Abstract
Objective
To understand the causes of child deaths in order to implement appropriate child survival interventions in the country. We present a systematic review of studies reporting causes of child, infant, and neonatal deaths from India for 1985 to 2008.
Methods
PubMed, EMBASE, Google Scholar, and WHO regional databases were searched along with a hand search and personal communication with researchers in child health to obtain studies and reports for the database. Study data was summarized and analyzed using appropriate statistical tools.
Results
We identified 28 published/unpublished studies and reports (6 multi-centric and 22 single sites). There was one nation wide study and rest were from 15 unique sites in 9 different states of India. There were differences in study design and cause of death assignment methods between the studies, which made comparisons and synthesis difficult. The median percentage of causes of deaths in neonatal period were sepsis/pneumonia: 24.9% (Q1: 19.6% and Q3: 33.4%); asphyxia: 18.5% (Q1: 14.2% and Q3: 21.9%); and pre-maturity/LBW: 16.8% (Q1: 12.5% and Q3: 26.5%). Amongst the infants, sepsis/pneumonia, asphyxia, and prematurity/low birth weight (LBW) remain substantial causes of deaths. The median proportional contribution of neonatal deaths to total infant deaths was 48.5% (Q1: 36.5–Q3: 57.5%). The proportion of deaths due to infectious diseases like diarrhoea, pneumonia, and measles seem to be greater in infancy, in comparison to that in neonatal period. There was no statistically significant difference in the proportional contribution of neonatal deaths to total deaths occurring during infancy (<1 year) between the two equal periods before and after 1996 (p = 0.141). There also was no difference in the proportional contribution by cause of death assignment method (Verbal autopsy vs. other methods; p = 0.715) or by study setting (urban vs. rural; p = 0.175). The median percentage of neonatal deaths by day 1 is 36.7% (Range: 20.0–58.0%). The median cumulative percentage of neonatal deaths by day 3 was 49.7% (Range 35.0–64.6%), and 70.9% (Range: 46.5–92.3%) by day 7. In addition, the timing of deaths during neonatal period seems to be static during the last 2 decades, with majority of deaths occurring during first week of life.
Conclusions
This review demonstrates the need for more studies with consistent methodological rigor investigating the causes of child death in India. We conclude that the structure of neonatal causes of death in India may be different from the rest of the world and that interventions to reduce neonatal deaths in first week of life may rapidly improve child survival in the country.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
More children under 5 years of age die annually in India than any other country of the world [1, 2]. Understanding the causes of these deaths may help in identifying and implementing appropriate, high-impact interventions to improve child survival in the country and achievement of Millennium development Goal 4 [3]. It is unfortunate that, for long, there were no systematic and organized mechanisms to identify and classify the causes of under five deaths in India; however, recently a few large scale surveys/studies were initiated to address this need [4–6].
The last literature review on the causes of child deaths in India was published in 1986 with published data up to 1985 [7]. The majority of studies included in this review were from hospital settings with a focus on causes of perinatal deaths. A number of health interventions have been introduced or expanded since 1985 as a result the pattern and causes of child deaths in India has likely changed thereafter. Consequently, we found it imperative to systematically review studies and reports published after 1985 in order to examine contemporary causes and timing of neonatal, infant, and child deaths in India. The other objective of this review was to provide relevant policy recommendations for implementing and/or expanding child survival interventions in India.
Material and Methods
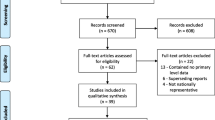
We systematically reviewed the literature from January 1, 1985 to December 31, 2008 to identify studies from India on causes, and timing of child, infant, and neonatal deaths. This time period was selected because the last review on the causes of child deaths in India was published in 1986, covering studies published prior to 1985. Further, the major child survival initiatives in India started after 1985. To find these studies, we conducted search of PubMed, EMBASE, Google scholar, and from the World Health Organization (WHO) regional databases using combination of the search terms “Child mortality”, “Infant mortality”, “Neonatal mortality”, “India”, “Child Health”, “Child Survival”. Recent government reports and data from known unpublished survey/reports were also included. The inclusion criteria for the studies or the reports was that the study participants were either in defined age group of less than 5 yrs and quantitative data on causes or timing of child, infant or neonatal mortality was presented. All studies meeting these criteria were included in the descriptive analysis, however if nested studies were conducted from the same study population only the larger original study was included in the final statistical analyses. All contributing data was double abstracted and compared for discrepancies. The neonatal period was defined as the first 28 days of life, infancy less than 1 yr old, and childhood under 5 yrs.
We decided to include all the studies, which met our inclusion criteria and present a descriptive analysis of including study location, setting, year, sample size, population studied, and causes of deaths. The causes of death were defined by study authors and median percentages were calculated for major causes of death. The proportional contribution of neonatal deaths occurring during infancy, along with the cumulative percentage of neonatal deaths by day 1, 3, and 7 are also presented. We decided not to use pooled data (means) but preferred the use of median for analyses, since the studies employed different designs and utilized different cause of death definitions.
Additionally, there have likely been changes in the structure of causes of child death due to interventions during the 24 yr study period. In order to statistically test the differences by study year and design, we utilized the Kruskal–Wallis test, a non-parametric method for testing equality of population medians among groups [8]. The study years were dichotomized before and after 1996, which was the midpoint year of the included studies. The study design was dichotomized by verbal autopsy vs. other methods. A p-value <0.05 was considered statistically significant for all analyses. Analyses were conducted using STATA 10.0 Special Edition (STATACORP, College Station, TX).
Results
Our literature review found 28 published/unpublished studies and reports on the causes of under 5, infant, and neonatal deaths in India [9–36]. A descriptive analysis of the studies is presented in Table 1. There were six multi-centric [9–12, 24, 34] and 22 single site studies. Multiple studies were conducted on the same study site, during different years; therefore, this review presents data from 15 unique sites. These sites are in nine different states of India, with a majority from Uttar Pradesh, Maharashtra, and New Delhi (summarized in Table 1).
A total of 20 studies presented cause of death for neonatal period. The three major causes of neonatal deaths were sepsis/pneumonia, asphyxia, and prematurity/low birth weight (LBW). The median percentage of deaths due to sepsis/pneumonia was 24.9% (Q1: 19.6% and Q3: 33.4%), due to asphyxia was 18.5% (Q1: 14.2% and Q3: 21.9%), and pre-maturity/LBW together had a median percentage of 16.8% (Q1: 12.5% and Q3: 26.5%). Other notable causes of death include tetanus, and congenital malformations. The proportions of deaths, due to these causes, were variable between studies. For example tetanus caused 21.4% of death in one study, while in others no deaths were attributable to tetanus [10, 26, 31].
Only six studies presented data on cause of infant (<1 yr) deaths [11, 15, 18, 24, 34, 35]. Sepsis/pneumonia, asphyxia, and prematurity/low birth weight (LBW) remain substantial causes of deaths due to a large proportion of infant deaths occurring during the neonatal period. However, the proportion of deaths due to infectious diseases like diarrhea, pneumonia, and measles seem to be greater, in comparison to the neonatal period. A total of five studies had data on cause of child deaths (<5 years) in India [9, 18, 19, 28, 35]. Statistical analyses were not possible for both causes of infant and under five deaths; due to the small number of studies in each group and since researchers in these studies used varying definitions and groupings of cause of death. However, a descriptive analysis suggests further increases in the proportion of deaths due to infectious diseases during childhood (<5 yrs) compared to that in the period of infancy.
Table 2 presents study data on the proportional contribution of neonatal deaths (first 28 days) to total deaths occurring during infancy (<1 yr). Two additional studies, which provided timing of neonatal deaths but not cause of death, were also included in this table [37, 38]. Analysis of all studies determined the median proportional contribution of neonatal deaths to total infant deaths was 48.5% (Q1: 36.5% and Q3: 57.5%). In order to investigate if neonatal contribution to infant deaths was changing overtime, we utilized the Kruskal–Wallis test for medians. We dichotomized year of study before and after 1996 as that was the midpoint year of our review. There was no significant difference in the proportional contribution of neonatal deaths to total deaths occurring during infancy (<1 yr) between the two periods (p = 0.141). Based on a descriptive analysis of the data, there seems to be some indication that the proportion may actually be increasing with time; however, we may have lacked sample size to determine a difference. There also was no difference in the proportional contribution by cause of death assignment method (Verbal autopsy vs. other methods; p = 0.715) or by study setting (urban vs. rural; p = 0.175).
The specific timing of neonatal deaths by day is also presented in Table 2. The median percentage of neonatal deaths by day 1 is 36.7% (Range: 20.0–58.0%). The median cumulative percentage of neonatal deaths by day 3 was 49.7% (Range 35.0–64.6%) and 70.9% (Range: 46.5–92.3%) by day 7.
Discussion
Multi-centric studies utilizing standardized tools to investigate child deaths in India were not conducted until the year 2000. Previous studies are characterized by small sample size and substantial variation in design and cause assignment methods, which makes comparisons between these early studies difficult and often unreasonable. The availability of comparable data is essential for accurate impact assessment of ongoing interventions and child survival programs. This scenario seems to be changing during the last decade, when not only study focus became multi-centric but more rigorous and tools like verbal autopsy were utilized [9–12, 39]. These recent surveys and studies likely provide a more accurate cause of child death structure for India compared to earlier institutional based studies which may not be representative of the general population [6, 9].
In this review, we were not able to assess trends in infant or child deaths due to a lack of methodologically similar data. It is expected that the recent advancements in design and analysis of cause of child death research in India discussed above will help in generating more comparable data, which in turn can be utilized for programmatic decision making.
On the other hand, there were a sufficient number of neonatal death studies, which employed reasonably similar cause of death definitions, to perform statistical analyses (Table 2). The studies reviewed in this article did not find any statistically significant change in the proportionate contribution of neonatal deaths to total infant deaths overtime. Similarly, there was no difference in the proportionate contribution of neonatal deaths between rural and urban areas. Both of these findings are contrary to the recent reported findings from two large scale surveys and a trend analysis of SRS data from India [4, 5, 40, 41]. We hypothesize that these differences may be due to methodological differences in older studies, where perinatal mortality was commonly studied and a large proportion of neonatal deaths were likely reported as still birth. Secondly, the majority of studies published in the 1980’s and 1990’s were conducted at academic institutions and hospitals, which may not be representative of the general Indian population. Global estimates on the causes of neonatal deaths, published in the year 2005, reported that neonatal deaths contributes to 37% of the all under five deaths [43]; however the National Family Health Survey-3 and a recent review article published data from SRS and RCGI, suggest that proportional contribution of neonatal deaths to the under five mortality rate (U5MR) in India is much higher than global proportion [4, 40]. We could not analyze the proportional contribution of neonatal deaths to the under five deaths in this review, since most studies with data on children under five did not present data specific to neonates.
This review also provides vital insight to the causes of neonatal deaths in India. Across all studies, the median percentage of neonatal deaths attributed to sepsis/pneumonia was 24.9%, while asphyxia was 18.5% and pre-maturity and Low Birth weight (LBW) together was 16.8%. Though estimates of the causes of under five deaths in India have recently became available [42], a separate analysis on causes of neonatal deaths is not available. Globally, preterm birth (28%), sepsis/pneumonia (26%), asphyxia (23%), congenital anomalies (8%), neonatal tetanus (7%), diarrhea (3%) are the most common causes of neonatal deaths [43]. This review and another article in this supplement suggest that the proportionate contribution from major causes of neonatal deaths in India i.e. pre-term births, sepsis or pneumonia and birth asphyxia, is slightly different than that in the rest of the world [4]. Furthermore, it is interesting to note that the timing of neonatal deaths seems to have remained strikingly constant during the last two decades with a majority occurring during the early neonatal period [10–26]. These findings are corroborated by the recent SRS survey report [9].
Authors in the past have also reported limited use of data for decision making in child survival, especially for the neonatal period [44]. It is time for accurate country specific child survival data to become regularly available for decision making in India. Our findings insist that more attention be placed on survival through the early neonatal period. The recently announced ‘Navjat Shishu Suraksha Karyakram’ and the platform of ‘Janani Suraksha Yojana’ may provide appropriate strategies to improve early neonatal survival in the country [45, 46].
Conclusions
During the last decade, there had been a few multi-centric studies and a national wide survey, which have provided valuable insight into the causes and timings of child deaths in India. Our review demonstrates the importance of continuing the methodological rigour and large sample sizes in future studies and surveys. Secondly, the review suggests that the causes of neonatal deaths in India may be different from the rest of the world. Our findings demand that neonatal survival interventions be prioritized in India and established upon country specific data. Thirdly, the majority of neonatal deaths still occur in early neonatal period in India, which is an important indication that continuum of care needs to be ensured throughout the country. The findings of this review may be useful for the program managers and policy makers to make informed decisions to ensure that India achieve MDG4 on time.
References
UNICEF United Nations Children’s Fund. The State of the World Children 2009: celebrating 20 years of the conventions on the right of the child. New York: UNICEF; 2009.
Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, post neonatal, childhood, and under 5 mortality for 187 countries, 1970–2010: a systematic analysis for progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2008.
United Nations. Millennium Development Goals. Accessed at www.un.org/millenniumgoals/ on Nov 18, 2007.
Lahariya C, Paul VK. Burden, differentials, and causes of child deaths in India. Indian J Pediatr 2010; 77: (Published online ahead of print on Sept 10, 2010). doi:10.1007/s12098-010-0185-z
Registrar General of India. Compendium of the vital statistics in India (1970–2007): Sample Registration system), RGI, Ministry of Home Affairs, New Delhi. 2009: 1–212.
Jha P, Gajalakshmi V, Gupta PC, Kumar R, Mony P, et al. Prospective study of one million deaths in India: rationale, design, and validation results. PLoS Med. 2006;3:e18.
Singh M. Hospital based data on perinatal and neonatal mortality in India. Indian Pediatr. 1986;23:579–84.
Kruskal WH, Wallis WA. Use of ranks in one criterion variance analysis. J Am Stat Assoc. 1952;47:583–621.
Registrar General of India. Report on causes of deaths in India 2001–2003. Sample Registration system, RGI, Ministry of Home Affairs, New Delhi. 2009;19–27.
Indian Council of Medical Research Young Infant Study Group. Age profile of neonatal deaths. Indian Pediatr. 2008;45:991–4.
Arora NK. The INCLEN Trust, New Delhi, India (Unpublished data: Personal Communication). 2010.
Baqui AH, Darmstadt GL, Williams EK, et al. Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programs. Bull World Health Organ. 2006;84:706–13.
Bang AT, Paul VK, Reddy HM, et al. Why do neonates die in rural Gadchiroli, India (Part I): primary causes of deaths assigned by neonatologist, based on prospective observed records. J Perinatol. 2005;25:S29–34.
Singhal PK, Mathur GP, Mathur S, et al. Neonatal morbidity and mortality in ICDS urban slums. Indian Pediatr. 1990;27:485–8.
Vaid A, Mammen A, Primrose B, et al. Infant mortality in an urban slum. Indian J Pediatr. 2007;74:449–53.
Thora S, Awadhiya S, Chansoriya M. Perinatal and infant mortality in an urban slums under ICDS scheme. Indian Pediatr. 1986;24:595–8.
Soudarssananne MB, Srinivasa DK, Narayan KA, et al. Infant mortality in Pondicherry—an anlysis of a cohort of 8185 births. Indian Pediatr. 1992;29:1379–84.
Hirve S, Ganatra B. A prospective cohort study on the survival experience of under 5 children in rural western India. Indian Pediatr. 1997;34:995–1001.
Awasthy S, Pande VK, Glick H. Under 5 mortality in urban slums of Lucknow. Indian J Pediatr. 1996;63:363–8.
Nandan D, Mishra SK, Jain M, et al. Social audit for community actions: a tool to initiate community action for reducing child mortality. Indian J Community Med. 2005;30:78–80.
Bhandari N, Bahl R, Taneja S, Martines J, Polian MK. Pathways to infant mortality in urban slums of Delhi, India: Implications for improving the quality of community and hospital-based programs. J Health Popul Nutr. 2002;20:148–55.
Shrivastava SP, Kumar A, Ojha AK. Verbal autopsy determined causes of deaths. Indian Pediatr. 2001;38:1022–5.
Chaturvedi P, Potdar S. Change in neonatal care pattern and neonatal mortality in rural medical college. Indian Pediatr. 1998;25:171–8.
Gupta HS, Baghel A. Infant mortality in urban slums: case study of Calcutta Metropolis and Raipur city. Int J Popul Geogr. 1999;5:353–66.
Bhardwaj N, Hasan SB. High perinatal and neonatal mortality in rural India. J R Soc Health. 1993;113:60–3.
Garg SK, Mishra VN, Singh JV, et al. Neonatal mortality in Meerut district. Indian J Med Sci. 1993;47(9):222–5.
Ravi Kumar M, Vishnu Bhatt B, Oumachigui A. Perinatal mortality trends in a referral hospital. Indian J Pediatr. 1996;63:357–61.
Awasthy S, Pande VK. Cause specific mortality in under in urban slums of Lucknow, North India. J Trop Pediatr. 1998;44:358–61.
Phukan RK, Mahanta J. A study of neonatal deaths in the tea gardens of Dibrugarh district of upper Assam. J Indian Med Assoc. 1998;96:333–4. 337.
Kapoor RK, Srivatava AK, Mishra PK, et al. Perinatal mortality in urban slums of Lucknow. Indian Pediatr. 1996;33:19–23.
Chavan YS, Dattal MS, Khadilkar VV, et al. Causes of early neonatal mortality. Indian Pediatr. 1992;29:781–3.
Sarna MS, Saili A, Dutta AK, et al. Neonatal mortality patterns in an urban hospital. Indian Pediatr. 1991;28:719–24.
Suguna Bai S, Mathews E, Nair PM, et al. Perinatal mortality rate in a south Indian population. J Indian Med Assoc. 1991;89:97–8.
Tandon BN, Sahai A, Balaji LN, et al. Morbidity pattern and cause specific mortality in infancy in ICDS projects. J Trop Pediatr. 1987;33:190–3.
Singhal PK, Mathur GP, Mathur S, et al. Mortality patterns in under six children in I.C.D.S. urban slum. Indian Pediatr. 1986;23:617–22.
Singh M, Deorari AK, Paul VK, et al. Primary causes of neonatal deaths in a tertiary care hospital in Delhi: an autopsy study of 331 cases. Ann Trop Pediatr. 1990;10:151–7.
Murthy BMS, PV WL, et al. Maternal nutritional status and practices & perinatal, neonatal mortality in rural Andhra Pradesh, India. Indian J Med Res. 2008;127:44–51.
Neilsen BB, Liljestrand J, Hedegaard M, et al. Reproductive pattern, perinatal mortality, and sex preference in rural Tamil Nadu, south India: community based, cross sectional study. BMJ. 1997;314:1521–4.
Jha P, Jacob B, Kumar R. Reliable measurement of the causes of mortality in developing countries. Int J Epidemiol. 2007;36:651–3.
International Institute for Population Sciences and Macro International. National Family Health Survey (NFHS-3), 2005–06: India: volume I. Mumbai: IIPS; 2007.
Pandey A, Bhattacharya BN, Sahu D, et al. Components of under five mortality trends, current stagnation and future forecasting levels. In: National Commission on Macroeconomics and Health: background papers—burden of disease in India. 2005: New Delhi; 152–78.
Registrar General of India. SRS Bulletin. Sample Registration system, RGI, Ministry of Home Affairs, New Delhi 2009: 44; 1: 1–6.
Bryce J, Boschi-Pinto C, Shibuya K, Black RE, WHO Child Health Epidemiology reference group. WHO estimates of causes of deaths in children. Lancet. 2005;365:1145–52.
Lahariya C, Khandekar J. How the findings of national family health survey-3 can act as a trigger for improving the status of anemic mothers and undernourished children in India: a review. Indian J Med Sci. 2007;61:535–44.
Lahariya C. Cash incentive for institutional delivery: linking with ante natal and post natal care may ensure ‘continuum of care’ in India. Indian J Community Med. 2009;34:15–8.
Government of India. National Rural Health Mission: progress over first 100 days of present government. Ministry of Health and Family Welfare press release on Sept 17, 2009. MoHFW, Nirman Bhawan, New Delhi. Accessed at http://www.pib.nic.in/release/rel_print_page.asp?relid=52710
The views expressed in this article are those of the authors and does not reflects the views of the organizations with whom they have been affiliated in the past or present. The author’s affiliation reflects the affiliation at the time of writing this article. The first author was at the G.R. Medical College, Gwalior at the time of data retrieval and writing the first draft of this manuscript.
Conflicts of interest
None.
Role of Funding Source
No funding was received for this work by any named author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lahariya, C., Sudfeld, C.R., Lahariya, D. et al. Causes of Child Deaths in India, 1985–2008: A Systematic Review of Literature. Indian J Pediatr 77, 1303–1311 (2010). https://doi.org/10.1007/s12098-010-0246-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-010-0246-3