Abstract
To know the normative ranges of VEMP response metrics in healthy young adults. To know the pathological cutoff of VEMP metrics in unilateral vestibular loss patients. To compare our VEMP metrics with the normative values of other studies from the western world. Prospective cross-sectional study. Tertiary care audiovestibular laboratory. 30 healthy subjects and 15 cases with a unilateral complete compensated loss. Various VEMP parameters-p1 latency, n1 latency, p1-n1 amplitude and Interaural asymmetry ratio (IAR) were entered into databases and analyzed. We compared our parameters with the most cited scientific data on VEMP available in the PubMed database, and we analyzed the results. 90% of controls and 80% of cases got VEMP responses at 95 dB HL threshold, 500 Hz with subject/patient placed in sitting upright with head turned to opposite side position. The normative data of VEMP response metrics in young adults for p1, n1 latencies, p1-n1 amplitude, and IAR are 13 ± 2 ms, 21 ± 2 ms, 91 ± 33 uV, and 9.25 ± 7.3, respectively. As the VEMP test has 100% sensitivity and 100% (95% CI 87–100%) negative predictive value in detecting the saccular dysfunction, we recommend the VEMP test as a mandatory tool in the vestibular test battery. There is no statistically significant difference in various VEMP parameters between the control and normal sides of the case group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular-evoked myogenic potential (VEMP) is a test of the integrity of the sacculo-collic reflex. Vestibular afferents with regular spontaneous activity are unresponsive to sound, whereas a sizable fraction of vestibular afferents with irregular activity is acoustically responsive [1]. Sufficiently high-intensity sounds can stimulate Saccule and its afferent fibres. The Saccular afferents project to the lateral portions of vestibular nuclei, which gives vestibulospinal tracts. The reflexive response to such auditory stimuli would be the relaxation of flexor muscles. These transient relaxation potentials recorded in electromyography of a tonically contracted flexor muscle, preferably sternocleidomastoid, are called VEMPs. Because they arise from Saccule, the absence of cervical VEMP can be considered an abnormality in the function of the Saccule and the saccular afferent pathways.
For the last decade, extensive work is being done on VEMP, site of origin, afferent pathways [2,3,4], spinal and central connections, its role in human vestibular physiology, and clinical importance. Many centres worldwide have performed VEMPs in the normal population [5, 6] with different intensity(thresholds) and duration of auditory stimuli and the patient's position. However, very few scientific papers [7] are available explaining the standard protocol for conducting the test procedure, the normative ranges of latencies, and amplitudes in the Indian population. The present study is undertaken to address grey areas in the VEMP, standardize the test protocol, and know the normative ranges of various VEMP metrics in normal subjects. We also compared the VEMP metrics between normal subjects and patients with unilateral complete compensated vestibular loss patients.
Objectives
-
1.
To know the normative ranges of VEMP response metrics in healthy young adults.
-
2.
To know the pathological cutoff of VEMP metrics in unilateral vestibular loss patients.
-
3.
To compare our VEMP metrics with the normative values of other studies from the western world.
Materials and Methods
Study Design
Prospective Cross-Sectional study incorporating normal controls and cases with unilateral compensated complete vestibular loss.
Ethical Considerations
Institutional Ethical board approval was obtained with minutes no: IESC/T-308/2011. All subjects had informed consent of the study aims and intent and consented to participation.
Study Site
Tertiary care Academic Otolaryngology and Audiology facility. Institutional vestibular physiology laboratory incorporating Vestibular Evoked Myogenic Potential (VEMP) equipment. (VEMP—NEUROSOFT with audioneuro.net version 7.0 software).
Participants
Control Group
Thirty healthy young volunteer adults between 20 and 45 years of age with no previous evidence of otologic or neurologic illness, systemic illness, or ototoxic drug intake, and a normal pure tone audiogram. Any subsequent detection of vestibular abnormalities at a comprehensive video-nystagmic-graphic (VNG) evaluation conducted concurrently with otolith function testing was an excluding criteria—but was not noted in any.
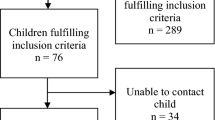
Case Group
Fifteen cases with complete unilateral cochleovestibular loss consequent to previous surgery (15 unilateral retrosigmoid vestibular schwannoma excision and one unilateral total labyrinthectomy). The period from surgery to study inclusion ranged from 6 to 24 months. All cases were symptom-free at study inclusion with no significant neurological sequelae (excepting HB Grade II-V lower motor neuron facial palsy in post-surgical vestibular schwannoma patients). The complete cochleovestibular loss was further confirmed by the absence of responses on ipsilateral pure tone audiogram and caloric testing. No subject had any current symptoms relating to vertigo or imbalance, thus indicating complete clinical compensation of the vestibular deficit.
Methodology
In the preparatory phase of this study, we performed a comprehensive vestibular evaluation using VNG and VEMP test in ten young, healthy volunteers between 20 and 45 years. We also took eight patients who underwent complete excision of the vestibular schwannoma by retromastoid suboccipital craniotomy. These patients had unilateral profound hearing loss and absent caloric on the side of surgery. VEMP test is performed in supine with head raised position for a duration of 200 stimuli, 0.1 ms each. As most of the controls and cases were unable to complete the test procedure, we changed the test position to sitting with the head turned to the opposite side.
We have conducted the VEMP test in all 30 controls and 15 cases in the experimental phase with a standard protocol. We compared our testing protocol and VEMP metrics with the most cited scientific papers from PubMed in the last two decades and analyzed the data.
Test Procedure
We took adequate precautions to maintain absolute silence and switch off all the electronic devices that can interfere with the responses. The subject sits in an erect chair and turns their head to the opposite side to contract the sternocleidomastoid being tested. We used appropriate manufacturer software for effective spectral analysis, biofeedback, and noise filtering of the EMG signal (audioneuro.net version 7.0 provided by NEUROSOFT RUSSIA). We placed the positive electrode at the sternal notch; the negative electrode at the upper third of the sternocleidomastoid muscle. The reference electrode is placed on the forehead (Fig. 1). The air conducted alternating 500 Hz Short tone bursts at 95 dB nHL (0.1 ms, 200 bursts) were delivered by a snugly fitting headphone and Sternomastoid EMG recorded by surface electrodes.
The test was repeated twice on both sides to look for a better superimposition of the waveforms. The latencies of p1, n1 were measured. The amplitude of the waveform obtained by the difference between the p1 and n1 (p1-n1) (Fig. 2). Interaural amplitude asymmetry ratio(IAR) obtained by dividing the difference of the p1-n1 amplitude by the sum of the p1-n1 amplitude of both ears.
Statistical Analysis
The descriptive statistics, quartile coefficient of dispersion of upper and lower limits of various VEMP response metrics, positive and negative predictive values, sensitivity, and specificity were calculated using SPSS software (SPSS Inc., Chicago, USA) version 19.0.0.2. Independent student t-test and Mann Whitney U tests are used to testing the statistical significance between the controls (54 ears) and normal sides of the case group (12 ears) for various VEMP parameters.
Our VEMP response metrics were compared with most cited scientific articles in PubMed.We calculated the Quartile coefficient of dispersion (COD) for mean values of various VEMP metrics from the cited scientific papers and compared it with our study.
Results
The VEMP test is successfully conducted in all thirty subjects and fifteen cases. We got satisfactory waveforms in 27/30 (90%)subjects. There was no significant difference between male–female and right-left ears in controls. In the case group, VEMP responses are absent on the side of ablation in all 15 patients (100%). The VEMP testing of the contralateral (presumably normal) side indicated 3/15 (20%) absent responses. The mean, median of p1, n1 latencies, mean amplitude (p1-n1) and mean interaural amplitude asymmetry ratio (IAR) in both control and case groups were illustrated in Table 1. There is no statistically significant difference between the control and normal sides of the case group for various VEMP metrics with p > 0.05 (Mann Whitney U test, p < 0.05 is considered significant).
The sensitivity (95% CI) and specificity (95% CI) of VEMP testing in detecting saccular dysfunction is noted at 100% (78.2% -100%) and 90% (73.5%-97.9%) respectively. Table 2 enlists the 95% Confidence intervals for PPV (positive predictive value), NPV (negative predictive value), sensitivity and specificity for VEMP test.
Our VEMP response metrics were compared with most cited scientific articles in PubMed (Table 3). Figures 3,4,5 and 6 depict the comparisons of p1,n1 latencies, p1-n1 interpeak amplitudes, and interaural amplitude asymmetry ratios(IAR). The quartile co-efficient of dispersion for upper and lower limits of all VEMP response metrics were calculated and shown in Table 4.
Discussion
One can test the human vestibular function by examination of vestibulo-ocular, vestibulospinal, and vestibulocollic reflexes. The vestibulocollic reflex helps stabilize the head's position during movements of the body [8]. Sacculocollic reflex depends on the inhibitory projections of the Saccule to the spinal accessory nucleus, thereby to ipsilateral sternomastoid muscles via inhibitory neurons and medial vestibulospinal tract [9]. The influence of other areas and projections in the brainstem and other higher centres on sacculocollic reflex is poorly understood. However, some animal models have proven the projections of vestibular nuclei to the cerebellum, external cuneate nucleus, cochlear nucleus, and interstitial nucleus of the eighth nerve [2].
The present study is undertaken to know the normative ranges in healthy young adults (27 ± 2.5 years) without any prior history of vestibular dysfunction. We also checked the VEMP responses in patients (mean age of 30 ± 3.2 years) with the unilateral complete compensated vestibular loss on the normal and lesioned sides.
Ergonomics Related to the Testing Procedure
Maintaining the optimal contraction of sternomastoid muscle throughout the test procedure is paramount important for obtaining good responses. In the present study's preparatory phase, 4/10 controls and 8/8 cases could not complete the procedure supine with head raised in pitch plane (Fig. 7). Hence, as an alternate method to neck flexion, we attempted to do the test sitting upright with the head turned to the opposite side. Though many workers suggested VEMP in sitting position [6, 10,11,12,13], other centres also adopted supine with head rise with consistent results[14, 15]. Kim et al. [16], Isaradisaikul et al. [10] recommended head turned to the opposite side in a seated position as the best test position due to good compliance and consistent level of sternomastoid contraction.
We recommend the positive/active/noninverting electrode placement on the sternal notch. Negative/inverting electrode placement on the upper one-third of the sternomastoid muscle showed a larger amplitude than any other part of the muscle [17]. Placing the electrode at a constant location on the muscle yielded more consistent responses between the sides and also between the subjects [10].
VEMP Settings
The recommended protocol that yielded more consistent results in this study was using air conduction short tone bursts of 500 Hz, 95 nHL stimulation intensity,0.1 ms, 200 stimuli monaurally when the subject was sitting upright with the neck rotated to the opposite side to contract the ipsilateral sternomastoid muscle. Table 3 depicts various other protocols with a difference in the test position, type of stimulus, intensity threshold. Because acoustically responsive vestibular fibres are more responsive between 500 and 1000 Hz [1], optimal stimulus frequencies for VEMP testing were in this range. However, Todd et al. [18] noticed a maximum response at 300–350 Hz. In the present study's preparatory phase, authors found the use of rarefaction clicks had yielded a scattered response, and poor compliance in both controls and patients as the stimulation intensity required for rarefaction clicks was higher than with STBs, as was noticed by other authors [6, 19]. We recommend Tone bursts at 500 Hz with a stimulation intensity of 95dBnHL (115dBSPL) as an ideal setting for obtaining VEMP responses [20, 21].
VEMP Response Metrics
In the present study, the VEMP response rate for the control and case group is 90% (27/30) and 80% (12/15) (the contralateral normal side in the case group) respectively at the stimulus threshold of 95dBnHL at 500 Hz. Increasing the threshold to 100dBnHL has not evoked responses in the rest of the controls and cases. (3 controls and 3 cases). The response rates of 97%(at 115dbSPL) [11] and 100%(at 113dBSPL) [13] were reported using short tone bursts. There were reports with 95 dBnHL click stimulation, the response rates of 90% (in older people) and 97% (in younger people) [22]. Some studies have considered VEMP thresholds as the only clinically important parameter [5]. But the variation in the thresholds between the studies is more, and thresholds depend on the test position and muscle contractility [10]. We opine VEMP thresholds alone should not be considered in interpreting the results. In the present study, the authors noted that absent responses in the control group are probably thinner sternomastoid, bulky neck [7], and repeated attempts in performing the procedure, which could cause fatigue of the muscle. All 15 patients in our study have absent responses on the side of vestibular ablation (sensitivity 100% in detecting the saccular dysfunction). Three of the fifteen cases had no appreciable responses on the normal side (intact vestibular function) in our study. The reason for the absence of responses on the normal side is not known. Poor compliance, inability to complete the test procedure by keeping the muscle in contracted state throughout was the noted cause in the case group. Studies have noted the absent responses on the normal side of early Meniere's disease were pointed to binaural interactions of otolith-cervical reflex arc [21]. The saccular central connections need to be elaborately studied to know the exact reason for absent responses on the normal sides in the case group.
There was no statistically significant difference between the p1,n1 latencies,p1-n1 amplitudes between the normal sides of controls and cases (Table 1). There was no correlation between p1 and n1 latencies in our study; however, few workers noted the more prolonged the p1 latency, the longer n1 latency was noted in some studies [10, 23]. The quartile coefficient of dispersion of the upper and lower limits of p1, n1 latencies across the literature was less variable than p1-n1 amplitudes and IAR. As p1-n1 amplitude depends on the muscle's contractility, its negative correlation with age [6, 24], and as the range of amplitude is wide across the literature, its clinical significance is questionable. Our study's mean IAR was 9.25 ± 7.3, consistent with the literature (Table 3). Some authors consider IAR more than 33% as abnormal. IAR may increase when subjects are old or very young and when the test procedure time is delayed due to muscle fatigue [7]. The clinical application of the VEMP in the literature helps diagnose vestibular neuritis, Meniere's disease, Vestibular Migraine, the nerve of origin of vestibular schwannomas, monitoring the efficacy of intratympanic gentamycin therapy, superior canal dehiscence [25]. However, no particular VEMP parameter reliably guides us towards the diagnosis of any of these pathologies. Sequential testing in a specific patient may nevertheless help assess the response to treatment.
The VEMP parameters studied in the present study are p1, n1 latency, p1-n1 interpeak amplitude in both control and case groups. Interaural asymmetry ratio (IAR) in the control group only as one side responses are absent in the case group. Though various studies quote the usefulness of VEMP in peripheral and central vestibular pathologies, the VEMP test as a single stand-alone diagnostic test should not be considered.
Conclusions
The normative data of VEMP response metrics in young adults for p1, n1 latencies, p1-n1 amplitude, and IAR are 13 ± 2 ms, 21 ± 2 ms, 91 ± 33 uV, and 9.25 ± 7.3, respectively. VEMP test's sensitivity in detecting the saccular dysfunction in the present study is 100% ( 95% CI 78.2- 100%). The normal sides of patients with unilateral complete compensated vestibular loss showed a similar range of VEMP response metrics as controls (p > 0.05). One has to customize the protocols to evoke VEMP responses in individual clinic and case scenario. The subject sitting upright with the neck turned to the opposite side has given the best evoked responses in the present study. The authors support using VEMP in standard vestibular test battery and not as a replacement for conventional testing. As the sensitivity of VEMP in diagnosing saccular dysfunction is 100%, when performed along with another strip of vestibular investigation, it could point us towards pathologies of otolith (saccular) origin or pathologies involving otolith organs. The absence of VEMP responses on the intact vestibular function in the case group is unknown and cannot be explained by current knowledge. Further studies are required to know the higher saccular connections and binaural interactions.
References
McCue MP, Guinan JJ (1997) Sound-evoked activity in primary afferent neurons of a mammalian vestibular system. Am J Otol 18:355–360
Newlands SD, Vrabec JT, Purcell IM, Stewart CM, Zimmerman BE, Perachio AA (2003) Central projections of the saccular and utricular nerves in macaques. J Comp Neurol 466:31–47
Uchino Y, Sato H, Sasaki M, Imagawa M, Ikegami H, Isu N et al (1997) Sacculocollic reflex arcs in cats. J Neurophysiol 77:3003–3012
Uchino Y (1997) Connections between otolith receptors and neck motoneurons. Acta Oto-Laryngol Suppl 528:49–51
Blakley BW, Wong V (2015) Normal values for cervical Vestibular-Evoked Myogenic potentials. Otol Neurotol 36:1069–1073
Basta D, Todt I, Ernst A (2005) Normative data for P1/N1-latencies of vestibular evoked myogenic potentials induced by air- or bone-conducted tone bursts. Clin Neurophysiol 1(116):2216–2219
Khan FK, Balraj A, Lepcha A (2014) Normative data for vestibular evoked myogenic potential in different age groups among a heterogeneous indian population. Indian J Otolaryngol Head Neck Surg 66:149–154
Peterson BW, Bilotto G, Goldberg J, Wilson VJ (1981) Dynamics of vestibulo-ocular, vestibulocollic, and cervicocollic reflexes. Ann N Y Acad Sci 374:395–402
Wilson VJ, Schor RH (1999) The neural substrate of the vestibulocollic reflex. Exp Brain Res 3(129):0483–0493
Isaradisaikul S, Navacharoen N, Hanprasertpong C, Kangsanarak J (2012) Cervical Vestibular-Evoked Myogenic Potentials: norms and protocols. Int J otolaryngol [Internet]. [cited 2020 Aug 27];2012. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3332197/.
Janky KL, Shepard N (2009) Vestibular Evoked Myogenic potential (VEMP) testing: normative threshold response curves and effects of age. J Am Acad Audiol 20:514–522
Ochi K, Ohashi T, Nishino H (2001) Variance of Vestibular-Evoked Myogenic potentials. Laryngoscope 111:522–527
Maes L, Vinck BM, De Vel E, D’haenens W, Bockstael A, Keppler H et al (2009) The vestibular evoked myogenic potential: a test-retest reliability study. Clin Neurophysiol Off J Int Fed Clin Neurophysiol 120:594–600
Wu H-J, Shiao A-S, Yang Y-L, Lee G-S (2007) Comparison of short tone burst-evoked and click-evoked vestibular myogenic potentials in healthy individuals. J Chin Med Assoc 70:159–163
Kelsch TA, Schaefer LA, Esquivel CR (2006) Vestibular Evoked Myogenic potentials in young children: test parameters and normative data. Laryngoscope 116:895–900
Kim JH, Park JM, Yong SY, Kim JH, Kim H, Park S-Y (2014) Difference of diagnostic rates and analytical methods in the test positions of vestibular evoked Myogenic potentials. Ann Rehabil Med 38:226–233
Sheykholeslami K, Murofushi T, Kaga K (2001) The effect of sternocleidomastoid electrode location on vestibular evoked myogenic potential. Auris Nasus Larynx 28:41–43
Todd NPM, Cody FWJ, Banks JR (2000) A saccular origin of frequency tuning in myogenic vestibular evoked potentials?: implications for human responses to loud sounds. Hear Res 1(141):180–188
Akin FW, Murnane OD (2001) Vestibular evoked myogenic potentials: preliminary report. J Am Acad Audiol 12:445–452
Young Y-H (2006) Vestibular evoked myogenic potentials: optimal stimulation and clinical application. J Biomed Sci 13:745–751
Rauch SD, Zhou G, Kujawa SG, Guinan JJ, Herrmann BS (2004) Vestibular evoked myogenic potentials show altered tuning in patients with Ménière’s disease. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol 25:333–338
Su H-C, Huang T-W, Young Y-H, Cheng P-W (2004) Aging effect on vestibular evoked myogenic potential. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol 25:977–980
Isaradisaikul S, Strong DA, Moushey JM, Gabbard SA, Ackley SR, Jenkins HA (2008) Reliability of Vestibular evoked Myogenic potentials in healthy subjects. Otol Neurotol 29:542–544
Lee SK, Cha CI, Jung TS, Park DC, Yeo SG (2008) Age-related differences in parameters of vestibular evoked myogenic potentials. Acta Otolaryngol (Stockh) 128:66–72
Welgampola MS, Colebatch JG (2005) Characteristics and clinical applications of vestibular-evoked myogenic potentials. Neurology 24(64):1682–1688
Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, L., Kairo, A. & Thakar, A. Normative and Pathological Ranges of Cervical Vestibular Evoked Myogenic Potentials in Normal Subjects and Patients with Complete Compensated Unilateral Vestibular Loss: A Cross Sectional Study. Indian J Otolaryngol Head Neck Surg 74 (Suppl 3), 4020–4027 (2022). https://doi.org/10.1007/s12070-021-02723-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02723-5