Abstract
İnternal carotid artery (ICA) aneurysms are rare but they can cause high morbidity and mortality. Although these aneurysms are usually asymptomatic, they can reach huge sizes and compress the surrounding neurovascular structures. Patients typically present with neurologic symptoms due to cranial nerve compression. If they rupture, they can lead to massive epistaxis and autorage. In physical examination, pulsatile mass in the middle ear or nasal cavity can be seen. If there is a clinical suspicion of an ICA aneurysms, diagnostic radiological imaging should be performed before the surgical procedure or biopsy. Cerebral digital subtraction angiography (DSA) should be performed for definitive diagnosis. After diagnosis, appropriate endovascular or open intervention should be performed. In this case report, we present a 48-year-old female patient with severe epistaxis complaint due to an ICA aneurysm. This report aims to present this case and review the current literature.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Internal carotid artery (ICA) aneurysms are divided into intradural and extradural. Extradural ICA aneurysms are rare and have lower morbidity and mortality rates compared to intradural ICA aneurysms since they do not cause subarachnoid hemorrhage [1, 2]. Extradural ICA aneurysms most commonly originate from the cavernous sinus (2–9% of all ICAs). When they are located in the cavernous sinus, they can cause dysfunction of III., IV., VI. cranial nerve (ophthalmoplegia), V. cranial nerve first and second branches (forehead and facial half pain and/or hypoesthesia) and sometimes II. cranial nerve (vision impairment). If the aneurysm is completely inside the cavernous sinus, in case of rupture, a caroticocavernous fistula develops and classical findings (exophthalmos, chemosis, and murmur) occur [3]. On the other hand, petrous ICA aneurysms are extremely rare. Although these aneurysms are usually asymptomatic, they can grow to a significant size and compress the surrounding neurovascular structures. If they rupture, they can lead to massive epistaxis and otorrhagia and a mortality rate up to 30%. Currently, endovascular interventions are preferred over open surgery for treatment due to lower morbidity and mortality rates.
Case
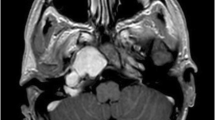
A forty-nine year-old female patient was admitted to our department with complaints of recurrent severe epistaxis and headache. There was no known additional diseases or head and neck trauma in the patient's medical records. Her vital signs were stable. On the head and neck examination of the patient, a bluish mass behind the left intact tympanic membrane was observed in the otoscopic examination, and a hemorrhagic polypoid mass in the bilateral sphenoethmoidal recess was seen on the endoscopic nasal examination. At the time of admission, labarotary parameters were: Hb 5.3 g/dL, Hct 18%; all others were normal. Patient was hospitalized and received appropriate erythrocyte suspension replacement according to the hematology department. Bleeding disorder tests showed normal coagulation factors levels. Contrast enhaced computed tomography (CT) images suggested that aneurysm at the petrous and cavernous parts of the internal carotid artery. There was ruptured aneurysm at siphon level of the internal carotid artery (Fig. 1). Later, cerebral digital subtraction angiography (DSA) was performed by the interventional radiology department doctors. During DSA, a giant aneurysm opening into ethmoidal sinuses near the distal segment of the left internal carotid artery was observed (Fig. 2). After obtaining informed consent, an endovascular stent was placed and coil embolization was performed by the inventional radiology department. The patient was discharged in good health three days alter.
In contrast-enhanced computed tomography images; areas that may be compatible with bleeding that filling the posterior ethmoid sinuses and sphenoid sinus, tubular areas suggesting aneurysm at this level, ruptured aneurysm thought to be associated with the siphon level of the internal carotid artery. A, B Axial images, C and D Coronal images, E and F Sagittal images
Discussion
The petrous and cavernous internal carotid artery aneurysms are extremely rare. They are usually seen in giant sizes. Petrous ICA aneurysms are usually fusiform, while cavernous ICA aneurysms are more saccular. Exact ethiology is unknown. Since there is no etiological factor in most cases, they are mostly considered to be congenital. Other etiological causes are trauma, mastoid surgery, middle ear infections, hypertension, hyperlipidemia, OD polycystic kidney disease, Type 4 Ehler Danlos syndrome, aortic coarctation, Marfan syndrome, NF type 1 [5]. In our patient, the etiological factor leading to ICA aneurysm was unknown.
In literature, patients present clinically at the age of 30–40 years, with a male/female ratio = 1/1 [6]. Our patient was a 48-year-old female patient.
The clinical presentation of ICA aneurysms depends on where the aneurysm extends and presses on. They mostly present with cranial nerve palsies, headaches, and epistaxis [7]. Headache and epistaxis were present in our case. The patient's cranial nerve examination was normal.
Otoscopic examination revealed a bluish mass behind the left tympanic membrane and a hemorrhagic polypoid appearance in bilateral sphenoethmoidal recess in the endoscopic nasal examination.
If there is a suspicion of an ICA aneurysm, diagnostic radiological imaging should be performed before the surgical procedure or biopsy. CT, magnetic resonance imaging (MRI), computed tomography angiography (CTA), magnetic resonance angiography (MRA) can be used for diagnosis. In the differential diagnosis; glomus jugulare, glomus tympanicum, high jugular bulb, aberrant carotid artery, and persistent stapedial artery should be considered [8]. Due to the suspicion of aneurysm in contrast-enhanced maxillofacial CT and temporal bone CT imaging in our patient, DSA was performed by the interventional radiology department and the definitive diagnosis of ICA aneurysm was made.
Currently, endovascular interventions in the treatment of ICA aneurysms have replaced open surgery because of their lower morbidity and mortality rates. Occlusion/embolization of the ipsilateral internal carotid artery or common carotid artery is performed endovascularly. In literature, some interventional radiology experts use the balloon occlusion test before permanent endovascular occlusion to check the collateral circulation of the affected side. After ICA ligation, a reperfusion phenomenon characterized by persistent epistaxis can be seen as a result of anastomoses of the ipsilateral and collateral carotid systems [9]. Our patient was modeled endovascularly with a stent under general anesthesia by the interventional radiology department, and then the aneurysm was treated with coil embolization. Before the operation, a balloon occlusion test wasn’t performed. After the endovascular intervention, the patient didn’t have any neurovascular deficits.
Conclusion
Although internal carotid artery aneurysms are uncommon, they should be considered in patients who have a history of severe epistaxis. Especially in petrous ICA aneurysms; there may be a pulsatile, bluish polyp-like mass in the middle ear on otoscopy and hemorrhagic polypoid appearance in sphenoethmoidal recess when examined through endoscopic nasal examination. If there is any suspicion of an ICA aneurysm, imaging tests should be performed before any surgical procedures or biopsies are considered. Cerebral digital subtraction angiography (DSA) is the preferred method of definitive diagnosis. After diagnosis, appropriate endovascular or open intervention should be performed without losing time. Nowadays, endovascular interventions have replaced open surgery in the treatment of ICA aneurysms because of their lower morbidity and mortality rates.
References
Halbach VV, Higashida RT, Hieshima GB (1990) Aneurysms of the petrous portion of the internal carotid artery, results of treatment with endovascular or surgical occlusion. Am J Neuroradiol 11:253–257
Kudo S, Colley DP (1983) Multiple intrapetrous aneurysms of the internal carotid artery. Am J Neuroradiol 4:1119–1121
Constantino PD, Russell E, Reisch D (1991) Ruptured petrous carotid aneurysm presenting with otorrhagia and epistaxis. Am J Otol 12:378–383
Wiebers DO (2003) International study of unruptured intracranial aneurysms investigators: unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110
Linskey ME, Sekhar LN, Hirsch W Jr, Yonas H, Horton JA (1990) Aneurysms of the intracavernous carotid artery: clinical presentation, radiographic features, and pathogenesis. Neurosurgery 26(1):71–79
Liu JK, Gottfried ON, Amini A, Couldwell WT (2004) Aneurysms of the petrous internal carotid artery: anatomy, origins, and treatment. Neurosurg Focus 17:E13
Willinsky R, Lasjaunias P, Pruvost P, Boucherat M (1987) Petrous internal carotid aneurysm causing epistaxis: balloon embolization with preservation of the parent vessel. Neuroradiology 29:570–572
Lee SH, Jang JH, Kim KH, Kim YZ (2015) Stent-assisted coil embolization of petrous ICA in a teenager with neurofibromatosis. J Cerebrovasc Endovasc Neurosurg 17:252–256
Singh H, Thomas J, Hoe WL, Sethi DS (2008) Giant petrous carotid aneurysm: persistent epistaxis despite internal carotid artery ligation. J Laryngol Otol 122:E18
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors claim no financial or non-financial conflict of interest.
Ethical Approval
No ethical committee was necessary for this case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aslan, C., Bal, K., Gur, H. et al. Aneurysm of Petrous and Cavernous Parts of the Internal Carotid Artery: A Case Report. Indian J Otolaryngol Head Neck Surg 76, 3637–3640 (2024). https://doi.org/10.1007/s12070-024-04656-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-024-04656-1