Abstract
Introduction
Modern multidisciplinary cancer treatments aim at obtaining minimal influence on patients’ quality of life (QoL). The purpose of this study was to assess QoL and correlate it with dose–volume parameters of organ at risks (OARs) in patients who received adjuvant radiotherapy for endometrial and cervical cancers.
Materials and methods
We administered the EORTC QLQ-C30 and EN24 or CX24 questionnaires to 124 patients, 100 with endometrial cancer and 24 with cervical cancer treated with postoperative radiotherapy ± chemotherapy in regular follow-up. Bladder function, fecal incontinence or urgency and sexual functioning were investigated and correlated with dose–volume parameters of OAR by multiple linear regression analysis. This correlation was assessed by R 2 value.
Results
QoL was very high in the majority of patients (82.3 % of patients). Few patients referred urinary incontinence (3.2 %) or abdominal discomfort of high grade (4.0 %). We found a significant correlation between bladder V40, i.e., absolute percentage of bladder volume that received a dose of 40 Gy, and global health status (p < 0.05, R 2 = 0.17), urinary urgency (p < 0.05, R 2 = 0.24), urinary incontinence (p < 0.05, R 2 = 0.23) and dyspareunia (p < 0.05, R 2 = 0.04). We found also a correlation between global health status and mean dose to vagina (p < 0.05, R 2 = 0.17) and between maximum dose to lumbo-sacral plexus and abdominal pain (p < 0.05, R 2 = 0.07).
Conclusions
Women treated with surgery and adjuvant radiotherapy for endometrial and cervical cancers have good QoL with minimal limitations of daily activities. QoL was correlated with dose–volume parameters such as bladder V40, mean dose to vagina, maximum dose to trigone and LSP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometrial and cervical are the most common gynecologic malignancies among women in Western countries. Surgery, radiotherapy and chemotherapy are commonly used and highly effective treatment modalities; however, they can be associated with relevant adverse effects on physical comfort, body image, sexual function and quality of life (QoL). Assessment and measurement of cancer-related symptoms are a challenge because of complex interactions between multimodality treatments and symptoms [1].
A higher incidence of late sequelae is reported after postoperative radiation than after surgery alone, such as abdominal pain, sexual symptoms and bladder dysfunctions [2]. The use of multimodal treatment regimens is associated with a rise of incidence of late effects within the pelvis [3].
There is paucity of data on long-term treatment effects and the subsequent impact on QoL in gynecologic cancer patients, and no studies have assessed the weight of the treatment modalities in inducing worsening of QoL.
The purpose of this study is to assess QoL in endometrial and cervical cancer patients after surgery and adjuvant radiotherapy ± chemotherapy in relation to radiation dose–volume parameters of the organs at risk (OARs).
Materials and methods
We assessed QoL in 124 patients in regular follow-up for endometrial and cervical cancers and previously treated by a multidisciplinary approach including surgery and radiotherapy ± chemotherapy. The institutional review board approved the study.
Eligibility criteria were: previous radical hysterectomy Piver II or type B–C, according to Querleu and Morrow classification in case of laparoscopic surgery [4], no neo-adjuvant chemotherapy, no post-surgical residual disease, no postoperative major complications, indication to pelvic external beam radiotherapy, minimum follow-up of 3 years without disease relapse, performance status higher than 60 according to Karnofsky scale.
We report the patients’ characteristics and the treatment modalities in Table 1. All patients were treated with external beam radiotherapy (EBRT) with 3D conformal or intensity-modulated radiation therapy (IMRT) to 45 Gy (1.8 Gy/fx) on the pelvis and the upper half of vagina or 45 Gy (1.8 Gy/fx) on the pelvis and 50 Gy (2.0 Gy/fx) on the upper half of vagina in case of simultaneous integrated boost (SIB).
According to guidelines, we completed adjuvant treatment with vaginal pulsed dose rate brachytherapy (BRT) in 85 cases [5]. Clinical target volume (CTV) contours were based on the guidelines from the Radiation Therapy Oncology Group (RTOG) and the Gynecologic IMRT Consortium [6]. For BRT, we used the guidelines of the European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) [7]. In particular, we contoured bladder, trigone, vagina and rectum according to the RTOG atlas [8] and LSP according to the guideline proposed by Yi et al. [9]. In all treatment plans, dose constraints for all OARs were strictly respected. We report values of the main dose–volume parameters for EBRT and BRT in Table 2.
Acute genito-urinary and gastro-intestinal toxicity according to the RTOG scale are reported in Table 3 [10].
Forty-five out of 100 patients with endometrial cancer and all patients with cervical cancer were treated with cisplatin or carboplatin regimen-based chemotherapy concomitantly to radiotherapy.
Self-reported QoL was assessed using the questionnaires EORTC QLQ-C30 and QLQ-CX24 or QLQ-EN24. The EORTC QLQ-C30 (version 3.0) consists of 30 items measuring functioning (physical, role, emotional, social functioning and a global health scale) and symptoms. Global health status was evaluated with the item 30 of the EORTC QLQ-C30 in which patients had to assign a score from zero (low QoL) to seven (high QoL).
All patients completed also the EORTC QLQ-CX24 or QLQ-EN24 questionnaire specific for cervical and endometrial cancer patients. These disease-related questionnaires contain 24 items summarized in three scales: symptoms experience, body image and sexual/vaginal functioning.
To assess bladder and intestinal functions, we analyzed items related to urinary frequency, incontinence/urgency and fecal incontinence. We also analyzed items related to abdominal pain and sexual activity, in particular dyspareunia. For all these items, patients could assign a score from one (no problems) to four (problems that cause discomforts).
The QoL items were subsequently correlated with dose–volume parameters of OARs, and the possible relationships were analyzed by multiple regression analysis. A p value of <0.05 was considered as statistically significant. Multiple linear regression analysis was used to assess also the association between two or more independent variables and a single continuous dependent variable. The magnitude and the goodness of fit were assessed by adjusted R 2 value.
Results
Based on selection criteria, we enrolled 124 out of 145 consecutive patients in regular follow-up of 3.5–11.5 years (median 4.5 years) after surgery and adjuvant radiotherapy for endometrial and cervical cancers. At treatment time, median age was 67.4 years (range 29–86) and median BMI was 23.7 (range 19.8–27.3).
Compliance to questionnaires was 100 % except for questions about sexual/vaginal functioning that were answered by 85/124 patients (65.4 %).
We report the answers to the EORTC questionnaires items in Table 4. We did not observe any statistical correlations between QoL parameters and acute toxicities. We summarize the results of the correlation between QoL and dose–volume parameters in Table 5.
According to multiple linear regression analysis, bladder V40, i.e., the absolute percentage of bladder volume that received at least 40 Gy, was significantly associated with worsening of global health status (p < 0.001). Mean dose to the vagina was significantly associated with worsening of global health status (p = 0.03) with an adjusted R 2 value of 0.17 (Fig. 1).
Bladder V40 (p < 0.001) and mean dose to vagina (p = 0.02) were correlated with urinary urgency with an adjusted R 2 value of 0.24, meaning an increasing urinary urgency with increase in bladder V40 and mean dose to vagina (Fig. 2). Bladder V40 was correlated also with urinary incontinence (p < 0.001) with an adjusted R 2 value of 0.24, meaning that the parameter V40 can explain the worsening of 24 % of urinary incontinence variance (Fig. 3).
We did not find any statistical correlation between global health status, bladder discomforts and dose to the trigone.
No correlation was found between gastro-intestinal symptoms (fecal incontinence and urgency) and dose–volume parameters. Conversely, a significant correlation between maximum dose to LSP and abdominal pain (p = 0.008, R 2 = 0.07) was observed (Fig. 4).
We found a statistical correlation between dyspareunia and bladder V40 (p < 0.05) but not with vaginal radiation dose. Goodness of this fit is poor, being the adjusted R 2 value 0.04, meaning that this relationship is able to explain only of 4 % dyspareunia variance.
We did not find any statistical correlation of BRT doses to bladder or rectum with QoL in terms of gastro-intestinal or genito-urinary symptoms.
In this analysis, we did not find any significant difference in terms of QoL items and dose–volume parameters between patients with endometrial or cervical cancers, patients treated with EBRT or EBRT + BRT and also between patients treated with adjuvant radiotherapy alone or radiochemotherapy.
Discussion
Since treatment of the large majority of patients (80–95 %) with endometrial and cervical cancer is curative, it is important to pay attention on its impact of long-term QoL and on the interventions that could improve QoL itself. As a matter of fact, gynecologic cancer survivors commonly report late effects [11]. The level of health-related QoL should become a central element within therapeutic standards in clinical practice.
The relevance of the role of QoL in gynecologic cancer has increased after the publication of PORTEC-2 study. This study showed that patients treated by BRT had less morbidity and better QoL compared to those who received EBRT [12].
We decided to analyze a homogeneous group of endometrial and cervical cancer patients treated in our center, with similar multidisciplinary treatment approach. Interestingly, this analysis is one of the first analyzing the relationship between QoL and dosimetry values, in terms of dose–volume parameters, among gynecologic cancer survivors.
As stated by the PORTEC-2 study, QoL assessed in follow-up can be correlated with toxicity occurred during treatment [12]. In our experience, as reported in a previous literature study [13], patients showed a good tolerance profile, with no gastro-intestinal and genito-urinary acute toxicity grade 3 or 4 according to RTOG scale, but no correlation with QoL parameters assessed at later time during follow-up.
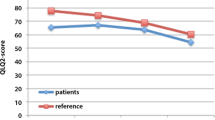
From EORTC QLQ-C30, it emerged an overall good profile of “global health.” It is likely that a recent cancer diagnosis, performance of surgery and cancer symptoms had negatively interfered with the perception of health before treatment. As a result, there was a significant improvement in QoL score for the question on general health status.
QoL of gynecologic cancer patients tends to be worst between time of diagnosis and completion of radiotherapy, but it can improve during follow-up [14]. We considered a minimum follow-up time of 3.5 years to avoid the potential confounding effect of immediate post-treatment phase.
In our study, a low rate of gastro-intestinal complications (only 4 % of grade 3–4 abdominal pain) was reported, while PORTEC-2 study showed an increase in abdominal pain even years after treatment. In the same way, the answers related to urinary symptoms pointed out no discomforts, while other studies reported an increased incidence of urinary incontinence and dysuria in particular in patients treated with radiotherapy for cervical cancer [1]. These results should be related not only to radiotherapy but also to surgery. Radical hysterectomy is characterized by pelvic anatomic dislocation of ureters and excision of tissues around vagina that could damage pelvic nerves with reduction in bladder continence. All patients of our series underwent similar surgical approaches, and we selected patients, as pointed out in “Materials and methods” section, with minimal surgical sequelae.
In our study, as well as in PORTEC-2, women were generally quite reluctant to answer questions on sexual activity. More than a half of patients (65.4 %) answering these questions declared to be sexually active. The most important symptom referred in our series was vaginal dryness with painful intercourse (dyspareunia) and tightening and/or shortening of the vagina, in particular in patients treated with adjuvant EBRT. Previous studies reported similar results: Vaz et al. [1] observed decreased sexual interest (29.7 %) with dyspareunia (45.9 %), and Jensen et al. [15] described vaginal dryness (35 %) and painful intercourse (55 %). In our study, we found dyspareunia in 5.9 % of sexually active patients, but probably this rate could be underestimated.
Sexual dysfunction from surgery is mainly caused by a shortened vagina [16], vaginal dryness [16, 17] and decreased libido [15, 17]. In contrast, sexual dysfunction from radiotherapy is caused by vaginal stenosis, which often yields dyspareunia, difficulty in orgasm, decrease in sexual satisfaction and changes in body image [17]. In the past, the results of studies concerning sexual function of the cervical cancer patients had shown that the RT group had worse sexual function than the surgery-alone group. In fact, according to Jensen et al. [15, 16], 63 % of the women who received RT and 91 % of those who received surgery had been sexually active. These historical data are similar to our findings.
An original aspect of our study is the correlation of specific items of QoL questionnaires with dose–volume parameters. We found a statistically significant correlation between increasing bladder V40 and declined self-reported QoL (item 30). Interestingly, a higher bladder V40 was also correlated with an increased urgency and incontinence. We considered patients with minor postoperative sequelae with the purpose to evaluate more selectively the role of adjuvant therapies, since several surgical studies showed how dissection of parametria and upper vagina could adversely affect autonomic innervations (S2–S4 levels) after radical hysterectomy [4].
A recent publication compared the low urinary tract dysfunctions between patients who received concurrent chemoradiation and those who received radical hysterectomy [18]. This study showed that storage dysfunction was significantly more prevalent after adjuvant radiotherapy than after radical hysterectomy alone. Despite the high incidence of long-term urinary symptoms, QoL was minimally affected, suggesting that these symptoms have mild severity and minimal impact in survivors. In our experience, bladder V40 was statistically correlated with worsening of global health status (p < 0.05), but this parameter alone can explain a relatively small proportion (17 %) of QoL changes.
In our study, we found that only 14.6 % of patients had bladder urgency after radiotherapy, while 3.1 % had urinary incontinence. Interestingly, increasing in bladder V40 explained 24 % of these storage symptoms. From our analysis, it emerged also a correlation between the mean dose to vagina and urinary incontinence. We could explain this fact considering that vagina is surrounded by pelvic nerves that control bladder function and can be damaged by high radiation doses.
From our analysis, it emerged that the increasing mean dose to vagina was correlated with worsening of global health status (p = 0.03). Probably, these data could be related to urinary incontinence: in fact, patients with higher mean doses to vagina present higher bladder discomfort that could cause deterioration in self-reported global health status.
Patients included in the present study referred only few rectal discomforts after radiotherapy. A previous controlled study suggested that bowel symptoms are more prevalent in long-term survivors [19]. We can underline that the large majority of our patients was treated with IMRT with strictly respected dose constraints and that the relatively low value of the average rectal volume (50.6 cc) would indicate an adequate bowel preparation [7]. These factors could have contributed to reduce the occurrence of late rectal symptoms.
Radiation-induced damage on LSP in gynecologic cancers is a quite rare complication of pelvic irradiation. The reported frequency ranges from 1.3 to 6.7 %, and the clinical course is associated with different degrees of bilateral lower limb pain, abdominal diffuse pain, numbness, weakness, paresis or paralysis, and rarely, urinary or fecal incontinence [20]. We found a statistically significant correlation between LSP maximum dose and abdominal pain without correlation with bladder or fecal symptoms. LSP maximum dose alone explained a small proportion of the variance in QoL with R 2 value of 0.07. We should point out that abdominal pain is an unspecific symptom and could relate to multiple factors including radiotherapy as observed in our experience.
Both radical surgery and postoperative radiotherapy can have medium- and long-term impact on sexual functioning among cervical cancer survivors as shown by other authors who found that patients who received radiotherapy had a significantly worse score in health-related QoL, psychosocial distress, menopausal symptoms and sexual functioning [21, 22]. In our study, we found that out of 85 patients answering questions related to sexual function 34.6 % was not sexually active. This value is similar to that reported in other series [23]. According to our analysis, only 5.9 % of sexually active patients referred deep dyspareunia. This value may contain an internal bias: in fact, women with sexual activity most likely have no or minimal vaginal discomforts (lack of vaginal elasticity and lack of lubrification) [24]. Similarly, we could not assess how many patients had sexual alterations in postoperative setting, because no patient was sexually active in the transition period between surgery and radiotherapy. In agreement with our findings, a recent study showed that patients after hysterectomy had persistent sexual dysfunctions [25].
Gondi et al. [22] observed no demonstrable association between dose–volume parameters and vaginal toxicity. In our study, the significant correlation between bladder V40 and dyspareunia explained a very small proportion of relation (R 2 = 0.04). We should underline that sexual QoL is related not only to treatments but also to psychological and more general health factors.
Although to the best of our knowledge, this study is the first that correlates QoL and radiation dose–volume parameters in gynecologic cancer long survivors, it has some limitations. QoL was not assessed before and after surgery, and this fact could bias the results observed during long-term follow-up by impairing to clearly distinguish dysfunctions related to each single treatment modality. Another limitation is the relatively low response rate (65.4 %) to sexual function questions with respect to participation in the overall study.
Conclusions
The present study shows that QoL of long-term survivors after surgery and postoperative radiotherapy for endometrial and cervical cancer has a quite favorable profile.
From our analysis, it emerges that parameters related to bladder function may be negatively affected by bladder V40 and mean dose to vagina. Moreover, sexual function can be worsened by bladder V40 and abdominal pain by maximum dose to LSP.
Based on the available literature data and the present study, radiation optimization should take more carefully into account patients’ QoL after long-term follow-up, and future prospective trials could further investigate the correlation between specific QoL items and dose–volume parameters in patients affected by gynecologic malignancies undergoing surgery and adjuvant radiotherapy.
References
Vaz AF, Conde DM, Costa-Paiva L, Morais SS, Esteves SB, Pinto-Neto AM. Quality of life and adverse events after radiotherapy in gynecologic cancer survivors: a cohort study. Arch Gynecol Obstet. 2011;284:1523–31.
Peters WA III, Liu PY, Barett RJ, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high risk early stage cancer of the cervix. J Clin Oncol. 2000;18:1606–13.
Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery vs radiotherapy for stage Ib–IIa cervical cancer. Lancet. 1997;350:535–40.
Querleu D, Morrow CP. Classification of radical hysterectomy. Gynecol Oncol. 2009;115:314–5.
NCCN clinical practice guidelines in Oncology: cervical cancer version 2.2015. http://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. NCCN clinical practice guidelines in Oncology: endometrial uterine neoplasms version 2.2015. http://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf.
Small W Jr, Mell LK, Anderson P, Creutzberg C, De Los Santos J, Gaffney D, et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy in postoperative treatment of endometrial and cervical cancer. Int J Radiat Oncol Biol Phys. 2008;71:428–34.
Pötter R, Haie-Meder C, Van Limbergen E, Barillot I, De Brabandere M, Dimopoulos J, et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. GEC ESTRO Working Group. Radiother Oncol. 2006;78:67–77.
Gay HA, Barthold HJ, O’Meara E, Bosch WR, El Naqa I, Al-Lozi R, et al. Pelvic normal tissue contouring guidelines for radiation therapy: a Radiation Therapy Oncology Group consensus panel atlas. Int J Radiat Oncol Biol Phys. 2012;83:353–62.
Yi SK, Mak W, Yang CC, Liu T, Cui J, Chen AM, et al. Development of a standardized method for contouring the lumbosacral plexus: a preliminary dosimetric analysis of this organ at risk among 15 patients treated with intensity-modulated radiotherapy for lower gastrointestinal cancers and the incidence of radiation-induced lumbosacral plexopathy. Int J Radiat Oncol Biol Phys. 2012;84:376–82.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31:1341–6.
Mirabeau-Beale KL, Viswanathan AN. Quality of life (QoL) in women treated for gynecologic malignancies with radiation therapy: a literature review of patient-reported outcomes. Gynecol Oncol. 2014;134:403–9.
Nout RA, Putter H, Jürgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, van der Steen-Banasik EM, et al. Quality of life after pelvic radiotherapy or vaginal brachytherapy for endometrial cancer: first results of the randomized PORTEC-2 trial. J Clin Oncol. 2009;27:3547–56.
Vaz AF, Pinto-Neto AM, Conde DM, Costa-Paiva L, Morais SS, Esteves SB. Quality of life and acute toxicity of radiotherapy in women with gynecologic cancer: a prospective longitudinal study. Arch Gynecol Obstet. 2008;278:215–23.
Fang P, Tan KS, Grover S, McFadien MK, Troxel AB, Lin L. Psychosocial encounters correlates with higher patient-reported functional quality of life in gynaecological cancer patients receiving radiotherapy. Radiat Oncol. 2015;10:34–41.
Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2003;56:937–49.
Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Early-stage cervical carcinoma, radical hysterectomy, and sexual function. A longitudinal study. Cancer. 2004;100:97–106.
Bukovic D, Strinic T, Habek M, Hojsak I, Silovski H, Krhen I, et al. Sexual life after cervical carcinoma. Coll Antropol. 2003;27:173–80.
Katepratoom C, Manchana T, Amornwichet N. Lower urinary tract dysfunction and quality of life in cervical cancer survivors after concurrent chemoradiation versus radical hysterectomy. Int Urogynecol J. 2014;25:91–6.
Lind H, Waldenström AC, Dunberger G, Al-Abany M, Alevronta E, Johansson KA, et al. Late symptoms in long-term gynaecological cancer survivors after radiation therapy: a population-based cohort study. Br J Cancer. 2011;105:737–45.
Dahele M, Davey P, Reingold S, Shun Wong C. Radiation-induced lumbo-sacral plexopathy (RILSP): an important enigma. Clin Oncol. 2006;18:427–8.
Frumovitz M, Sun CC, Schover LR, Munsell MF, Jhingran A, Wharton JT, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol. 2005;23:7428–36.
Gondi V, Bentzen SM, Sklenar KL, Dunn EF, Petereit DG, Tannehill SP, et al. Severe late toxicities following concomitant chemoradiotherapy compared to radiotherapy alone in cervical cancer: an inter-era analysis. Int J Radiat Oncol Biol Phys. 2012;84:973–82.
Rodrigues AC, Teixiera R, Teixeira T, Conde S, Soares P, Torgal I. Impact of pelvic radiotherapy on female sexuality. Arch Gynecol Obstet. 2012;285:505–14.
Stinesen Kollberg K, Waldenström AC, Bergmark K, Dunberger G, Rossander A, Wilderäng U, et al. Reduced vaginal elasticity, reduced lubrication, and deep and superficial dyspareunia in irradiated gynecological cancer survivors. Acta Oncol. 2015;54:772–9.
Froeding LP, Ottosen C, Rung-Hansen H, Svane D, Mosgaard BJ, Jensen PT. Sexual functioning and vaginal changes after radical vaginal trachelectomy in early stage cervical cancer patients: a longitudinal study. J Sex Med. 2014;11:595–604.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Pisani, C., Deantonio, L., Surico, D. et al. Quality of life in patients treated by adjuvant radiotherapy for endometrial and cervical cancers: correlation with dose–volume parameters. Clin Transl Oncol 18, 901–908 (2016). https://doi.org/10.1007/s12094-015-1458-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-015-1458-9