Abstract
Background
Capectiabine is an oral antineoplastic drug used in multiple malignancies. Proton pump inhibitors (PPI) have been proven to interact with other oral antineoplastic agents. In this systematic review we will summarize the clinical evidence on the efficacy of capecitabine when used concomitantly with PPI.
Materials and methods
We performed a systematic literature search on the main databases up to November 2019.
Results
Nine studies met our inclusion criteria: 8 retrospective studies and 1 phase II clinical trial. Patients with colorectal, breast and gastroesophageal were represented. Four out of the 9 studies reported a shorter efficacy outcome in uni- or multivariate analysis when capecitabine was taken concomitantly with PPI than alone.
Conclusions
Up to date, the clinical evidence reported on the use of capecitabine concomitantly with PPI is scarce and shows conflicting results. While awaiting further data, avoiding misuse of PPI in cancer patients taking capecitabine is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Capecitabine is an antineoplastic drug with widespread use in oncology. It is commonly used alone or in combination in colorectal, breast, gastroesophageal, hepatobiliary, pancreatic, anal and neuroendocrine cancers [1]. Capecitabine is an oral pyrimidine analog of the antimetabolite group. It is a prodrug of 5-fluorouracil that needs to be hydrolyzed in tissues and liver and subsequently metabolized within cells into the active metabolites [2]. Proton pump inhibitors (PPIs) are the most effective therapy for gastric-acid-related diseases [3]. They bind covalently to the H+/K+ ATPase of the gastric parietal cell reducing gastric-acid secretion [4]. Their efficacy, tolerability, and safety have led a widespread use worldwide [5]. In fact, 20–55% of cancer patients take PPI [6]. However, concerns about overuse and misuse have been increasingly reported [5]. There is a well-known interaction between PPI and some oral antineoplastic agents, mainly multikinase inhibitors [7]. However, there is conflicting data regarding capecitabine. Although preclinical data suggest no interaction [8], the report of some retrospective studies showing decreased clinical efficacy when capecitabine was given concomitantly with PPI has led to the inclusion of this interaction in drug interaction databases such as Micromedex and Lexicomp [9, 10]. This systematic review aims to summarize the clinical evidence on the efficacy of capecitabine when administered concomitantly with PPI.
Materials and methods
Review design
This review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Data sources and search strategy
We searched the electronic databases MEDLINE, Pubmed Central, Embase and the Cochrane Library CENTRAL to identify all relevant records to November 2019. Our search strategy was restricted “proton pump”, “omeprazole”, “lansoprazole”, “dexlansoprazole”, “esomeprazole”, “pantoprazole”, “rabeprazole” or “ilaprazole” and “capecitabine” with no limits for time or language. We also searched published conference abstracts from the annual meetings of the American Society of Clinical Oncology (ASCO), European Society of Medical Oncology (ESMO) and other international meetings. Finally, we searched for ongoing clinical trials in US National Institutes of Health Ongoing Trials Register (www.clinicaltrials.gov). There was no restriction for language. The main author independently selected the reports included and then was revisited by the remaining authors. The study was conducted in compliance with local ethics regulations.
Inclusion and exclusion criteria
We included clinical trials and observational studies. Eligibility was restricted manuscripts that included comparative studies in patients with cancer treated with capecitabine, alone or in combination, with or without proton pump inhibitors. Manuscripts have to report at least one efficacy outcome (overall response rate [ORR], progression-free survival [PFS], disease-free survival [DFS] or overall survival [OS]). Single-arm studies and preclinical studies were excluded.
The primary outcomes were median PFS/DFS, median OS since the start of the treatment and ORR. ORR was determined by the sum of complete response (CR) and partial response (PR).
Study selection, data extraction and quality assessment
The lead author (DV) carried out the first screening of article. A author (NR) validated the screening. DV and both assessed full-text articles. Discrepancies were discussed to reach a consensus. Three independent reviewers (JF, OH, IG) assessed study quality.
Results
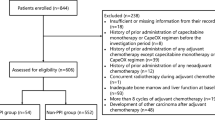
Within a multistep process, we have screened 468 records for duplicates and eligibility, resulting in 10 publications undergoing abstract/full-text screening (Fig. 1) [11,12,13,14,15,16,17,18,19,20]. Our final study selection included 8 retrospective studies [11,12,13,14,15,16,17,18,19] and 1 phase II clinical trial [19]. Of these records, there are 2 conference abstracts found on Embase that met the inclusion criteria [17, 19]. Significant heterogeneity was found between studies. Six of the 9 studies included patients with colorectal cancer [11,12,13,14,15,16]. Other types of tumor included were breast [17], gastroesophageal [18], and gastrointestinal [19]. Patients had capecitabine in the neoadjuvant (N = 1), adjuvant (N = 2), metastatic (N = 4) or both (N = 2) setting. The number of patients varies between 61 and 455. Capecitabine was administered either alone (N = 4) or in combination with oxaliplatin (CapeOX) (N = 3). One arm of the study by Chu MP et al. added lapatinib to capecitabine-oxaliplatin as part of a clinical trial [18]. The PPI under evaluation also varied between the studies. Most of the studies included all PPI [12, 14, 16,17,18], while others only included patients treated with omeprazole [11, 15] or rabeprazole [20]. Rineheart et al. included any anti-acid suppressant therapy [15].
Efficacy results of the 9 studies are included in Table 1. Overall, 4 out of the 9 studies showed that patients treated with capecitabine and PPI had worse clinical outcome than patients treated with capecitabine alone [12, 13, 16, 18]. Three of the 6 studies including patients with colorectal cancer showed a shorter PFS for the combination group in uni or multivariate analysis [12, 13, 16]. However, none of them showed a significant association with OS. Patients with gastric cancer were represented in two studies [17, 18]. The retrospective study by Yang et al. (abstract) [17], did not show any association with survival. In the post-hoc analysis of a phase III trial by Chu et al. [18], a significant association with worse PFS and OS was seen in multivariate analysis for patients treated with CapeOX and PPI. This difference was not seen in the arm of CapeOX-lapatinib. Breast cancer patients were included in the study of Yang et al. [17], but no difference was seen for efficacy between the two arms.
Discussion
Up to date, 9 studies [11,12,13,14,15,16,17,18,19], including 2 congress abstracts [17, 19], have explored the efficacy of capecitabine when given concomitantly with PPI. Four of them found a detrimental effect of PPI on capecitabine efficacy [12, 13, 16, 18], while the small phase II trial [19] and other retrospective studies do not [11, 14, 15, 17].
Capecitabine should be taken with water within 30 min after a meal. Food decreases the rate of absorption but does not affect systemic metabolite levels [1]. Although traditionally there has been no advice for concomitant PPI use, recent drug interaction platforms have included this interaction based on two of the most solid retrospective studies [9, 10]. Wong et al. [12] reported a detrimental effect in RFS and OS of concomitant adjuvant CapeOX and PPI in patients with localized colorectal cancer (HR for RFS: 2.20, P: 0.018 in multivariate analysis). Interestingly, in patients receiving FOLFOX as adjuvant therapy, no significant effect of concomitant PPI was observed. Chu et al. [18] also reported a detrimental effect on PFS and OS in multivariate analysis when CapeOX was administered concomitantly with PPI vs alone in patients with metastatic GE cancer in a post-hoc analysis of a phase III trial (TRIO-013). This effect was not significant when lapatinib was added to the chemotherapy backbone. Other studies support to some extent this hypothesis. Rhinehart et al. [13] found a shorter PFS in 70 patients with localized or metastatic colon cancer treated with capecitabine and concomitant acid-suppression therapy (PPI or histamine 2 receptor antagonists) after adjustment for disease severity and age. Sun et al. [16] found a detrimental association for PFS in univariate analysis in patients with localized colon cancer when adjuvant capecitabine was administered concomitantly with PPI. However, it did not reach significance in multivariate analysis.
On the other hand, a small phase II trial and other less robust studies have indeed opposite outcomes. Roberto M et al. [19], owing to a possible beneficial effect of rabeprazole in preclinical and early clinical data [20], presented at ESMO 21st World Congress on Gastrointestinal Cancer as an abstract the updated results of combining high-dose proton-pump inhibitor rabeprazole as a salvage treatment for 61 patients with refractory advanced GI cancers. There were no significant differences in PFS in both arms of the study. OS was numerically better in the combination arm (10 vs 6 months); however, it did not reach statistical significance (P = 0.6). Surprisingly, hand-foot syndrome was more frequently reported in the combination arm. Yang et al. [17] presented as an abstract at the 33rd International Conference on Pharmacoepidemiology & Therapeutic Risk Management a post-hoc analysis evaluating the efficacy of capecitabine and PPI of three randomized phase III trials including breast and gastric cancer. No effect on PFS was observed and results on OS were not reported. Zhang et al. [15] did not find a significant difference among users and non-users of omeprazole in patients with colorectal cancer when capecitabine was used with concomitant radiotherapy as part of the neoadjuvant treatment. However, patients that had 200 mg of omeprazole have a longer DFS and OS in multivariate analysis (HR = 0.30, 95%CI: 0.09–0.99, P = 0.048). The concomitant use of radiotherapy may hinder the actual effect of capecitabine. Other retrospective studies did not find any relationship of combination therapy with efficacy.
One of the main reasons for this possible interaction relies on the hypothesis that PPI, by increasing gastric pH, may reduce dissolution and absorption of capecitabine. However, the dissolution of capecitabine tablet is similar in a wide range of pH (2–6.8) and drug ionization is theoretically minimal at the pH induced by PPI [8]. A study with the antiacid Maalox found a small increase in capecitabine and little impact of 5-FU systemic levels. However, PPI are more potent gastric antiacid than Maalox, and thus the former may have more impact on blood levels of capecitabine [21]. Other authors have even attributed antineoplastic properties to PPI due to the blockade of the V-H(+)-ATPases on cancer cells [14, 22]. There are few pharmacokinetic studies on the topic. Sekido M et al. [20] found no significant effects of rabeprazole on the area under the plasma concentration–time curve divided by capecitabine dose for capecitabine and its three metabolites. Overall, preclinical and pharmacokinetic evidence does not seem to preclude the use of capecitabine with concomitant PPI. Recently, it has been postulated that gut microbiome modulates the toxicity profile of chemotherapy and the response to cancer therapy, mainly immunotherapy [23]. A preclinical report showed that some bacteria may modify some chemotherapy agents efficacy, although it was not for capecitabine [24].
This controversy is raised in a context of a worldwide overuse and misuse of PPI. In Europe, the use of PPI has dramatically increased in some countries. For example, in Spain, omeprazole ranked number one in drug sales in 2010, and the use has quadrupled since the year 2000 [25]. It is estimated that misuse reaches 50% of the prescriptions, mainly due to inappropriate prevention of pharmacological gastric damage and stress ulcer prevention in low-risk hospitalized patients [26].
Multiple caveats limit the interpretation of the results. The retrospective nature of the main studies and the small number of patients in the clinical trial only provides low-quality evidence. Different tumors, clinical scenarios, chemotherapy regimens, and PPI used further limits the generalization of the results. The use of PPI previous to the start of capecitabine may reflect an underlying disease that could influence efficacy outcomes and concomitant disease, concomitant medications and performance status are not commonly taken into account in the studies.
In conclusion, at this moment, only low-quality studies have addressed the efficacy of capecitabine and concomitant PPI and the results are conflicting. Prospective studies addressing the role of capecitabine and proton pump inhibitors need to be carried out. Until further evidence sheds some light in the issue, adequate prescription of PPI should be encouraged to avoid overuse and misuse of PPI.
References
Capecitabine (package insert). San Francisco, CA: Genentech USA Inc; 2016.
Miwa M, Ura M, Nishida M, et al. Design of a novel oral fluoropyrimidine carbamate, capecitabine, which generates 5-fluorouracil selectively in tumours by enzymes concentrated in human liver and cancer tissue. Eur J Cancer. 1998;34:1274–81.
Malfertheiner P, Kandulski A, Venerito M. Proton-pump inhibitors: understanding the complications and risks. Nat Rev Gastroenterol Hepatol. 2017;14(12):697–710. https://doi.org/10.1038/nrgastro.2017.117.
Sachs G, Shin JM, Briving C, Wallmark B, Hersey S. The pharmacology of the gastric acid pump: the H+, K+ ATPase. Annu Rev Pharmacol Toxicol. 1995;35:277–305.
Savarino V, Marabotto E, Zentilin P, et al. Proton pump inhibitors: use and misuse in the clinical setting. Expert Rev Clin Pharmacol. 2018;11(11):1123–34. https://doi.org/10.1080/17512433.2018.1531703.
Smelick GS, Heffron TP, Chu L, Dean B. Prevalence of acid-reducing agents (ARA) in cancer populations and ARA drug–drug interaction potential for molecular targeted agents in clinical development. Mol Pharm. 2013;10(11):4055–62. https://doi.org/10.1021/mp400403s.
Hussaarts KGAM, Veerman GDM, Jansman FGA, et al. Clinically relevant drug interactions with multikinase inhibitors: a review. Ther Adv Med Oncol. 2019;11:1758835918818347. https://doi.org/10.1177/1758835918818347.
Cheng V, Lemos M, Hunter N, Badry N, Lemos J. Concomitant use of capecitabine and proton pump inhibitors—is it safe? J Oncol Pharm Pract. 2019;25(7):1705–11. https://doi.org/10.1177/1078155219846952.
MICROMEDEX 2.0 Drug Interactions (database on the Internet). Capecitabine. Truven Health Analytics, updated periodically. www.micromedexsolutions.com. Accessed 1 Dec 2017.
Lexicomp Online: interactions (database on the Internet). Capecitabine. Lexi-Comp.
Lu CX, Zheng BW, Bai B, et al. Effect of omeprazole on plasma concentration and adverse reactions of capecitabine in patients with colon cancer. Zhonghua Zhong Liu Za Zhi. 2019;41(9):708–11. https://doi.org/10.3760/cma.j.issn.0253-3766.2019.09.012.
Wong GG, Ha V, Chu MP, Dersch-Mills D, et al. Effects of proton pump inhibitors on FOLFOX and CapeOx regimens in colorectal cancer. Clin Colorectal Cancer. 2019;18(1):72–9. https://doi.org/10.1016/j.clcc.2018.11.001.
Rhinehart HE, Phillips MA, Wade N, Baran A. Evaluation of the clinical impact of concomitant acid suppression therapy in colorectal cancer patients treated with capecitabine monotherapy. J Oncol Pharm Pract. 2019;25(8):1839–45. https://doi.org/10.1177/1078155218818237.
Wang X, Liu C, Wang J, Fan Y, Wang Z, Wang Y. Proton pump inhibitors increase the chemosensitivity of patients with advanced colorectal cancer. Oncotarget. 2017;8(35):58801–8. https://doi.org/10.18632/oncotarget.18522.
Zhang JL, Liu M, Yang Q, Lin SY, Shan HB, Wang HY, Xu GL. Effects of omeprazole in improving concurrent chemoradiotherapy efficacy in rectal cancer. World J Gastroenterol. 2017;23(14):2575–84. https://doi.org/10.3748/wjg.v23.i14.2575.
Sun J, Ilich AI, Kim CA, Chu MP, Wong GG, Ghosh S, Danilak M, Mulder KE, Spratlin JL, Chambers CR, Sawyer MB. Concomitant administration of proton pump inhibitors and capecitabine is associated with increased recurrence risk in early stage colorectal cancer patients. Clin Colorectal Cancer. 2016;15(3):257–63. https://doi.org/10.1016/j.clcc.2015.12.008.
Yang JY, Sanoff HK, Sandler RS, Stürmer T, Funk MJ, Lund JL. Does proton-pump inhibitor use diminish capecitabine efficacy in advanced cancer patients? Pharmacoepidemiology Drug Safety. 2017;26(Supplement 2):222–3.
Chu MP, Hecht JR, Slamon D, et al. Association of proton pump inhibitors and capecitabine efficacy in advanced gastroesophageal cancer: secondary analysis of the TRIO-013/LOGiC randomized clinical trial. JAMA Oncol. 2017;3(6):767–73. https://doi.org/10.1001/jamaoncol.2016.3358. (Erratum. In: JAMA Oncol. 2017 Dec 1;3(12):1742).
Roberto M, Arrivi G, Milano A, et al. Updated results of a phase II randomized trial with high dose proton pump inhibitors and metronomic capecitabine as salvage treatment for patients with advanced gastrointestinal tumours. Ann Oncol. 2019;30(Supplement 4):AA43–AA44.
Sekido M, Fujita KI, Kubota Y, et al. Rabeprazole intake does not affect systemic exposure to capecitabine and its metabolites, 5′-deoxy-5-fluorocytidine, 5′-deoxy-5-fluorouridine, and 5-fluorouracil. Cancer Chemother Pharmacol. 2019;83(6):1127–35. https://doi.org/10.1007/s00280-019-03837-y.
Reigner B, Clive S, Cassidy J, et al. Influence of the antacid Maalox on the pharmacokinetics of capecitabine in cancer patients. Cancer Chemother Pharmacol. 1999;43:309–15.
Chen M, Zou X, Luo H, et al. Effects and mechanisms of proton pump inhibitors as a novel chemosensitizer on human gastric adenocarcinoma (SGC7901) cells. Cell Biol Int. 2009;33(9):1008–199. https://doi.org/10.1016/j.cellbi.2009.05.004.
Roy S, Trinchieri G. Microbiota: a key orchestrator of cancer therapy. Nat Rev Cancer. 2017;17(5):271–85. https://doi.org/10.1038/nrc.2017.13.
Lehouritis P, Cummins J, Stanton M, et al. Local bacteria affect the efficacy of chemotherapeutic drugs. Sci Rep. 2015;5:14554. https://doi.org/10.1038/srep14554.
Lanas A. We are using too many PPIs, and we need to stop: a European perspective. Am J Gastroenterol. 2016;111(8):1085–6. https://doi.org/10.1038/ajg.2016.166.
Van Vliet EP, Otten HJ, Rudolphus A, et al. Inappropriate prescription of proton pump inhibitors on two pulmonary medicine wards. Eur J Gastroenterol Hepatol. 2008;20:608–12.
Acknowledgements
This work has not been supported by public grants or financial support. No sources of funding were used to assist in the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: DV; writing—original draft preparation: DV, NR; writing—review and editing: PP-W, JF, OH, IG. Supervision: NR-S, JF.
Corresponding author
Ethics declarations
Conflict of interest
JF has a consulting and advisory role in Amgen, Ipsen, Eisai, Merck, Roche and Novartis, Has received research funding from Merck and has received travel and accommodation expenses from Servier. The rest of the authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Viñal, D., Rodriguez-Salas, N., Perez-Wert, P. et al. Efficacy of capecitabine when used concomitantly with proton pump inhibitors in cancer patients: a systematic review. Clin Transl Oncol 22, 1288–1294 (2020). https://doi.org/10.1007/s12094-019-02254-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02254-0