Abstract
Background and aims
Status 1A patients are prioritized over end-stage liver disease (ESLD) for liver transplantation (LT). ESLD patients with high MELD may have higher waitlist mortality than Status 1A patients, and may require LT more urgently.
Methods
Using United Network for Organ Sharing registry data, we retrospectively evaluated LT waitlist mortality and probability of LT between adults in the United States with Status 1A or ESLD with MELD >30 listed for LT from 2003–2013. Overall waitlist mortality and probability of LT were evaluated with Kaplan–Meier and multivariate logistic regression models.
Results
From 2003–2013, 15,049 ESLD patients with MELD >30 and 3049 Status 1A patients were listed for LT. While overall 14-day waitlist survival decreased with increasing MELD score among ESLD patients (54.0 % for MELD 31–35; 37.1 % for MELD 36–40; 27.5 % for MELD >40), overall survival at 14 days was significantly lower among Status 1A (14.4 %). Compared to Status 1A, ESLD patients with MELD >40 had significantly higher 14-day waitlist mortality (OR 1.92; 95 % CI 1.56–2.36; p < 0.001), whereas ESLD patients with MELD 36–40 had a non-significant trend towards higher waitlist mortality (OR 1.16; 95 % CI 0.93–1.45; p = 0.181). No difference in probability of LT within 14 days was observed between ESLD with MELD >40 and Status 1A (p = 0.89). ESLD patients with MELD >40 had higher post-LT survival compared to Status 1A on multivariate regression modeling (HR 0.80; 95 % CI 0.66–0.96; p < 0.02).
Conclusion
Among adults in the United States awaiting LT, ESLD patients with MELD >40 have significantly higher waitlist mortality, but similar probability of receiving LT compared to Status 1A patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Key Points
-
Increasing MELD scores among end-stage liver disease (ESLD) awaiting liver transplantation (LT) are associated with higher waitlist mortality.
-
ESLD patients with MELD >40 have higher waitlist mortality than Status 1A patients awaiting LT.
-
However, probability of receiving LT was similar between patients with ESLD with MELD >40 and Status 1A.
-
Among patients that receive LT, overall post-LT survival was significantly higher among ESLD with MELD >40 than Status 1A patients.
Introduction
Both fulminant hepatic failure (FHF) and decompensated end-stage liver disease (ESLD) are serious and irreversible conditions with high morbidity and mortality [1–5]. FHF is defined as the acute development of severe liver injury with encephalopathy and impaired synthetic function within 8 weeks of the first symptoms of liver disease in a patient without preexisting liver disease, while ESLD refers to cirrhosis at its late stages [2, 6]. Liver transplantation (LT) is a highly effective curative option for both FHF and ESLD, but it is not readily available to many patients due to shortage of available donor organs [1, 2, 6–10]. Consequently, the most ideal policy for equitable prioritization and allocation of liver transplants among these seriously ill patients continues to be debated. In the United States, The Final Rule (Code of Regulations, Title 42, Part 121.8) mandates “equitable allocation of organs among patients from most to least medically urgent” [11]. Adoption of the model for end-stage liver disease (MELD) score in 2002 established an objective method of prioritizing waitlisted ESLD patients according to disease severity, but Status 1A patients, or patients with FHF, continue to take priority over ESLD patients regardless of MELD score under the assumption that FHF patients have significantly higher waitlist mortality and thereby are in most urgent need of LT [1, 3, 7–10, 12–15]. Recent data from Sharma et al. suggested that ESLD patients with high MELD scores >40 have higher waitlist mortality than Status 1A patients [16]. However, this prior study included patients before and after implementation of the MELD score. Furthermore, waitlist mortality is multi-factorial and is affected by disease progression leading to potential waitlist drop-off from being too ill, and directly related to one’s probability of receiving LT. Our present study utilizes 11 years of post-MELD era data to evaluate waitlist mortality and probability of LT among patients with Status 1A and ESLD patients with high MELD scores.
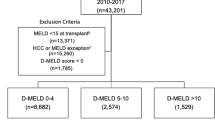
Methods
Adult male and female patients (age >18 years) who were registered on the waitlist for liver transplant in the United States from January 1, 2003 to December 31, 2013 were evaluated using data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network (UNOS/OPTN) registry. The UNOS/OPTN database includes demographic and clinical information on all organ donors and transplant recipients in the United States, submitted by their transplant centers, and is provided to investigators as de-identified data. The Health Resources and Services Administration, US Department of Health and Human Services, provides oversight of the activities of the UNOS/OPTN. Our target population consisted of ESLD patients with MELD scores >30 and Status 1A patients who were awaiting liver transplant. MELD scores at the time of waitlist registration were calculated for each individual with ESLD using standard formulas that incorporate the natural logarithms (ln) of INR, bilirubin, and creatinine: 11.2 × ln(INR) + 9.57 × ln(creatinine, in mg/dL) + 3.78 × ln(bilirubin, in mg/dL) + 6.43, with a lower limit of 1 for all variables and upper limit of 4 for creatinine. Patients on hemodialysis are given a creatinine score of 4 [13, 14]. Patients who received MELD exception points (e.g., patients with hepatocellular carcinoma) were excluded from our analyses. All adult patients with Status 1A designation at time of LT listing were included.
Clinical and demographic comparisons between Status 1A and ESLD patients were presented as proportions (%) and frequencies (N) for categorical variables, or mean and standard deviation for continuous variables. The chi-square test was utilized for comparing categorical variables and Student’s t test or analysis of variance methods were used for continuous variables. ESLD patients with MELD >30 were further stratified into three categories for analyses (MELD 31–35, MELD 36–40, and MELD >40). Overall 28-day waitlist mortality and overall 28-day probability of receiving LT were evaluated for Status 1A patients and the ESLD patients using Kaplan–Meier methods. Given the very high waitlist mortality at 28 days among Status 1A patients (28-day survival 7.2 %) and ESLD patients with MELD >40 (28-day survival 9.4 %), we decided to use 14-day waitlist mortality as the outcome measure in the multivariate model to improve the ability to detect clinically significant differences in waitlist mortality between the two comparator groups. Multivariate logistic regression models were utilized to evaluate 14-day waitlist mortality and 14-day probability of receiving LT between Status 1A and ESLD patients. Multivariate Cox proportional hazards models evaluated overall survival following LT between ESLD patients and Status 1A patients. Models were developed using forward stepwise regression methods, and variables that were significant in the univariate model (p < 0.10) or were of biological importance (e.g., age) were included in the final multivariate model. The final multivariate model included adjustments for age, sex, race/ethnicity, body mass index, hepatic encephalopathy, and ascites. Statistical significance was met with 2-tailed p-value <0.05. All statistical analyses were performed by using the Stata statistical package (version 10, Stata Corp, College Station, TX).
Results
Overview
From January 1, 2003 to December 31, 2013, there were a total of 18,098 adult patients on the liver transplant waitlist who met the criteria for either Status 1A (n = 3049) or ESLD with MELD > 30 (n = 15,049). Demographic characteristics of the Status 1A and MELD >30 patients are listed in Table 1. The etiology of liver disease among Status 1A and MELD >30 patients are listed in Supplemental Table A. While the majority of MELD >30 patients were male (56.5 %), the majority of Status 1A candidates were female (62.8 %). The average age of waitlist patients was significantly higher among patients with MELD >30 compared to those with Status 1A (57.4 vs 42.1, p < 0.01). While non-Hispanic whites accounted for the majority of patients among both Status 1A patients and ESLD patients, there were significantly more blacks in the MELD >30 group compared to the Status 1A group (32.5 vs. 15.6 %, p < 0.01). In addition, the prevalence of obesity was significantly higher among Status 1A patients when compared to MELD >30 patients (30.9 vs. 19.2 %, p < 0.01). While Status 1A patients had significantly higher rates of grade 3–4 hepatic encephalopathy compared to ESLD patients with MELD >30 (57.7 vs. 37.2 %, p < 0.01), ascites were only present in 51 % of Status 1A patients compared to 95.3 % of ESLD patients with MELD >30. Status 1A patients had higher INR, but patients with MELD >30 had higher levels of serum total bilirubin (Table 1).
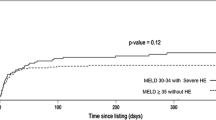
Liver transplant waitlist survival
Figure 1 shows the Kaplan–Meier curve for 28-day waitlist survival stratified by Status 1A and ESLD patients. While overall 14-day waitlist survival decreased with increasing MELD score among ESLD patients (54.0 % for MELD 31–35; 37.1 % for MELD 36–40; 27.5 % for MELD >40), overall survival at 14 days was significantly lower among Status 1A patients (14.4 %) (median survival, 95 % CI MELD 31–35, 17 days, 95 % CI 14–19; MELD 36–40, 10 days, 95 % CI 9–12; MELD >40, 8 days, 95 % CI 8–9; Status 1A, 3 days, 95 % CI 2–3). Compared to Status 1A patients, 28-day waitlist survival was significantly higher among ESLD patients with MELD 31–35 and MELD 36–40, but no significant difference was seen when compared to ESLD patients with MELD >40 (Status 1A: 7.2 % vs. MELD >40: 9.4 %, p = 0.33) (Fig. 1).
On multivariate logistic regression analysis, ESLD patients with MELD scores 31–35 had significantly lower 14-day waitlist mortality compared to Status 1A (OR 0.47; 95 % CI 0.37–0.60; p < 0.001), whereas ESLD patients with MELD 36–40 had a non-significant trend towards higher waitlist mortality (OR 1.16; 95 % CI 0.93–1.45; p = 0.181), and ESLD patients with MELD >40 had significantly higher 14-day waitlist mortality (OR 1.92; 95 % CI 1.56–2.36; p < 0.001) (Table 2).
Probability of receiving liver transplant
Given that the probability of receiving LT directly affects waitlist mortality, we evaluated differences in probability of receiving LT between Status 1A and ESLD patients to better understand the survival differences observed. Figure 2 shows the Kaplan–Meier curve for 28-day probability of liver transplant stratified by Status 1A and ESLD patients with MELD >30. Overall 14-day liver transplant probability was significantly lower among ESLD patients of all MELD categories evaluated when compared to Status 1A patients [71.9 % (Status 1A) vs. 49.9 % (MELD 31–35) vs. 61.0 % (MELD 36–40) vs. 59 % (MELD >40)] (median time to LT, 95 % CI MELD 31–35, 15 days, 95 % CI 13–18; MELD 36–40, 10 days, 95 % CI 9–11; MELD >40, 10 days, 95 % CI 9–11; Status 1A, 4 days, 95 % CI 3–4) (Fig. 2). The overall probability of receiving LT at 28-days was significantly lower among ESLD patients with MELD 31–35 when compared to Status 1A patients (53.2 vs. 74.0 %, p < 0.01), whereas the probability of LT among ESLD patients with MELD 36–40 and MELD >40 were similar to that of Status 1A patients (Fig. 2).
On multivariate logistic regression analysis, patients with MELD scores 31–35 had significantly lower 14-day probability of receiving liver transplant compared to Status 1A (OR 0.81; 95 % CI 0.71–0.91; p < 0.001), whereas patients with MELD scores 36–40 had significantly higher probability of 14-day liver transplant (OR 1.35; 95 % CI 1.18–1.55; p < 0.001). Patients with MELD scores >40 had no significant difference in probability of receiving LT within 14-days compared to Status 1A patients (OR 1.01; 95 % CI 0.88–1.16; p = 0.895) (Table 2).
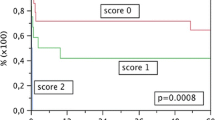
Survival following liver transplantation
Overall crude post-LT survival was similar for Status 1A, ESLD patients with MELD 36–40, and MELD >40 (Fig. 3). The 1-, 3-, and 5-year post-LT survival rates were 83, 78, and 74 % for Status 1A FHF, 83, 75, 70 % for ESLD patients with MELD 36–40, and 84, 76, and 70 % for ESLD patients with MELD >40 (Fig. 3). While the crude overall survival following LT was similar between the different patient groups, on multivariate Cox regression analysis, ESLD patients with MELD >40 had significantly lower post-LT mortality compared to Status 1A patients (HR 0.80; 95 % CI 0.66–0.96; p < 0.02) (Fig. 3).
Discussion
The most equitable approach to prioritizing LT between patients with ESLD and those with FHF requiring Status 1A designation remains controversial. However, the foundational objective to prioritize those with highest waitlist mortality and thereby those in greatest need of LT remains the goal. Our present analysis utilized the most recent data from all adult LT in the United States to compare waitlist mortality risk among Status 1A and ESLD candidates with high MELD scores. While Status 1A patients are prioritized over those with ESLD in clinical practice, our study demonstrates that ESLD patients with MELD >40 had significantly higher waitlist mortality compared to Status 1A patients awaiting LT. Furthermore, even ESLD patients with MELD 36–40 demonstrated a non-significant trend towards higher waitlist mortality when compared to Status 1A patients.
Among patients with decompensated ESLD, LT remains the only option for potential cure. The same is true for many patients presenting with fulminant hepatic failure, and without LT, mortality is high [1–3, 5, 7–10, 12, 15]. However, the limited availability of available donor organs has continued to fuel debate regarding the best model for organ allocation. While the MELD score was introduced in 2002 to help prioritize patients with chronic liver disease for LT, Status 1A patients continue to take priority over ESLD patients regardless of MELD score. Yet, it is not clear if this policy truly follows the original mandate of prioritizing organs to the sickest patients first, and some have questioned whether all Status 1A patients are truly sicker (i.e., higher waitlist mortality) when compared to ESLD with higher MELD scores. A recent study by Sharma et al. retrospectively analyzed data from September 1, 2001 to December 31, 2007 using US adult LT registry data from Scientific Registry of Transplant Recipients [16]. The authors observed that ESLD patients with MELD scores 36–40 had similar waitlist mortality risk compared to Status 1A patients, and those with MELD >40 had significantly higher waitlist mortality compared to Status 1A patients (HR = 1.96, p < 0.001). Based on this result, the authors concluded that liver transplant survival benefit was greater for ESLD patients with MELD >40 than for Status 1A patients, and suggested that the mechanism of broader sharing of organs should be made available to patients with high MELD scores. However, the study period included data before and after the periods which MELD was formally implemented and included outcomes from both pre-MELD and post-MELD eras. To further investigate this compelling observation, our present study sought to focus our analyses starting in 2003 and provides and updated analysis through 2013. In addition, cognizant of the relationship between waitlist mortality and probability of receiving liver transplantation, we evaluated waitlist mortality risk and probability of receiving liver transplantation among Status 1A and ESLD patients with MELD >30.
While our findings confirm those of Sharma et al. that waitlist mortality among ESLD patients with MELD >40 is significantly higher than those with Status 1A designation, the exact etiology for these observations is not clear. One hypothesis that has been implicated is the continued increasing prevalence of ESLD patients added to the LT waitlist, which given the growing imbalance between patients requiring LT and the availability of organs to be transplanted, contributes to overall rising MELD scores needed to achieve adequate priority to receive LT [17, 18]. Furthermore, the adoption of MELD exception points given to HCC patients has also led to increasing number of patients awaiting liver transplantation. In a recent study evaluating trends in LT in the United States, Wong et al. reported that while MELD at time of waitlist registration only increased minimally from 2004 to 2013 (from 16.4 ± 7.8 in 2004 to 17.4 ± 8.7 in 2013), the MELD at time of LT increased more significantly (from 28.9 ± 11.8 in 2004 to 35.3 ± 9.2 in 2013) [17]. This rising MELD score needed to receive LT contributes to sicker patients on the LT waitlist and thereby higher rates of waitlist mortality.
It is possible that categorization of patients as Status 1A may not have been completely accurate as is suggested by the patient characteristics in Table 1, with nearly 11 % of Status 1A patients without hepatic encephalopathy and a median INR of 3.2 or that patients listed as Status 1A may not be as critically sick as imagined. Furthermore, our findings may not be completely generalizable to other countries, where eligibility for Status 1A designation may be different. For example, in the United Kingdom and the rest of Europe, only patients with FHF who meet the King’s College Criteria or the Clichy criteria are listed as super-urgent or high urgency, whereas in Australia and New Zealand, only patients with FHF who are intubated in the intensive care unit are eligible for urgent listing for LT.
The probability of waitlist survival is directly correlated with one’s probability of receiving LT. When evaluating differences in probability of receiving LT, our present study observed no statistically significant differences in probability in receiving LT between Status 1A patients and patients with MELD >40, despite the latter group demonstrating waitlist mortality rates nearly double that of Status 1A patients. Furthermore, our analysis of post-LT survival showed that ESLD patients with MELD >40 have similar to higher likelihood of post-LT survival compared to Status 1A patients, suggesting that they obtain greater benefit from LT. These findings hold important implications for the current allocation policy. If the central aim of liver allocation is to minimize waitlist mortality and to maximize the benefit from LT, a modification of the current allocation policy to allow greater chances of LT for ESLD patients with MELD >40 may reduce overall waitlist mortality, and redistribute prioritization to those that are in most urgent need of LT.
Increasing MELD scores translate into increasing risk of mortality on the waitlist. A recently implemented policy that affects those with ESLD awaiting liver transplantation adds further complexity to the allocation process. The “Share 35” policy implemented on June 18, 2013 mandates that deceased donor livers are offered to regional candidates with MELD ≥35 before local candidates with MELD <35 in an effort to better redistribute livers to those in most urgent need, and more effectively apply the principles of the Final Rule. According to the 2013 OPTN/SRTR Annual Data Report, implementation of the Share 35 policy in 2013 resulted in dramatic reduction of median waiting time for ESLD patients with MELD scores of 35 or higher from 14.0 months in 2012 to 1.4 months in 2013 [18]. Massie et al. also reported that this translated into an 8 % decrease in overall waitlist mortality (sub-hazard ratio 0.92, p = 0.03), and steep fall in waitlist mortality by 30 % (SHR 0.70, p < 0.001) without an increase in mortality for patients with MELD scores ≤30 [19]. While there is no perfect solution to the complexities of organ allocation for liver transplantation, more research is needed to better define a more equitable approach for all patients that is safe, effective, and sustainable. The Share 35 policies have already shown improvements in waitlist survival, and more research is needed to further evaluate post-Share 35 outcomes to analyze its impact on liver allocation and waitlist survival among ESLD patients at the highest MELD scores.
Strengths of our study include the utilization of a large transplant registry (UNOS/OPTN) that incorporates all adult LT patients in the United States from 2003 to 2013. Furthermore, while previous studies incorporated a study period that included both pre-MELD and post-MELD eras, our study focused primarily on the post-MELD era to improve consistency and generalizability of our findings. However, our study has several limitations that are typical of retrospective observational study designs, including the potential for unmeasured confounders despite multivariate logistic regression analysis. Furthermore MELD scores are dynamic and can change with disease progression or decompensation while awaiting liver transplantation. The ability to evaluate MELD score at multiple time points could provide valuable information regarding disease progression among different cohorts on the waitlist. However, UNOS/OPTN only provides MELD scores at time of registration and time of LT for analyses, thus limiting our ability to evaluate differences in MELD score progression or the reasons for decompensation leading to liver transplantation. Admission to the intensive care unit or need for mechanical ventilation among patients awaiting LT are also important factors influencing the decision for LT as well as post-LT survival [20, 21]. Furthermore, concurrent complications such as sepsis and multi-organ failure may also affect eligibility for LT among waitlisted patients. However, additional data were not readily available for inclusion in our analyses. While our study focused mainly on LT waitlist survival and odds of receiving LT, we also reported findings of post-LT survival. In addition to the variables included in our multivariate regression, specific donor factors or graft factors affecting marginality of transplanted liver may also affect post-LT survival, but detailed information about the graft was not available for inclusion in the study. In addition, the end of our study period coincided with the implementation of the Share 35 policy and thus our study could not fully evaluate the impact of this policy on our hypotheses. Despite these limitations, our study provides important data regarding waitlist outcomes among patients with Status 1A and ESLD patients with MELD >30 awaiting LT in the United States.
In conclusion, among adults in the United States awaiting liver transplantation, ESLD patients with MELD >40 have significantly higher waitlist mortality compared to Status 1A patients. Even among ESLD patients with MELD scores 36 to 40, there was a trend towards higher waitlist mortality when compared to Status 1A patients. Despite having waitlist mortality nearly double that of Status 1A patients, ESLD patients with MELD >40 had similar probability of receiving LT compared to Status 1A patients, suggesting that these patients may be under-prioritized and Status 1A patients may be over-prioritized according to current allocation policies. The recent implementation of Share 35 policies have attempted to address some of these concerns, with modifications in prioritizing livers for patients with ESLD at the highest MELD scores. The demand for liver transplantation greatly exceeds the availability of donor organs, and this imbalance is expected to become worse. While important discussions and resulting adoption of new modifications (e.g., Share 35) continue to improve the equitability of organ allocation for LT, more research is needed to improve the distribution of livers to those in most urgent need. Specifically, given the increasing evidence suggesting over-prioritization of patients with fulminant hepatic failure, more research is needed to better define a safe, effective, and equitable modification that better achieves the principles of the Final Rule.
Abbreviations
- CI:
-
Confidence interval
- ESLD:
-
End stage liver disease
- FHF:
-
Fulminant hepatic failure
- HR:
-
Hazards ratio
- INR:
-
International normalized ratio
- LT:
-
Liver transplantation
- MELD:
-
Model for end-stage liver disease
- OPTN:
-
Organ procurement and transplantation network
- OR:
-
Odds ratio
- SHR:
-
Sub-hazard ratio
- SRTR:
-
Scientific registry of transplant recipients
- UNOS:
-
Unified Network for Organ Sharing
References
Kremers Wk, Van IM, Kim WR, et al. MELD score as a predictor of pretransplant and posttransplant survival in OPTN/UNOS Status 1 patients. Hepatology (Baltimore, Md) 2004;39(3):764–769
Lee WM, Stravitz RT, Larson AM. Introduction to the revised American Association for the study of liver diseases position paper on acute liver failure 2011. Hepatology (Baltimore, Md) 2012;55(3):965–967
Schmidt LE, Larsen FS. MELD score as a predictor of liver failure and death in patients with acetaminophen-induced liver injury. Hepatology (Baltimore, Md) 2007;45(3):789–796
Shakil AO, Kramer D, Mazariegos GV, Fung JJ, Rakela J. Acute liver failure: clinical features, outcome analysis, and applicability of prognostic criteria. Liver Transpl: Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 2000;6(2):163–169
Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Annals Intern Med 2002;137(12):947–954
Murray KF, Carithers RL, Jr, AASLD. AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology (Baltimore, Md) 2005;41(6):1407–1432
Merion RM, Schaubel DE, Dykstra DM, Freeman RB, Port FK, Wolfe RA. The survival benefit of liver transplantation. Am J Transpl: Off J Am Soc Transpl Am Soc Transpl Surg 2005;5(2):307–313
Farmer DG, Anselmo DM, Ghobrial RM, et al. Liver transplantation for fulminant hepatic failure: experience with more than 200 patients over a 17-year period. Ann Surg 2003;237(5):666–675 (discussion 75-6)
O’Grady JG, Alexander GJ, Hayllar KM, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 1989;97(2):439–445
Simpson KJ, Bates CM, Henderson NC, et al. The utilization of liver transplantation in the management of acute liver failure: comparison between acetaminophen and non-acetaminophen etiologies. Liver Transpl: Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 2009;15(6):600–609
Organ Procurement and Transplantation Network. Health resources and services administration, HHS. Final rule. Fed Regist 1999;64(202):56650–56661
Dhiman RK, Jain S, Maheshwari U, et al. Early indicators of prognosis in fulminant hepatic failure: an assessment of the model for end-stage liver disease (MELD) and King’s College Hospital criteria. Liver Transpl: Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 2007;13(6):814–821
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, Ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology (Baltimore, Md) 2000;31(4):864–871
Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003;124(1):91–96
Yantorno SE, Kremers WK, Ruf AE, Trentadue JJ, Podesta LG, Villamil FG. MELD is superior to King’s college and Clichy’s criteria to assess prognosis in fulminant hepatic failure. Liver Transpl: Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 2007;13(6):822–828
Sharma P, Schaubel DE, Gong Q, Guidinger M, Merion RM. End-stage liver disease candidates at the highest model for end-stage liver disease scores have higher wait-list mortality than status-1A candidates. Hepatology (Baltimore, Md) 2012;55(1):192–198
Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015;148(3):547–555
Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2013 Annual data report: liver. Am J Transpl: Off J Am Soc Transpl Am Soc Transpl Surg 2015;15 Suppl 2:1–28
Massie AB, Chow EK, Wickliffe C E, et al. Early changes in liver distribution following implementation of Share 35. Am J Transpl: Off J Am Soc Transpl Am Soc Transpl Surg 2015;15(3):659–667
Bittermann T, Makar G, Goldberg DS. Early post-transplant survival: interaction of MELD score and hospitalization status. J Hepatol 2015;63(3):601–608
Kaltenborn A, Hartmann C, Salinas R, et al. Risk factors for short- and long-term mortality in liver transplant recipients with MELD score ≥ 30. Ann Transpl 2015;20:59–69
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was provided for this study.
Conflict of interest
Joseph Ahn, Taft Bhuket, Sasan Mosadeghi, Catherine Frenette, Benny Liu, and Robert J Wong have no relevant conflicts of interest to report.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not required given the retrospective observational study design.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ahn, J., Bhuket, T., Mosadeghi, S. et al. End-stage liver disease patients with MELD >40 have higher waitlist mortality compared to Status 1A patients. Hepatol Int 10, 838–846 (2016). https://doi.org/10.1007/s12072-016-9735-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-016-9735-4