Abstract
Shoulder dysfunction is one of the most common complications seen in patients who have undergone neck dissection surgery. The prevalence of shoulder dysfunction increases depending on the type and extent of neck dissection surgery. We aim to study the relationship between changes in intraoperative neuromonitoring (IONM) threshold during SAN stimulation, ultrasonographic measurement of muscle size and shear wave elastography with shoulder dysfunction. This is a prospective study. All patients who have undergone neck dissection in our centre have been recruited. Analysis of demographic data, IONM threshold during exposure and pre-closure, shoulder function score, neck disability index score (NDII) and ultrasonographic parameters pre-op and during follow up was done. The cohort was divided into patients who suffered from shoulder dysfunction post op (Group A) and patients with normal shoulder function post op (Group B). Statistical significance were seen in IONM threshold during SAN stimulation and Constant shoulder score for 6 months follow up in Group A. IONM threshold difference during exposure and pre-closure could effectively prognosticate shoulder dysfunction post op. A return of shoulder function could be seen in patients who suffered from shoulder dysfunction if early physiotherapy could be commenced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neck dissection is a common therapeutic procedure in head and neck surgery. As with other procedures, it is not without potential complications. Shoulder dysfunction post neck dissection has been a complication that has been consistently overlooked in favour of other more life-threatening complications such as hematoma, chyle leak and other cranial nerves palsies.
Shoulder dysfunction postoperatively significantly affects a patient’s morbidity and quality of life as simple tasks such as hair combing require intact shoulder movement. A systematic review has found that prevalence rate of shoulder pain in selective neck dissection to be ranging from 9 to 25% while reduction in shoulder range of motion was found in 5–20% of the cases depending on surgery type [1]. The incidences of shoulder dysfunction in non-selective neck dissection was found to be even higher up to 70% [2]. This prevalent complication can easily be detected by history taking and simple shoulder examination after the surgery. Early detection can lead to early physiotherapy referral that will decrease duration of morbidity and improve functional outcome.
The gold standard for prevention of shoulder dysfunction post neck dissection is accurate identification of spinal accessory nerve (SAN) via direct visualization during the surgery. Knowledge on detailed anatomy and variable course of the nerve is crucial for any surgeon performing neck dissection. In addition, adjuncts such as nerve monitor can be employed to aid identification however its usefulness could not be ascertain due to limited studies and small sample size [3,4,5]. Despite nerve preservation, it is probable that nerve injury can occur via stretching, retraction and devascularization.
Our study implores the probability of changes in intraoperative spinal accessory nerve monitoring during neck dissection as a predictor for severity of shoulder dysfunction. The objective of this prospective study is to explore the relationship between changes in intraoperative neuromonitoring (IONM) threshold and amplitude with shoulder disability post neck dissection. Shoulder dysfunction is measured subjectively and objectively using the Constant Shoulder Score and Neck Dissection Impairment Index questionnaires. In addition, we aim to study the outcome of neck dissection regarding shoulder function and its correlation with objective radiological measurements of trapezius and sternocleidomastoid (SCM) muscles using ultrasound (US) and shear wave elastography (SWE).
Methodology
This is a prospective study done in a tertiary head and neck center in Malaysia from August 2020 to February 2022. All patients who underwent neck dissection involving level IIb and/or V were recruited. Exclusion criteria includes patients who have preexisting myelopathy or neuropathy of upper limb, history of radiotherapy to the neck, previous history of surgery or trauma to shoulder and patients with any postoperative complications such as hematoma, wound breakdown, or infection.
All neck dissections are performed by two head and neck surgeons. During neck dissection, the SAN is identified and stimulated 1 cm proximal to its entrance into the SCM muscle, using NIM-Neuro 3.0 stimulator (Medtronic Surgical Tech, Jacksonville, Florida, USA). Stimulation was repeated 2 times with 3 milliampere (mA) stimuli, and the amplitudes of the electromyography (EMG) waves obtained from the trapezius muscle were recorded in millivolts (mV). The mean of these 3 amplitude values was calculated and recorded. The stimulus intensity was increased at 0.1 mA intervals starting from 0mV until a significant waveform was obtained in the trapezius muscle, then the stimulus amplitude was decreased gradually at 0.1 mA intervals to determine the minimum stimulus intensity producing a visible EMG amplitude. The mean of 3 values was also calculated to determine the minimum intensity threshold. At the end of neck dissection, the amplitude and threshold values were again determined using the same methods. Spinal accessory nerve retraction has been handled gently with a retractor and vessel loop.
Outcome measures are done using 2 validated questionnaires: the Constant Shoulder Score and Neck Dissection Impairment Index [6, 7]. These are done by a single physiotherapist throughout the study. Additionally, the anteroposterior (AP) diameter and length of SCM and trapezius muscle are measured using US and SWE by a single radiology trainee during follow-up.
Patients undergoing neck dissection are evaluated one day prior to surgery and subsequently all outcome measures are done postoperative at 72 h, 1 month and 6 months.
The Pearson chi-squared test was used to compare categorical data while the student’s t-test was used to analyze continuous variables. Statistical analysis was done using SPSS software v23.0 (SPSS Inc, Chicago, IL, USA) and statistically significant differences were defined as p > 0.05.
Results
Seventeen patients undergone neck dissection from August 2020 to February 2022. All patients undergone selective neck dissection procedure. Two patients were lost to follow-up and one patient passed away due to progression of disease. Fourteen patients completed the follow up and were included as the subjects of the analysis. Nine (64.3%) were male and 5 (35.7%) were female. The mean age is 55.4 ± 19.25 years old (range: 27–81-year-old). Demographic data, diagnosis, operation and neuromonitoring threshold readings upon encounter of SAN and pre-closure were presented in Table 1.
A loss of shoulder function assessed by the Constant score pre-op and post-op 72 h were taken as presence of shoulder dysfunction. Ten (71.4%) patients had a deterioration of interpreted Constant score post-op (Group A) while 4 (28.6%) had no shoulder dysfunction (Group B).
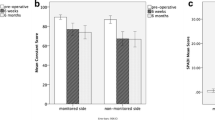
Intraoperative neuromonitoring findings, shoulder function assessment by Constant score and neck disability index score during follow-up for these 2 groups of patients were shown in Table 2. Statistical significance difference was noted during comparison of mean neuromonitoring threshold pre-closure at 1 mA and mean Constant score for 6 months follow-up. It was found that patients with shoulder dysfunction postoperatively (Group A) have difference in pre-closure threshold at 1 mA and Constant score at 6 months as compared to Constant score 72 h postop. Comparison between Constant Shoulder Score and NDII between groups during pre-operation and follow up were shown in Figs. 1 and 2. Ultrasonographic findings have not shown any statistically significant findings between either group of patients (Table 3; Figs. 3 and 4).
Discussion
Shoulder dysfunction has been known to be one of the most common complications following neck dissection. Previous literature has loosely defined shoulder dysfunction as presence of shoulder droop, presence of shoulder pain, reductions in shoulder active abduction range, reduction in active flexion range or weak shoulder shrug [1, 8]. The presence of neck dysfunction was assessed by presence of neck pain, reduced neck range of motion and limitation of neck rotation. In our study, we have decided to use the Constant score to assess the shoulder function of the patients more objectively. The score encompasses level of shoulder pain, activities of daily living, range of movement and power. The NDII was used to assess neck function and pain. We believe that our study is one of the first to employ these questionnaires for shoulder and neck assessments for patients who have undergone neck dissection.
In our cohort, 10 out of the 14 patients have experienced deterioration of shoulder function after neck dissection surgery. All these patients had undergone selective neck dissection. Studies have shown that shoulder syndrome was less in SAN sparing neck dissection as compared to radical or modified radical neck dissection surgery [1, 9]. However, most of our patients had experienced deterioration of shoulder function post SAN sparing surgery. This is in line with other studies which reported the prevalence of shoulder dysfunction post selective neck dissection ranges between 13 and 56% [9,10,11]. Some authors have attributed presence of shoulder syndrome in SAN sparing surgery was likely due to transection of SAN or strong traction during surgery [8]. The risk of shoulder dysfunction must be carefully explained to patients undergoing neck dissection procedures due to its high prevalence and incidence rate.
Neuromonitoring of the SAN has been shown to be effective, safe and useful in its identification during neck dissection [3, 12, 13]. Further study of neuromonitoring threshold and amplitude has been done in hope to be able to prognosticate shoulder function in the early post op period. In our study, there is a statistically significant difference between mean pre-closure neuromonitoring threshold between these 2 groups of patients. Recent study by Birinci et al. has showed that shoulder dysfunction do happen in SAN preserving surgery and changes on neuromonitoring findings have a positive predictive value in prognosticating post op shoulder dysfunction [14]. However, the quantitative figure which signifies significant changes between pre op and pre closure neuromonitoring threshold could not be established. In contrast, Witt et al. reported no significant electrophysiologic shift in his cohort of patients who undergone selective neck dissection surgery [8, 15].
We have found that there is no correlation between radiological findings of mid trapezius AP diameter and diameter of SCM with shoulder function. Mid trapezius AP diameter was found to reduce consistently during follow up while SCM diameter has increase during the 1st month follow up. However, these findings do not correlate with shoulder functions during follow up. We postulate that this could be due to the minute changes of diameter which does not signify significant atrophy. Furthermore, physiotherapy was started immediately in our cohort once shoulder dysfunction has been diagnosed. This findings are in contrast with other study which shown shoulder sonography to be useful in determining shoulder muscles atrophy [16]. SWE utilizes the shear wave speed to visualize tissue displacements and provide information on tissue biomechanics [17]. In our study, changes of the SWE were insignificant. We think that the SWE could not pick up changes despite the presence of shoulder dysfunction in Group A most likely due to the early post op period and the relatively intact shoulder anatomy. SWE is effective in study of elastic modulus and detecting stiffness however this technology is still in its infancy [18, 19]. A longer follow up would provide more information on whether SWE could effectively detect shoulder dysfunction. However, we could conclude that this technology could not detect changes in shoulder function primarily caused by SAN injury.
All our patients who suffered from shoulder dysfunction post op undergone early rehabilitation program. There is statistically significant difference for shoulder function between these 2 groups of patients for 6 months follow up. Fordham et al. reported a specialized rehabilitation program for patients who undergone neck dissection [20]. All patients showed improvement of shoulder function clinically and objectively using scoring systems used in this study at the end of the study.
The limitation of this study includes small patient size and short follow up duration. A longer follow up duration could potentially detect changes of muscle size and evaluate the effectiveness of early physiotherapy intervention and rehabilitative program.
Conclusion
A significant changes of SAN neuromonitoring threshold pre-op and pre-closure could be used to prognosticate shoulder dysfunction post op. There is significant difference of shoulder function at 6 months post op between patients who suffered from shoulder dysfunction detected 72 h post op and patients without shoulder dysfunction in the early post op period.
References
Gane EM, Michaleff ZA, Cottrell MA, McPhail SM, Hatton AL, Panizza BJ et al (2017) Prevalence, incidence, and risk factors for shoulder and neck dysfunction after neck dissection: a systematic review. Eur J Surg Oncol 43(7):1199–1218
Stuiver MM, van Wilgen CP, de Boer EM, de Goede CJT, Koolstra M, van Opzeeland A et al (2008) Impact of shoulder complaints after neck dissection on shoulder disability and quality of life. Otolaryngol - Head Neck Surg 139(1):32–39
Midwinter K, Willatt D (2002) Accessory nerve monitoring and stimulation during neck surgery. J Laryngol Otol 116(4):272–274
McGarvey AC, Hoffman GR, Osmotherly PG, Chiarelli PE (2014) Intra-operative monitoring of the spinal accessory nerve: a systematic review. J Laryngol Otol 128(9):746–751
Polistena A, Ranalli M, Avenia S, Lucchini R, Sanguinetti A, Galasse S et al (2021) The role of IONM in reducing the occurrence of shoulder syndrome following lateral neck dissection for thyroid cancer. J Clin Med 10(18):10
Constant CR, Murley AHG A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;no 214:160–164
Taylor RJ, Chepeha JC, Teknos TN, Bradford CR, Sharma PK, Terrell JE et al (2002) Development and validation of the neck dissection impairment index: a quality of life measure. Arch Otolaryngol - Head Neck Surg 128(1):44–49
Witt RL, Rejto L (2007) Spinal accessory nerve monitoring in selective and modified neck dissection. Laryngoscope 117(5):776–780
Leipzig B, Suen JY, English JL, Barnes J, Hooper M (1983) Functional evaluation of the spinal accessory nerve after neck dissection. Am J Surg 146(4):526–530
van Wilgen CP, Dijkstra PU, van der Laan BFAM, Plukker JTM, Roodenburg JLN (2004) Shoulder complaints after nerve sparing neck dissections. Int J Oral Maxillofac Surg 33(3):253–257
Zhang B, Tang P, zhang, Xu Z gang, Qi Y fa, Wang Xlei (2004) Functional evaluation of the selective neck dissection in patients with carcinoma of head and neck. Vol. 39, Zhonghua er bi yan hou ke za zhi. pp. 28–31
Lee C-H, Huang N-C, Chen H-C, Chen M-K (2013) Minimizing shoulder syndrome with intra-operative spinal accessory nerve monitoring for neck dissection. 33, Acta Otorhinolaryngol Ital
Palacios-García JM, Vizcarra-Melgar J, Sánchez-Gómez S (2021) Intraoperative spinal accessory nerve monitoring in neck dissections. Eur Arch Oto-Rhino-Laryngology 278(9):3579–3581
Birinci Y, Genc A, Ecevit MC, Erdag TK, Guneri EA, Oztura I et al (2014) Spinal accessory nerve monitoring and clinical outcome results of nerve-sparing neck dissections. Otolaryngol - Head Neck Surg (United States) 151(2):253–259
Witt RL, Gillis T, Pratt R (2006) Spinal accessory nerve monitoring with clinical outcome measures. Ear Nose Throat J 85(8):540–544
Huang YC, Lee YY, Tso HH, Chen PC, Chen YC, Chien CY et al (2019) The Sonography and Physical Findings on Shoulder after Selective Neck Dissection in Patients with Head and Neck Cancer: A Pilot Study. Biomed Res Int. ;2019
Babaei-Ghazani A, Majdalani C-E, Luong DH, Bertrand-Grenier A, Sobczak S (2021) Sonoelastography of the shoulder: a narrative review. Front Rehabil Sci. ;2
Lawrence RL, Ruder MC, Moutzouros V, Makhni EC, Muh SJ, Siegal D et al (2021) Ultrasound shear wave elastography and its association with rotator cuff tear characteristics. JSES Int 5(3):500–506
Bedewi MA, Kotb MA, Aldossary NM, Abodonya AM, Saleh AK, Swify SM (2021) Shear wave elastography of the radial nerve in healthy subjects. J Int Med Res. ;49(1)
Fordham B, Smith T, Lamb S, Morris A, Open SW-B (2022) U Patient and physiotherapist perceptions of the getting recovery right after Neck Dissection (GRRAND) rehabilitation intervention: a qualitative interview study. ueaeprints.uea.ac.uk
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
Amy Oon, Liew Yew Toong, Sakina Ghauth, Ng Wei Lin, Rizman contributed equally to this work. Author order was determined by lot.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The authors declare they have no financial interests. Ethical approval given by University Malaya Medical Research Ethics Committee (MREC ID no : 2020918-9080). Written informed consent has been taken from all participants of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ling, A.L., Toong, L.Y., Ghauth, S. et al. Intraoperative Spinal Accessory Nerve Monitoring During Neck Dissection Surgery as a Predictor for Shoulder Dysfunction. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04785-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12070-024-04785-7