Abstract
Head and neck osteosarcoma is an uncommon yet aggressive tumor which presents therapeutic challenges to get favourable results. Surgery remained the most effective treatment modality in this entity eventhough chemoradiotherapy have been tried in various studies for better outcome but still not yet becomes the standard in the management of these cases unlike in extremity osteosarcoma. We present our experience in the management of this uncommon yet lethal malignant tumor, i.e. head and neck osteosarcoma. To study the clinicopathological and prognostic features of Osteosarcoma in head and neck subsite. Retrospective study of patients diagnosed with head and neck osteosarcoma between 2003 and 2019. Total of 25 patients were included in our study. Mean age of our population is 27.5 years with slight male predominant. Mandible is the most commonly involved site. Multimodal treatment applied with surgical resection forms the main part in the management. Median DFS and OS were 16 and 36 months respectively with 5 year overall survival of 42%. Out of the various factors studied, absence of surgery, margin positivity are the principle features affecting the prognosis. Head and neck osteosarcoma is generally a jaw bone tumor commonly occurs in young adults with poor outcome. Since there is no universal guidelines to address this uncommon tumor, multiple studies have shown various results in the management. Till date, surgery remained the curative modality with mixed response on the role of chemotherapy and radiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck osteosarcoma is a unusual primary malignant bone tumor (< 10% of all osteosarcoma) with aggressive behaviour which often requires multimodal management for better outcome [1]. It has got wide range of age distribution even though it occurs slightly at younger age than extremity variant, males are most commonly affected. Very few patients gives history of radiation exposure in the development of head and neck osteosarcoma before the diagnosis which says that radiation is one of the aetiologies explained [2]. Surgical excision forms the most important variable in the management of head and neck osteosarcoma [3]. We have reviewed 25 patients of head and neck OS in our tertiary cancer care center (Table 1).
Materials and Methods
Retrospective study of all the patients visited our head and neck OPD with the diagnosis of Osteosarcoma who are further evaluated and treated in Gujarat Cancer Research Institute, India during the period between 2013 and 2019 done after taking the ethical committee clearance.
All the patients were assessed by detailed documented clinical history and physical examination, relevant blood investigations, biopsy and imaging study. Contrast enhanced computed tomography is used to evaluate the local extent of the lesion. Treatment plan was decided on individual basis in multidisciplinary tumor board meeting (Table 2).
Results
Total 25 patients with diagnosis of head and neck osteosarcoma were further evaluated and treated in our tertiary cancer care center between 2013 and 2019 are included in our study. Gender distribution in our study shows 14 male and 11 female patients with age range from 10 to 55 years. Mean age of the study is 27.5 years.
The site of primary tumor is mandible in 18 patients, maxilla in 3 and 2 in nasal cavity, one in sphenoid sinus and infratemporal fossa each. None of the patients had previous history of radiation exposure in the past.
20 patients received surgery as the primary curative treatment out of 25 patients. 5 patients received curative chemoradiotherapy as these patients were medically unfit for surgery/unwilling for surgery. Among surgically treated patients, 6 patients received neoadjuvant chemotherapy which was decided on the basis of advanced size of the lesion with local soft tissue extent. Regimen of the same was minimum 2 cycles of cisplatin and adriamycin. Response assessment after neoadjuvant chemotherapy was done with contrast enhanced computed tomography of head and neck region.
Curative surgery was done in the form of mandibulectomy (segmental, hemi or extended) or maxillectomy. Two patients underwent craniofacial resection.
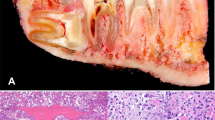
Reconstruction was done either with free fibula, locoregional flaps such as temporalis or pectoralis major myocutaneous flap. Neck dissection was selectively done in 4 patients either level 1a and 1b lymph node dissection in free flap, and supraomohyoid neck dissection in other three patients but none of the patients had nodal metastasis in final histopathological specimen. Osteoblastic variant was the most common subtype found in our study followed by chondroblastic type.
About 18 patients received adjuvant treatment which includes both chemotherapy and radiotherapy in 10 patients, only chemotherapy in 5 patients, whereas 3 patients received only radiotherapy.
Recurrence was noted in 14 patients (local—8, distant—6) out of 25 patients.
Two patients underwent surgical resection after neoadjuvant chemotherapy for local recurrences whereas all other patients of local recurrences were managed with either chemotherapy and/or radiotherapy in palliative setting. Lung, brain were the site of distant recurrences. All distant recurrences were managed with palliative chemotherapy.
Median DFS of our study was 16 months and median OS was 36 months, irrespective of the modality of the treatment. All five patients who did not underwent surgery were died and median OS was only 11 months. 2 yr survival in our study is 60%and 5 year overall survival is 42%.
Discussion
Osteosarcomas are primary malignant tumors of bone that are characterized by the production of osteoid or immature bone by the malignant cells. It is the most common primary malignant tumor of bone with usual occurrence in extremities and almost about 10 percent of cases arise in the head and neck region [4]. The median age at presentation is 36 years that is at least 10 years older than patients with non-head and neck osteosarcomas [2], although for non-head and neck osteosarcomas, there is a second peak in incidence in later adulthood that corresponds to secondary Paget disease-related osteosarcoma. Mean age of our study population is 27.5 years which is slightly younger age group than the usual presentation.
Head and neck osteosarcoma most commonly arise in the upper and lower jaws. In comparison to previous studies, our study also showed that the mandible is the most common site involved (72%) followed by maxilla [1]. The classical presentation is that of a mass or swelling in the cheek or jaw, sometimes associated with pain, and occasionally with dental complaints [5, 6]. All of our patients presented with complaints of mass, and local pain experienced by few patients. Local symptoms like diplopia, nasal discharge, epistaxis also noted in patients with paranasal sinus site as tumor. Gender distribution showed slight male predominance (M: F 1.08:1) which is similar to other previous studies [7].
Extremity osteosarcoma is ideally managed with neoadjuvant chemotherapy followed by surgery. Unlike extremity variant, head and neck subsite is usually managed by upfront surgery as shown in many previous studies. We also believe that chemotherapy in neoadjuvant setting is not beneficial in the management of head and neck osteosarcoma as shown in meta-analysis since we also did not see any advantage in 6 patients who had received neoadjuvant chemotherapy. Few authors in contrast says that neo-adjuvant chemotherapy helps by improving local control, by decreasing the incidence of lung metastases and also by prolonging the time to development of lung metastases [5, 8, 9].
The principle of surgery for head and neck OS is wide excision with adequate margins which is much more than other usual histology like squamous cell carcinoma. Adequate margin for head and neck osteosarcoma considered to be minimum of 2 cm of bony margins with soft tissue margins of 0.5 cm as the risk of local recurrences increases if margin is less than 1 cm [8, 10]. But due to the complex anatomy of the head and neck, adequate wide margins are not able to achieve in all cases [11], reflect the higher incidence of margin positivity and local recurrences in head and neck subsite osteosarcoma whereas extremity type usually display higher chance of distant recurrences [12, 13]. Margin positivity in our study group is 20% which is slightly lesser than other studies.
Lymph node involvement is very unusual in all the variants of osteosarcoma, hence routinely lymph node dissection is not required during surgery even though selective neck dissection can be done if clinically indicated [13,14,15]. Most of these tumors are high grade which often represents high local recurrence requiring adjuvant treatment like chemotherapy [16]. Low grade tumors can be managed with surgery alone if adequate margins can be achieved. Adjuvant radiotherapy is only indicated in positive margins cases which helps in decreasing the local recurrences [1, 14].
We had considered several factors to decide about adjuvant treatment like grade of the tumor, margin positivity, advanced size of the lesion (> 7 cm) and adverse histopathological features like perineural invasion [2]. Mandible site tumors have better results compared to maxilla as it is easy to get adequate anatomical margins for mandible and due to high vascularity of maxilla, they tend to have more distant metastasis [7]. Only 2 patients who underwent surgery did not receive adjuvant treatment who had no adverse features on histopathology. Similar to previous studies, our results also showed higher local recurrences than distant metastasis which were managed either with surgery if feasible or palliative chemotherapy or radiotherapy. 5 year survival of head and neck osteosarcoma cases in various studies ranges from 30 to 63%, with our study demonstrating considerable 5 year overall survival of 42% [2].
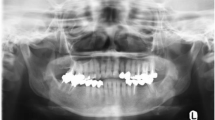
Outcome of our study design clearly demonstrated that surgery as the principle curative modality of treatment which stands tall among multimodality management of head and neck osteosarcoma [1, 2, 7, 17,18,19] as surgery with positive margins decreases the survival (5 year survival 25% vs 62%). Surgery alone or with chemotherapy has similar survival (mean DFS 44 months vs 42 months) even though few differ in this. Adjuvant treatment especially, radiotherapy has a survival advantage when it is given either alone or with chemotherapy by decreasing the local recurrence (mean DFS 58 months vs 43 months). Similar outcomes shown by various previous studies as well [1, 2, 20] (Figs. 1, 2, 3).
Conclusion
Head and neck osteosarcoma, in our experience primarily affecting the jaw bone which has got aggressive clinicopathological features. Surgical wide excision played a pivotal role in the management of these cases. Adjuvant treatment like chemotherapy and/or radiotherapy is needed as surgically free margins are difficult to achieve due to complex anatomy of the head and neck with preservation of aesthetic and functional outcome. Among the various factors studied for the prognosis, nonsurgical therapy as a primary modality of treatment and margin positivity affected the survival (Fig. 4).
References
Guadagnolo BA, Zagars GK, Raymond AK, Benjamin RS, Sturgis EM (2009) Osteosarcoma of the jaw/craniofacial region: outcomes after multimodality treatment. Cancer 115(14):3262–3270. https://doi.org/10.1002/cncr.24297
Krishnamurthy A, Palaniappan R (2018) Osteosarcomas of the head and neck region: a case series with a review of literature. J Maxillofac Oral Surg 17(1):38–43. https://doi.org/10.1007/s12663-017-1017-8
Mendenhall WM, Fernandes R, Werning JW, Vaysberg M, Malyapa RS, Mendenhall NP (2011) Head and neck osteosarcoma. Am J Otolaryngol 32(6):597–600. https://doi.org/10.1016/j.amjoto.2010.09.002
Gadwal SR, Gannon FH, Fanburg-Smith JC, Becoskie EM, Thompson LD (2001) Primary osteosarcoma of the head and neck in pediatric patients: a clinicopathologic study of 22 cases with a review of the literature. Cancer 91(3):598–605
Nissanka EH, Amaratunge EA, Tilakaratne WM (2007) Clinicopathological analysis of osteosarcoma of jaw bones. Oral Dis 13(1):82–87. https://doi.org/10.1111/j.1601-0825.2006.01251.x
Bennett JH, Thomas G, Evans AW, Speight PM (2000) Osteosarcoma of the jaws: a 30-year retrospective review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90(3):323–332. https://doi.org/10.1067/moe.2000.108274
Granowski-LeCornu M, Chuang SK, Kaban LB, August M (2011) Osteosarcoma of the jaws: factors influencing prognosis. J Oral Maxillofac Surg 69(9):2368–2375. https://doi.org/10.1016/j.joms.2010.10.023
Kimura Y, Tomihara K, Tachinami H, Imaue S, Nakamori K, Fujiwara K, Suzuki K, Yasuda T, Miwa S, Nakayama E, Noguchi M (2017) Conventional osteosarcoma of the mandible successfully treated with radical surgery and adjuvant chemotherapy after responding poorly to neoadjuvant chemotherapy: a case report. J Med Case Rep 11(1):210. https://doi.org/10.1186/s13256-017-1386-0
Patel SG, Meyers P, Huvos AG, Wolden S, Singh B, Shaha AR, Boyle JO, Pfister D, Shah JP, Kraus DH (2002) Improved outcomes in patients with osteogenic sarcoma of the head and neck. Cancer 95(7):1495–1503. https://doi.org/10.1002/cncr.10849
Thariat J, Julieron M, Brouchet A, Italiano A, Schouman T, Marcy PY, Odin G, Lacout A, Dassonville O, Peyrottes-Birstwisles I, Miller R, Thyss A, Isambert N (2012) Osteosarcomas of the mandible: are they different from other tumor sites? Crit Rev Oncol Hematol 82(3):280–295. https://doi.org/10.1016/j.critrevonc.2011.07.001
Cassoni A, Brauner E, Pucci R, Terenzi V, Mangini N, Battisti A, Della Monaca M, Ciolfi A, Laudoni F, Di Carlo S, Valentini V (2020) Head and neck osteosarcoma-the ongoing challenge about reconstruction and dental rehabilitation. Cancers (Basel) 12(7):1948. https://doi.org/10.3390/cancers12071948
Jasnau S, Meyer U, Potratz J, Jundt G, Kevric M, Joos UK, Jürgens H, Bielack SS, Cooperative Osteosarcoma Study Group COSS (2008) Craniofacial osteosarcoma experience of the cooperative German-Austrian-Swiss osteosarcoma study group. Oral Oncol 44(3):286–294. https://doi.org/10.1016/j.oraloncology.2007.03.001
Ferrari D, Codecà C, Battisti N, Broggio F, Crepaldi F, Violati M, Bertuzzi C, Dottorini L, Caldiera S, Luciani A, Moneghini L, Biglioli F, Cassinelli G, Morabito A, Foa P (2014) Multimodality treatment of osteosarcoma of the jaw: a single institution experience. Med Oncol 31(9):171. https://doi.org/10.1007/s12032-014-0171-9
Sturgis EM, Potter BO (2003) Sarcomas of the head and neck region. Curr Opin Oncol 15(3):239–252. https://doi.org/10.1097/00001622-200305000-00011
Perspective chapter: osteosarcomas of the head and neck. https://doi.org/10.5772/intechopen.107456
Smith RB, Apostolakis LW, Karnell LH, Koch BB, Robinson RA, Zhen W, Menck HR, Hoffman HT (2003) National Cancer Data Base report on osteosarcoma of the head and neck. Cancer 98(8):1670–1680. https://doi.org/10.1002/cncr.11716
Smeele LE, van der Wal JE, van Diest PJ, van der Waal I, Snow GB (1994) Radical surgical treatment in craniofacial osteosarcoma gives excellent survival. A retrospective cohort study of 14 patients. Eur J Cancer B Oral Oncol 30B(6):374–376. https://doi.org/10.1016/0964-1955(94)90014-0
Kassir RR, Rassekh CH, Kinsella JB, Segas J, Carrau RL, Hokanson JA (1997) Osteosarcoma of the head and neck: meta-analysis of nonrandomized studies. Laryngoscope 107(1):56–61. https://doi.org/10.1097/00005537-199701000-00013
Bertoni F, Dallera P, Bacchini P, Marchetti C, Campobassi A (1991) The Istituto Rizzoli-Beretta experience with osteosarcoma of the jaw. Cancer 68(7):1555–1563. https://doi.org/10.1002/1097-0142(19911001)68:7%3c1555::aid-cncr2820680717%3e3.0.co;2-0
Chen Y, Shen Q, Gokavarapu S, Lin C, Yahiya CW, Chauhan S, Liu Z, Ji T, Tian Z (2016) Osteosarcoma of head and neck: a retrospective study on prognostic factors from a single institute database. Oral Oncol 58:1–7. https://doi.org/10.1016/j.oraloncology.2016.04.008
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology—PR. Formal analysis and investigation—KSS, RD, AP, ST. Writing—original draft preparation—KSS. Writing—review and editing—PR, VW, SP. Supervision—SP, SP, MS.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no financial or non-financial interests to disclose.
Ethical Approval and Consent
All the research work done following the institutional ethical committee clearance guidelines and consent from all the patients was taken for institutional research purpose.
Informed Consent
For institutional research and publication purposes, all patients were informed about the usage of their data and consent was taken for the same.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sandeep, K.S., Rathod, P., Dalvi, R. et al. Osteosarcoma of Head and Neck Region: Tertiary Cancer Care Center Experience. Indian J Otolaryngol Head Neck Surg 76, 581–586 (2024). https://doi.org/10.1007/s12070-023-04216-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04216-z