Abstract
Background/purpose of the study
Worldwide and national efforts are directed against eradication of HCV. The introduction of direct-acting antivirals (DAAs) has changed dramatically the outcome of HCV treatment. In spite of the Food and Drug Administration approval of the oral drugs sofosbuvir (SOF) and ledipasvir (LED) for the treatment of HCV in adolescents more than or equal to 12 years old, sufficient real-world experience is still lacking. The aim of this study was to assess the safety and efficacy of the generic SOF/LED fixed-dose combination 400/90 (400 mg SOF + 90 mg LED) for the treatment of adolescents and children (9–12 years) with chronic hepatitis C (CHC).
Methods
In this prospective observational study, 100 cases of genotype 4 CHC were recruited consecutively from those fulfilling the inclusion and exclusion criteria. All cases received the generic fixed-dose combination SOF/LED (400/90), one tablet daily for 12 weeks. All clinical, laboratory, and virologic characteristics were evaluated at base line, and week (W) 2, 4, 8, and 12 of therapy and W12 post-treatment (SVR12).
Results
Recruited children (9–12) and adolescents weighed 28–83 and 31–90 kg, respectively. Eighty cases were naïve and 20 cases were pegylated interferon/ribavirin treatment-experienced. Very rapid virologic response (vRVR) at W2 was 96%, while at W4 response rate was 100% and maintained till the end of treatment and at W12 post-treatment (SVR12). All reported side effects were mild and did not lead to treatment termination and disappeared at W12 post-treatment.
Conclusion
The generic SOF/LED fixed-dose combination is safe and effective in children, 9–12 years, and adolescents with vRVR rate of 96%, 100% EOT response and SVR12.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) infection constitutes a significant burden on health worldwide with special concern in countries with high prevalence, like Egypt [1]. Although most of cases are adults, about 5 million children have active HCV infection worldwide [2]. Prevalence of HCV in Egyptian pediatric age was reported to be high ranging from 1.4 to 5.8% [3,4,5,6], in comparison to a lower prevalence in United States ranging from 0.2 to 0.4% [7, 8] and Middle East and North African countries; zero % in Iraq, 0.7–1.8% in Saudi Arabia, 1.7% in Pakistan, and 2.1% in Yemen [6].
Even though HCV causes in most of cases a mild disease throughout childhood, HCV-infected children often suffer stigmatization and discrimination in school and child-care settings because of inadequate public understanding of hepatitis C. Although uncommon, cirrhosis is occasionally seen in infected children and adolescents younger than 18 [9]. Moreover, children have a long life expectancy during which HCV complications may develop. So, HCV treatment in children and adolescent is important to avoid progressive disease with the development of cirrhosis and subsequent hepatocellular carcinoma [10]. Moreover, infected children and adolescents could transmit HCV to others. So, they should be treated hand in hand with the treatment of adults.
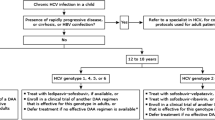
Although, the major concern of HCV treatment was directed to adults due to the higher prevalence rate when compared to pediatrics, eradication of HCV infection in childhood could be equally important to achieve HCV-free community. HCV treatment is rapidly evolving since the introduction of direct-acting antivirals (DAAs). Interferon (IFN) with its high rate of complications is no longer recommended for the treatment of HCV in children 12 years and older. Instead, ledipasvir (LED) and sofosbuvir (SOF) with different treatment regimens are the nowadays accepted treatment in this age group [11].
Genotype 4 is relatively exclusively the prevalent genotype in Egypt [2, 12,13,14]. Few studies [15,16,17] have shown the efficacy and safety of the fixed-dose combination therapy with SOF/LED in Egyptian children with genotype 4. In spite of the safety and effectiveness, the cost might stand against the feasibility of treatment of all affected children, especially in developing countries with limited resources and high prevalence rate. Moreover, its safety and efficacy in cirrhotic cases and in those below 12 years or less than 35 kg, and children with different comorbidities is not known. We aimed in this study to assess the safety and efficacy of the generic SOF/LED fixed-dose combination 400/90 (400 mg SOF + 90 mg LED) for the treatment of adolescents and children (9–12 years) with chronic hepatitis C (CHC).
Materials and methods
Study population
In this longitudinal prospective observational study 100 children with CHC seeking medical advice at the Pediatric Hepatology, Gastroenterology, and Nutrition Department, National Liver Institute, Menofiya University were recruited consecutively according to fulfillment of the defined inclusion and exclusion criteria. Cases were documented to have chronic HCV by positivity for anti-HCV and HCV-RNA for more than 6 months. The study duration was from August 2017 to June 2018. Parents/guardians of all cases signed an informed consent.
Workup before start of therapy
All cases underwent full history taking, thorough clinical examination, and a list of investigations. In history, stress was laid on comorbidity, past history of HCV therapy, duration of HCV acquisition, history of operations, blood transfusion, dentist visit, community barber, exposure to used syringes or razors, and family history for affected other members. Thorough clinical examination was performed for all cases stressing on jaundice, hepatomegaly, splenomegaly, ascites, and ocular, cardiac and neurologic examinations.
A list of pretreatment investigations was performed for all cases; it included: (1) Anti-HCV, HCV-RNA, and HCV genotype: Hepatitis C virus antibody was tested by 4th generation enzyme-linked immunosorbent assay (ELISA) (Innogenetics, Ghent-Belgium). Real-time polymerase chain reaction for HCV-RNA was performed using COBAS® Ampliprep/COBAS® TaqMan®, Roche Molecular Systems, Inc., Branchburg, NJ, 08876 USA. Detection limit was 15 IU/ml. For genotyping, restriction fragment length polymorphism analysis was performed using restriction enzymes Hae III, Rsa I, Mva I and Hinf I on PCR amplified 5′-untranslated region; (2) serology for hepatitis B virus: HEPATITIS B surface antigen (HBsAg), anti-hepatitis B core IgM, and IgG types were tested using an ELISA kit (Sorin Biomedica Co, Saluggia, Italy); (3) biochemical and hematological analysis: liver function tests (total and direct bilirubin, total proteins, albumin, alanine transaminase (ALT), aspartate transaminase (AST), γ-glutamyl transpeptidase, alkaline phosphatase), prothrombin time and international normalized ratio (INR), complete blood count (CBC), random blood sugar, serum creatinine with calculation of estimated glomerular filtration rate (eGFR) using Schwartz formula [18] were performed for each patient; (4) transient elastograhy: liver fibrosis was assessed by the measurement of liver stiffness through transient elastography (Fibroscan, Echosens, France). The liver stiffness was expressed in kilopascals (kPa). A higher kPa reflects a stiffer liver and more severe liver fibrosis. The following cutoff values defined by meta-analysis of different studies [19] were used to assess the different fibrosis stages; METAVIR F0/F1 < 7.1 kPa, F2 = 7.1–9.9 kPa, F3 = 10–13 kPa, F4 > 13 kPa; (5) echocardiography and electrocardiogram (ECG).
Inclusion and exclusion criteria
All cases with confirmed chronic HCV, aged 12–18 years and/or weighing ≥ 35 kg, treatment naïve and experienced cases were included. Another seven cases with an age of 9–12 years and weighing < 35 kg were also included.
All cases with coinfection with hepatitis B virus, concomitant malignancy, decompensated cirrhosis, with eGFR < 30 ml/min/1.73 m2, or with cardiac disease were excluded from the study. Those with comorbidities such as thalassemia minor, epilepsy, nephrotic syndrome, hemophilia, hypothyroidism, and cerebral palsy were not excluded.
One hundred and sixty-three cases were referred and evaluated during the recruitment period. The included 100 cases in the present study were consecutive subjects according to fulfillment of the reported inclusion and exclusion criteria while the remaining 63 cases were excluded due to the presence of any of the exclusion criteria mentioned above.
Treatment regimen and monitoring during and after finishing therapy
All children received a fixed-dose SOF/LED (400 mg/90 mg), one tablet per day, at fixed daily time, for 12 weeks. In our study we used the generic preparation Heterosofir Plus tablets, that cost 1100 LE (≈ 60$) for the 28 tablets bottle (Pharmed Healthcare, Al Sadat city, Al Menofia, Egypt; Ministry of Health registration number 31,264/2016). Fortunately all recruited cases were able to swallow the whole tablet as it is without the need of its crushing. The manufacturer company had no role in the study design, recruitment of cases, or manuscript writing.
Follow-up for all cases was on the week 2 (very rapid virologic response “vRVR”), 4, 8, and 12 (end of treatment “EOT”) from the start of therapy and 12 weeks after the stoppage of therapy (sustained virologic response 12 “SVR12″). For any complaint in-between these defined timing of follow-up, telephone contact with the working team was available all the time for all patients, besides daily morning outpatient clinic service. In every follow-up visit, the following was performed:
-
Checking for any possible drug-related side effect namely; fatigue, headache, nausea, diarrhea, insomnia, weakness, bradycardia, cough, myalgia, dyspnea, irritability, dizziness, depression, skin rash, abdominal pain, chest pain, increased skin pigmentation, itching, and fever. All these side effects were reported in five grades where grade (G) 0; negative, G1; mild (does not interfere with daily activity), G2; moderate (interferes with daily activity), G3; severe, and G4; life-threatening.
-
Assessment of compliance: parents were given charts to register daily the timing of the tablet ingestion and any adverse effects. These charts were checked during the regular visits. All cases were compliant without missing any dose.
-
Full examination; general, neurological, cardiorespiratory, and abdominal examination.
-
Total and direct bilirubin, AST, ALT, Albumin, INR, and CBC.
-
HCV-RNA testing.
Statistical analysis
Quantitative variables were expressed as mean ± standard deviation (SD) or a median (minimum–maximum) according to the nature of the data, while qualitative variables were expressed as number (percentage) of individuals with a condition. For quantitative data, statistical significance was tested by independent samples t test or by non-parametric Mann–Whitney U test according to the nature of the data. For comparison between the pre- and post-treatment data the paired t test and Wilcoxon test were used according to the nature of the data. For qualitative data, significance was tested by Chi-square test or Fisher’s exact test. Analysis of covariance (ANCOVA) was performed for the relation of certain parameters to age adjusted for weight as a covariate. Results were considered significant if p value was < 0.05. Statistical analysis was performed using SPSS, version 16 (SPSS Inc, Chicago, IL, USA).
Results
Demographic and clinical characteristics of the studied groups at baseline
One hundred cases of CHC with a mean of age 13.8 ± 2.1 years were recruited. Age ranged from 9 to 18 years, 13 of them were below 12 years (six cases ≥ 35 kg and seven cases < 35 kg). Weight ranged from 28 to 90 kg with a mean of 48.4 ± 15 kg. Twenty-one cases were below 35 kg; 14 of them were ≥ 12 years while seven cases were < 12 years old. Most of the cases were males (66%). Body mass index was 21.5 ± 4.9 kg/m2. Twenty cases (20%) had a past history of treatment with pegylated interferon (PegIFN) and ribavirin (RBV); while the remaining eighty cases (80%) were naïve.
Comorbidities were present in 11 (11%) cases in the form of; thalassemia minor (4), nephrotic syndrome (2), epilepsy (2), hemophilia (1), hypothyroidism (1), and cerebral palsy (1).
Documented duration of HCV acquisition, defined at recruitment in the study, had a median of 24 months (range 95 months). Risk factors were present in 83 cases (83%); they were, in descending order of frequency, dentist visit (45), community barber (30), history of operation (29), blood transfusion (28), used syringes (2). Positive family history of HCV infection was present in 64 (64%) cases; mother (30), father (18), mother and father (7), mother and brother (1), and others (8).
None of the recruited cases had jaundice, ascites, nor a history or clinical findings of cardiac disease. Hepatomegaly was detectable in 16 (16%) of cases while splenomegaly was present in only 2 (2%) of cases.
All previously mentioned demographic, history, and clinical data showed no significant difference between naïve and treatment-experienced cases, except for splenomegaly which was significantly higher in treatment-experienced cases (0% for naïve, 10% for treatment experienced; p = 0.038).
Pretreatment baseline laboratory parameters
Liver function tests, INR, CBC, RBS, and creatinine showed normal median and mean values despite an elevation of some parameters in some cases. AST was significantly higher in treatment experienced cases (p = 0.039) while ANC was significantly higher in the naïve group (p = 0.045). No significant differences were found between naïve and the treatment-experienced groups regarding all other laboratory parameters (p values in Table 1).
Laboratory parameters during, at the end, and 12 weeks post-treatment
All laboratory parameters were maintained normal at W2, W4, W8, and W12 of therapy and 12 weeks post-treatment. Those cases (n = 13) with elevated ALT pretreatment, showed normalization at W2 and maintained normal till the EOT and at week 12 post-treatment, except for two cases which showed slight fluctuation of ALT during treatment but achieved normal level at week 12 post-treatment (Fig. 1a). While cases with elevated AST at W0 (n = 28) showed rapid normalization at W2 except for elevated levels for 8 cases, 5 cases at W4, 2 cases at W8 and W12 (EOT). All achieved normal AST at W12 post-treatment (Fig. 1b).
Follow-up of individual cases within the total study group with elevated ALT (a) and AST (b) before start of therapy. The dotted lines in Fig. 1a, b represent the upper level of the normal values of ALT (44 U/L) and AST (34 U/L), respectively
Follow-up of individual cases, within the treatment-experienced group, with elevated ALT (a) and AST (b) before start of therapy. The dotted lines in Fig. 2a, b represent the upper level of the normal values of ALT (44 U/L) and AST (34 U/L), respectively
AST, ALT, and creatinine showed significant decrease at the EOT from the pretreatment level (p < 0.001, < 0.001, and 0.014; respectively). Also, hemoglobin showed a significant decrease from baseline (p < 0.001), in spite of normal level (Table 1).
Baseline and follow-up viral load
Baseline viral load ranged from 17,700 to 105 × 106 with a median of 364,710 IU/ml. All tested cases were genotype 4. Interestingly in the present study, 96 cases (96%) achieved negative PCR at week 2 of treatment (96% vRVR) with the remaining positive 4 cases having a low viral load (1500, 244, 234, and 186 IU/ml). All the four cases were naïve, had no comorbidity, and had a weight > 35 kg. They were two males and two females, with no-mild degree of fibrosis (F0/F1). The vRVR was not related to age when adjusted for weight (p = 0.415). At weeks 4, 8, and 12 of treatment all cases were negative for PCR; 100% response rate since week 4 till the EOT. SVR12 was also 100%. Figure 4 shows the virologic response in the present study at weeks 2, 4, 8, 12 of therapy and 12 weeks post-treatment (W24) and another two pediatric studies [15, 16] used the standard drug Harvoni® for the treatment of Egyptian children and adolescents with genotype 4 CHC.
Bar diagram of the virologic response at weeks 2, 4, 8,12 of therapy and 12 weeks post-treatment (W24) of the present study using the generic drug and two pediatric studies [15, 16] treating Egyptian children and adolescents with genotype 4 chronic hepatitis C using the standard brand drug, Harvoni®
Fibrosis stage
Most of cases (94%) showed none to mild degree of fibrosis (F0/F1) with kPa of 4.8 ± 0.9 as assessed by Fibroscan with only few cases showed a significant degree of fibrosis (F2, 5% with kPa of 9.1 ± 1.2; F3, 1% with kPa of 12.5). Fibrosis stage showed no significant difference between both naïve and treatment-experienced groups. However, absent liver biopsy data is considered a limitation of this study.
Safety and side effects
All cases had no serious side effects or side effects that led to treatment stoppage. However, all side effects were G1. Rate of side effects was highest (58%) in the start of therapy at week 2, decreasing to 40%, 39%, 31% at weeks 4, 8, 12 of therapy. All side effects disappeared after treatment stoppage, scoring zero % at W12 post-treatment (Fig. 3a). The most reported side effects were fatigue, headache, weakness, nausea, and abdominal pain scoring 37%, 33%, 14%, 13%, and 11%, respectively, at week 2 of therapy (Fig. 3b). Side effects were not different according to age when adjusted for weight except for those reported at week 4 of treatment, at which time side effects were more significantly reported with increasing age. No statistical difference was reported between naïve and treatment-experienced cases regarding the incidence of side effects; totally or individually (p > 0.05, for all).
The treatment-experienced group
The treatment-experienced group consists of 20 children with a mean age of 13.2 ± 1.7 years (10–16 years) with a weight of 49.2 ± 18 kg (28–83 kg), 11 males and 9 females. The baseline ALT before start of therapy showed normal level except for five cases with an ALT ranging from 66 to 132 U/L. Three of these cases achieved normal level at W2 till the EOT and at W12 post-treatment (W24). While the other two cases remained with elevated levels till the EOT but achieved normal values at W24 of therapy. The baseline AST showed high levels in eight cases ranging from 51 to 144 U/L. Four cases achieved normal level at W2 of treatment and remained normal till the EOT and at W24 of therapy, except for one case that showed mild elevation at W4 of therapy with re-normalization on further follow-up. Two cases achieved normal level at W4 and remained normal, while the last two cases remained high till the EOT (W12) and achieved normal level at W24 of therapy (Fig. 2).
The pretreatment baseline level of viremia had a median of 493,143 IU/ml (40,000 − 2.5 × 106 Iu/ml). All cases (100%) achieved negative viremia at W2 of therapy (vRVR) and remained negative at W4, W8, and W12 of therapy with 100% SVR12.
Discussion
There has been a great transition of CHC treatment since the introduction of the recent DAAs [11]. The effort that was extensively carried out in Egypt by the governmental and nongovernmental organizations to treat chronic HCV in the era of PegIFN/RBV is now extending in the era of the DAAs targeting eradication of HCV in the near future. More than 1 million of Egyptian adults have been successfully treated by DAAs till now [20].
Even though adults constitute the major sector of infected people; those below 18 years are not few [4] and could be affected significantly with some complications [21]. Moreover, they constitute a reservoir for infection that should be targeted together with the adult treatment programs to eradicate the viral infection worldwide.
In adolescents aged 12–17 years or weighing at least 35 kg with chronic HCV and without cirrhosis or with only compensated cirrhosis, WHO [22] recommends: SOF/LED for 12 weeks (for 24 weeks in those who are treatment experienced and with compensated cirrhosis) in genotypes 1, 4, 5 and 6; SOF/LED for 12 weeks in genotype 2; SOF/LED for 24 weeks in genotype 3. Although all these recommendations are graded as strong, they have very low quality of evidence. This clarifies the need for more added real-world experiences in this age group, and the importance of the present study that could help in the way of developing high quality of evidence for the future treatment guidelines.
Even though DAAs showed a high efficacy and safety in adolescents with genotype 4 [15, 16, 23] and the other genotypes [24, 25] in the few studies till now, cost is a matter of concern. In Egypt, following negotiation with Gilead for reducing price of SOF [26], the government has supported the development of the domestic pharmaceutical industry with the production of Heterosofir Plus [27]. To the best of our knowledge, the present study is the first observational open-labeled study to evaluate the efficacy and safety of the generic fixed-dose SOF/LED (400 + 90) (Heterosofir Plus) in the treatment of both naïve and treatment-experienced genotype 4 CHC in children, 9–12 years, and adolescents. Previous studies reported the efficacy and safety of the brand combination, Harvoni®, with its high cost for the treatment of chronic HCV genotype 4 in adolescents [15, 16].
A 12 weeks course of the brand drug SOF/LED (400 + 90), Harvoni® manufactured by Gilead Sciences costs $94,500 per patient in the US market. Gilead Sciences ultimately agreed to license Harvoni® in Egypt at a price of $300 for a 1-month supply, or $900 for a full 12-week course of treatment [28]. Eventually, generic manufacturers in Egypt drove that price down. Pharmed Healthcare, a pharmaceutical company in Egypt, manufactured Heterosofir Plus tablets that cost about $180 per patient for 12 weeks [27]. Other Egyptian companies manufactured the same fixed-dose combination with a similar price range to Heterosofir Plus. The efficacy of the used cheaper generic preparation in the present study was comparable to the brand drug used [15, 16], achieving 100% EOT response and SVR12.
Our results revealed 96% vRVR at W2, 100% response rate at W4 that was maintained till the EOT, and finally SVR12 of 100%. Compliance was monitored regularly and no patient had skipped doses. These results are unique to the present study. Even those with positive viremia at week 2, had significant reduction of their viral load from baseline level to a level of viremia ranging from 186 to 1500 IU/ml. Of an important note, that the frequent testing of the level of viremia, at 2–4 weekly intervals, is not recommended when treating children in routine practice, rather it was just tested in the present study for research purpose. El-Khayat et al. [16] reported a SVR12 of 99% of their treated adolescents, while El-Karaksy et al. [15] reported 97.5% response rate at W4 of treatment and 100% response rate at W8, 12 and SVR12. Neither of the studies reported a response rate at W2.
Moreover, there was no report of the same dose SOF/LED (400 + 90) in ages younger than 12 years or below 35 kg. In the present study, we used the same fixed-dose recommended for adolescents 12–18 years old and/or above 35 kg for children aged 9–12 years and/or weighing 28–35 kg. Elkaraksy et al. [15] used the same dose for two children aged 11.5 years but weighing > 35 kg. El-Shabrawi et al. [29] used half the dose in a pilot study for the treatment of 20 children with an age 6–12 years and a weight ranging from 15 to 30 kg.
The present study included six children with an age below 12 years (10–11.5) but weighing ≥ 35 kg, and another 14 cases weighing less than 35 kg (28–34 kg) but aged ≥ 12. Both categories were within the FDA guidelines criteria of adolescents’ treatment [22]. None of the categories showed significant side effects and the treatment was 100% effective. This encouraged us to recruit few cases out of the criteria regarding age and weight. The study included seven cases with an age (9–11 years) and weighing 29–32 kg. All seven cases achieved 100% vRVR and SVR12 with negligible side effects.
Reported side effects in the present work were all mild, decreasing in frequency with follow-up, and did not lead to treatment termination in any of the cases. The most reported side effects were fatigue, headache, weakness, nausea, and abdominal pain scoring 37%, 33%, 14%, 13%, and 11%, respectively, at week 2 of therapy. Similarly, El-Karaksy et al. [15] reported that fatigue was the most frequently reported side effect in about half of their treated patients followed by headache, nausea, irritability and dizziness.
The reason for this higher rate of side effects than those reported in adults [30, 31] could be attributed to the age difference. Some side effects that were reported by children and adolescents could be tolerated and ignored by adults. Moreover, being a newly introduced drug therapy there was a meticulous attitude from both the medical team and parents about reporting any trivial symptoms, which we believe they will be ignored later on after experience in the drug. Also, the association of some comorbidity (11% of cases) could have a share in this higher rate of adverse effects.
In the present study, there was no relapse of any case even those with baseline elevated AST and ALT or those with advanced disease stage with F2–F3. El-Khayat et al. [16] reported a relapse rate of 1% (2 cases of their treated 144 adolescents). Their relapsed cases had baseline elevated liver enzymes and F0/F1, with elevation of AST and ALT at W12 of treatment. This result augments the value of AST and ALT monitoring during therapy and at the EOT, to predict relapse. In the present study, AST and ALT were maintained normal for most of cases after W2 of treatment.
The strength of this study is the usage of the cheaper generic fixed-dose combination SOF/LED that improves the opportunity for the treatment of all infected cases without the handicap of the treatment cost. Moreover, it is the first study that shows the vRVR at W2 of therapy in adolescents. Also, the 100% response rate at W4 till the EOT and SVR12 is unique for this study in spite of the inclusion of few cases with a significant degree of fibrosis, and comorbid conditions. Lastly, it shows the safety and efficacy in the age 9–12 years and weight 28–35 kg with the same fixed-dose combination given for adolescents.
In conclusion, this study shows that the cheap generic fixed-dose SOF/LED is safe and effective for children 9–12 years old and adolescents with genotype 4 chronic hepatitis C, with no reported significant side effects. Moreover, it is safe in those with significant fibrosis and comorbidities like thalassemia, epilepsy, and hemophilia.
References
Guerra J, Garenne M, Mohamed MK, et al. HCV burden of infection in Egypt: results from a nationwide survey. J Viral Hepat 2012;19(8):560–567.
Gower E, Estes C, Blach S, et al. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol 2014;61(1 Suppl):S45–S57.
El-Karaksy H, Anwar GH, El-Raziky MS, et al. Anti-HCV prevalence among diabetic and non-diabetic Egyptian children. Curr Diabetes Rev 2010;6(6):388–392.
Barakat SH, El-Bashir N. Hepatitis C virus infection among healthy Egyptian children: prevalence and risk factors. J Viral Hepat 2011;18(11):779–784.
El-Raziky MS, El-Hawary M, Esmat G, et al. Prevalence and risk factors of asymptomatic hepatitis C virus infection in Egyptian children. World J Gastroenterol 2007;13(12):1828–1832.
Chaabna K, Cheema S, Abraham A, et al. Systematic overview of hepatitis C infection in the Middle East and North Africa. World J Gastroenterol 2018;24(27):3038–3054.
Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and nutrition examination survey 2003–2010. Ann Intern Med 2014;160(5):293–300.
Khaderi S, Shepherd R, Goss JA, et al. Hepatitis C in the pediatric population: transmission, natural history, treatment and liver transplantation. World J Gastroenterol. 2014;20(32):11281–11286.
El-Araby HA, Ehsan NA, Konsowa HA, et al. Hepatic progenitor cells in children with chronic hepatitis C: correlation with histopathology, viremia, and treatment response. Eur J Gastroenterol Hepatol 2015;27(5):561–569.
Gonzalez-Peralta RP, Langham MR Jr, Andres JM, et al. Hepatocellular carcinoma in 2 young adolescents with chronic hepatitis C. J Pediatr Gastroenterol Nutr 2009;48(5):630–635.
Hepatitis C. Guidance 2018 update: AASLD-IDSA Recommendations for testing, managing, and treating hepatitis C virus infection. Clin Infect Dis 2018;67(10):1477–1492.
El Naghi S, Abdel-Ghaffar TY, El-Karaksy H, et al. Safety and efficacy of Hansenula-derived PEGylated-interferon alpha-2a and ribavirin combination in chronic hepatitis C Egyptian children. World J Gastroenterol 2014;20(16):4681–4691.
Kamal SM, Nasser IA. Hepatitis C genotype 4: What we know and what we don’t yet know. Hepatology 2008;47(4):1371–1383.
Abdel-Hamid M, El-Daly M, Molnegren V, et al. Genetic diversity in hepatitis C virus in Egypt and possible association with hepatocellular carcinoma. J Gen Virol 2007;88(Pt 5):1526–1531.
El-Karaksy H, Mogahed EA, Abdullatif H, et al. Sustained viral response in genotype 4 chronic hepatitis C virus-infected children and adolescents treated with Sofosbuvir/Ledipasvir. J Pediatr Gastroenterol Nutr. 2018;67(5):626–30.
El-Khayat HR, Kamal EM, El-Sayed MH, et al. The effectiveness and safety of ledipasvir plus sofosbuvir in adolescents with chronic hepatitis C virus genotype 4 infection: a real-world experience. Aliment Pharmacol Ther 2018;47(6):838–844.
Ghobrial C, Sobhy R, Mogahed E, et al. Is sofosbuvir/ledipasvir safe for the hearts of children with hepatitis C virus? Dig Liver Dis 2019;51(2):258–262.
Schwartz GJ, Brion LP, Spitzer A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 1987;34(3):571–590.
Friedrich-Rust M, Ong MF, Martens S, et al. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology 2008;134(4):960–974.
El-Akel W, El-Sayed MH, El Kassas M, et al. National treatment programme of hepatitis C in Egypt: hepatitis C virus model of care. J Viral Hepat 2017;24(4):262–267.
Squires JE, Balistreri WF. Hepatitis C virus infection in children and adolescents. Hepatol Commun 2017;1(2):87–98.
Guidelines for the care and treatment of persons diagnosed with chronic hepatitis C virus infection. Geneva: World Health Organization; 2018. p. 1–86. ISBN 978-92-4-155034-5. https://www.ncbi.nlm.nih.gov/books/NBK531733/pdf/Bookshelf_NBK531733.pdf.
El-Shabrawi MH, Abdo AM, El-Khayat HR, et al. Shortened 8 weeks course of dual Sofosbuvir/Daclatasvir therapy in adolescent patients, with chronic hepatitis C infection. J Pediatr Gastroenterol Nutr 2018;66(3):425–427.
Balistreri WF, Murray KF, Rosenthal P, et al. The safety and effectiveness of ledipasvir-sofosbuvir in adolescents 12–17 years old with hepatitis C virus genotype 1 infection. Hepatology 2017;66(2):371–378.
Wirth S, Rosenthal P, Gonzalez-Peralta RP, et al. Sofosbuvir and ribavirin in adolescents 12–17 years old with hepatitis C virus genotype 2 or 3 infection. Hepatology 2017;66(4):1102–1110.
Lemoine M, Eholie S, Lacombe K. Reducing the neglected burden of viral hepatitis in Africa: strategies for a global approach. J Hepatol 2015;62(2):469–476.
Healthcare P. Heterosofir Plus. 2019 [cited 2019 7 January 2019]; http://pharmedhc.com/heterosofir-plus/.
Halter C. Egypt Could Eliminate Hepatitis C Among Its Population by 2023. 2018 May 29 [cited 2019 August 13]. https://www.hepmag.com/article/egypt-eliminate-hepatitis-c-among-population-2023.
El-Shabrawi MHF, Kamal NM, El-Khayat HR, et al. A pilot single arm observational study of sofosbuvir/ledipasvir (200 + 45 mg) in 6- to 12- year old children. Aliment Pharmacol Ther 2018;47(12):1699–1704.
Shiha G, Esmat G, Hassany M, et al. Ledipasvir/sofosbuvir with or without ribavirin for 8 or 12 weeks for the treatment of HCV genotype 4 infection: results from a randomised phase III study in Egypt. Gut 2019;68(4):721–728.
Tao T, Jiang X, Chen Y, et al. Efficacy and safety of Ledipasvir/Sofosbuvir with and without ribavirin in patients with chronic hepatitis C virus genotype 1 infection: a meta-analysis. Int J Infect Dis 2017;55:56–71.
Acknowledgements
We acknowledge National Liver Institute, Menofiya University, for funding this work. We would like to thank the residents and nursing staff of the Pediatric Hepatology, Gastroenterology, and Nutrition Department and all physicians and working staff of the Clinical Biochemistry and Radiology Departments for their contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The study was approved by the Research Ethics Committee of the National Liver Institute, Menofiya University and conforms to the 1964 Declaration of Helsinki and its later amendments. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from parents/guardians of all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El-Araby, H.A., Behairy, B.E., El-Guindi, M.A. et al. Generic sofosbuvir/ledipasvir for the treatment of genotype 4 chronic hepatitis C in Egyptian children (9–12 years) and adolescents. Hepatol Int 13, 706–714 (2019). https://doi.org/10.1007/s12072-019-09985-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09985-w