otol. 1995;109(12):1211–4.
Hunt JT, Stack BC Jr, Futran ND, Glass LF, Endicott JN. Pathologic quiz case 1. microcystic adnexal carcinoma (MAC). Arch Otolaryngol Head Neck Surg. 1995;121(12):1430–3.
Wick MR, Cooper PH, Swanson PE, Kaye VN, Sun TT. Microcystic adnexal carcinoma. An immunohistochemical comparison with other cutaneous appendage tumors. Arch Dermatol. 1990;126(2):189–94.
Requena L, Marquina A, Alegre V, Aliaga A, Sanchez Yus E. Sclerosing-sweat-duct (microcystic adnexal) carcinoma—a tumor from a single eccrine origin. Clin Exp Dermatol. 1990;15(3):222–4.
Ackerman AB, Briggs PL, Bravo F. Differential diagnosis in dermatopathology. 1st ed. Philadelphia: Lea & Febiger; 1993. p. 86.
Heenan PJ. Sebaceous differentiation in microcystic adnexal carcinoma. Am J Dermatopathol. 1998;20(5):537–8.
Krahl D, Sellheyer K. Monoclonal antibody ber-EP4 reliably discriminates between microcystic adnexal carcinoma and basal cell carcinoma. J Cutan Pathol. 2007;34(10):782–7.
Schwarze HP, Loche F, Lamant L, Kuchta J, Bazex J. Microcystic adnexal carcinoma induced by multiple radiation therapy. Int J Dermatol. 2000;39(5):369–72.
Antley CA, Carney M, Smoller BR. Microcystic adnexal carcinoma arising in the setting of previous radiation therapy. J Cutan Pathol. 1999;26(1):48–50.
Lei JY, Wang Y, Jaffe ES, et al. Microcystic adnexal carcinoma associated with primary immunodeficiency, recurrent diffuse herpes simplex virus infection, and cutaneous T-cell lymphoma. Am J Dermatopathol. 2000;22(6):524–9.
Carroll P, Goldstein GD, Brown CW Jr. Metastatic microcystic adnexal carcinoma in an immunocompromised patient. Dermatol Surg. 2000;26(6):531–4.
Moskaluk CA. Adenoid cystic carcinoma: clinical and molecular features. Head Neck Pathol. 2013;7(1):17–22. doi:10.1007/s12105-013-0426-3.
Thompson LD, Penner C, Ho NJ, et al. Sinonasal tract and nasopharyngeal adenoid cystic carcinoma: a clinicopathologic and immunophenotypic study of 86 cases. Head Neck Pathol. 2014;8(1):88–109. doi:10.1007/s12105-013-0487-3.
Gnepp DR, Chen JC, Warren C. Polymorphous low-grade adenocarcinoma of minor salivary gland. An immunohistochemical and clinicopathologic study. Am J Surg Pathol. 1988;12(6):461–8.
Thompson LD. Polymorphous low-grade adenocarcinoma. Ear Nose Throat J. 2014;93(1):24–5.
Brandwein MS, Ivanov K, Wallace DI, et al. Mucoepidermoid carcinoma: a clinicopathologic study of 80 patients with special reference to histological grading. Am J Surg Pathol. 2001;25(7):835–45.
Connor A, Perez-Ordonez B, Shago M, Skalova A, Weinreb I. Mammary analog secretory carcinoma of salivary gland origin with the ETV6 gene rearrangement by FISH: expanded morphologic and immunohistochemical spectrum of a recently described entity. Am J Surg Pathol. 2012;36(1):27–34. doi:10.1097/PAS.0b013e318231542a.
Smith KJ, Williams J, Corbett D, Skelton H. Microcystic adnexal carcinoma: an immunohistochemical study including markers of proliferation and apoptosis. Am J Surg Pathol. 2001;25(4):464–71.
Weinreb I. Translocation-associated salivary gland tumors: a review and update. Adv Anat Pathol. 2013;20(6):367–77. doi:10.1097/PAP.0b013e3182a92cc3.
Seethala RR, Dacic S, Cieply K, Kelly LM, Nikiforova MN. A reappraisal of the MECT1/MAML2 translocation in salivary mucoepidermoid carcinomas. Am J Surg Pathol. 2010;34(8):1106–21. doi:10.1097/PAS.0b013e3181de3021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Mills, A.M., Policarpio-Nicholas, M.L.C., Agaimy, A. et al. Sclerosing Microcystic Adenocarcinoma of the Head and Neck Mucosa: A Neoplasm Closely Resembling Microcystic Adnexal Carcinoma. Head and Neck Pathol 10, 501–508 (2016). https://doi.org/10.1007/s12105-016-0731-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-016-0731-8