Abstract
Background and aims
Despite the association between sarcopenia and non-alcoholic fatty liver disease (NAFLD), no study has evaluated the predictive role of NAFLD in sarcopenia. We investigated impact of NAFLD on the risk of low muscle mass (LMM) and low muscle strength (LMS) in a nationwide multicenter study.
Methods
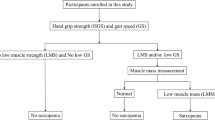
A total of 1595 community-dwelling people aged 70–84 years were followed for 2 years in the Korean Frailty and Aging Cohort Study. Muscle mass was estimated by dividing appendicular skeletal muscle mass (ASM) by body mass index (BMI). Muscle strength was measured as handgrip strength (HGS) divided by BMI. The sex-specific lowest quintiles of ASM/BMI and HGS/BMI of the study population were used as cutoffs for LMM and LMS, respectively. The risk of LMM and LMS were assessed according to hepatic steatosis index (HSI) and fatty liver index (FLI) quartiles.
Results
As HSI quartiles increased, the LMM risk increased gradually, after adjusting for age, sex, lifestyle factors, comorbidities, and several causative factors (insulin resistance, inflammation, and vitamin D) (Q4 vs. Q1 OR [95% CI] 3.46 [2.23–5.35]). The increased risk of LMS was even higher according to HSI quartiles (Q4 vs. Q1 5.81 [3.67–9.21]). Multivariate analyses based on FLI showed similar results. People with NAFLD (HSI > 36) were at higher risk of developing LMM and LMS compared to those without (1.65 [1.19–2.31] and 2.29 [1.61–3.26], respectively).
Conclusions
The presence of NAFLD may predict future risk of LMM and LMS, with greater impact on LMS than on LMM.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is characterized by the accumulation of excess fat in the liver in the absence of excessive alcohol consumption. NAFLD has become a predominant cause of chronic liver disease worldwide. The rapidly rising prevalence of NAFLD is accompanied by increased rates of obesity and the growing population of older adults [1]. In addition, sarcopenia, the progressive loss of skeletal muscle mass and strength, has also emerged as a global health problem owing to the aging of the world’s population [2]. Sarcopenia and obesity synergistically increase the risk of developing a series of adverse health issues, including physical disability, cardiometabolic diseases, and mortality [3, 4].
Several cross-sectional studies, including our previous study, demonstrated an independent association between low muscle mass (LMM) and NAFLD [5,6,7]. The relationship between LMM and incident NAFLD was supported by the results of subsequent longitudinal studies using retrospective health examination data [7, 8]. Recently, the concept of sarcopenia and the key factors used in determining sarcopenia have been modified to facilitate its early detection in practice [9]. Low muscle strength (LMS) was adopted as a principal determinant of sarcopenia because muscle strength is more important than muscle mass in predicting adverse outcomes [10]. Recent cross-sectional studies reported an independent association between LMS and NAFLD [11,12,13]. Aging, diet, physical inactivity, hormonal change, insulin resistance, inflammation, and vitamin D deficiency have been described as common underlying mechanisms linking sarcopenia and NAFLD [14, 15]. Although a vicious cycle between NAFLD and sarcopenia has been suggested, no previous study has assessed the influence of NAFLD on the risk of LMM and LMS.
Therefore, we investigated the contribution of NAFLD to the development of LMM and LMS after extensive adjustment for various confounding factors in elderly adults using 2-year follow-up data from the Korean Frailty and Aging Cohort Study (KFACS), a nationwide multicenter longitudinal cohort study. We also assessed the interactions of insulin resistance, inflammation, and vitamin D status, which are critical risk factors for both diseases, in the association between sarcopenia and NAFLD. Finally, we conducted sensitivity analyses to exclude the effects of confounding disorders such as diabetes, heavy alcohol consumption, viral hepatitis, and impaired liver function tests.
Methods and materials
Data source and study population
This study used data from the KFACS, which is dedicated to frailty and sarcopenia. The baseline survey was conducted from May 2016 to November 2017. The participants were recruited from among community-dwelling residents aged 70–84 years from ten different medical centers nationwide using quota sampling methods stratified by age and sex [16]. Of the 3014 participants, 1559 (51.7%) and 1455 (48.3%) participated in the study in 2016 ∙and 2017, respectively, during the 2-year enrollment period. The prospective cohort design of the KFACS included data collection and follow-up surveys on a 2-year basis. The database includes face-to-face interviews, health examinations and laboratory measurements (details in Supplementary Methods).
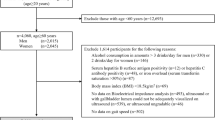
For this study, body composition data from two community health centers that used bioelectrical impedance analysis instead of dual-energy X-ray absorptiometry (DXA) measurements were excluded (n = 604) because of the systematic bias in appendicular lean mass between two measurements. Subjects lost to follow-up after the first visit (n = 128); those with missing data on baseline hepatic steatosis index (HSI), appendicular skeletal muscle mass (ASM), and handgrip strength (HGS, n = 9) measurements; those with missing data on follow-up ASM and HGS (n = 280); and those with sex-specific lowest quintiles of ASM/BMI or HGS/BMI (n = 398) were excluded (Fig. 1). Thus, this study included a total of 1595 participants.
Measurement of skeletal muscle mass and muscle strength
Body composition was measured using DXA (Lunar [GE Healthcare, Madison, WI, USA] and Hologic [Hologic Inc., Bedford, MA, USA]) instruments. ASM, the sum of the muscle masses of the four limbs, was measured by excluding the bone mass from the lean mass of the extremities using DXA. For the muscle mass index, we used the ASM adjusted for BMI and ASM/BMI, as previously described by the foundation for the National Institutes of Health (FNIH) sarcopenia project [17]. The muscle strength index was calculated from the HGS of the dominant arm adjusted for BMI, namely HGS/BMI, which was also introduced in FNIH sarcopenia project [17]. Using a digital hand grip dynamometer (Takei TKK 5401; Takei Scientific Instruments Co. Ltd., Tokyo, Japan), HGS was measured twice for each hand, with the highest value used for the analysis. We used the sex-specific lowest quintiles of ASM/BMI and HGS/BMI of the study population as cutoffs of defining LMM and LMS, respectively [18]. The cutoff points for LMM were 0.678 for men and 0.468 for women, while those for LMS were 1.246 for men and 0.768 for women.
Assessment of NAFLD
NAFLD was defined using HSI, a previously validated fatty liver prediction model [19]. The equation for HSI includes measurements of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels, BMI, and information on sex and diabetes as follows: \({\text{HSI}} = { 8 } \times \left( {\text{ALT/AST ratio}} \right) + {\text{ BMI }}\left( { + {\text{2, if female; }} + {\text{2, if diabetes mellitus}}} \right)\). HSI value > 36 indicates hepatic steatosis (specificity 92.4%) and HSI < 30 indicates no hepatic steatosis (sensitivity 93.1%) [19]. We also used the fatty liver index (FLI) as a surrogate marker of NAFLD. The FLI uses an algorithm based on BMI, WC, serum triglycerides (TG) and γ-glutamyl transferase (GGT) levels as follows: FLI = \(\frac{e^{x}}{1 + e^{x}}\) × 100 where x = 0.953 × log(TG) + 0.139 × BMI + 0.718 × log(GGT) + 0.053 × WC – 15.745. FLI value ≥ 60 indicated hepatic steatosis (specificity 86%), while FLI < 30 ruled out hepatic steatosis (sensitivity 87%) [20]. Since the indices of muscle mass and muscle strength are adjusted for BMI, we used NAFLD liver fat score (NLFS) that does not include BMI in its formula as follows: \(1.18 \, \times {\text{ metabolic syndrome }} + \, 0.45 \, \times {\text{ type}} \, 2{\text{ diabetes }} \left( {2, {\text{ if yes}}; \, 0, {\text{ if no}}} \right) \, + \, 0.15 \, \times {\text{ fasting insulin }} + \, 0.04 \, \times {\text{ AST }} - \, 0.94 \, \times \, \left( {{\text{AST}}/{\text{ALT}}} \right) \, - 2.89\)\(.\) A NLFS value above − 0.640 predicted the presence of steatosis with 86% sensitivity and 71% specificity [21].
Advanced liver fibrosis was assessed using the BARD score, the sum of the following scores (BMI ≥ 28 = 1 point; AST/ALT ratio ≥ 0.8 = 2 points; type 2 diabetes = 1 point). Advanced fibrosis was defined as BARD score of 2–4 with a negative predictive value of 96% [22].
Statistical analysis
Categorical variables are presented as n (%), while continuous variables are expressed as means ± standard deviation or medians (interquartile range [IQR]). The baseline characteristics of the study subjects were analyzed according to the HSI quartiles using Kruskal–Wallis and chi-squared (χ2) tests for continuous and categorical variables, respectively. The characteristics of the study subjects according to the presence of LMM or LMS after the 2-year follow-up were analyzed using Mann–Whitney U test for continuous variables and χ2 tests for categorical variables. Multivariable logistic regression analysis was performed to determine the independent association between baseline NAFLD indices and the incidence of LMM and LMS after adjusting for age and sex in model 1; smoking, alcohol, physical activity, and household income in model 2; hypertension, dyslipidemia, and chronic kidney disease in model 3; and HOMA-IR, high sensitivity C-reactive protein (hs-CRP), and vitamin D levels in model 4. The odds ratios (ORs) and 95% confidence intervals (CIs) for LMM and LMS according to HSI, FLI, and NFLS cutoff values for predicting NAFLD were calculated using logistic regression. Sensitivity analyses were conducted to exclude the effects of excessive alcohol consumption (> 140 g/week for men and > 70 g/week for women), viral hepatitis, and impaired liver function tests (AST, ALT, and bilirubin levels > 2 times the upper limit of each normal). To determine the impact of HSI quartiles on the risk of incident LMM and LMS not related to diabetes, another sensitivity analysis was performed after excluding subjects with diabetes at baseline and those who developed diabetes during follow-up. To verify whether NAFLD (defined as HSI > 36) had an independent effect on the incidence of LMM, LMS, and sarcopenia, multivariate logistic regression analyses were performed with the same adjustment in models 1, 2, 3, and 4. All tests were two-sided, and p < 005 was considered statistically significant. Statistical analyses were performed by an experienced professional statistician using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics of study population
This study included a total of 1595 participants. The median age of the study population was 75 years (IQR 72–78 years) and 47.6% of the participants were men. The baseline characteristics of the study population according to HSI quartiles are shown in Table 1. As HSI quartiles increased, the proportion of females, BMI, WC, SBP, DBP, ALT, GGT, TG, FPG, HOMA-IR, the proportion of never smokers, low physical activity, hypertension, dyslipidemia, and diabetic cases increased significantly. After the 2-year follow-up, 318 (19.9%) of 1,595 participants developed LMM or LMS (Supplementary Table 1). Participants with LMM had higher BMI, WC, GGT, HOMA-IR, TG, and hs-CRP levels and a higher proportion of hypertension and diabetes compared to those in participants without LMM. Subjects with LMS showed clinical features similar to those in subjects without LMS.
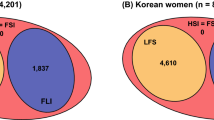
The risk of LMM and LMS according to HSI, FLI, and NLFS quartiles
When the study population was stratified by HSI quartiles and quintiles of ASM/BMI and HGS/BMI, HSI quartiles showed a significant positive association with ASM/BMI and HGS/BMI quintiles in both men and women (all p < 0.001; Fig. 2). A similar positive correlation was also found between FLI quartiles and ASM/BMI and HGS/BMI quintiles in both sexes (all p < 0.001) (Supplementary Fig. 1). The risks of LMM and LMS were then analyzed according to quartiles of baseline HSI. As HSI quartiles increased, the risks of LMM also increased showed stepwise (Table 2). In full-adjusted model, the risk of LMM was significantly elevated in participants with HSI Q4 compared to those with HSI Q1 (OR 3.46 [95% CI 2.23–5.35]). Furthermore, the risk of LMS increased stepwise as HSI quartiles increased (Table 2). Participants with HSI Q4 showed a significantly higher risk of LMS after full adjustments compared to the risk in participants with HSI Q1 (5.81 [3.67–9.21]). Although the risk of LMM did not increase gradually with the increase in FLI quartile, participants with FLI Q4 showed the highest risk of LMM relative to those with FLI Q1 (2.91 [1.94–4.36]) (Supplementary Table 2). In contrast, the risk of LMS gradually increased as FLI quartiles increased. The risk of LMS was significantly elevated in participants with FLI Q4 compared to those with FLI Q1 (4.86 [3.12–7.55]). Likewise, as NLFS quartiles increased, the risk of LMM and LMS gradually increased (In model 4, Q4 vs. Q1 1.81 [1.15–2.85] for LMM and 3.13 [1.90–5.16] for LMS).
The risk of LMM and LMS according to the presence of NAFLD
Next, we compared the risk of LMM and LMS according to the baseline existence of NAFLD defined by HSI > 36 (Table 3). Compared to participants without NAFLD (HSI ≤ 36), those with NAFLD (HSI > 36) had an increased risk of LMM (1.65 [1.19–2.31]) and LMS (2.29 [1.61–3.26]) in the fully adjusted model. Moreover, the risk of LMS from NAFLD was higher compared to the risk of LMM in the elderly Korean population. Then, we assessed the risk of LMM and LMS according to HSI, FLI, and NFLS cutoff values to predict NAFLD (Supplementary Table 4). When compared to the reference group of HSI < 30 (not having NAFLD), the ORs for LMM in individuals with the HSI 30 to ≤ 36 (intermediated HSI) and HSI > 36 (having NAFLD) were 2.09 [1.47–2.95] and 3.03 [1.94–4.72], respectively. The ORs for LMS also increased in the participants with the HSI 30 to ≤ 36 and HSI > 36 (2.85 [1.98–4.10] and 5.53 [3.43–8.92], respectively), compared to the reference group of HSI < 30. Similarly, comparing FLI ≥ 60 (having NAFLD) and FLI 30 to < 30 (intermediate FLI) with FLI < 30 (not having NAFLD), the risk of LMM increased (1.29 [0.97–1.71] and 2.03 [1.32–3.13], respectively). The risk of LMS increased even more in participants with FLI ≥ 60 and FLI 30 to < 30 (2.21 [1.65–2.96] and 3.94 [2.45–6.33], respectively), compared to those with FLI < 30. Individuals with NLFS ≥ − 0.640 (having NAFLD) had increased risk of LMS (1.90 [1.35–2.68]) compared to those with NLFS < − 0.640 (not having NAFLD) in full adjusted model. The risk of LMM in individuals with NLFS ≥ − 0.640 was significantly increased in the unadjusted model, but attenuated after adjustment for several causative factors (model 3). In contrast, having advanced fibrosis (BARD ≥ 2) at baseline did not increase the risk of LMM or LMS after 2 years (Supplementary 5).
Sensitivity analyses
Sensitivity analyses were performed by excluding participants with heavy alcohol consumption (Supplementary Table 6), hepatitis B and C (Supplementary Table 7), impaired liver function tests (Supplementary Table 8), and diabetes at baseline and those who developed diabetes during follow-up (Supplementary Table 9) and produced consistent results.
Discussion
In this nationwide longitudinal study, baseline hepatic steatosis was significantly associated with the future risk of sarcopenia in community-dwelling older individuals, independent of age, sex, lifestyle factors, comorbidities, and risk factors such as HOMA-IR, hs-CRP levels, and vitamin D levels. Despite recent reports of the association between sarcopenia and NAFLD [4,5,6,7], whether NAFLD predicts future sarcopenia remains uncertain. Our multicenter prospective study including elderly adults provides the first evidence that NAFLD is an independent risk factor for the development of both LMM and LMS. The risks of LMM and LMS at 2 years of follow-up were linearly related to the HSI and FLI at baseline.
As muscle mass is correlated with body size, ASM has been used as the skeletal muscle mass index after adjusting for body size in different ways, including height2, weight, or BMI. The prevalence of sarcopenia and the risk of adverse health outcomes associated with sarcopenia can vary depending on the operational methods used to define LMM [3, 23]. Lim et al. reported a positive correlation between ASM/height2 and BMI, visceral fat area, and insulin resistance, whereas ASM/weight was negatively correlated with these metabolic risk parameters [24]. Our previous study findings supported that ASM/BMI-defined sarcopenia was more closely related to cardiometabolic risk factors than ASM/height2-defined sarcopenia [25]. Moreover, recent studies have reported a relationship between relative handgrip strength, defined as HGS/BMI, and cardiometabolic diseases [26]. Thus, in the present study, ASM/BMI and HGS/BMI were used as the muscle mass index and muscle strength index for comparison, respectively. Since ethnic- and sex-specific cutoffs, the lowest quintile for each parameter, predicted a higher risk of mortality than the FNIH-recommended values [18], we used sex-specific lowest quintiles of ASM/BMI or HGS/BMI of the study population for cutoffs for defining LMM and LMS.
Cross-sectional studies have reported the association between low relative muscle mass and NAFLD [5, 6]. In the Korean Sarcopenic Obesity Study, the lowest quartile of weight-adjusted ASM was associated with a five-fold higher risk of NAFLD compared to that in the highest quartile after adjusting for potential confounding factors [5]. Lee et al. also showed an independent association between sarcopenia, defined using ASM/BMI cutoffs by the FNIH, and NAFLD after adjusting for confounding factors related to obesity or insulin resistance [6]. Furthermore, two longitudinal studies using retrospective health examination data reported the relationship between muscle mass and NAFLD [7, 8]. LMS has recently been emphasized as the principal determinant of sarcopenia as muscle strength is more important than muscle mass in predicting adverse health outcomes [10]. In 2018, the revised consensus on the definition and diagnosis of sarcopenia, European Working Group on Sarcopenia in Older People 2, reported that LMS is a key characteristic of sarcopenia that facilitates the prompt identification of this condition in practice [9]. Recent studies have also reported a significant association between muscle strength and NAFLD [11,12,13]. Meng et al. first reported that lower weight-adjusted HGS was associated with a higher prevalence of NAFLD after adjusting for confounding factors [11]. Recently, Kang et al. reported that the lowest quartile of HGS/BMI was independently associated with NAFLD (OR 1.66 [95% CI 1.28–2.16]) [12]. However, as these studies were all cross-sectional, causal relationships could not be inferred.
In the present study, we first evaluated the predictive role of NAFLD in the development of sarcopenia based on prospective KFACS data. The baseline HSI quartiles showed a stepwise relationship with the risk of LMM and LMS, respectively. Participants with the highest quartile of HSI showed an approximately 3.5-fold increased risk of LMM and an approximately 5.8-fold increased risk of LMS 2 years later. When FLI was used instead of HSI, the risk of LMM was increased by 2.9-fold and the risk of LMS by 4.9-fold in people with the highest quartile of FLI. Since the indices for muscle mass and muscle strength are adjusted for BMI, we used NLFS that does not include BMI in its formula. The risk of LMM and LMS was slightly lower but significantly increased in individuals with the highest quartile of NLFS compared to those with the lowest quartile, 1.8 times for LMM and 3.1 times for LMS. Consistently, individuals having NAFLD showed increased risk of LMM and LMS than those without NAFLD, when the risk of LMM and LMS was assessed according to HSI, FLI, and NFLS cutoff values for predicting NAFLD. These results demonstrated the increased influence of NAFLD on LMS than on LMM, which may signify greater functional implications and clinical consequences.
The reported mechanisms underlying the association between sarcopenia and NAFLD include insulin resistance, inflammation, and vitamin D deficiency [14, 15]. Skeletal muscle is the main organ involved in inulin-mediated glucose disposal; thus, it has an important effect on insulin sensitivity. Therefore, muscle aging decreases the body’s glucose metabolism capacity and promotes insulin resistance independently of obesity [27]. As insulin resistance plays a main pathogenic role in the development of sarcopenia, NAFLD may result in a loss of muscle mass or function via the aggravation of insulin resistance. In addition, emerging evidence has suggested a possible contributing role of low-grade systemic inflammation and vitamin D deficiency in both sarcopenia and NAFLD [14, 15]. In the present study, the association between NAFLD and LMM was partially attenuated but remained significant after adjusting for HOMA-IR, hs-CRP level, and vitamin D level. In contrast, the association between NAFLD and LMS was not affected by these factors. These findings suggest a complex interplay between the pathophysiological mechanisms of NAFLD and LMM and LMS. Several hepatokines have been suggested to be involved in muscle homeostasis through direct effects or the promotion of insulin resistance [28]. Circulating levels of fetuin A, a physiological inhibitor of the insulin receptor tyrosine kinase in skeletal muscles [29], are elevated in NAFLD. Hepassocin is also increased in NAFLD, and overexpression of hepassocin in mice induced insulin resistance in skeletal muscle [30]. The greater effect of NAFLD on LMS than on LMM was attenuated after excluding subjects with diabetes. Patients with diabetes likely have more severe forms of NAFLD in terms of histology [31] and, thus, more severe changes in the secretion of hepatokines to influence metabolic homeostasis through inter-organ communication [28]. Further studies are needed on the causative role of NAFLD in the development of LMM and LMS by the secretion of various hepatokines.
This study has several limitations. First, although liver biopsy is the gold standard method for diagnosing NAFLD, data from liver imaging and histological information were not available. Liver biopsy has the risk of procedure-related complications such as bleeding and is difficult to use in large epidemiological studies. Therefore, our study adopted well-validated prediction models for the detection of NAFLD [19,20,21]. Second, despite the extensive collection of detailed information on confounding factors by trained and qualified staff, there might have been residual confounding or bias. Third, because this study included only people from South Korea, the results may not be applicable to other ethnic populations. Finally, we did not have information on the use of medications that could cause fatty liver, including amiodarone, corticosteroids, tamoxifen, and tetracycline. The strengths of our study include its prospective design, nationwide multicenter sampling focusing on an elderly population, high follow-up rates, standardized high-quality clinical and laboratory measurements, and extensive adjustment for potential confounders. Our study identified the causative role of NAFLD in the development of LMM and LMS in a cohort study that recruited only the elderly population. Furthermore, we adjusted for a series of confounding risk factors that might influence the association between sarcopenia and NAFLD, such as HOMA-IR, hs-CRP level, and vitamin D level. Furthermore, we conducted sensitivity analyses to exclude the effects of diabetes, alcohol consumption, and viral hepatitis, the consistent results of which may support the robustness of our study findings.
In conclusion, the results of our study using data from a nationwide, multicenter cohort study demonstrated for the first time the longitudinal impact of NAFLD on the development of LMM and LMS in older adults. Further well-designed, prospective studies are needed to confirm these results in other populations and to elucidate the role of additional causal factors, such as hepatokines, linking NAFLD and sarcopenia.
Data availability
Access to anonymized data may be granted following review.
Abbreviations
- ALT:
-
Alanine aminotransferase
- ASM:
-
Appendicular skeletal muscle mass
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- DXA:
-
Dual-energy X-ray absorptiometry
- FLI:
-
Fatty liver index
- FNIH:
-
Foundation for the National Institutes of Health
- FPG:
-
Fasting plasma glucose
- GGT:
-
γ-Glutamyl transferase
- HbA1c:
-
Hemoglobin A1c
- HGS:
-
Handgrip strength
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- hs-CRP:
-
High-sensitivity C-reactive protein
- HIS:
-
Hepatic steatosis index
- KFACS:
-
Korean Frailty and Aging Cohort Study
- KNHANES:
-
Korean National Health and Nutrition Examination Survey
- LMM:
-
Low muscle mass
- LMS:
-
Low muscle strength
- NAFLD:
-
Nonalcoholic fatty liver disease
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- TG:
-
Triglycerides
- WC:
-
Waist circumference
References
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690
Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. 2017;16:21
Roh E, Choi KM. Health consequences of sarcopenic obesity: a narrative review. Front Endocrinol (Lausanne). 2020;11:332
Kim D, Wijarnpreecha K, Sandhu KK, Cholankeril G, Ahmed A. Sarcopenia in nonalcoholic fatty liver disease and all-cause and cause-specific mortality in the United States. Liver Int. 2021;41(8):1832–1840
Hong HC, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean Sarcopenic Obesity Study. Hepatology. 2014;59:1772–1778
Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008–2011). J Hepatol. 2015;63:486–493
Kim G, Lee SE, Lee YB, Jun JE, Ahn J, Bae JC, et al. Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: a 7-year longitudinal study. Hepatology. 2018;68:1755–1768
Lee MJ, Kim EH, Bae SJ, Kim GA, Park SW, Choe J, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver. 2019;13:67–76
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:601
Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A Jr, Orlandini A, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386:266–273
Meng G, Wu H, Fang L, Li C, Yu F, Zhang Q, et al. Relationship between grip strength and newly diagnosed nonalcoholic fatty liver disease in a large-scale adult population. Sci Rep. 2016;6:33255
Kang S, Moon MK, Kim W, Koo BK. Association between muscle strength and advanced fibrosis in non-alcoholic fatty liver disease: a Korean nationwide survey. J Cachexia Sarcopenia Muscle. 2020;11:1232–1241
Gan D, Wang L, Jia M, Ru Y, Ma Y, Zheng W, et al. Low muscle mass and low muscle strength associate with nonalcoholic fatty liver disease. Clin Nutr. 2020;39:1124–1130
Tilg H, Moschen AR. Insulin resistance, inflammation, and non-alcoholic fatty liver disease. Trends Endocrinol Metab. 2008;19:371–379
Kim JA, Choi KM. Sarcopenia and fatty liver disease. Hepatol Int. 2019;13:674–687
Won CW, Lee S, Kim J, Chon D, Kim S, Kim C-O, et al. Korean frailty and aging cohort study (KFACS): cohort profile. BMJ Open. 2020;10:e035573
McLean RR, Shardell MD, Alley DE, Cawthon PM, Fragala MS, Harris TB, et al. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. J Gerontol A Biol Sci Med Sci. 2014;69:576–583
Moon JH, Kim KM, Kim JH, Moon JH, Choi SH, Lim S, et al. Predictive values of the new sarcopenia index by the Foundation for the National Institutes of Health Sarcopenia Project for mortality among older Korean adults. PLoS ONE. 2016;11:e0166344
Lee J-H, Kim D, Kim HJ, Lee C-H, Yang JI, Kim W, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42:503–508
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33
Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, Johansson LM, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–872
Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008;57:1441–1447
Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med. 2016;31:643–650
Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care. 2010;33:1652–1654
Kim TN, Park MS, Lee EJ, Chung HS, Yoo HJ, Kang HJ, et al. Comparisons of three different methods for defining sarcopenia: an aspect of cardiometabolic risk. Sci Rep. 2017;7:6491
Li D, Guo G, Xia L, Yang X, Zhang B, Liu F, et al. Relative handgrip strength is inversely associated with metabolic profile and metabolic disease in the general population in China. Front Physiol. 2018;9:59
Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS ONE. 2010;5:10805
Meex RCR, Watt MJ. Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance. Nat Rev Endocrinol. 2017;13:509–520
Mathews ST, Chellam N, Srinivas PR, Cintron VJ, Leon MA, Goustin AS, et al. Alpha2-HSG, a specific inhibitor of insulin receptor autophosphorylation, interacts with the insulin receptor. Mol Cell Endocrinol. 2000;164:87–98
Wu H-T, Ou H-Y, Hung H-C, Su Y-C, Lu F-H, Wu J-S, et al. A novel hepatokine, HFREP1, plays a crucial role in the development of insulin resistance and type 2 diabetes. Diabetologia. 2016;59:1732–1742
Valenti L, Bugianesi E, Pajvani U, Targher G. Nonalcoholic fatty liver disease: cause or consequence of type 2 diabetes? Liver Int. 2016;36:1563–1579
Acknowledgements
This study was supported by grant from the Korea Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI) funded by the Ministry of Health and Welfare of Korea (grant number: HI15C3153) and grant from the National Research Foundation of Korea (NRF) funded by the Ministry of Education of Korea (grant number: 2020R1I1A1A01070499) This work was also supported by Korea University Guro Hospital (Korea Research-Driven Hospital) and grant funded by Korea University Medicine (K2115701).
Author information
Authors and Affiliations
Contributions
ER, SYH, CWW and KMC participated in the design of the study. ER, JL, SJS, HJK, YSP, SL, BLC, HCJ, BJK, CWW and KMC contributed to data collection and quality control. SYH performed the statistical analysis. ER, HJY, SHB, CWW and KMC contributed to analysis and interpretation of data. ER, CWW and KMC wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Eun Roh, Soon Young Hwang, Hye Jin Yoo, Sei Hyun Baik, Jin-Hee Lee, Sang Joon Son, Hyeon Ju Kim, Yong Soon Park, Sam-Gyu Lee, Be Long Cho, Hak Chul Jang, Bong Jo Kim, Miji Kim, Chang Won Won and Kyung Mook Choi have nothing to disclose.
Ethical approval
The study was performed according to the 1964 Declaration of Helsinki. The study protocol for the KFACS was approved by the Institutional Review Board of Korea University Guro Hospital (approval no. 2020GR0134).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Roh, E., Hwang, S.Y., Yoo, H.J. et al. Impact of non-alcoholic fatty liver disease on the risk of sarcopenia: a nationwide multicenter prospective study. Hepatol Int 16, 545–554 (2022). https://doi.org/10.1007/s12072-021-10258-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10258-8