Abstract
Astrocytes are functionally diverse glial cells that maintain blood-brain barrier (BBB) integrity, provide metabolic and trophic support, and react to pathogens or harmful stimuli through inflammatory response. Impairment of astrocyte functions has been implicated in hepatic encephalopathy (HE), a neurological complication associated with hyperammonemia. Although hyperammonemia is more common in adults, ammonia gliotoxicity has been mainly studied in cultured astrocytes derived from neonate animals. However, these cells can sense and respond to stimuli in different ways from astrocytes obtained from adult animals. Thus, the aim of this study was to investigate the direct effects of ammonia on astrocyte cultures obtained from adult rats compared with those obtained from neonate rats. Our main findings pointed that ammonia increased the gene expression of proteins associated with BBB permeability, in addition to cause an inflammatory response and decrease the release of trophic factors, which were dependent on p38 mitogen-activated protein kinase (p38 MAPK)/nuclear factor κB (NFκB) pathways and aquaporin 4, in both neonatal and mature astrocytes. Considering the age, mature astrocytes presented an overall increase of the expression of inflammatory signaling components and a decrease of the expression of cytoprotective pathways, compared with neonatal astrocytes. Importantly, ammonia exposure in mature astrocytes potentiated the expression of the senescence marker p21, inflammatory response, activation of p38 MAPK/NFκB pathways, and the decrease of cytoprotective pathways. In this regard, ammonia can trigger and/or accelerate the inflammaging of mature astrocytes, a phenomenon characterized by an age-related chronic and low-grade inflammation, which may be implicated in HE neurological symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Astrocytes are multifunctional glial cells that play essential roles in central nervous system (CNS) homeostasis. They maintain a close interaction with the synapses and cerebral vessels, thus regulating both microenvironments, neural metabolism, and blood-brain barrier (BBB) [1,2,3]. As active communicating cells, astrocytes secrete several trophic molecules, including vascular endothelial growth factor (VEGF), glial-derived neurotrophic factor (GDNF), and brain-derived neurotrophic factor (BDNF) [3, 4]. During brain injuries, astrocytes can become activated and fulfill an important function in inflammatory response and immunity, by releasing inflammatory mediators such as cytokines, chemokines, prostaglandins, and nitric oxide [5, 6]. Moreover, the expression of pattern recognition receptors, as toll-like receptors (TLRs), allows astrocytes to respond to different stimuli [7]. As a consequence, p38 mitogen-activated protein kinase (p38 MAPK), nuclear factor κB (NFκB), nuclear factor erythroid-derived 2-like 2 (Nrf2), heme oxygenase-1 (HO-1), phosphatidylinositide 3-kinase (PI3K), and other signaling pathways are triggered, driving either inflammation or cellular protection [7,8,9,10].
Ammonia is a metabolite produced by several reactions throughout the body and is finally metabolized in the liver by urea cycle. Pathological increase in circulating ammonia levels occurs mainly in adults as a consequence of acquired liver diseases, but it can also have congenital causes (i.e., inborn errors of urea cycle) in infants and children [11, 12]. Hyperammonemia interferes profoundly with brain metabolism, a condition referred as hepatic encephalopathy (HE) [13]. Within the CNS, ammonia is detoxified mainly by glutamine synthetase (GS), a specific astrocytic enzyme in the brain [14]. However, hyperammonemia conditions might exceed astrocytic metabolic capacity and cause several toxic effects to the brain, including inflammatory response, oxidative stress, and cerebral edema [15,16,17,18]. Particularly this last effect can be associated with changes in aquaporin 4 (AQP4), a water channel protein expressed by astrocytes [19, 20]. Additionally, it has been reported that ammonia also induces astrocyte senescence, associated with increased p21 expression [21].
Although hyperammonemic disorders can affect neonatal and adult brain, ammonia toxicity has been studied in primary astrocyte cultures derived from neonate rodents [18, 22]. It has been demonstrated that astrocytes from immature brain present different metabolic activities, as well as can sense and respond to stimuli in different ways from mature cells, obtained from adult animals [23,24,25,26,27]. The diversity of protective stimuli and/or challenges experienced by an animal (i.e., immune and stressful) can leave brain marks, and supposedly influence astrocytic responses in later ages [28,29,30,31]. In line with this, the aim of this study was to investigate the direct effects of ammonia on primary astrocytes obtained from adult rats compared with those obtained from neonate rats, referred to herein after as mature and neonatal cultures, respectively. We considered important functional parameters of astrocytes, in addition to evaluate the roles of AQP4 and p38 MAPK in the mechanisms underlying ammonia effects. The main findings of our study showed that ammonia can potentiate intrinsic age-related inflammatory and senescence markers in mature astrocytes. In other words, in adult brain, ammonia can trigger and/or accelerate glial-inflammaging, a phenomenon characterized by an age-related chronic and low-grade inflammation potentially associated with diseases [32,33,34].
Materials and Methods
Reagents
Dulbecco’s modified Eagle’s medium/F12 (DMEM/F12) and other materials for cell culture, TRIzol reagent, and ELISA kits for interleukin-1β (IL-1β), interleukin-6 (IL-6), interleukin-10 (IL-10), NFκB p65, and BDNF were purchased from Gibco/Invitrogen (Carlsbad, CA, USA). High Capacity cDNA Reverse Transcription kit, Taqman Universal PCR Master Mix, and TaqMan® Assays were purchased from Applied Biosystems (Foster City, CA, USA). 5-Diphenyltetrazolium bromide (MTT) and phospho-p38 MAPK kit were obtained from Sigma-Aldrich (St. Louis, MO, USA). GDNF ELISA kit was obtained from R&D Systems (Minneapolis, MN, USA) and ELISA kit for tumor necrosis factor-α (TNF-α) from PeproTech (Rocky Hill, NJ, USA). Anti-AQP4, anti-HO-1, and anti-phospho-PI3K p85 (Tyr458)/p55 (Tyr199) were purchased from Millipore (Burlington, MA, USA), Santa Cruz Biotechnology (Santa Cruz, CA, USA), and Cell Signaling Technology (Danvers, MA, USA), respectively, and HRP-conjugated β-actin antibody was from Proteintech (Rosemont, IL, USA). All other chemicals were purchased from common commercial suppliers.
Animals
Male Wistar rats (1–2 and 90 days old) were obtained from our breeding colony (Department of Biochemistry, UFRGS, Porto Alegre, Brazil), maintained under controlled environment (12 h light/12 h dark cycle; 22 ± 1 °C; ad libitum access to food and water). All animal experiments were performed in accordance with the National Institute of Health (NIH) Guide for the Care and Use of Laboratory Animals and Brazilian Society for Neuroscience and Behavior recommendations for animal care. The experimental protocols were approved by the Federal University of Rio Grande do Sul Animal Care and Use Committee (process number 21215).
Neonatal and Mature Astrocyte Cultures
Neonate (1–2 days old) and adult (90 days old) Wistar rats had their cortices aseptically dissected from cerebral hemispheres, followed by meninges removal. The tissues were digested in Hank’s balanced salt solution (HBSS) containing 0.003% DNase using trypsin (0.05%) and papain (40 U/mL), as previously described [27, 35]. After mechanical dissociation and centrifugation, the cells were resuspended in DMEM/F12 (10% fetal bovine serum (FBS), 15 mM HEPES, 14.3 mM NaHCO3, 2.5 μg/mL Fungizone, and 0.05 mg/mL gentamicin), plated on 6- or 24-well plates pre-coated with poly-L-lysine at a density of 3–5 × 105 cells/cm2. Neonatal and mature astrocytes were cultured at 37 °C in a 5% CO2 incubator. From the third week on, astrocytes received medium supplemented with 20% FBS until they reached confluence (at approximately the fourth week for mature astrocytes), when were used for the experiments.
Ammonia Exposure and Inhibitor Treatments
Neonatal and mature astrocytes were exposed to ammonia (NH4Cl; 5 mM) for 24 h [15, 16, 36] in DMEM/F12 1% FBS, maintained at 37 °C in a 5% CO2 incubator. The effect of AQP4 and p38 MAPK inhibition was evaluated by adding tetraethylammonium (TEA; 10 μM) and SB 203580 (10 μM), respectively, to the culture medium 1 h prior to ammonia incubation [37, 38]. It is important to note that we performed an experimental control using the weak base trimethylamine (5 mM) to test a possible influence of changes in pH [39] on astroglial parameters, but any result was observed (data not shown), indicating that the effects observed in our study were specific for ammonia.
MTT Reduction Assay
MTT was added to the medium at a concentration of 50 μg/mL and cells were incubated for 3 h at 37 °C in an atmosphere of 5% CO2. Subsequently, the medium was removed and the MTT crystals were dissolved in dimethyl-sulfoxide. Absorbance values were measured at 560 nm and 650 nm [24]. The results are expressed as percentages relative to the control conditions.
Actin-Labeling Analysis
For actin-labeling analysis, cells were fixed for 20 min with 4% paraformaldehyde in 0.1 M phosphate-buffered saline (PBS), rinsed with PBS, and then permeabilized for 10 min in PBS containing 0.2% Triton X-100. After, an incubation with 10 μg/mL rhodamine-labeled phalloidin in PBS for 20 min was performed, followed by two washes with PBS [26]. Cell nuclei were stained with 0.2 μg/mL of 4′, 6′-diamidino-2-phenylindole (DAPI) for further 20 min. Astrocyte cultures were analyzed using a Nikon microscope and photographed with a digital camera DXM1200C and TE-FM Epi-Fluorescence accessory.
Extracellular Lactate Content
Lactate content in the extracellular medium was determined using a commercial UV assay from Bioclin (Brazil), according to the manufacturer’s instructions. Results were calculated using a standard and are expressed in mM.
RNA Extraction and Quantitative RT-PCR
Total RNA was isolated from astrocyte cultures using TRIzol Reagent (Invitrogen, Carlsbad, CA) [8]. The concentration and purity of the RNA were determined spectrophotometrically at a ratio of 260:280. Then, 0.5 μg of total RNA was reverse transcribed using Applied Biosystems™ HighCapacity complementary DNA (cDNA) Reverse Transcription Kit (Applied Biosystems) in a 20-μL reaction according to manufacturer’s instructions. The messenger RNA (mRNA) encoding GS (#Rn01483107_m1), TNF-α (#Rn99999017_m1), TNF receptor 1 (TNFR1; #Rn01492348_m1), IL-1β (#Rn00580432_m1), IL-1 receptor type I (IL1R1; #Rn00565482_m1), p65 NFκB (#Rn01502266_m1), p50 NFκB (#Rn01399572_m1), TLR2 (#Rn02133647_s1), TLR4 (#Rn00569848_m1), high mobility group box 1 (HMGB1; #Rn02377062_g1), Nrf2 (#Rn00582415_m1), HO-1 (#Rn01536933_m1), PI3K (#Rn01769524_m1), and β-actin (#Rn00667869_m1) were quantified using the TaqMan real-time RT-PCR system using inventory primers and probes purchased from Applied Biosystems. The mRNA quantification for the genes encoding p21, VEGF, AQP4, inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2), and β-actin was performed using the primer pairs described in Table 1 and Power SYBR Green PCR Master Mix (Invitrogen). Quantitative RT-PCR was performed using the Applied Biosystems 7500 Fast system. Target mRNA levels were normalized to β-actin levels. The results were analyzed employing the 2−ΔΔCt method [40] and expressed relative to the levels of neonatal control astrocytes.
Western Blotting Analysis
Astrocytes were lysed in a solution containing 4% SDS, 2 mM EDTA, and 50 mM Tris–HCl (pH 6.8). Samples were separated by SDS/PAGE, and transferred to nitrocellulose membranes, which were blocked with 4% albumin and then incubated overnight (4 °C) with anti-AQP4 (1:2000), anti-HO-1 (1:1000), or anti-phospho-PI3K (1:2000). β-actin was used as a loading control. Then, the membranes were incubated with a peroxidase-conjugated anti-immunoglobulin (IgG) at a dilution of 1:10,000 for 2 h. Chemiluminescence signal was detected in an Image Quant LAS4010 system (GE Healthcare) using an ECL kit [8]. The results are expressed as percentages relative to control conditions.
ELISA Assays
ELISA assays were performed using intracellular content to evaluate phospho-p38 MAPK in the cell lysate suspended in a specific buffer from ELISA kit, and the levels of NFκB p65 in the nuclear fraction, which had been isolated from lysed cells with 1% Igepal CA-630 and centrifugation (following manufacturer’s instructions). These results were calculated as pg/mL and then corrected by the total amount of protein; thus, they are expressed as pg/mg protein. In the extracellular medium, it evaluated the levels of TNF-α, IL-1β, IL-6, IL-10, BDNF, and GDNF. Table 2 summarizes each ELISA kit information.
Statistical Analyses
Differences among groups were statistically analyzed using two-way analysis of variance (ANOVA), followed by Tukey’s test. All analyses were performed using the GraphPad Prism 6 (GraphPad Software, Inc., La Jolla, CA, USA). Values of p < 0.05 were considered significant; * refers to statistically significant differences between control and ammonia (same age) and # refers to statistically significant differences between ages (neonatal versus mature astrocytes).
Results
Differences Between Neonatal and Mature Cultures in Important Astrocytic-Associated Functions After Ammonia Exposure
In line with our previous data [16, 35], ammonia (1; 5 or 10 mM, 24 h) did not affect cell viability, measured by the MTT reduction assay, in neonatal astrocytes when compared with untreated controls (Fig. 1a). We therefore analyzed the effect of the same concentrations of ammonia in primary astrocyte cultures obtained from adult rats (mature astrocytes). Similarly, ammonia did not cause impairment in cell viability of mature astrocytes (Fig. 1b). Moreover, ammonia did not significantly change the membrane integrity (measured by PI incorporation) and the total number of cells in both neonatal and mature astrocyte cultures (data now shown). Based on these results, we used the well-established concentration of 5 mM [16, 21, 41] to investigate the effects of ammonia on functionality of neonatal and mature astrocytes.
Effects of ammonia in neonatal and mature astrocyte cultures. Neonatal and mature astrocyte cultures were incubated with ammonia (1; 5 or 10 mM) for 24 h for assessing cell viability (a and b). For actin cytoskeleton analysis, cultured astrocytes were incubated with 5 mM ammonia for 24 h (c). For evaluating lactate levels (d), mRNA expression of GS (e), p21 (f), VEGF (g) and AQP4 (h), and immunocontent of AQP4 (i), neonatal and mature astrocyte cultures were incubated with 5 mM ammonia for 24 h. The data represent the means ± S.E.M. of at least four independent experiments performed in triplicate. Differences between groups were statistically analyzed using one or two-way ANOVA, followed by Tukey’s test. p values < 0.05 were considered significant. * indicates differences between control and ammonia (same age); # indicates differences between ages (neonatal versus mature astrocytes)
Actin cytoskeleton is the major determinant of the cell morphology, and neonatal and mature astrocyte cultures showed significant staining for actin with parallel arrangement of stress fiber organization (Fig. 1c). However, ammonia induced actin reorganization at 24 h of exposure, mainly in mature astrocytes, indicating the participation of cytoskeleton in the ammonia effects.
The release of lactate, a product of glycolytic metabolism, was decreased in mature astrocytes compared with those obtained from neonatal rats (Fig. 1d; #p < 0.05). However, ammonia (5 mM) did not change lactate release from astrocytes in both ages.
To investigate the putative ability of astrocytes to detoxify ammonia, we evaluated the mRNA expression of GS. Mature astrocytes expressed less GS than neonatal cells (Fig. 1e; #p < 0.0001), suggesting that mature astrocytes can be more susceptible to ammonia toxicity. Additionally, when exposed to ammonia, neonatal and mature astrocytes showed an opposite response regarding to GS mRNA expression. Ammonia increased mRNA levels of GS in neonatal astrocytes (*p < 0.0001), while decreased in mature astrocytes (*p < 0.0001).
To focus on the ammonia-induced astrocyte senescence, we analyzed the mRNA expression of p21, a cycle inhibitory gene which upregulation has been associated with senescence. As expected, we observed an increase in mRNA levels of p21 in mature astrocytes compared with neonatal astrocytes (Fig. 1f; #p < 0.001). Moreover, ammonia increased p21 mRNA expression in neonatal astrocytes (*p < 0.001) and further enhanced the upregulation of this gene in mature astrocytes (*p < 0.001).
Since ammonia has been reported to impair BBB integrity, we evaluated the expression of VEGF, an astrocyte-derived inducer of vascular permeability, and the astrocytic water channel AQP4. Ammonia was able to similarly increase the VEGF mRNA levels in neonatal and mature astrocytes (*p < 0.0001), whereas the gene expression of this factor was not dependent on age (Fig. 1g). Regarding AQP4, ammonia significantly increased its mRNA expression only in mature astrocytes (Fig. 1h; *p < 0.0001). Moreover, at basal conditions, mature astrocytes showed increased mRNA levels of AQP4 (#p < 0.01). Immunocontent of AQP4 was also evaluated (Fig. 1i); however, any statistically significant change was not observed.
Altogether, these data firstly reinforce that our primary astrocyte cultures derived from adult rats are metabolically and functionally different from astrocyte cultures derived from neonatal animals, probably due to the cellular maturation stage. Consequently, the astrocytic response to external challenges, such as ammonia, might be different dependent on age.
Effects of Ammonia on Astrocytic Inflammatory and Trophic Responses Are Dependent on AQP4 and p38 MAPK/NFκB Signaling
We subsequently investigated the role of p38 MAPK pathway, which is associated with AQP4 expression and also with neuroinflammation, in ammonia-induced inflammatory and trophic responses in astrocytes. The protein levels of p38 MAPK were markedly increased by ammonia (*p < 0.0001; Fig. 2a). In addition, an age-dependent increase in p38 MAPK levels was observed (#p < 0.0001). Interestingly, when both neonatal and mature astrocytes were co-incubated with TEA, a non-specific inhibitor of AQP4, ammonia no longer increased p38 MAPK levels. These results suggest a crosstalk between AQP4 and p38 MAPK, which can be mechanistically involved in astroglial response to ammonia.
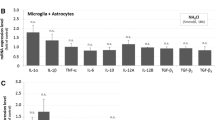
Inflammatory and trophic responses in ammonia-exposed astrocytes were dependent on AQP4 and p38 MAPK/NFκB signaling. Neonatal and mature astrocyte cultures were incubated with TEA (AQP4 inhibitor; 10 μM) or SB 203580 (p38 MAPK inhibitor; 10 μM) for 1 h. Then, 5 mM ammonia was added until 24 h. We evaluated intracellular p38 MAPK levels (a), nuclear p65 NFκB levels (b), and extracellular levels of TNF-α (c), IL-1β (d), IL-6 (e), IL-10 (f), BDNF (g), and GDNF (h). The data represent the means ± S.E.M. of at least four independent experiments performed in triplicate. Differences between groups were statistically analyzed using one or two-way ANOVA, followed by Tukey’s test. p values < 0.05 were considered significant. * indicates differences between control and ammonia (same age); # indicates differences between ages (neonatal versus mature astrocytes). SB, SB 203580
The p38 MAPK signaling pathway can induce the transcriptional activity of NFκB, a master regulator of cellular inflammatory and oxidative responses. As shown in Fig. 2b, ammonia increased nuclear protein levels of p65 NFκB (*p < 0.0001). Comparing neonatal and mature cells, we observed higher p65 NFκB protein levels in the nuclear fraction of mature astrocytes (#p < 0.0001). When astrocytes from both ages were co-incubated with TEA or SB 203580, a p38 MAPK inhibitor, the effects of ammonia on NFκB activation were completely abrogated. Interestingly, considering mature astrocytes, p38 MAPK inhibitor was also able to decrease age-related NFκB activation, not only in the presence of ammonia but also at basal conditions.
Consistently with an activation of p38 MAPK/NFκB in the presence of ammonia, both neonatal (*p < 0.0001) and mature astrocytes (p < 0.0001) release higher levels of TNF-α relative to its respective control cells (Fig. 2c). When co-incubated with AQP4 inhibitor TEA, the effect of ammonia on TNF-α in astrocytes was completely abolished. Using the p38 MAPK inhibitor SB 203580, the ammonia-induced increase of TNF-α was also prevented. Ammonia additionally increased the release of IL-1β (Fig. 2d; *p < 0.0001) and IL-6 (Fig. 2e; *p < 0.0001) in both neonatal and mature astrocytes. In agreement with the results found for TNF-α, co-incubation with either TEA or SB 203580 prevented the ammonia-induced increase of extracellular IL-1β and IL-6. However, we did not observe any change for IL-10 release (Fig. 2f).
Importantly, mature astrocytes showed elevated extracellular levels of TNF-α (Fig. 2c), IL-1β (Fig. 2d), and IL-6 (Fig. 2e) compared with neonatal cultures at basal conditions. In agreement with the result found for NFκB activation, blocking p38 MAPK in mature astrocytes decreased the release of all these cytokines. Thus, our results suggest an involvement of AQP4/p38 MAPK/NFκB activation in ammonia-induced inflammatory response of astrocytes, and the role of p38 MAPK in the inflamed status of mature cells.
In contrast, extracellular levels of GDNF (Fig. 2g) and BDNF (Fig. 2h) were markedly decreased in response to ammonia (*p < 0.0001). Interestingly, when astrocytes were co-incubated with ammonia and AQP4 or p38 MAPK inhibitors, different effects were observed. Inhibition of AQP4 totally abolished the ammonia-induced decrease in the extracellular content of GDNF and BDNF in neonatal and mature astrocytes. However, p38 MAPK inhibitor could partially prevent the effect of ammonia on GDNF release, but only in neonatal astrocytes. Regarding BDNF levels, they were not affected by p38 MAPK blockage. Moreover, the release of both these trophic factors did not change with age in cortical astrocytes.
Ammonia Enhanced Age-Related Upregulation of Inflammatory Genes in Astrocytes
Following the pro-inflammatory effects of age and ammonia on cytokine release, we further analyzed the expression of several genes associated with inflammatory responses of astrocytes. Interestingly, despite of which was found for TNF-α release, mature astrocytes showed similar mRNA levels of TNF-α (Fig. 3a) and TNFR1 (Fig. 3b) compared with neonatal astrocytes. However, there was a markedly upregulation of the IL-1β gene (#p < 0.05; Fig. 3c), as well as of its receptor IL1R1 (#p < 0.01; Fig. 3d), with age. Regarding the effects of ammonia, it increased mRNA levels of TNF-α only in neonatal cells (Fig. 3a; *p < 0.0001), but TNFR1 was upregulated in both neonatal and mature astrocytes (Fig. 3b; *p < 0.05). Considering the mRNA expression of IL-1β, it was upregulated by ammonia in mature but not in neonatal cells (Fig. 3c; *p < 0.05), whereas the IL1R1 (Fig. 3d) was not changed by ammonia. Of interest, genes related to TNF-α and IL-1β inflammatory signaling can be differently activated in astrocytes; TNF-α appeared to be more related to ammonia challenge, while IL-1β was mainly affected by age.
Ammonia enhanced inflammaging-related gene expression in mature astrocytes. Neonatal and mature astrocyte cultures were incubated with 5 mM ammonia for 24 h. The mRNA expression of TNF-α (a), TNFR1 (b), IL-1β (c), IL1R1 (d), p65 NFκB (e), p50 NFκB (f), COX-2 (g), iNOS (h), TLR2 (i), TLR4 (j), and HMGB1 (k) was assessed. The data represent the means ± S.E.M. of at least four independent experiments performed in triplicate. Differences between groups were statistically analyzed using one or two-way ANOVA, followed by Tukey’s test. p values < 0.05 were considered significant. * indicates differences between control and ammonia (same age); # indicates differences between ages (neonatal versus mature astrocytes)
In addition to show an increase in the transcriptional activity of NFκB, mature astrocytes had higher mRNA levels of p65 NFκB (Fig. 3e; #p < 0.05). However, the mRNA expression of p50 NFκB was not changed compared with neonatal astrocytes (Fig. 3f). Ammonia, in turn, upregulated both NFκB subunits in neonatal (*p < 0.001 for p65 and *p < 0.01 for p50) and mature astrocytes (*p < 0.001 for p65 and p50). Importantly, the effect of ammonia on the expression of NFκB subunits was greater in mature compared with neonatal cells (#p < 0.05). Along this line, genes encoding COX-2 (Fig. 3g) and iNOS (Fig. 3h), which can be subjected to transcriptional activation by NFκB, were significantly upregulated by age (#p < 0.0001). Ammonia raised both of COX-2 and iNOS expression in neonatal astrocytes (*p < 0.0001), and potentiated the increase found in mature cells (*p < 0.0001; #p < 0.0001).
TLRs are a family of receptors with a crucial role in inducing inflammatory activation mediated by extracellular stimuli. The mRNA levels of TLR2 were significantly increased in mature astrocytes with respect to neonatal astrocytes (#p < 0.05, Fig. 3i), but were not changed by ammonia. In contrast, mRNA expression of TLR4 (Fig. 3j) was increased in an age-dependent manner (#p < 0.01) and also in response to ammonia, but this last effect occurred only in neonatal astrocytes (*p < 0.05).
The transcription of the alarmin HMGB1 was not affected by age, but it was similarly upregulated in response to ammonia in neonatal and mature astrocytes (*p < 0.05; Fig. 3k).
Ammonia and Age Change Gene Expression of Cytoprotective Pathways in Astrocytes
Nrf2/HO-1 signaling pathway provides cellular protection against several stressor stimuli. Compared with neonatal astrocytes, mature cells expressed lower mRNA levels of Nrf2 (#p < 0.001; Fig. 4a), whereas the expression of HO-1 was not statistically different between ages (Fig. 4b). In neonatal astrocytes, ammonia increased the gene expression of both Nrf2 (*p < 0.0001) and HO-1 (*p < 0.0001). However, an opposite effect was observed in mature astrocytes, in which ammonia further downregulated Nrf2 (*p < 0.001) and decreased the mRNA expression of HO-1 (*p < 0.0001) compared with untreated mature cells. We also analyzed HO-1 content by western blotting (Fig. 4c). Although we found a statistically significant increase in HO-1 only between neonatal and mature astrocytes (#p < 0.01), the protein levels followed a similar profile of gene expression, with an apparent ammonia-associated increase in HO-1 in neonatal astrocytes and a decrease in mature astrocytes.
Effects of ammonia and age in astrocytic gene expression of cytoprotective pathways. Neonatal and mature astrocyte cultures were incubated with 5 mM ammonia for 24 h. The mRNA expression of Nrf2 (a), HO-1 (b), and PI3K (d) was evaluated, as well as the HO-1 (c) and phospho-PI3K (e) protein levels. The data represent the means ± S.E.M. of at least four independent experiments performed in triplicate. Differences between groups were statistically analyzed using one or two-way ANOVA, followed by Tukey’s test. p values < 0.05 were considered significant. * indicates differences between control and ammonia (same age); # indicates differences between ages (neonatal versus mature astrocytes)
PI3K pathway, in turn, regulates cell growth, proliferation, and survival. Figure 4 d and e depict the gene expression of the catalytic subunit gamma of PI3K and phospho-PI3K (p55 Tyr199) levels, respectively. PI3K was downregulated in mature astrocytes compared with neonatal astrocytes (#p < 0.0001). Ammonia exposure reduced mRNA levels of PI3K in neonatal astrocytes (*p < 0.0001), and caused a further decline in mature astrocytes (*p < 0.001; *p < 0.0001). Phospho-PI3K levels, however, were decreased only by ammonia in neonatal astrocytes (*p < 0.05; Fig. 4e).
Discussion
The use of ammonia-treated cultured astrocytes, classically obtained from neonate animals, has been widely used to investigate the underlying mechanisms of ammonia toxicity and the pathogenesis of HE [22]. In fact, most of the findings suggest that HE is a primary gliopathy (astrocyte as the major cell type affected), mainly obtained using primary astrocyte cultures [42,43,44,45,46]. However, neonatal hyperammonemia is rare, and there are few data about ammonia toxicity and its underlying mechanisms in mature astrocyte cultures (i.e., obtained from adult animals). Therefore, here, we showed that ammonia can induce a wide range of cellular responses, not only in neonatal, but also in mature astrocytes.
In extrahepatic tissues, ammonia is metabolized mainly via GS. This reaction, which incorporates ammonia into glutamate to form glutamine, occurs in astrocytes in the CNS [14]. According to our results, mature astrocytes had a decreased expression of GS, compared with neonatal astrocytes. In addition, ammonia exposure further decreased GS expression in adult astrocytes, but not in neonatal cells. It is important to note that GS expression is highly regulated and can be influenced by several signaling pathways and extracellular factors, including hormones and even ammonia [47], and the mRNA levels of GS are closely correlated with their protein expression and activity [23, 48, 49]. Our previous works have demonstrated that GS expression and/or activity decrease in cultured astrocytes in an age-dependent manner [23, 26, 50]. Importantly, other parameters related to astrocyte functionality are also affected by aging, showing that astrocytes can undergo a neurochemical remodeling with age, which involves changes in gene transcription [23, 26, 27, 50]. In this context, neonatal and mature astrocytes can present a different ability to respond to harmful stimuli. Here, the increase in mRNA expression of GS in neonatal astrocytes may represent a compensatory response against hyperammonemia. On the contrary, mature astrocytes could not upregulate GS expression to compensate the excess of ammonia, since there is an age-dependent downregulation that potentially makes these cells more susceptible to ammonia toxicity. Moreover, decreased GS expression can also impair the metabolism of the excitatory neurotransmitter glutamate, which can generate excitotoxicity.
Physiologically, the brain can be partially protected from peripheral toxic agents, including ammonia, by the BBB. It regulates the transport of molecules into and out the CNS, and astrocytes are important constitutive components of the BBB [51, 52]. Among the proteins that participate in the transport functions across the BBB are the water channels aquaporins. Particularly, AQP4 is expressed in astrocyte processes and is the main responsible for water transport [53, 54]. An interplay among ammonia, AQP4 expression, and edema, a common pathophysiological feature of HE, can be suggested [55,56,57]. Our results showed that ammonia can increase AQP4 expression, particularly in mature astrocytes. In addition, AQP4 mRNA expression was higher in mature astrocytes, compared with neonatal cells. Although alterations in mRNA expression of AQP4 have been commonly accompanied by alterations in its protein levels in response to different stimuli [58,59,60], AQP4 immunocontent was not changed in our study. Regarding the differences found between RT-PCR and western blotting analysis, it is important to consider some points. First, we cannot rule out earlier alterations in AQP4 protein levels during the 24 h of treatment, due to the protein turnover (translation and/or degradation). Second, total protein levels of AQP4 measured by western blotting do not necessarily reflect the content of active molecules in the plasma membrane, since AQP4 subcellular location and trafficking can be regulated by phosphorylation by several signaling pathways, including protein cinases A and C (PKA and PKC) [61]. Third, a previous study regarding the effects of ammonia in cultured astrocytes showed that AQP4 protein content was dependent on the method of analysis, perhaps due to differences in AQP4 aggregation [41].
In addition to regulate water transport, AQP4 has been demonstrated other roles in the CNS, including an involvement in neuroinflammation [62, 63]. Previously, studies using AQP4 null mice or deleting AQP4 demonstrated neuroprotective effects in pathological conditions including hepatic encephalopathy, autoimmune encephalomyelitis, ischemia, and traumatic brain injury [64,65,66,67]. Moreover, AQP4 modulation has been considered a potential target for therapeutic drugs [68]. In agreement with these data, we showed that inhibition of AQP4 with TEA avoided ammonia-induced inflammatory response in both neonatal and mature astrocytes.
Neuroinflammation involving activated astrocytes is another important characteristic of hyperammonemia [16, 35, 69,70,71], which was notably observed in our cultures. Several inflammatory markers, including TNF-α and its receptor TNFR1, IL-1β, IL-6, HMGB1, COX-2, and iNOS, were markedly augmented in ammonia-treated astrocytes. Additionally, ammonia caused an increase in p38 MAPK and NFκB signaling pathways, which are related to expression of pro-inflammatory proteins [16, 72, 73]. Inhibition of AQP4 also prevented the increase of both p38 MAPK and p65 NFκB levels, indicating that ammonia-induced upregulation of AQP4 triggers the activation of these inflammatory pathways. Furthermore, when neonatal and mature astrocytes were co-incubated with SB 203580, a p38 MAPK inhibitor, ammonia no longer promoted the increase of pro-inflammatory cytokine release (TNF-α, IL-1β, and IL-6) and p65 NFκB activation. An interrelationship between AQP4 and p38 MAPK has been described, mainly regarding the induction of AQP4 expression by p38 MAPK [55, 74]. Our study also suggests that ammonia is able to stimulate AQP4 transport activity, which in turn, promoted the activation of p38 MAPK signaling, with consequent p65 NFκB nuclear translocation and induction of cytokine production.
Consequently, this plethora of inflammatory mediators might impact CNS homeostasis, by inducing neurochemical, neuroendocrine, and neuroimmune alterations [75]. Depending on time and inflamed milieu, disruption of BBB integrity can occur, leading to immune cell trafficking into the CNS [10, 76]. Astrocyte-derived VEGF, which is regulated by NFκB, mediates BBB permeability by increasing tight junction protein levels [52, 77]; we demonstrated that its expression increased in response to ammonia in both neonatal and mature astrocytes. In this scenario, peripheral immune signaling might exacerbate the inflammatory response in HE [78], promoting detrimental effects on other neural cells.
It is also important to point out some interesting differences found in our study regarding the expression of inflammatory and immune response-related genes between neonatal and mature astrocytes. In agreement with our previous findings, we observed an age-related increase of pro-inflammatory markers in mature astrocytes compared with neonatal cells [23, 26, 79, 80]. Previous studies have shown the role of IL-1β signaling in impairing synaptic plasticity processes and in aging brain [81,82,83]. Particularly, we herein found that mRNA expression of IL-1β was markedly upregulated in mature astrocytes under control conditions, as well as there was an increase in its receptor IL1R1. However, we did not observe age-related differences in mRNA expression of TNF-α and its receptor TNFR1. On the other hand, considering the pro-inflammatory effects of ammonia, they were more evident in the expression of genes associated with TNF-α signaling. Therefore, these results suggest that age- and ammonia-related inflammatory responses in astrocytes may occur by different mechanisms. However, both of them seem to be regulated in a p38 MAPK-dependent signaling [84, 85]. The p38 MAPK inhibitor (SB 203580) abolished the increased release of TNF-α and IL-1β in mature astrocytes when compared with neonatal controls, and in astrocyte (neonatal and mature) cultures exposed to ammonia.
Interestingly, the upregulation of IL-1β gene expression may be related to the increased expression of TLR4 by mature astrocytes [7, 86]. TLRs are pattern recognition receptors of the innate immune system whose function is sensing potentially dangerous signals, including pathogen- and damage-associated molecular patterns, to drive inflammatory responses [7, 87]. TLR2 and TLR4 are the main family members expressed by neural cells, including astrocytes [88]. The expression of these receptors can be modulated in response to pathogens and other environmental stresses [30, 89, 90]. Moreover, it has been reported that aging induces an upregulation of some family members of TLRs in mouse brain [87, 91]. Using our primary astrocyte cultures, we demonstrated that the mRNA expression of both TLR2 and TLR4 was higher in astrocytes obtained from adult brain relative to those derived from neonate animals. Thus, the challenging experiences to which an organism is exposed throughout life can leave an immune mark in their astrocytes and can determine how these cells will respond to damage stimuli, such as ammonia.
Several trophic factors associated with protective functions of astrocytes, such as BDNF and GDNF, were also modulated by either ammonia or age. BDNF and GDNF expression and/or functions have been associated with AQP4 in the CNS [92, 93]. Moreover, ammonia decreased BDNF release in hippocampal slices [94]. Our data are in agreement with these recent findings, and showed that GDNF, another important trophic factor, also had its release decreased by ammonia. The impairment in the release of BDNF and GDNF by ammonia was prevented by AQP4 inhibitor, but appears to be independent of p38 MAPK. A deficit in trophic signaling in the CNS can be related to impaired synaptic connectivity in HE [95]. In contrast with our previous data [23, 26], these parameters were not changed by age in cortical astrocytes.
In addition, signaling pathways including Nrf2, HO-1, and p21 presented interesting age-dependent changes after ammonia challenge. HO-1 belongs to a family of enzymes whose expression can be transcriptionally regulated by Nrf2, the master regulator of antioxidant response, as an adaptive defense mechanism to protect cells from damage [96,97,98]. Products of HO-1 activity, mainly biliverdin and monoxide carbon, have been shown antioxidant and anti-inflammatory properties [99, 100]. In our study, we observed that ammonia upregulated mRNA levels of both HO-1 and Nrf2 in neonatal astrocytes, but in mature astrocytes, their expression was downregulated. These results suggest that neonatal and mature astrocytes may have different abilities to generate cytoprotective responses under stressful conditions, such as ammonia exposure. It is important to note that other works also demonstrated an inducer effect of ammonia on HO-1 in cultured astrocytes (derived from neonatal animals), in in vivo models of HE using adult animals, and in post-mortem brains [101,102,103]. However, it remains to be established in which cell types, the expression of HO-1, are increased in adult brain, since a previous study showed that ammonia did not affect HO-1 expression in neurons [103], and we demonstrated that in mature astrocytes, ammonia decreased HO-1 gene expression.
In agreement with recent reports, we observed that ammonia increased mRNA expression of p21, a cell cycle inhibitory factor used as a marker of senescence [21, 104]. In addition, p21 was also upregulated in mature astrocyte cultures relative to neonatal cells at control conditions, indicating a natural course of senescence of these cells. Senescence is a process that occurs during biological aging, characterized by the loss of cellular ability to replicate as a consequence of the arrest of the cell cycle [105, 106]. Moreover, senescent astrocytes acquire a pro-inflammatory secretory phenotype [107]. Although senescence is commonly associated with aging, it can also be prematurely induced, including in astrocytes, by a variety of stressors, such as ammonia [21, 108]. Importantly, p38 MAPK pathway can regulate the expression of p21 by astrocytes [21]. Moreover, although HO-1 exerts beneficial effects, its persistent expression can be deleterious. In line with this, HO-1 was proposed to participate in ammonia-induced senescence [102]. However, it is important to point out that such effect was reported in primary astrocyte cultures obtained from neonate animals. In mature astrocytes, probably other mechanisms rather than HO-1 (i.e., inflammatory response) can participate in ammonia-induced increase of p21. It is important to note that as astrocyte senescence correlates with cognitive decline, it may be associated with the persistent cognitive impairment in HE patients [104, 109, 110]. Depending upon the degree of hyperammonemia and its duration, irreversible brain damages and disabilities can be established [111].
Two possible limitations of this study should be mentioned. Firstly, TEA is a non-specific inhibitor of AQP4. Although TEA incubation suggests a role of AQP4 in the effects of ammonia on neonatal and mature astrocytes, other strategies, such as gene silencing and/or more specific pharmacological inhibitors for AQP4, are needed to support this evidence and to further investigate the dynamics of AQP4 in ammonia gliotoxicity. Secondly, the effects of ammonia on mature astrocytes were evaluated only in primary cultures obtained from 90-day-old rats. In this regard, data from cultured astrocytes derived from older rats, as well as from animals subjected to in vivo experimental hyperammonemia models, will confirm and expand the knowledge about ammonia-induced glial-inflammaging.
In summary, we observed age-dependent differences in astrocyte gene expression, which may reflect age-related functional properties of these cells (Fig. 5). The present study also showed that ammonia markedly altered a wide range of signaling pathways and molecules that mediate important astrocyte functions. Moreover, we demonstrated a role of AQP4 and p38 MAPK, at least in part, as potentially mediators of ammonia damage effects. Considering the essential roles of astrocytes in brain homeostasis and support to neurons, it is reasonable to assume that functional alterations caused by ammonia in mature astrocytes, which potentially accelerate the inflammaging process, may be associated with the permanence of cognitive symptoms in adult after HE.
Ammonia-induced inflammaging in primary astrocyte cultures. Summarizing scheme showing the effects of ammonia on primary astrocyte cultures obtained from neonate and adult Wistar rats. It is important to note that inflammatory signaling increased from neonatal to mature astrocytes, while cytoprotective mechanisms were decreased. Ammonia, in turn, was able to potentiate intrinsic age-related inflammatory and senescence markers in mature astrocytes
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Dallérac G, Zapata J, Rouach N (2018) Versatile control of synaptic circuits by astrocytes: where, when and how? Nat Rev Neurosci 19:729–743. https://doi.org/10.1038/s41583-018-0080-6
Gonçalves C-A, Rodrigues L, Bobermin LD, Zanotto C, Vizuete A, Quincozes-Santos A, Souza DO, Leite MC (2018) Glycolysis-derived compounds from astrocytes that modulate synaptic communication. Front Neurosci 12:1035. https://doi.org/10.3389/fnins.2018.01035
Michinaga S, Koyama Y (2019) Dual roles of astrocyte-derived factors in regulation of blood-brain barrier function after brain damage Int J Mol Sci 20:. https://doi.org/10.3390/ijms20030571,
Markiewicz I, Lukomska B (2006) The role of astrocytes in the physiology and pathology of the central nervous system. Acta Neurobiol Exp (Wars) 66:343–358
Colombo E, Farina C (2016) Astrocytes: key regulators of neuroinflammation. Trends Immunol 37:608–620. https://doi.org/10.1016/j.it.2016.06.006
Cunningham C, Dunne A, Lopez-Rodriguez AB (2018) Astrocytes: heterogeneous and dynamic phenotypes in neurodegeneration and innate immunity. Neuroscientist 1073858418809941. https://doi.org/10.1177/1073858418809941
Okun E, Griffioen KJ, Mattson MP (2011) Toll-like receptor signaling in neural plasticity and disease. Trends Neurosci 34:269–281. https://doi.org/10.1016/j.tins.2011.02.005
Bobermin LD, Roppa RHA, Quincozes-Santos A (2019) Adenosine receptors as a new target for resveratrol-mediated glioprotection. Biochim Biophys Acta Mol basis Dis 1865:634–647. https://doi.org/10.1016/j.bbadis.2019.01.004
Gorina R, Font-Nieves M, Márquez-Kisinousky L, Santalucia T, Planas AM (2011) Astrocyte TLR4 activation induces a proinflammatory environment through the interplay between MyD88-dependent NFκB signaling, MAPK, and Jak1/Stat1 pathways. Glia 59:242–255. https://doi.org/10.1002/glia.21094
Yi W, Schlüter D, Wang X (2019) Astrocytes in multiple sclerosis and experimental autoimmune encephalomyelitis: star-shaped cells illuminating the darkness of CNS autoimmunity. Brain Behav Immun 80:10–24. https://doi.org/10.1016/j.bbi.2019.05.029
Dasarathy S, Mookerjee RP, Rackayova V, Rangroo Thrane V, Vairappan B, Ott P, Rose CF (2017) Ammonia toxicity: from head to toe? Metab Brain Dis 32:529–538. https://doi.org/10.1007/s11011-016-9938-3
Walker V (2014) Ammonia metabolism and hyperammonemic disorders. In: Advances in Clinical Chemistry. Elsevier, pp 73–150
Felipo V (2013) Hepatic encephalopathy: effects of liver failure on brain function. Nat Rev Neurosci 14:851–858. https://doi.org/10.1038/nrn3587
Jayakumar AR, Norenberg MD (2016) Glutamine synthetase: role in neurological disorders. Adv Neurobiol 13:327–350. https://doi.org/10.1007/978-3-319-45096-4_13
Bobermin LD, Souza DO, Gonçalves C-A, Quincozes-Santos A (2018) Resveratrol prevents ammonia-induced mitochondrial dysfunction and cellular redox imbalance in C6 astroglial cells. Nutr Neurosci 21:276–285. https://doi.org/10.1080/1028415X.2017.1284375
Bobermin LD, Quincozes-Santos A, Guerra MC, Leite MC, Souza DO, Gonçalves CA, Gottfried C (2012) Resveratrol prevents ammonia toxicity in astroglial cells. PLoS One 7:e52164. https://doi.org/10.1371/journal.pone.0052164
Hernández-Rabaza V, Cabrera-Pastor A, Taoro-González L, Malaguarnera M, Agustí A, Llansola M, Felipo V (2016) Hyperammonemia induces glial activation, neuroinflammation and alters neurotransmitter receptors in hippocampus, impairing spatial learning: reversal by sulforaphane. J Neuroinflammation 13:41. https://doi.org/10.1186/s12974-016-0505-y
Oja SS, Saransaari P, Korpi ER (2017) Neurotoxicity of ammonia. Neurochem Res 42:713–720. https://doi.org/10.1007/s11064-016-2014-x
Rama Rao KV, Jayakumar AR, Tong X, Curtis KM, Norenberg MD (2010) Brain aquaporin-4 in experimental acute liver failure. J Neuropathol Exp Neurol 69:869–879. https://doi.org/10.1097/NEN.0b013e3181ebe581
Wright G, Soper R, Brooks HF, Stadlbauer V, Vairappan B, Davies NA, Andreola F, Hodges S et al (2010) Role of aquaporin-4 in the development of brain oedema in liver failure. J Hepatol 53:91–97. https://doi.org/10.1016/j.jhep.2010.02.020
Görg B, Karababa A, Shafigullina A, Bidmon HJ, Häussinger D (2015) Ammonia-induced senescence in cultured rat astrocytes and in human cerebral cortex in hepatic encephalopathy. Glia 63:37–50. https://doi.org/10.1002/glia.22731
Lange SC, Bak LK, Waagepetersen HS, Schousboe A, Norenberg MD (2012) Primary cultures of astrocytes: their value in understanding astrocytes in health and disease. Neurochem Res 37:2569–2588. https://doi.org/10.1007/s11064-012-0868-0
Bellaver B, Souza DG, Souza DO, Quincozes-Santos A (2017) Hippocampal astrocyte cultures from adult and aged rats reproduce changes in glial functionality observed in the aging brain. Mol Neurobiol 54:2969–2985. https://doi.org/10.1007/s12035-016-9880-8
Longoni A, Bellaver B, Bobermin LD, Santos CL, Nonose Y, Kolling J, dos Santos TM, de Assis AM et al (2018) Homocysteine induces glial reactivity in adult rat astrocyte cultures. Mol Neurobiol 55:1966–1976. https://doi.org/10.1007/s12035-017-0463-0
Santos CL, Bobermin LD, Souza DO, Quincozes-Santos A (2018) Leptin stimulates the release of pro-inflammatory cytokines in hypothalamic astrocyte cultures from adult and aged rats. Metab Brain Dis 33:2059–2063. https://doi.org/10.1007/s11011-018-0311-6
Santos CL, Roppa PHA, Truccolo P, Fontella FU, Souza DO, Bobermin LD, Quincozes-Santos A (2018) Age-dependent neurochemical remodeling of hypothalamic astrocytes. Mol Neurobiol 55:5565–5579. https://doi.org/10.1007/s12035-017-0786-x
Souza DG, Bellaver B, Souza DO, Quincozes-Santos A (2013) Characterization of adult rat astrocyte cultures. PLoS One 8:e60282. https://doi.org/10.1371/journal.pone.0060282
Bellaver B, Dos Santos JP, Leffa DT et al (2018) Systemic inflammation as a driver of brain injury: the astrocyte as an emerging player. Mol Neurobiol 55:2685–2695. https://doi.org/10.1007/s12035-017-0526-2
Christensen LB, Woods TA, Carmody AB, Caughey B, Peterson KE (2014) Age-related differences in neuroinflammatory responses associated with a distinct profile of regulatory markers on neonatal microglia. J Neuroinflammation 11:70. https://doi.org/10.1186/1742-2094-11-70
Gárate I, Garcia-Bueno B, Madrigal JLM, Caso JR, Alou L, Gomez-Lus ML, Micó JA, Leza JC (2013) Stress-induced neuroinflammation: role of the toll-like receptor-4 pathway. Biol Psychiatry 73:32–43. https://doi.org/10.1016/j.biopsych.2012.07.005
Klein RS, Hunter CA (2017) Protective and pathological immunity during CNS infections. Immunity 46:891–909. https://doi.org/10.1016/j.immuni.2017.06.012
Franceschi C, Campisi J (2014) Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S4–S9. https://doi.org/10.1093/gerona/glu057
Griñan-Ferré C, Palomera-Ávalos V, Puigoriol-Illamola D, Camins A, Porquet D, Plá V, Aguado F, Pallàs M (2016) Behaviour and cognitive changes correlated with hippocampal neuroinflammaging and neuronal markers in female SAMP8, a model of accelerated senescence. Exp Gerontol 80:57–69. https://doi.org/10.1016/j.exger.2016.03.014
Pizza V, Agresta A, D’Acunto CW et al (2011) Neuroinflamm-aging and neurodegenerative diseases: an overview. CNS Neurol Disord Drug Targets 10:621–634
Bobermin LD, Arús BA, Leite MC, Souza DO, Gonçalves CA, Quincozes-Santos A (2016) Gap junction intercellular communication mediates ammonia-induced neurotoxicity. Neurotox Res 29:314–324. https://doi.org/10.1007/s12640-015-9581-5
Bobermin LD, Hansel G, Scherer EBS, Wyse ATS, Souza DO, Quincozes-Santos A, Gonçalves CA (2015) Ammonia impairs glutamatergic communication in astroglial cells: protective role of resveratrol. Toxicol in Vitro 29:2022–2029. https://doi.org/10.1016/j.tiv.2015.08.008
Wartchow KM, Tramontina AC, de Souza DF, Biasibetti R, Bobermin LD, Gonçalves CA (2016) Insulin stimulates S100B secretion and these proteins antagonistically modulate brain glucose metabolism. Neurochem Res 41:1420–1429. https://doi.org/10.1007/s11064-016-1851-y
Zanotto C, Abib RT, Batassini C, Tortorelli LS, Biasibetti R, Rodrigues L, Nardin P, Hansen F et al (2013) Non-specific inhibitors of aquaporin-4 stimulate S100B secretion in acute hippocampal slices of rats. Brain Res 1491:14–22. https://doi.org/10.1016/j.brainres.2012.10.065
Rose C, Kresse W, Kettenmann H (2005) Acute insult of ammonia leads to calcium-dependent glutamate release from cultured astrocytes, an effect of pH. J Biol Chem 280:20937–20944. https://doi.org/10.1074/jbc.M412448200
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408. https://doi.org/10.1006/meth.2001.1262
Bodega G, Suárez I, López-Fernández LA, García MI, Köber M, Penedo M, Luna M, Juárez S et al (2012) Ammonia induces aquaporin-4 rearrangement in the plasma membrane of cultured astrocytes. Neurochem Int 61:1314–1324. https://doi.org/10.1016/j.neuint.2012.09.008
Bender AS, Norenberg MD (1996) Effects of ammonia on L-glutamate uptake in cultured astrocytes. Neurochem Res 21:567–573. https://doi.org/10.1007/bf02527755
Gregorios JB, Mozes LW, Norenberg MD (1985) Morphologic effects of ammonia on primary astrocyte cultures II Electron microscopic studies. J Neuropathol Exp Neurol 44:404–414. https://doi.org/10.1097/00005072-198507000-00004
Murthy CR, Rama Rao KV, Bai G, Norenberg MD (2001) Ammonia-induced production of free radicals in primary cultures of rat astrocytes. J Neurosci Res 66:282–288. https://doi.org/10.1002/jnr.1222
Neary JT, Woodson C, Blicharska J, Norenberg LOB, Norenberg MD (1990) Effect of ammonia on calcium homeostasis in primary astrocyte cultures. Brain Res 524:231–235. https://doi.org/10.1016/0006-8993(90)90696-9
Neary JT, Norenberg LO, Gutierrez MP, Norenberg MD (1987) Hyperammonemia causes altered protein phosphorylation in astrocytes. Brain Res 437:161–164. https://doi.org/10.1016/0006-8993(87)91538-1
Suárez I, Bodega G, Fernández B (2002) Glutamine synthetase in brain: effect of ammonia. Neurochem Int 41:123–142. https://doi.org/10.1016/S0197-0186(02)00033-5
Li Y, Wang S, Ran K et al (2015) Differential hippocampal protein expression between normal aged rats and aged rats with postoperative cognitive dysfunction: a proteomic analysis. Mol Med Rep 12:2953–2960. https://doi.org/10.3892/mmr.2015.3697
Shen Y, Gao H, Shi X, Wang N, Ai D, Li J, Ouyang L, Yang J et al (2014) Glutamine synthetase plays a role in d-galactose-induced astrocyte aging in vitro and in vivo. Exp Gerontol 58:166–173. https://doi.org/10.1016/j.exger.2014.08.006
Souza DG, Bellaver B, Raupp GS, Souza DO, Quincozes-Santos A (2015) Astrocytes from adult Wistar rats aged in vitro show changes in glial functions. Neurochem Int 90:93–97. https://doi.org/10.1016/j.neuint.2015.07.016
Abbott NJ, Rönnbäck L, Hansson E (2006) Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci 7:41–53. https://doi.org/10.1038/nrn1824
Sweeney MD, Zhao Z, Montagne A, Nelson AR, Zlokovic BV (2019) Blood-brain barrier: from physiology to disease and back. Physiol Rev 99:21–78. https://doi.org/10.1152/physrev.00050.2017
Papadopoulos MC, Verkman AS (2013) Aquaporin water channels in the nervous system. Nat Rev Neurosci 14:265–277. https://doi.org/10.1038/nrn3468
Potokar M, Jorgačevski J, Zorec R (2016) Astrocyte aquaporin dynamics in health and disease. Int J Mol Sci 17. https://doi.org/10.3390/ijms17071121
Pan C-F, Zhu S-M, Zheng Y-Y (2010) Ammonia induces upregulation of aquaporin-4 in neocortical astrocytes of rats through the p38 mitogen-activated protein kinase pathway. Chin Med J 123:1888–1892
Rama Rao KV, Chen M, Simard JM, Norenberg MD (2003) Increased aquaporin-4 expression in ammonia-treated cultured astrocytes. Neuroreport 14:2379–2382. https://doi.org/10.1097/00001756-200312190-00018
Rama Rao KV, Norenberg MD (2007) Aquaporin-4 in hepatic encephalopathy. Metab Brain Dis 22:265–275. https://doi.org/10.1007/s11011-007-9063-4
He L, Zhang X, Wei X, Li Y (2014) Progesterone attenuates aquaporin-4 expression in an astrocyte model of ischemia/reperfusion. Neurochem Res 39:2251–2261. https://doi.org/10.1007/s11064-014-1427-7
Katoozi S, Skauli N, Zahl S, Deshpande T, Ezan P, Palazzo C, Steinhäuser C, Frigeri A et al (2020) Uncoupling of the astrocyte syncytium differentially affects AQP4 isoforms. Cells 9:382. https://doi.org/10.3390/cells9020382
Skowrońska K, Obara-Michlewska M, Czarnecka A, Dąbrowska K, Zielińska M, Albrecht J (2019) Persistent overexposure to N-methyl-d-aspartate (NMDA) calcium-dependently downregulates glutamine synthetase, aquaporin 4, and Kir4.1 channel in mouse cortical astrocytes. Neurotox Res 35:271–280. https://doi.org/10.1007/s12640-018-9958-3
Vandebroek A, Yasui M (2020) Regulation of AQP4 in the central nervous system. IJMS 21:1603. https://doi.org/10.3390/ijms21051603
Fukuda AM, Badaut J (2012) Aquaporin 4: a player in cerebral edema and neuroinflammation. J Neuroinflammation 9:279. https://doi.org/10.1186/1742-2094-9-279
Ikeshima-Kataoka H (2016) Neuroimmunological implications of AQP4 in astrocytes. Int J Mol Sci 17:1306. https://doi.org/10.3390/ijms17081306
Akdemir G, Ratelade J, Asavapanumas N, Verkman AS (2014) Neuroprotective effect of aquaporin-4 deficiency in a mouse model of severe global cerebral ischemia produced by transient 4-vessel occlusion. Neurosci Lett 574:70–75. https://doi.org/10.1016/j.neulet.2014.03.073
Li L, Zhang H, Varrin-Doyer M, Zamvil SS, Verkman AS (2011) Proinflammatory role of aquaporin-4 in autoimmune neuroinflammation. FASEB J 25:1556–1566. https://doi.org/10.1096/fj.10-177279
Liang F, Luo C, Xu G, Su F, He X, Long S, Ren H, Liu Y et al (2015) Deletion of aquaporin-4 is neuroprotective during the acute stage of micro traumatic brain injury in mice. Neurosci Lett 598:29–35. https://doi.org/10.1016/j.neulet.2015.05.006
Rama Rao KV, Verkman AS, Curtis KM, Norenberg MD (2014) Aquaporin-4 deletion in mice reduces encephalopathy and brain edema in experimental acute liver failure. Neurobiol Dis 63:222–228. https://doi.org/10.1016/j.nbd.2013.11.018
Verkman AS, Smith AJ, Phuan P-W, Tradtrantip L, Anderson MO (2017) The aquaporin-4 water channel as a potential drug target in neurological disorders. Expert Opin Ther Targets 21:1161–1170. https://doi.org/10.1080/14728222.2017.1398236
Jayakumar AR, Rama Rao KV, Norenberg MD (2015) Neuroinflammation in hepatic encephalopathy: mechanistic aspects. J Clin Exp Hepatol 5:S21–S28. https://doi.org/10.1016/j.jceh.2014.07.006
Rodrigo R, Cauli O, Gomez-Pinedo U et al (2010) Hyperammonemia induces neuroinflammation that contributes to cognitive impairment in rats with hepatic encephalopathy. Gastroenterology 139:675–684. https://doi.org/10.1053/j.gastro.2010.03.040
Santos CL, Bobermin LD, Souza DG, Bellaver B, Bellaver G, Arús BA, Souza DO, Gonçalves CA et al (2015) Lipoic acid and N-acetylcysteine prevent ammonia-induced inflammatory response in C6 astroglial cells: The putative role of ERK and HO1 signaling pathways. Toxicol in Vitro 29:1350–1357. https://doi.org/10.1016/j.tiv.2015.05.023
Dresselhaus EC, Meffert MK (2019) Cellular specificity of NF-κB function in the nervous system. Front Immunol 10:1043. https://doi.org/10.3389/fimmu.2019.01043
Wang X, Yang L, Yang L, Xing F, Yang H, Qin L, Lan Y, Wu H et al (2017) Gypenoside IX suppresses p38 MAPK/Akt/NFκB signaling pathway activation and inflammatory responses in astrocytes stimulated by proinflammatory mediators. Inflammation 40:2137–2150. https://doi.org/10.1007/s10753-017-0654-x
Nito C, Kamada H, Endo H, Narasimhan P, Lee YS, Chan PH (2012) Involvement of mitogen-activated protein kinase pathways in expression of the water channel protein aquaporin-4 after ischemia in rat cortical astrocytes. J Neurotrauma 29:2404–2412. https://doi.org/10.1089/neu.2012.2430
Miller AH, Haroon E, Raison CL, Felger JC (2013) Cytokine targets in the brain: impact on neurotransmitters and neurocircuits. Depress Anxiety 30:297–306. https://doi.org/10.1002/da.22084
De Luca C, Colangelo AM, Alberghina L, Papa M (2018) Neuro-immune hemostasis: homeostasis and diseases in the central nervous system. Front Cell Neurosci 12:459. https://doi.org/10.3389/fncel.2018.00459
Argaw AT, Asp L, Zhang J, Navrazhina K, Pham T, Mariani JN, Mahase S, Dutta DJ et al (2012) Astrocyte-derived VEGF-A drives blood-brain barrier disruption in CNS inflammatory disease. J Clin Invest 122:2454–2468. https://doi.org/10.1172/JCI60842
Butterworth RF (2013) The liver-brain axis in liver failure: neuroinflammation and encephalopathy. Nat Rev Gastroenterol Hepatol 10:522–528. https://doi.org/10.1038/nrgastro.2013.99
Bellaver B, Souza DG, Souza DO, Quincozes-Santos A (2014) Resveratrol increases antioxidant defenses and decreases proinflammatory cytokines in hippocampal astrocyte cultures from newborn, adult and aged Wistar rats. Toxicol in Vitro 28:479–484. https://doi.org/10.1016/j.tiv.2014.01.006
Souza DG, Bellaver B, Bobermin LD, Souza DO, Quincozes-Santos A (2016) Anti-aging effects of guanosine in glial cells. Purinergic Signal 12:697–706. https://doi.org/10.1007/s11302-016-9533-4
Patterson SL (2015) Immune dysregulation and cognitive vulnerability in the aging brain: interactions of microglia, IL-1β, BDNF and synaptic plasticity. Neuropharmacology 96:11–18. https://doi.org/10.1016/j.neuropharm.2014.12.020
Spulber S, Schultzberg M (2010) Connection between inflammatory processes and transmittor function-modulatory effects of interleukin-1. Prog Neurobiol 90:256–262. https://doi.org/10.1016/j.pneurobio.2009.10.015
Takao T, Nagano I, Tojo C, Takemura T, Makino S, Hashimoto K, de Souza EB (1996) Age-related reciprocal modulation of interleukin-1βand interleukin-1 receptors in the mouse brain-endocrine-immune axis. Neuroimmunomodulation 3:205–212. https://doi.org/10.1159/000097272
Agusti A, Cauli O, Rodrigo R, Llansola M, Hernandez-Rabaza V, Felipo V (2011) p38 MAP kinase is a therapeutic target for hepatic encephalopathy in rats with portacaval shunts. Gut 60:1572–1579. https://doi.org/10.1136/gut.2010.236083
Bachstetter AD, Van Eldik LJ (2010) The p38 MAP kinase family as regulators of proinflammatory cytokine production in degenerative diseases of the CNS. Aging Dis 1:199–211
Rosciszewski G, Cadena V, Murta V, Lukin J, Villarreal A, Roger T, Ramos AJ (2018) Toll-like receptor 4 (TLR4) and triggering receptor expressed on myeloid cells-2 (TREM-2) activation balance astrocyte polarization into a proinflammatory phenotype. Mol Neurobiol 55:3875–3888. https://doi.org/10.1007/s12035-017-0618-z
Wilhelm I, Nyúl-Tóth Á, Kozma M, Farkas AE, Krizbai IA (2017) Role of pattern recognition receptors of the neurovascular unit in inflamm-aging. Am J Physiol Heart Circ Physiol 313:H1000–H1012. https://doi.org/10.1152/ajpheart.00106.2017
Hanke ML, Kielian T (2011) Toll-like receptors in health and disease in the brain: mechanisms and therapeutic potential. Clin Sci 121:367–387. https://doi.org/10.1042/CS20110164
Akira S, Uematsu S, Takeuchi O (2006) Pathogen recognition and innate immunity. Cell 124:783–801. https://doi.org/10.1016/j.cell.2006.02.015
Gárate I, García-Bueno B, Madrigal JLM, Bravo L, Berrocoso E, Caso JR, Micó JA, Leza JC (2011) Origin and consequences of brain toll-like receptor 4 pathway stimulation in an experimental model of depression. J Neuroinflammation 8:151. https://doi.org/10.1186/1742-2094-8-151
Letiembre M, Hao W, Liu Y, Walter S, Mihaljevic I, Rivest S, Hartmann T, Fassbender K (2007) Innate immune receptor expression in normal brain aging. Neuroscience 146:248–254. https://doi.org/10.1016/j.neuroscience.2007.01.004
Kong H, Zeng X-N, Fan Y, Yuan ST, Ge S, Xie WP, Wang H, Hu G (2014) Aquaporin-4 knockout exacerbates corticosterone-induced depression by inhibiting astrocyte function and hippocampal neurogenesis. CNS Neurosci Ther 20:391–402. https://doi.org/10.1111/cns.12222
Skucas VA, Mathews IB, Yang J, Cheng Q, Treister A, Duffy AM, Verkman AS, Hempstead BL et al (2011) Impairment of select forms of spatial memory and neurotrophin-dependent synaptic plasticity by deletion of glial aquaporin-4. J Neurosci 31:6392–6397. https://doi.org/10.1523/JNEUROSCI.6249-10.2011
Galland F, Negri E, Da Ré C et al (2017) Hyperammonemia compromises glutamate metabolism and reduces BDNF in the rat hippocampus. Neurotoxicology 62:46–55. https://doi.org/10.1016/j.neuro.2017.05.006
Dhanda S, Gupta S, Halder A, Sunkaria A, Sandhir R (2018) Systemic inflammation without gliosis mediates cognitive deficits through impaired BDNF expression in bile duct ligation model of hepatic encephalopathy. Brain Behav Immun 70:214–232. https://doi.org/10.1016/j.bbi.2018.03.002
Ahmad AS, Zhuang H, Doré S (2006) Heme oxygenase-1 protects brain from acute excitotoxicity. Neuroscience 141:1703–1708. https://doi.org/10.1016/j.neuroscience.2006.05.035
Chen-Roetling J, Kamalapathy P, Cao Y, Song W, Schipper HM, Regan RF (2017) Astrocyte heme oxygenase-1 reduces mortality and improves outcome after collagenase-induced intracerebral hemorrhage. Neurobiol Dis 102:140–146. https://doi.org/10.1016/j.nbd.2017.03.008
Yu X, Song N, Guo X, Jiang H, Zhang H, Xie J (2016) Differences in vulnerability of neurons and astrocytes to heme oxygenase-1 modulation: implications for mitochondrial ferritin. Sci Rep 6:24200. https://doi.org/10.1038/srep24200
Kim Y, Park J, Choi YK (2019) The role of astrocytes in the central nervous system focused on BK channel and heme oxygenase metabolites: a review. Antioxidants 8:121. https://doi.org/10.3390/antiox8050121
Wegiel B, Nemeth Z, Correa-Costa M, Bulmer AC, Otterbein LE (2014) Heme oxygenase-1: a metabolic nike. Antioxid Redox Signal 20:1709–1722. https://doi.org/10.1089/ars.2013.5667
Görg B, Bidmon H-J, Häussinger D (2013) Gene expression profiling in the cerebral cortex of patients with cirrhosis with and without hepatic encephalopathy. Hepatology 57:2436–2447. https://doi.org/10.1002/hep.26265
Oenarto J, Karababa A, Castoldi M, Bidmon HJ, Görg B, Häussinger D (2016) Ammonia-induced miRNA expression changes in cultured rat astrocytes. Sci Rep 6:18493. https://doi.org/10.1038/srep18493
Warskulat U, Görg B, Bidmon H-J, Müller HW, Schliess F, Häussinger D (2002) Ammonia-induced heme oxygenase-1 expression in cultured rat astrocytes and rat brain in vivo. Glia 40:324–336. https://doi.org/10.1002/glia.10128
Görg B, Karababa A, Häussinger D (2018) Hepatic encephalopathy and astrocyte senescence. J Clin Exp Hepatol 8:294–300. https://doi.org/10.1016/j.jceh.2018.05.003
Kuilman T, Michaloglou C, Mooi WJ, Peeper DS (2010) The essence of senescence. Genes Dev 24:2463–2479. https://doi.org/10.1101/gad.1971610
Nagelhus EA, Amiry-Moghaddam M, Bergersen LH, Bjaalie JG, Eriksson J, Gundersen V, Leergaard TB, Morth JP et al (2013) The glia doctrine: addressing the role of glial cells in healthy brain ageing. Mech Ageing Dev 134:449–459. https://doi.org/10.1016/j.mad.2013.10.001
Salminen A, Ojala J, Kaarniranta K, Haapasalo A, Hiltunen M, Soininen H (2011) Astrocytes in the aging brain express characteristics of senescence-associated secretory phenotype. Eur J Neurosci 34:3–11. https://doi.org/10.1111/j.1460-9568.2011.07738.x
Chen QM (2000) Replicative senescence and oxidant-induced premature senescence. Beyond the control of cell cycle checkpoints. Ann N Y Acad Sci 908:111–125. https://doi.org/10.1111/j.1749-6632.2000.tb06640.x
Umapathy S, Dhiman RK, Grover S, Duseja A, Chawla YK (2014) Persistence of cognitive impairment after resolution of overt hepatic encephalopathy. Am J Gastroenterol 109:1011–1019. https://doi.org/10.1038/ajg.2014.107
Bajaj JS, Schubert CM, Heuman DM, Wade JB, Gibson DP, Topaz A, Saeian K, Hafeezullah M et al (2010) Persistence of cognitive impairment after resolution of overt hepatic encephalopathy. Gastroenterology 138:2332–2340. https://doi.org/10.1053/j.gastro.2010.02.015
Braissant O, McLin VA, Cudalbu C (2013) Ammonia toxicity to the brain. J Inherit Metab Dis 36:595–612. https://doi.org/10.1007/s10545-012-9546-2
Code Availability
Not applicable.
Funding
This study was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS), Universidade Federal do Rio Grande do Sul, and Instituto Nacional de Ciência e Tecnologia para Excitotoxicidade e Neuroproteção (INCTEN/CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All animal experiments were performed in accordance with the National Institute of Health (NIH) Guide for the Care and Use of Laboratory Animals and Brazilian Society for Neuroscience and Behavior recommendations for animal care. The experimental protocols were approved by the Federal University of Rio Grande do Sul Animal Care and Use Committee (process number 21215).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bobermin, L.D., Roppa, R.H.A., Gonçalves, CA. et al. Ammonia-Induced Glial-Inflammaging. Mol Neurobiol 57, 3552–3567 (2020). https://doi.org/10.1007/s12035-020-01985-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-020-01985-4