Abstract
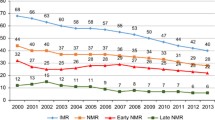
India is committed to achieve a single-digit neonatal mortality rate (NMR) and stillbirth rate (SBR) by 2030 through India Newborn Action Plan (INAP) 2014. However, the current rate of decline is not enough to achieve the target neonatal mortality rate. Course correction and renewed efforts are required. This review outlines the current scenario and proposed scale-up of services included during labour, childbirth, and the immediate newborn period. The article summarises the challenges and bottlenecks in achieving a reduction in neonatal mortality rate and INAP targets. India has achieved over 80% coverage of three of the four ENAP coverage targets, but antenatal care coverage is still poor. There are concerns about the quality and completeness of antenatal care visits and other program interventions. The ongoing quality assurance should be strengthened through continuous supportive supervision by involving the medical colleges in a hub and spoke model and other key stakeholders. There is a need for effective and strategic engagement of the private sector in these initiatives. The states need to systematically assess the gaps as per population requirements and find effective solutions to overcome them quickly. The state and district-wise data maps show immense variations in coverage between states and within states, mirroring the variations in NMR. This indicates the need to ensure contextual micro-plans and provides an opportunity for the districts and states to learn from each other. The recent initiatives to strengthen primary healthcare should be used as a platform for all stillbirth and neonatal mortality prevention interventions in India.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
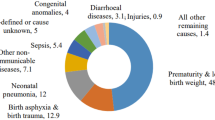
India has achieved a major reduction in childhood mortality in the past two decades. However, it remains high, and the proportional share of neonatal mortality has increased [1]. Prematurity, birth complications (including perinatal asphyxia), and sepsis contribute to more than 90% of neonatal deaths [2, 3]. Even among preterm neonates, intrapartum-related causes (perinatal asphyxia) are the most common cause of mortality in the Indian subcontinent [4]. Around 40% of all stillbirths occur during labour [3, 5]. About 75% of neonatal deaths occur within the first seven days of life, and 40% within 48 h [3, 6]. The labour, childbirth, and immediate newborn period are critical for neonatal survival. Therefore, care during labour, childbirth, and the immediate newborn period - pillars two and three of the six pillars of the India Newborn Action Plan (INAP), need the closest attention to accelerate the decline in maternal and neonatal mortality [6]. This review summarizes the progress made under these pillars of INAP and elucidates the services included during labour, childbirth, and the immediate newborn period. It highlights the bottlenecks to achieving the INAP goals.
Material and Methods
The authors searched PubMed, Embase, Scopus, Google Scholar, and the official websites of the World Health Organization (WHO), United Nations International Children’s Emergency Fund (UNICEF), National Health Mission India, and Ministry of Health and Family Welfare (MoHFW) for the relevant original articles, reviews, policy documents, and statistical reports. The search strategy included keywords like labour care, newborn care, INAP, safe deliveries, skilled birth attendants, stillbirths, neonatal deaths, etc. The search was limited to the last 10 y (2012–2022). A manual search of the bibliography of the relevant articles supplemented the electronic search. Only studies and reviews conducted in the Indian context were included. All sources were identified, collated, analyzed, and summarized per the review's objective.
Care During Labour and Childbirth
The indicators reflecting the care during labour and childbirth include the proportion of safe deliveries, clean perinatal practices, women with preterm labour receiving antenatal steroids, women with premature rupture of membranes receiving a pre-referral dose of antibiotics, number of skilled birth attendants (SBA), proportions of labour room staff trained in Navjat Shishu Suraksha Karyakram (NSSK), health facilities providing basic and emergency obstetrical care, and intrapartum stillbirths. A summary of interventions during labour, childbirth, and immediate newborn care, and their potential process indicators is provided in Table 1.
As per National Family Health Survey (NFHS)-5, India has achieved 80% or more coverage for three of the four Every Newborn Action Plan (ENAP) targets: SBAs at delivery, postnatal visit within two days for the mother, and availability of at least one special newborn care unit (SNCU) in the district [7]. The coverage for four antenatal care visits stands at 58%. However, there are marked variations in the coverage between states and districts. The district-wise composite coverage of the four ENAP targets mentioned above mirrors the neonatal mortality rate (NMR) (Fig. 1). States like Kerala and Goa have single-digit NMR and have achieved most of the ENAP targets. Many states still perform poorly in almost all healthcare indices (Bihar, Uttar Pradesh, Uttarakhand, Madhya Pradesh, Rajasthan, Jharkhand, Odisha, Chhattisgarh, and Assam) and account for over 60% of maternal and 70% of infant deaths in India. The authors have compared some of the indicators of labour and childbirth between these nine targeted states, and Kerala and Goa (Figs. 2 and 3).
Proportion of Safe Deliveries
Safe deliveries include institutional deliveries and home births attended by SBAs. As per NFHS-5, the share of institutional deliveries increased from 78.9% in 2015–16 to 88.6% in 2019–2021 [7]. The proportion of institutional births in Kerala and Goa is 99.8% and 99.7%, respectively. However, in the nine states with high NMR, the proportion of institutional births ranges between 75.8% and 94.9%. Amongst these states, Odisha registered the lowest increase (7%), while Chhattisgarh and Jharkhand had the highest increase (18%) in institutional deliveries between 2015–16 and 2019–21. The overall proportion of deliveries attended by SBA in these nine states ranged between 79% to 95.6% (Fig. 2). Seven of these nine states have over 10% unsafe deliveries. This may be one reason for high neonatal and maternal mortality rates in these states.
Clean Perinatal Practices
The six cleans for childbirth are well-known, but there is limited information about their compliance in the community. Clean birth practices, especially hand hygiene by birth attendants, can reduce sepsis-related mortality in home births by 15% and in facility births by 27% [6]. As per a recent survey, hand hygiene compliance before delivery was poor (27%) in public facilities [8]. Compliance with hand hygiene during per-vaginal examinations was just 35%. In a survey done at 49 newborn care units (19 private, 30 public) and 35 labour rooms (5 private, 30 public), the compliance to all steps of hand hygiene was suboptimal: private 44% vs. public 12%, tertiary 33% vs. secondary units 12% [9]. According to a Water Supply, Sanitation, and Hygiene (WASH) program survey, only 19.2% of labor rooms and 3.2% of postnatal care wards had proper hygiene and sanitation facilities [9]. The government of India has introduced Swachh Bharat Mission and Kayakalp to improve WASH services in healthcare facilities.
Antenatal Steroids in Women with Preterm Labour
Around 13% of all births in India i.e., 3.5 million per annum are preterm [10]. Over 10% of preterm neonates die due to birth-related complications, and many experience neurodevelopmental impairment [4, 6, 10]. Antenatal corticosteroids (ACS) are a low-cost, effective intervention to improve the outcomes in premature births [11]. There is limited data about the proportion of preterm deliveries receiving ACS in India. In the ACT trial, the use of ACS for women with small (<5th percentile) babies ranged from 5–11% in the control arm [11]. A cross-sectional study conducted in 37 public health facilities in Haryana found that the ACS operational guidelines were not followed uniformly [12]. Only 6–35% of nurses and 52–67% of doctors were aware of these guidelines. Less than 20% of all healthcare professionals received ACS-related training. The limited coverage of ACS could be due to multiple issues related to awareness, training, and clear protocols at the grass-root level.
Antibiotic Prophylaxis for Preterm Premature Rupture of Membranes
Preterm premature rupture of membranes (PPROM) precedes 40–50% of preterm deliveries and can lead to intrauterine infection [13]. Antibiotic prophylaxis given to women with PPROM is an evidence-based intervention to reduce neonatal mortality [14]. MoHFW, Government of India has authorized auxiliary nurse midwives (ANMs)/lady health visitors/staff nurses to give the first dose of antibiotics before referring them to higher institutions [15]. However, there is limited data on its compliance.
Number of Skilled Birth Attendants
According to rural health statistics for 2020–21, there is a substantial shortfall of SBAs in rural areas [16]. Among nine targeted states, the shortfall of ANMs is especially conspicuous in Chhattisgarh, Odisha, Rajasthan, and Jharkhand. While the shortfall of medical officers in rural areas is conspicuous in Odisha, Rajasthan, and Uttar Pradesh, the shortfall of specialists is prevalent across India.
Proportions of Labour Room Staff Trained in NSSK
Status reports suggest inadequate availability of staff trained in NSSK across the states. In Odisha's 2019–20 status report, 80% of targeted batches from 30 districts received training. In most states, fewer candidates were trained than planned due to non-deputation of candidates and logistic reasons [17]. COVID-19 further disrupted the training sessions. Transfers and attrition of contractual employees contributes to the low availability of trained staff in labour rooms.
Health Facilities Providing Basic and Comprehensive Emergency Obstetrical Care
The use of partograph and the proportion of cesarean deliveries are taken as operational indicators for monitoring comprehensive emergency obstetrical care (CEmOC) services. The partograph is the 'gold standard' tool for labour monitoring, but the rate of partograph use is low in resource-limited settings [18]. In a cross-sectional study in 10 public health facilities in Odisha, adherence to partograph plotting was 48.7%. It was significantly better at community health centres than district and subdivisional hospitals [19]. The challenges in the optimal use of the partograph include increased workload, decreased awareness, inadequate training/ monitoring, and lack of clear protocols. In the nine high NMR states, the proportion of babies delivered by cesarean section (CS) ranges between 9.7–21.6% (Fig. 3), much lower than Kerala (38.9%) and Goa (39.5%). In these high NMR states, the proportion of CS in public sector hospitals ranges between 3.6–15.3%, against 37.2% and 31.5% in Kerala and Goa, respectively. In private-sector hospitals, the proportion of cesarean deliveries ranges between 39.4–70.6% in high NMR states as against 39.9% and 50.0% in Kerala and Goa, respectively. Thus, CEmOC coverage is suboptimal in public health facilities, and the private sector fulfils a large proportion of the requirement in these states.
Intrapartum Stillbirths
The stillbirth rate in India is reported to be 3 to 12.2 per 1,000 total births; however, data quality and inequity are major challenges [20, 21]. A major reason stillbirth has gone unnoticed as a public health issue in India is its lack of recognition at policy level, societal acceptance, and possible stigma towards miscarriage [22]. The factors associated with higher stillbirths include poor antenatal care, delivery-related variables, maternal condition, pregnancy complications including anemia, bleeding, hypertension, place of delivery, etc. The issues related to healthcare providers include lack of timely attention, poor skills, and reluctance to deliver a dead baby. A few articles published in this special issue have proposed a few solutions to tackle the stillbirth challenge [20, 21].
Immediate Newborn Care
There are six essential components of immediate newborn care – delayed cord clamping, prevention of hypothermia, early initiation of breastfeeding, clean perinatal practices, vitamin K administration, and effective resuscitation. Of these, clean perinatal practices have been addressed above. If these components are universally implemented, 70–80% of preventable early neonatal deaths can be averted [3, 6, 23]. The number of facilities providing neonatal care has increased exponentially over the past 15 y (Table 2) [24].
Delayed Cord Clamping (DCC)
DCC for 1–3 min in infants not requiring resuscitation reduces the risk of mortality (2.6% absolute reduction rate), intraventricular hemorrhage (2.4% absolute reduction rate), and the need for blood transfusion in preterm infants. It also improves hemoglobin levels and iron stores in term infants, which may improve developmental outcomes [25, 26]. Data on DCC coverage is limited. A prospective audit from the level 2 healthcare facilities of Gujarat and Uttar Pradesh showed coverage of 98.2% in Gujarat and 93.6% in UP [27]. However, the practice of DCC was generally not followed during cesarean section and multiple pregnancies. The coverage was also poor during the daytime when the number of deliveries was high. A significant challenge was the lack of resources to monitor and document the time that had elapsed since birth.
Prevention of Hypothermia
The global prevalence of hypothermia is 32–85% in low-birth weight (LBW) infants and contributes to nearly 70% of preterm deaths in low-and middle-income countries [28, 29]. Prevention of hypothermia can avert 18–42% of neonatal deaths [23]. The interventions to prevent hypothermia include immediate skin-to-skin contact for at least one hour (term infants), immediate drying or use of plastic wraps (<32 wk), immediate continuous kangaroo mother care (LBW infants), and delaying the first bath. Immediate skin-to-skin contact between the mother and baby just after delivery and initiation of continuous kangaroo mother care (KMC) soon after birth is associated with improved survival by 25–40% in LBW infants [23, 30, 31]. Although these are high-impact interventions, their implementation has several challenges. Prevention of hypothermia requires adequate infrastructure, such as newborn care corners, and measures to control air draughts and room temperature. However, interventions such as skin-to-skin contact and KMC can be performed even with limited resources, with a simple reorganization of care processes.
Early Initiation of Breastfeeding
Initiating breastfeeding within the first hour of life can decrease neonatal mortality by 20%, and continuing exclusive breastfeeding until six months can reduce infant mortality by up to 50% [23, 32]. Although it seems simple, only 41.8% of infants receive breastfeeds within one hour of birth [7]. Today, 90% of women deliver in a health facility, but breastfeeding rates have not improved over a decade. This highlights the knowledge practice gap and emphasizes the need for better implementation strategies. Major bottlenecks for universal coverage of initiating breastfeeding within one hour are a non-conducive labour room environment, lack of privacy, lack of enough nurses or birth companions, lack of motivation, and cesarean deliveries [33].
Vitamin K Administration
All neonates should receive vitamin K injections at birth to prevent hemorrhagic disease of the newborn.
Neonatal Resuscitation
Infants who fail to breathe on their own within 60 s of birth should receive gentle, positive-pressure ventilation with a self-inflating bag and mask, or T-piece resuscitator (preferred in <32 wk). This intervention might help reduce neonatal mortality by 6–40% [23]. Poor availability of SBAs for bag and mask ventilation is a significant bottleneck. Facility-based newborn care training aims to train nurses, ANMs, and doctors on basic resuscitation skills. However, data on the coverage and quality of resuscitation are lacking. The universal coverage of the above interventions can help reduce neonatal mortality by three-fourths and accelerate progress towards achieving the SDG goals of NMR. The important process indicators (along with their current coverage and targets for 2025) for monitoring the care during labour, childbirth, and the immediate newborn period are summarized in Table 3.
National Programs on Newborn Health
Over the last two decades, several programs linked to improving neonatal survival have been initiated and successfully implemented. Until recently, increasing the coverage of interventions was the main target. However, in the last few years, rightfully the attention has now shifted to providing respectful, equitable, and patient-centered quality care. National Quality Assurance Standards (NQAS) have been developed for public health facilities. The NQAS is available for primary and community health centers and district hospitals. Several objective indicators have been developed under LaQshya and MusQan programs to assess the quality for certification and improvement. Ongoing quality improvement programs and handholding are required to sustain these changes.
Discussion
Care during labour, childbirth, and the immediate postnatal period is critical for prevention of stillbirth and neonatal death. Most stillbirths are preventable, and nearly half happen during the intrapartum period. Similarly, around three-fourths of neonatal deaths occur in the first week of life. Hence interventions should be prioritized during this period. As many as 75% of first-week neonatal deaths can be prevented by the effective and equitable use of evidence-based, low-cost interventions [23].
Recent evidence suggests that even in the first week, the causes of death at 0–2 d differ from those at 3–7 d [34]. In a study from Bihar, perinatal asphyxia and prematurity accounted for nearly 85% of 0–2-d deaths, whereas sepsis (including pneumonia) accounted for 65% of 3–7-d deaths. This suggests interventions for preventing neonatal deaths differ during the first 2 d vs. 3–7 d of life. In addition, there is wide variation in neonatal mortality and its causes across states and districts [3]. Hence, microplanning is required at the district level. In Kerala, the burden of asphyxia and sepsis is low, but prematurity- and malformation-related deaths are increasing [3]. Perinatal asphyxia and neonatal infections remain predominant in Bihar, Madhya Pradesh, and the northeast region. Apart from availability and affordability, inequality and poor quality are significant concerns that may be responsible for wide variations within the country [3, 5, 7].
Reports suggest insufficient awareness among expectant mothers regarding government schemes [35]. This can be increased by leveraging existing community actions for health interventions that have evolved under the national health mission in the last 15 y [36]. Awareness of both health professionals and potential beneficiaries can be increased using web/ application-based solutions, mass media, and print media to enhance demand and utilization. Specific areas that need attention are the care of pregnant women with threatened preterm birth, including the rationale use of ACS, and antibiotics for PPROM. Programs like Pradhan Mantri Surakshit Matritva Yojana (PMSMY), media awareness campaigns, mother–child tracking using digital media, and field health workers are immensely helpful in improving the coverage of ANC check-ups. The initiatives and success in ensuring the availability of CEmOC services, including cesarean deliveries in the public sector, have been variable amongst states and districts. One of the most common reasons is the non-availability of specialists. States and districts can learn from each other about successful strategies to overcome this. The Ayushman Bharat program, and health and wellness center initiative have expanded facility-based and consultation services and decreased out-of-pocket expenses. These should be optimally used for achieving INAP targets of stillbirth and neonatal mortality and to achieve equity [37,38,39]. However, the number of currently empanelled private facilities are insufficient.
Each state should calculate its bed requirements and the shortfall as per the population. Enough private facilities should be empanelled to meet the gap until new facilities can be developed in the public sector. The expertise of medical colleges can be utilized in national programs by developing coordination and synergy between the directorates of medical education and National health missions. Supportive supervision by medical colleges for on-site mentoring, tele-mentoring, teleconsultation, and capacity building in a hub and spoke model can be helpful. The GoI operational guidelines for the safe and effective use of ACS in threatened preterm births and antibiotics for PPROM need to be updated, disseminated, and integrated with the training programs. Mechanisms need to be developed to capture the quality and completeness of antenatal check-ups and client satisfaction to improve the antenatal services and pick-up rates of high-risk pregnancies.
Conclusions
India has made tremendous strides in maternal, neonatal, and child health with the help of several national and state programs and initiatives. The immense variation between states and districts is of concern and may dampen our efforts to reach the SDG goals and INAP targets. However, this is also an opportunity for the states and districts, to learn from each other and implement new strategies for improving coverage and quality. The variation is also a clear message for local microplanning based on contextual challenges. The data collection and review systems need strengthening and synchronization. Select process measures need to be captured in real-time to help improve the quality of care. The ongoing programs to strengthen primary healthcare should be optimally used to achieve INAP goals.
Key Messages
-
India has committed to achieve a single-digit Neonatal mortality rate (NMR) and Stillbirth rate by 2030. However, the current rate of decline in NMR is not enough to achieve the goal, and a course correction is required.
-
There are huge variations in coverage and mortality rates between states as well as districts. Micro-panning is required to address this. The states and districts can learn from each other's experiences.
-
There is a need to improve awareness among the community and healthcare workers about the entitlements under government schemes to improve demand and utilization.
-
Though the coverage of interventions has increased, the quality and completeness of package delivery must be ensured. Quality care during labour, childbirth, and immediate newborn period is most critical, and several low-cost, evidence-based interventions are available. The guidelines for their use need to be updated and disseminated effectively while removing the bottlenecks preventing their effective utilization.
-
Supportive supervision involving medical colleges in the hub and spoke models can yield good dividends. There should be strategic engagement with the private sector and professional associations.
-
The ongoing initiatives to strengthen the primary healthcare initiatives should be optimally used to achieve the INAP goals.
References
Lahariya C, Paul VK. Burden, differentials, and causes of child deaths in India. Indian J Pediatr. 2010;77:1312–21.
Lahariya C, Sudfeld CR, Tomar SS. Causes of child deaths in India, 1985–2008: A systematic review of literature. Indian J Pediatr. 2010;77:1303–11.
Collaborators I-L. Subnational mapping of under-5 and neonatal mortality trends in India: The Global Burden of Disease Study 2000–17. Lancet. 2020;395:1640–58.
Dhaded SM, Saleem S, Goudar SS, et al. The causes of preterm neonatal deaths in India and Pakistan (PURPOSe): A prospective cohort study. Lancet Glob Health. 2022;10:e1575–81.
Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128.
India Newborn Action Plan (INAP). National Health Mission. Available at: https://nhm.gov.in/images/pdf/programmes/inap-final.pdf. Accessed on 22 Jan 2023.
Ending Preventable Newborn Deaths and Stillbirths by 2030. WHO and UNICEF September 2020. Available at: https://data.unicef.org/resources/resource-type/publications/. Accessed on 23 May 2023.
Tyagi M, Hanson C, Schellenberg J, Chamarty S, Singh S. Hand hygiene in hospitals: An observational study in hospitals from two southern states of India. BMC Public Health. 2018;18:1299.
WASH in Health Care Facilities. Available at: https://www.unicef.org/india/what-we-do/wash-facilities. Accessed on 21 Oct 2022.
Chawanpaiboon S, Vogel JP, Moller A-B, et al. Global, regional, and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis. Lancet Glob Health. 2019;7:e37–46.
WHO ACTION Trials Collaborators; Oladapo OT, Vogel JP, Piaggio G, et al. Antenatal Dexamethasone for early preterm birth in low-resource countries. N Engl J Med. 2020;383:2514–25.
Kankaria A, Duggal M, Chauhan A, et al. Readiness to provide antenatal corticosteroids for threatened preterm birth in public health facilities in northern India. Glob Health Sci Pract. 2021;9:575–89.
Menon R, Richardson LS. Preterm prelabor rupture of the membranes: A disease of the fetal membranes. Semin Perinatol. 2017;41:409–19.
Kenyon S, Boulvain M, Neilson JP. Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev. 2010;8:CD001058.
National Rural Health Mission. Ministry of Health & Family Welfare GoI. Skilled Birth Attendance (SBA) Trainer's Guide for conducting Training of Auxillary Nurse Midwives, Lady Health Visitors & Staff Nurses. Available at: http://tripuranrhm.gov.in/Guidlines/Staff_Nurses2.pdf. Accessed on 22 Jan 2023.
Rural Health Statistics 2020–21. Ministry of Health and Family Welfare. GOI. Available at: https://main.mohfw.gov.in/newshighlights-90. Accessed on 29 Apr 2023.
Training Status Report 2019–20. Mission Directorate NHM, Department of Health & Family Welfare, Govt. of Odisha. Available at: http://www.nrhmorissa.gov.in/writereaddata/Upload/Documents/Training%20Status%20Report%20.pdf. Accessed on 20 Mar 2023.
Dalal AR, Purandare AC. The partograph in childbirth: An absolute essentiality or a mere exercise? J Obstet Gynaecol India. 2018;68:3–14.
Palo SK, Patel K, Singh S, Priyadarshini S, Pati S. Intrapartum monitoring using partograph at secondary level public health facilities-A cross-sectional study in Odisha. India J Fam Med Prim Care. 2019;8:2685–90.
Sharma B, Lahariya C, Majella MG, et al. Burden, differentials and causes of stillbirths in India: A systematic review & meta analysis. Indian J Pediatr. 2023;in press.
Agarwal N, Lahariya C, Sharma B, et al. Stillbirth in India: Current status, challenges, and the way forward. Indian J Pediatr. 2023;in press.
Sharma B, Raina A, Kumar V, Mohanty P, Sharma M, Gupta A. Counting stillbirth in a community - To understand the burden. Clin Epidemiol Glob Health. 2022;14:100977.
Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–88.
Ministry of Health and Family Welfare. Annual Report 2020–21. Available at: https://main.mohfw.gov.in/sites/default/files/Annual%20Report%202020-21%20English.pdf. Accessed on 29 Apr 2023.
Jasani B, Torgalkar R, Ye XY, Syed S, Shah PS. Association of umbilical cord management strategies with outcomes of preterm infants: A systematic review and network meta-analysis. JAMA Pediatr. 2021;175:e210102.
American College of Obstetricians and Gynecologists' Committee on Obstetric Practice. Delayed umbilical cord clamping after birth: ACOG Committee Opinion, Number 814. Obstet Gynecol. 2020;136:e100–6.
Chowdhury A, Neogi SB, Prakash V, et al. Implementation of delayed cord clamping in public health facilities: A case study from India. BMC Pregnancy Childbirth. 2022;22:457.
Lunze K, Bloom DE, Jamison DT, Hamer DH. The global burden of neonatal hypothermia: Systematic review of a major challenge for newborn survival. BMC Med. 2013;11:24.
Muhe LM, McClure EM, Nigussie AK, et al. Major causes of death in preterm infants in selected hospitals in Ethiopia (SIP): A prospective, cross-sectional, observational study. Lancet Glob Health. 2019;7:e1130–8.
Abiramalatha T, Ramaswamy VV, Bandyopadhyay T, et al. Delivery room interventions for hypothermia in preterm neonates: A systematic review and network meta-analysis. JAMA Pediatr. 2021;175:e210775.
WHO Immediate KMC Study Group, Arya S, Naburi H, Kawaza K, et al. Immediate "Kangaroo Mother Care" and survival of infants with low birth weight. N Engl J Med. 2021;384:2028–38.
Victora CG, Bahl R, Barros AJD, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–90.
Rollins NC, Bhandari N, Hajeebhoy N, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387:491–504.
Dandona R, Kumar GA, Bhattacharya D, et al. Distinct mortality patterns at 0–2 days versus the remaining neonatal period: Results from population-based assessment in the Indian state of Bihar. BMC Med. 2019;17:140.
Mundargi K, Hiregoudar V. Awareness about government maternal benefit schemes among pregnant women attending Anganawadi centres in North Karnataka. Int J Commun Med Public Health. 2021;8:4801–5.
Lahariya C, Roy B, Shukla A, et al. Community action for health in India: Evolution, lessons learnt and ways forward to achieve universal health coverage. WHO South East Asia J Public Health. 2020;9:82–91.
Lahariya C. “Ayushman Bharat” program and universal health coverage in India. Indian Pediatr. 2018;55:495–506.
Lahariya C, Khanna R, Nandan D, et al. Primary health care and child survival in India. Indian J Pediatr. 2010;77:283–90.
Lahariya C. Health & wellness centers to strengthen primary health care in India: Concept, progress and ways forward. Indian J Pediatr. 2020;87:916–29.
Acknowledgements
The authors would like to thank Dr. Chandrakant Lahariya, Dr. Rodney P Vaz, and other technical staff at the Integrated Department of Health Policy, Epidemiology, Pediatrics and Preventive Medicine at the Foundation for People-centric Health Systems for reviewing and providing input on the earlier version of this manuscript.
Author information
Authors and Affiliations
Contributions
PK conceived the idea and outline, and critically reviewed, revised and finalized the manuscript; JK and SSS wrote parts of the initial draft and revised as per feedback. PK will act as the guarantor for this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kumar, J., Saini, S.S. & Kumar, P. Care During Labour, Childbirth, and Immediate Newborn Care in India: A Review. Indian J Pediatr 90 (Suppl 1), 20–28 (2023). https://doi.org/10.1007/s12098-023-04721-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-023-04721-7