Abstract
Purpose
Salvage radiotherapy (SRT) for biochemical recurrence (BCR) following radical prostatectomy (RP) should if possible be added at a prostate-specific antigen (PSA) level of <1–2 ng/mL. The value of positron emission tomography combined with computed tomography (PET/CT) at such low PSA values is not defined. The purpose was to determine what proportion of a well-defined cohort of hormone-naïve patients who were candidates for early salvage radiotherapy had 18F-choline PET/CT findings suggesting metastases.
Materials and methods
Patients with untreated BCR following RP, PSA <2 ng/mL, and Gleason score ≥7 or PSA doubling time ≤6 months underwent 18F-choline PET/CT. Focal choline uptake in lymph nodes or skeletal sites was recorded.
Results
PET/CT indicated metastases in 16 (28 %) of 58 patients. In five (9 %) patients, the scans suggested bone metastases, and in 11 (19 %) patients, the scans suggested regional lymph node metastases only. For patients with PSA levels <1.0 ng/mL, the PET/CT scans indicated metastatic recurrence in 25 %.
Conclusions
18F-choline PET/CT may be valuable for selecting patients with BCR following RP for SRT or experimental treatment of oligometastases, even at low PSA values.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy (RP) is one of the cornerstones in curative treatment of prostate cancer [1], significantly reducing cancer-specific mortality compared to watchful waiting [2]. Still, a large proportion of patients, up to 60 % depending on tumour characteristics [3, 4], will develop biochemical recurrence (BCR) and may need additional treatment. BCR is usually treated with either radiotherapy (RT) or hormonal therapy (HT), depending on the likelihood that the recurrence is local only [5]. Salvage RT, which is the curative option, is associated with significant risk of morbidity [6] and should therefore only be given when there is a reasonable chance for cure. A high prostate-specific antigen (PSA) value, short time to relapse, short PSA doubling time, Gleason score 8–10 and lymph node metastases at lymphadenectomy are associated with increased risk of metastatic recurrence and reduced chance of complete remission after salvage therapy [7, 8]. In particular, PSA >2.0 ng/mL has been associated with a low probability of complete remission [8–10]. However, even in the group of patients with PSA <2.0 ng/mL, some have metastatic disease and require systemic therapy, rather than local RT.
18F-choline positron emission tomography combined with computed tomography (PET/CT) has been studied as a modality for detecting regional and distant metastases in patients with newly detected prostate cancer, but the role of PET/CT in restaging after post-surgical recurrence is still uncertain [11, 12]. Few previous studies have reported specifically on patients with low PSA values, i.e. when the choice of secondary treatment usually has to be made [13–18]. Most of the studies included a large proportion of patients on HT, for whom the association between PSA values and tumour burden is different than for hormone-naïve patients and for whom treatment with additional RT is not evidence based. The primary aim of this study was to determine how large a proportion of hormone-naïve patients with BCR after RP would have positive 18F-choline PET/CT findings at PSA values <2 ng/mL.
Materials and methods
Patients
Between June 2008 and November 2012, urologists in the southern health-care region of Sweden were invited to refer patients with BCR after RP for a whole-torso 18F-choline PET/CT scan according to a specific protocol. The inclusion criteria were as follows: a rising PSA ≥0.2 ng/mL below 2 ng/mL, eligibility for salvage RT and either Gleason score ≥7 at prostatectomy or a PSA doubling time ≤6 months. Patients with ongoing or previous androgen deprivation therapy or anti-androgens were excluded. Enrolment was prospective according to the protocol, but the acquisition of the outcome data was performed retrospectively at the end of the study. The study aimed at including 50 patients. It was approved by the Research Ethical Review Board at the University of Lund (EPN Dnr 552/2007).
Imaging
18F-choline was synthesized according to the method described by Kryza et al. [19] using the TracerLab MXFDG module (GE Healthcare, Stockholm, Sweden). PET/CT images were obtained using an integrated PET/CT system (Philips Gemini TF, Philips Medical Systems, Ohio, USA) at the Center for Medical Imaging and Physiology, Skåne University Hospital, in Malmö and Lund. All patients were fasting for 4 h before tracer injection. Whole-torso PET was performed 1–1½ after intravenous injection of 4 MBq/kg of 18F-choline, using 2 min per bed position. A CT scan was performed immediately prior to the PET scan with a multi-detector CT scanner using 5 mm reconstructed slice thickness; 1000 mL oral contrast (Omnipaque, GE Healthcare, Stockholm, Sweden) was given 1 h before the scan. The CT scan was performed in three phases: the liver was scanned without contrast, the thorax was scanned with intravenous contrast in arterial phase during breath-holding, and then, a femur to skull base scan was obtained in portal contrast phase during normal breathing [20].
All PET/CT scans were interpreted by a nuclear medicine physician as well as by a radiologist. Focal tracer uptakes in regional or retroperitoneal lymph nodes, or in skeletal sites without evidence of degenerative causes or fractures, were considered positive findings. Focal uptake in the prostatic bed was noted, but was not included in further analyses.
Statistics
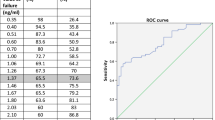
Statistical analysis was performed using SPSS Statistics 22 (IBM, Chicago, Ill, USA). PSA levels at the time of PET/CT, PSA doubling time, PSA nadir after RP and time to BCR were categorized according to Table 1. PSA doubling time was calculated by the log/slope method [21], using all available PSA levels after prostatectomy.
Results
A total of 58 patients were included. The clinical characteristics of all the patients are presented in Table 1. The PET/CT scans indicated metastases in 16 patients (28 %): regional lymph node metastases in 11 (19 %) and distant metastases in 5 (9 %). At PSA cut-off levels of 1.5, 1.0 and 0.5 ng/mL, metastatic recurrence was indicated in 26, 25 and 24 %, respectively. Local PET tracer uptake in the prostatic bed was noted in four patients (7 %), none of which had evidence of metastases.
Discussion
We investigated the utility of 18F-fluorocholine PET/CT in men with BCR after RP and PSA values in the low range (<2 ng/mL), when the decision whether to add salvage RT usually has to be made. The PET/CT scans suggested metastatic recurrence in 28 % of the patients, who were selected by having either Gleason score ≥7 cancers or a PSA doubling time shorter than 6 months. In the patients with PSA <1.5 ng/mL, 26 % of the scans suggested metastases, and for patients with PSA <1.0 ng/mL, the corresponding figure was 25 %.
There are only few other reports on PET/CT in patients with untreated BCR after RP and PSA <2.0 ng/mL. Castellucci et al. [15] reported 11C-choline PET/CT scans indicating metastases in 23 % of 605 patients with PSA <2 ng/mL and in 18 % of 291 patients with PSA <1.0 ng/mL. This is slightly less than in our study, but almost 25 % of the patients in their study received HT at the time of the PET/CT investigation, which is known to affect the sensitivity of choline PET/CT [22]. Also, their study population included more patients with Gleason score 5–6, with a lower likelihood of metastatic recurrence [7]. From a similar study, Giovacchini et al. [14] reported 29 % positive PET/CT scans in 358 patients with PSA <2 ng/mL, but 43 % of the patients received androgen deprivation therapy and it is unclear how many of the positive findings were metastases and how many were local recurrences. These results are in contrast to those from a study including patients with very low PSA levels only (≤0.76 ng/mL); PET/CT scans indicated metastases in only 1 of 22 patients [13]. However, taken together, these studies suggest that a significant proportion of patients with BCR after RP and PSA levels <2.0 ng/mL have metastatic recurrence, rather than local recurrence only. However, a limitation in our study, as well as in the others, is the lack of histopathological verification of the suspected metastases. Tilki et al. [23] reported a positive predictive value of only 50 % for choline PET/CT compared to a secondary lymphadenectomy following BCR after RP and PSA <2.0 ng/mL. However, their study included only 12 patients. In contrast, Jilg et al. [24] found a positive predictive value of 89 % in a similar study, but with much more heterogeneous clinical characteristics. Further validation is therefore required before choline PET/CT should be recommended outside clinical trials in the setting of BCR.
PET tracer uptake suggesting local recurrence was noted in only four patients. However, since all patients were planned to receive salvage RT if the scan did not reveal convincing evidence of metastases, we do not consider the absence or presence of uptake in the prostatic fossa as clinically relevant.
The most common purpose of using PET/CT for patients with BCR is to exclude those with metastases from local salvage RT. However, it is possible that aggressive treatment of oligo-metastatic disease, as determined by PET/CT, could lead to improved survival. Suardi et al. [25] recently reported 59 % complete biochemical response and 17 % recurrence-free 5-year survival following salvage lymphadenectomy in patients with nodal metastases only on choline PET/CT. Schick et al. [26] reported similar results of RT targeted against oligometastases for BCR after RP or RT. Further prospective, randomized trials in this setting could possibly lead to an improved management of patients with BCR.
Conclusions
In this study of hormone-naïve patients with BCR after RP, 18F-choline PET/CT scans indicated metastatic recurrence in 28 % of patients with PSA <2 ng/mL and in 25 % of patients with PSA <1 ng/mL. These results suggest that 18F-choline PET/CT may be valuable in selecting patients for local salvage RT or experimental treatment of regional oligometastases.
References
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T et al (2014) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol 65(1):124–137
Bill-Axelson A, Holmberg L, Garmo H, Rider JR, Taari K, Busch C et al (2014) Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med 370(10):932–942
Han M, Partin AW, Zahurak M, Piantadosi S, Epstein JI, Walsh PC (2003) Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol 169(2):517–523
Sooriakumaran P, Haendler L, Nyberg T, Gronberg H, Nilsson A, Carlsson S et al (2012) Biochemical recurrence after robot-assisted radical prostatectomy in a European single-centre cohort with a minimum follow-up time of 5 years. Eur Urol 62(5):768–774
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T et al (2014) EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 65(2):467–479
Bolla M, van Poppel H, Collette L, van Cangh P, Vekemans K, Da Pozzo L et al (2005) Postoperative radiotherapy after radical prostatectomy: a randomised controlled trial (EORTC trial 22911). Lancet 366(9485):572–578
Slovin SF, Wilton AS, Heller G, Scher HI (2005) Time to detectable metastatic disease in patients with rising prostate-specific antigen values following surgery or radiation therapy. Clin Cancer Res 11(24 Pt 1):8669–8673
Stephenson AJ, Scardino PT, Kattan MW, Pisansky TM, Slawin KM, Klein EA et al (2007) Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol 25(15):2035–2041
King CR (2012) The timing of salvage radiotherapy after radical prostatectomy: a systematic review. Int J Radiat Oncol Biol Phys 84(1):104–111
Pfister D, Bolla M, Briganti A, Carroll P, Cozzarini C, Joniau S et al (2014) Early salvage radiotherapy following radical prostatectomy. Eur Urol 65(6):1034–1043
Kjölhede H, Ahlgren G, Almquist H, Liedberg F, Lyttkens K, Ohlsson T et al (2014) 18F-fluorocholine PET/CT compared with extended pelvic lymph node dissection in high-risk prostate cancer. World J Urol 32(4):965–970
Evangelista L, Guttilla A, Zattoni F, Muzzio PC, Zattoni F (2013) Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate-to high-risk prostate cancer: a systematic literature review and meta-analysis. Eur Urol 63(6):1040–1048
Vees H, Buchegger F, Albrecht S, Khan H, Husarik D, Zaidi H et al (2007) 18F-choline and/or 11C-acetate positron emission tomography: detection of residual or progressive subclinical disease at very low prostate-specific antigen values (<1 ng/mL) after radical prostatectomy. BJU Int 99(6):1415–1420
Giovacchini G, Picchio M, Coradeschi E, Bettinardi V, Gianolli L, Scattoni V et al (2010) Predictive factors of [(11)C]choline PET/CT in patients with biochemical failure after radical prostatectomy. Eur J Nucl Med Mol Imaging 37(2):301–309
Castellucci P, Ceci F, Graziani T, Schiavina R, Brunocilla E, Mazzarotto R et al (2014) Early biochemical relapse after radical prostatectomy: which prostate cancer patients may benefit from a restaging 11C-choline PET/CT scan before salvage radiation therapy? J Nucl Med 55(9):1424–1429
Krause BJ, Souvatzoglou M, Tuncel M, Herrmann K, Buck AK, Praus C et al (2008) The detection rate of [11C]choline-PET/CT depends on the serum PSA-value in patients with biochemical recurrence of prostate cancer. Eur J Nucl Med Mol Imaging 35(1):18–23
Rinnab L, Mottaghy FM, Blumstein NM, Reske SN, Hautmann RE, Hohl K et al (2007) Evaluation of [11C]-choline positron-emission/computed tomography in patients with increasing prostate-specific antigen levels after primary treatment for prostate cancer. BJU Int 100(4):786–793
Scattoni V, Picchio M, Suardi N, Messa C, Freschi M, Roscigno M et al (2007) Detection of lymph-node metastases with integrated [11C]choline PET/CT in patients with PSA failure after radical retropubic prostatectomy: results confirmed by open pelvic-retroperitoneal lymphadenectomy. Eur Urol 52(2):423–429
Kryza D, Tadino V, Filannino MA, Villeret G, Lemoucheux L (2008) Fully automated [18F]fluorocholine synthesis in the TracerLab MX FDG Coincidence synthesizer. Nucl Med Biol 35(2):255–260
Kjölhede H, Ahlgren G, Almquist H, Liedberg F, Lyttkens K, Ohlsson T et al (2012) Combined 18F-fluorocholine and 18F-fluoride positron emission tomography/computed tomography imaging for staging of high-risk prostate cancer. BJU Int 110(10):1501–1506
Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC (1999) Natural history of progression after PSA elevation following radical prostatectomy. JAMA 281(17):1591–1597
Beheshti M, Haim S, Zakavi R, Steinmair M, Waldenberger P, Kunit T et al (2013) Impact of 18F-choline PET/CT in prostate cancer patients with biochemical recurrence: influence of androgen deprivation therapy and correlation with PSA kinetics. J Nucl Med 54(6):833–840
Tilki D, Reich O, Graser A, Hacker M, Silchinger J, Becker AJ et al (2013) 18F-fluoroethylcholine PET/CT identifies lymph node metastasis in patients with prostate-specific antigen failure after radical prostatectomy but underestimates its extent. Eur Urol 63(5):792–796
Jilg CA, Schultze-Seemann W, Drendel V, Vach W, Wieser G, Krauss T et al (2014) Detection of lymph node metastasis in patients with nodal prostate cancer relapse using (18)f/(11)c-choline positron emission tomography/computerized tomography. J Urol 192(1):103–111
Suardi N, Gandaglia G, Gallina A, Di Trapani E, Scattoni V, Vizziello D et al (2014) Long-term outcomes of salvage lymph node dissection for clinically recurrent prostate cancer: results of a single-institution series with a minimum follow-up of 5 years. Eur Urol. doi:10.1016/j.eururo.2014.02.011
Schick U, Jorcano S, Nouet P, Rouzaud M, Vees H, Zilli T et al (2013) Androgen deprivation and high-dose radiotherapy for oligometastatic prostate cancer patients with less than five regional and/or distant metastases. Acta Oncol (Madr) 52(8):1622–1628
Acknowledgments
This study has been funded by The Swedish Cancer Society (2012/475), Cancerstiftelsen Kronoberg, Region Skånes FoU-enhet, FoU Kronoberg and Philips.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kjölhede, H., Ahlgren, G., Almquist, H. et al. 18F-choline PET/CT for early detection of metastases in biochemical recurrence following radical prostatectomy. World J Urol 33, 1749–1752 (2015). https://doi.org/10.1007/s00345-015-1547-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1547-y