Abstract
Introduction
Primary objective of the study was to assess the relative weighting between benefit in survival time (SV), benefit in quality of life (QoL) and willingness to experience adverse events (AEs), in patient preferences for chemotherapy treatment.
Materials and methods
We included cancer patients with current or past systemic treatment of cancer (STC) as well as physicians placed as hypothetical patients. Participants filled a choice-based conjoint analysis questionnaire with 19 choices among three STC scenarios with variable amounts of benefit in SV or QoL and different types AEs.
Results
One hundred patients (50 on curative and 50 on palliative intention treatment) and 114 physicians (61 oncologists and 53 non-oncologists) were included and asked about their preferred chemotherapy treatment. The relative weighting (sum 100%) of SV–QoL–AEs for making the choice in the 100 patients was SV35%–CV33%–AEs31% what was not significantly different from a random distribution (Goodness of fit Chi square P = 0.91) just as it was not for both subgroups, palliative (SV37%–QoL29%–AEs34%; GoF Chi square P = 0.55) and curative (SV34%–QoL36%–AEs30%; GoF Chi square P = 0.73) treatment. The observed distribution in the group of 114 physicians (SV46%–QoL31%–AEs23%) was significantly different from a random distribution (GoF Chi square P = 0.018) just as it was for both subgroups, medical oncologists (SV48%-QoL29%-AEs23%; GoF Chi square P = 0.006) and non-medical oncologists (SV44%–QoL33%–AEs23%; GoF Chi square P = 0.04).
Conclusions
The three attributes (SV, QoL, and AEs) are considered in the same way by cancer patients to make choices on their STC. On the contrary, when placed as hypothetical patients, physicians prefer for themselves those treatments that provide more SV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
New drug developments come in many shapes and sizes. Some are disruptive and even life saving, but unfortunately, more often they come with only incremental clinical benefits. The former generate undisputable improvements in survival that outweigh the risk from their potential adverse events (AEs). For the latter, though, the benefit-risk ratio can be subject of different views and interpretations. In this context, patient preferences have been ignored by physicians when taking clinical decisions, by technology evaluation agencies [1] and regulatory bodies when delineating regulatory approval rules as well as by scientific societies when designing value framework tools [2, 3].
The so-called personalized treatment of cancer is a successful concept, accepted by all the stakeholders [4, 5]. Likewise, patient preferences would play a role in the personalization of cancer treatment if they could be used as therapeutic targets for treatment decision making [6, 7]. To investigate these issues, we have designed a mathematical model which simulates a perfect-competition market in which the consumer is a patient with an advanced cancer who seeks to acquire benefits from systemic treatment. In this market, the patient must pay the price in the form of AEs instead of paying with monetary units. We have named this model “The Oncology Market”. In the first study, published in 2017, we showed that patients were able to score, in a reproducible way, the impact of AES on their QoL [8]. In the second study, whose results we are presenting herein, we use choice-based conjoint analysis to determine the weighting of the benefits (prolongation of survival time and improvement in QoL) and the price to pay (AEs), in the choice of a therapeutic regimen as the preferred one by a particular patient who needs to be treatment for an advanced cancer. Conjoint analysis is useful to assess how people value several characteristics of consumer goods together and was originally designed to conduct market studies. However, it has also been used for more than 20 years to elicit patient preferences [9] and has recently proven to be useful in cancer patients [10]. Taking the comparison with a capitalist market to the extreme, we tried to assess the trade-off rate between “additional survival time” and “enhanced QoL”, as two market goods. The interest of this analysis lies in that both goods (benefits from treatment) are the two dimensions of the QALYs [11]. Indeed, using microeconomics terminology, we investigated if survival time and QoL may be defined as two perfect supplementary goods (such as blue and red pencils for a consumer who wants many pencils and he does not care about the color), or as two perfect complementary goods (such as shoes on the right and left foots which consumers mostly wants to buy in pairs).
Methods
Study design
This is a cross-sectional study in which the subjects responded to a questionnaire designed with choice-based conjoint analysis method. In addition, they must answer a single straightforward question outside the conjoint analysis questionnaire.
Conjoint analysis
Three different attributes were included, two benefits provided by chemotherapy treatment (the goods) and AEs (the price). The target benefits were additional survival time and improvement in QoL, both provided by treatment compared with the no-treatment option. Nineteen questions were formulated as follows: “Which of these three treatments associated with these three different scenarios of improvement in survival time, enhancement of QoL and AEs, would you prefer to receive as a treatment for advanced cancer? You can refuse those options and choose a no-treatment option (the fourth option in every choice)”. Table 1 shows the attributes, the levels and a sample of the 19 choices among 3 scenarios (out of 288 possible combinations of benefit in survival time/benefit in QoL/AEs) that the participants had to make. Survival time (SV) benefit was measured in months or years from < 1 month to 5 years or more (segmented into 6 levels). The benefit in QoL was measured with the result on a visual analog scale between 0, the worst conceivable QoL and 100, the best conceivable QoL. The scenarios showed increases of varying magnitude from one QoL level to another from “it is at 10, and it stands at 10” to “it goes up from 10 to 90” (six levels). QoL was meant as a scale of treatment benefit and, therefore, could only change towards improvement (or no changes, in the worst case). Patients received a detailed explanation (Fig. 1) of the four AEs: alopecia (total), vomiting (mild or NCI-CTC v4 grade 1–2, severe or grade 3–4), peripheral neuropathy (grade 1–2–3, according to the oxaliplatin-associated scale) and acneiform rash (mild or grade 1, severe or grade 2–3–4). The number of levels of the attributes must be limited; the four AEs were selected in an investigator discussion roundtable.
Straightforward question
The subjects answered the following question: “Please, imagine that you have 100 euros cash and you are in an outlet with two stores. One of them sells a good called quantity of life, and the other sells another good called quality of life. You are buying a basket with a certain amount of each good, according to your preferences. How would you distribute the 100 euros between the two goods?” You must spend the whole 100 euros available.
Study populations
Participating subjects were divided into two groups: on the one hand, patients with cancer who had received systemic antitumor treatment; on the other, physicians working in the participating centers. Of note, physicians were placed in the role of hypothetical patients, and, therefore, they were asked to respond for themselves as if they were cancer patients, not about their preferences for treating their patients. Key inclusion criteria for patients with cancer were age 18 years or older, histological diagnosis of cancer and previous or ongoing systemic cancer treatment. Physicians had to be over 18, and they should have not a prior history of cancer. The group of patients was divided into two subgroups, patients with systemic treatment of curative attempt (adjuvant or neoadjuvant) and patients with palliative treatment. The group of physicians was also divided into two subgroups, oncologists and non-oncologists.
Endpoints and format of the results
The results of the conjoint analysis are shown in percentages (sum to 100%) reflecting the relative weight of the impact of the three attributes (survival time, QoL and AEs) for the choices made by the subjects. The study was designed with two co-primary endpoints, to analyze the weighting between the quantity of time–QoL–AEs as assessed using conjoint analysis both in cancer patients and physicians, respectively. A secondary endpoint was the allocation of 100 euros amongst survival time and QoL in response to the straightforward additional single question.
Statistical analysis
Choice-based conjoint analysis was performed to carry out a conditional logit model. When estimating the utility for each attribute, it is possible to estimate the average importance (weight) for each of these attributes as well as the average utility of each of the levels of these factors. The weighting of each attribute is estimated as a function of the range of utilities observed for each level of the attributes. This means that an attribute with a wide range of utilities in its levels will have a greater estimated weight, Ii = [Max Ui − Min Ui) × 100/Σj (Max Uj − Min Uj)] where:
Ii = Importance (weight) of the attribute i,
Max Ui = Maximum utility of the attribute i,
Min Ui = Minimum utility of the attribute i,
Σj = Sum of the profit differences of all attributes.
We compared the distribution of responses of the conjoint analysis in the two cohorts (cancer patients and physicians) with a purely random distribution with the Goodness of fit Chi square test. In turn, the result of the straightforward question on the allocation of 100 euros is shown as a percentage for the eleven possible pairs of figures (survival time-QoL) from (0–100€) to (100–0€) and compared between patients and physicians with Chi square test of independence. For sample size calculation, Goodness of fit Chi square requires expected frequency counts higher than 5. A sample size of 100 patients and 100 physicians is considered enough to make this comparison because expected counts with three categories and 2 (3 minus 1) freedom-degrees are n × p (100 × 0.33) = 33, what is substantially higher than 5.
Ethics
The study was approved by the institutional review board (IRB) of the participant centers and was conducted by the regulations of the Declaration of Helsinki (Fortaleza 2013 version). All patients signed written informed consent before their inclusion in the study. Data from physicians were anonymized instead of codified so that, from the moment of the completion of the questionnaire, it was not possible to associate this questionnaire with that person; therefore, with the authorization of the IRB, only oral assent was required for physicians without the need to sign written consent.
Results
One hundred cancer patients and 114 physicians were included in the study between April 2016 and May 2017. Forty-nine and 71 (62%) were women among patients and physicians, respectively. The most frequent diagnostic was colorectal cancer (n = 29) followed by lung cancer (n = 17) and breast cancer (n = 17). Fifty and fifty patients received palliative systemic treatment of cancer and treatment with curative intention, respectively. Treatment included chemotherapy with or without biologicals in 90 patients, and 10 were treated with biologics without chemotherapy. Treatment was ongoing in 77 patients. Table 2 shows the demographic characteristics of the subjects. Physicians were chosen from six Hospitals. Among them, 61 (54%) were Medical Oncologists, and 53 (46%) were physicians with other medical and surgical specialties (general practitioners 10, medical specialties 18, surgical specialties 25).
Analysis on the primary endpoint showed that relative weighting of additional SV–improved QoL–AEs (or otherwise the two “goods” and their “price to pay” in the oncology market we have set up) are SV35%–QoL33%–AEs32%, respectively, as factors considered by cancer patients to decide what treatment regimen is their preferred one (Fig. 2). This distribution is not different from a random distribution of one third each (Goodness of fit Chi square P = 0.91). Neither the palliative subgroup of patients (SV37%–QoL29%–AEs34%; Goodness of fit Chi square P = 0.55) nor the curative subgroup of patients (SV34%–QoL36%–AEs30%; Goodness of fit Chi square P = 0.73) showed significant differences with a random distribution. The “goods” and “price to pay” distribution in the group of physicians was SV46%–QoL31%–AEs23%, respectively, which gives much more weight to survival time and far less to AEs (Goodness of fit Chi square P = 0.018). The weighting distribution was different from a random distribution in both physician subgroups, medical oncologists (SV48%–QoL29%–AEs23%; Goodness of fit Chi square P = 0.006) and non-medical oncologists (SV44%–QoL33%–AEs23%; Goodness of fit Chi square P = 0.04).
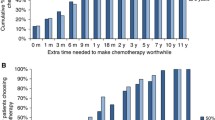
Regarding the monetary allocation of 100 euros between survival time and QoL (Fig. 3), 47% of the patients opted for (50–50), in contrast with only 17% physicians who opted for (50–50) with the other responses evenly distributed among the other pairs (Chi square P < 0.001 for comparison between patients and physicians).
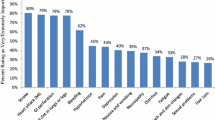
We measured the impact of the different levels on the choices made by the subjects (Fig. 4). The results are around 0 (no impact), with positive scores meaning that the presence of that in a particular scenario motivates the participants to choose that scenario, more intensely as the scores were higher; the reverse occurred for negative scores 1. It should be highlighted that alopecia is placed among the mild AEs with a positive impact on choices. The results on QoL are also remarkable. The impact associated to “improvement from 10 to 50” is negative while “improvement from 40 to 60” is positive whereas “improvement from 50 to 90” is the most valued and its value is somewhat higher than “improvement from 10 to 90”.
Discussion
The results of this study show that cancer patients give similar weight to the benefit in additional survival time, to the benefit in improved QoL and to the price they must pay for them in the form of AEs. Interestingly, physicians responded differently, with more weight put on survival time and less on price-AEs. The result of the conjoint analysis in patients, who weighted the three attributes equally, has been consistent with the result of the straightforward question about the distribution of 100 euros between survival time and QoL. Indeed, a remarkable accumulation of patient responses was observed in (50–50) which means that patients prefer those treatments from which they derive proportional and equivalent amounts of both benefits. We should underline that this result challenges the basics of the definition of QALYs [11] since all QALYs are equal concerning reimbursement [12], regardless of the specific contribution of quantity or quality of life. However, it seems that patients would prefer squared-shape QALYs to more rectangular-shape QALYs with extreme values of one of the two factors. As far as we know, this is the first time that conjoint analysis has been used to determine the relative value between lifetime and QoL. Previous studies that addressed this issue showed that oncologists value prolongation of survival time more than QoL [13-15]. One of these studies used the incremental cost-effectiveness ratio (ICER) values to estimate willingness to pay for the benefits in cancer patients and oncologists [15]. The results showed that oncologists prioritized, for their patients, treatments that improved survival time (106,000 €/QALY) over those treatments that improved QoL (65,000 €/QALY) while patients valued both similarly, with intermediate values for both, survival time improvement (73,520€/QALY) and QoL (82,917€/QALY). Our results are in full agreement with these observations which in turn, provide further support to our insight on the patient preferences for squared-shape over rectangular-shape QALYs.
The design of the questionnaire matters. We have evaluated the same endpoint with both a reliable, very difficult to deceive, complex questionnaire (conjoint analysis) and a straightforward, obvious and easier to deceive single question. While physicians have clearly shown a preference for survival time over QoL in the most reliable questionnaire, they evenly responded to the straightforward question without favouring either of them. Therefore, the complex or straightforward structure of the questionnaire may have an impact on the results. However, this concern seems less likely in patients, who have shown a perfect level of coherence in our study.
Two issues should be pointed out regarding the results on QoL. First, it looks like that patients pay more attention to the final value than the absolute benefit value. Second, what patients want not to hear about is to find themselves at any time with very poor quality of life. This explains why the enhancement of QoL “50–90” is the most preferred, even more than “10–90”, while the rise “10–50” is not valued by the subjects in the study.
This present study has some weaknesses. First, the AEs are not desired by the patients because they may impair QoL that, in turn, was one of the benefits that was considered. This could have been confusing for the subjects. However, the results have been coherent and did not show inconsistencies regarding this issue. Second, it is difficult to determine how the results of the study may have been affected by the fact that only one of the four subgroups of the study (patients with palliative treatment) is a genuinely ex-post population.
Our research group will conduct further works on this topic with a forthcoming third study in the setting of “The Oncology Market” project. We are committed to investigating how a preference-based decision-making strategy increases at zero-cost both the utility that patients derive and societal welfare. Incorporation of patient preferences will play an essential role in the treatment of cancer patients in the next years [16, 17] thus dismantling a paternalistic and inefficient attitude of decision-making bodies for drug approval and reimbursement. Moreover, all these aims would be achieved without challenging the constraint on the economic healthcare financial burden. These outcomes can be adequately measured with utility functions which assign numerical values to specific outcomes so that baskets with preferred outcomes combinations reach the highest scores [16, 18]. Utilitarianism-based decision-making guides choices to achieve the greatest benefit for the highest number of patients [19] aiming to reach a Pareto optimal balance [20] in which no patient may increase his welfare without worsening that of others.
In conclusion, unlike physicians, who prioritize survival prolongation over quality of life, cancer patients mostly prefer treatments providing equivalent and proportional amounts of survival time and QoL, which result in squared-shape QALYs. These two treatment benefit dimensions behave as two perfect complementary goods for cancer patients.
References
Ho M, Saha A, McCleary KK, et al. A Framework for incorporating patient preferences regarding benefits and risks into regulatory assessment of medical technologies. Value Health. 2016;19(6):746–50.
Allen JD, Stewart MD, Roberts SA, Sigal EV. The value of addressing patient preferences. Value Health. 2017;20(2):283–5.
Perfetto EM, Oehrlein EM, Boutin M, Reid S, Gascho E. Value to whom? the patient voice in the value discussion. Value Health. 2017;20(2):286–91.
Collins DC, Sundar R, Lim JSJ, Yap TA. Towards precision medicine in the clinic: from biomarker discovery to novel therapeutics. Trends Pharmacol Sci. 2017;38(1):25–40.
Arnedos M, Soria JC, Andre F, Tursz T. Personalized treatments of cancer patients: a reality in daily practice, a costly dream or a shared vision of the future from the oncology community? Cancer Treat Rev. 2014;40(10):1192–8.
Adunlin G, Diaby V, Montero AJ, Xiao H. Multicriteria decision analysis in oncology. Health Expect. 2015;18(6):1812–26.
Blinman P, King M, Norman R, Viney R, Stockler MR. Preferences for cancer treatments: an overview of methods and applications in oncology. Annals Oncol. 2012;23(5):1104–10.
Valentí V, Ramos J, Pérez C, et al. Adverse events from systemic treatment of cancer and patient-reported quality of life. JCSO. 2017;15(5):e256–e262262.
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530–3.
Beusterien K, Grinspan J, Kuchuk I, Mazzarello S, Dent S, Gertler S, Bouganim N, Vandermeer L, Clemons M. Use of conjoint analysis to assess breast cancer patient preferences for chemotherapy side effects. Oncologist. 2014;19(2):127–34.
Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Health. 2009;12(Suppl 1):S5–9.
Woodward RM, Menzin J, Neumann PJ. Quality-adjusted life years in cancer: pros, cons, and alternatives. Eur J Cancer Care (Engl). 2013;22(1):12–9.
Kozminski MA, Neumann PJ, Nadler ES, Jankovic A, Ubel PA. How long and how well: oncologists’ attitudes toward the relative value of life-prolonging v. quality of life-enhancing treatments. Med Decis Mak. 2011;31(3):380–5.
Greenberg D, Hammerman A, Vinker S, Shani A, Yermiahu Y, Neumann PJ. Which is more valuable, longer survival or better quality of life? Israeli oncologists’ and family physicians’ attitudes toward the relative value of new cancer and congestive heart failure interventions. Value Health. 2013;16(5):842–7.
Dilla T, Lizan L, Paz S, et al. Do new cancer drugs offer good value for money? The perspectives of oncologists, health care policy makers, patients, and the general population. Patient Prefer Adherence. 2015;10:1–7.
Broekhuizen H, IJzerman MJ, Hauber AB, Groothuis-Oudshoorn CGM. Weighing clinical evidence using patient preferences: an application of probabilistic multi-criteria decision analysis. Pharmacoeconomics. 2017;35(3):259–69.
EMA. Reflection paper on benefit-risk assessment methods in the context of the evaluation of marketing authorisation applications of medical products for human use: report of the CHMP working group on benefit-risk assessment methods. London; 2008. https://www.emea.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideline/2010/01/WC500069634.pdf. Accessed 6 Dec 2016.
Arnold D, Girling A, Stevens A, Lilford R. Comparison of direct and indirect methods of estimating health state utilities for resource allocation: review and empirical analysis. BMJ. 2009;339:b2688.
Dolan P. Utilitarianism and the measurement and aggregation of quality–adjusted life years. Health Care Anal. 2001;9(1):65–766.
Kaplan RM, Babad YM. Balancing influence between actors in healthcare decision making. BMC Health Serv Res. 2011;11:85.
Funding
“Associació Oncológica Dr Amadeu Pelegrí” (www.aodapelegri.com), which is a charitable association leaded by cancer patients based in Salou (Spain).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest regarding the publication of this article.
Ethical approval
The study was approved by the Institutional Review Board of the participant centers.
Informed consent
All the patients signed written informed consent before their inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valentí, V., Ramos, J., Pérez, C. et al. Increased survival time or better quality of life? Trade-off between benefits and adverse events in the systemic treatment of cancer. Clin Transl Oncol 22, 935–942 (2020). https://doi.org/10.1007/s12094-019-02216-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02216-6