Abstract
Ascorbic acid (AA), the reduced form of vitamin C, acts as a neuroprotector by eliminating free radicals in the brain. Sodium/vitamin C co-transporter isoform 2 (SVCT2) mediates uptake of AA by neurons. It has been reported that SVCT2 mRNA is induced in astrocytes under ischemic damage, suggesting that its expression is enhanced in pathological conditions. However, it remains to be established if SVCT expression is altered in the presence of reactive astrogliosis generated by different brain pathologies. In the present work, we demonstrate that SVCT2 expression is increased in astrocytes present at sites of neuroinflammation induced by intracerebroventricular injection of a GFP-adenovirus or the microbial enzyme, neuraminidase. A similar result was observed at 5 and 10 days after damage in a model of traumatic injury and in the hippocampus and cerebral cortex in the in vivo kindling model of epilepsy. Furthermore, we defined that cortical astrocytes maintained in culture for long periods acquire markers of reactive gliosis and express SVCT2, in a similar way as previously observed in situ. Finally, by means of second harmonic generation and 2-photon fluorescence imaging, we analyzed brain necropsied material from patients with Alzheimer’s disease (AD), which presented with an accumulation of amyloid plaques. Strikingly, although AD is characterized by focalized astrogliosis surrounding amyloid plaques, SVCT2 expression at the astroglial level was not detected. We conclude that SVCT2 is heterogeneously induced in reactive astrogliosis generated in different pathologies affecting the central nervous system (CNS).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin C is known for its role as an intracellular antioxidant, inhibiting lipid peroxidation through alpha-tocopherol recycling and scavenging free radicals that are produced in cells with high oxidative metabolism [1, 2]. In humans, vitamin C is obtained from the diet and is mostly available in its reduced form (95%) known as ascorbic acid (AA). Vitamin C oxidation also yields low levels (5%) of dehydroascorbic acid (DHA) [3]. Cells can capture both chemical forms through specific and non-overlapping transport systems [4].
In the brain, AA is taken up by the sodium/vitamin C co-transporter 2 (SVCT2), and several studies support the expression of SVCT2 in cortical, hippocampal and hypothalamic neurons in adults [5,6,7,8,9,10]. During development, SVCT2 has been detected in the ventricular and subventricular areas of embryonic rat brains [11, 12]. Postnatally, SVCT2 expression is induced in the cerebral and cerebellar cortex during the first 2 weeks, and its function is regulated by co-expression of a short isoform (SVCT2 short) [9, 13, 14]. SVCT2 has also been detected in microglia [7, 15], hypothalamic tanycytes [6], cells from the choroid plexus [2, 5, 7, 16, 17], and Schwann cells [18]. In adult brains, SVCT2 protein is not expressed in astrocytes, but its mRNA is detected in astrocytes at the marginal zone from the entorhinal cortex [19]. In contrast, SVCT2 mRNA is induced in astrocytes at different areas of the brain parenchyma under pathophysiological conditions, such as ischemia induced by occlusion of the middle cerebral artery [20]. To date, it remains to be established if different pathological conditions affecting the brain can induce SVCT2 expression in astrocytes.
Reactive astrocytes are generated following brain injury, neuroinflammation, stroke, aging, or neurodegenerative diseases. In these pathologies, production of reactive oxygen species is increased at different levels, which, in turn, might stimulate increased oxidized vitamin C (DHA) uptake by astrocytes in order to prevent DHA from reaching inappropriate concentrations that could impact neuronal metabolism [21] and potentially promote cell death [10].
In the present work, we report the expression and localization of SVCT2 in the presence of different brain pathologies. Similar results are observed in cultured astrocytes. Finally, we demonstrate that SVCT2 expression shows a different pattern in reactive astrocytes in brains from subjects with Alzheimer’s disease (AD).
Materials and Methods
Animals
The animals were housed in conditions of controlled light (12-h light/dark cycle) and temperature (20–24 °C) and received a standard diet and water ad libitum. The experiments were performed in accordance with a protocol approved by the Committee for Animal Experimentation of the University of Concepción.
Disruption of the Ventricular Wall Using Neuraminidase
Neuraminidase was injected in the right lateral ventricle of Sprague-Dawley rats (200–250 g) using a pump, via a stereotaxically positioned cannula (0.5 mm posterior from the bregma, 1.5 mm lateral from the sagittal suture, and 3.5 mm ventral from the dura). A single dose of 10 μg of neuraminidase from Clostridium perfringens (catalogue number 107590, 1995; Boehringer Mannheim, Biochemica, Germany) dissolved in 20 μL of distilled water was administered to 12 rats at a rate of 2 μL/min for 10 min. The rats were sacrificed at 3 days after the administration of neuraminidase. Control rats were injected with 20 μL of distilled water. Untreated rats were also used. The animals were transcardially perfused with 0.9% NaCl followed by Bouin’s fixative. The brains were dissected out and immersed in the same fixative for 2 days. Later they were dehydrated, embedded in paraffin, and cut in either transversal or sagittal sections of 10-μm thickness.
Induction of Brain Stab Wounds
Adult male rats (200–250 g) were deeply anesthetized with an intraperitoneal injection of a mixture of ketamine (50 mg/kg) and xylazine (10 mg/kg). After the rats were positioned in a stereotaxic apparatus (David Kopf, Tujunga, CA), a mid-sagittal incision was made in the scalp to expose the skull, and a 4-mm long para-sagittal fragment of the skull was removed with a dental drill. A unilateral stab wound of the forebrain was made by inserting a microdissecting knife through the opening, 1 mm rostral to the bregma, to a depth of 4 mm from the dura and slowly moving the knife 4 mm caudally, transecting the underlying white matter. The skull was sealed with bone wax, and the skin closed with wound clips. All animals recovered uneventfully from this procedure and were evaluated at 5 and 10 days after surgical intervention.
Intraventricular Injection of Adenoviral Particles
Deeply anesthetized rats were placed on a stereotaxic frame, and the skin over the cranium was removed to expose the junction of the sagittal and coronal sutures. A small borehole (1 mm in diameter) through the skull of the right hemisphere was used to grind away the bone and expose the dural membrane at the following coordinates: 3.14 mm caudal and 4.2 mm lateral to the bregma. Adenoviral particles (20 μL; 2 × 109 IFU/mL) carrying the green fluorescent protein (pDC311U6-GFP) were slowly injected manually over a period of 2 min, using a frame-fixed 50-μL Hamilton syringe at a depth of 4.2 mm from the dura into the lateral ventricle.
Kindling Protocol
Epileptogenesis was induced through a modified kindling protocol, as we described previously (Morales et al., 2014). Briefly, adult male Sprague-Dawley rats were anesthetized, and a stimulation electrode was implanted by stereotaxic surgery into the right basolateral amygdale complex (BLA) for electric stimulation. Two electrodes for cortical recording were implanted bilaterally into the primary motor cortex. After surgery, the rats had at least 1 week of recovery period before the kindling procedure was initiated. The kindling protocol consists of ten current pulses at subthreshold after-discharge intensity daily over a period of 3 days. Progression of epileptogenesis was assessed by EEG recordings of after-discharges, and convulsive behaviors evaluated according to the Racine scale (Racine 1972). Rats were considered as fully kindled when at least three consecutive generalized epileptic seizures were reached and long-term repetitive after-discharges occurred. Under these conditions, the cortical and mesolimbic structures of fully kindled rats were considered epileptic tissue, including hippocampal formation [22,23,24,25].
Astrocyte Primary Cultures
The cells were obtained from cerebral cortex samples of 1-day-old postnatal rats. The dissection was carried out with the samples immersed in dissection buffer containing 10 mM HEPES (pH 7.4, 320 mOsm/L). Tissues were incubated with 0.25% trypsin-0.2% EDTA (w/v) for 15 min at 37 °C, and then triturated to homogeneity with a fire-polished Pasteur pipette. Cells were seeded at 5 × 105 cells/cm2 in culture dishes and cultured in D-MEM high glucose supplemented with 10% fetal bovine serum, 2 mM L-glutamine, 100 U/mL penicillin, and 100 mg/mL streptomycin. The cell cultures were incubated in 5% CO2 in a humidified environment at 37 °C. The cultures reached confluence within 2 weeks when each 60-mm dish contained approximately 3 × 106 cells. All cells were used for experiments after 30 days in vitro (DIV).
Immunofluorescence and Spectral Confocal Microscopy
Cells were grown on coverslips and fixed with 4% (w/v) paraformaldehyde for 30 min. Additionally, rat brain samples were dissected and fixed directly by immersion or fixed in situ by vascular perfusion with 4% (w/v) paraformaldehyde for 12 h. Samples of post-mortem human brain tissue from healthy controls (Caucasian males 92 and 73 years) and AD patients (Caucasian males, 77 and 88 years and Caucasian females, 72 and 86 years) were obtained from the Harvard Brain Tissue Bank, and fixed directly by immersion in 4% (w/v) paraformaldehyde. The use of unidentified brain tissue samples was exempted under the regulations of the Office for the Protection of Research Subjects (UIC). Thick transverse sections (40 μm) were cut with a cryostat or a vibratome, and processed for free-floating immunostaining. For immunohistochemical co-localization analyses, we used the following antibodies and dilutions: goat anti-SVCT2 (G19 for rat SVCT2 or A16 for human SVCT2, 1:50, Santa Cruz Biotechnology, Santa Cruz, CA), rabbit anti-GFAP (glial fibrillary acidic protein; 1:50 (tissue) or 1:400 (cells), Dako, Campintene, CA), and mouse anti-vimentin (1:100; Boehringer Mannheim, Mannheim, Germany). The antibodies were diluted in Tris/HCl buffer (pH 7.8) containing 8.4 mM sodium phosphate, 3.5 mM potassium phosphate, 120 mM NaCl, and 1% BSA. Sections were incubated with the antibodies overnight at 20 °C in a humidified chamber. After extensive washing, the brain sections were incubated for 2 h at 20 °C with Cy2-, Cy3- or Cy5-labeled secondary antibodies (1:200; Jackson Immuno Research, West Grove, PA). Nuclei were counterstained with Topro-3 or Hoechst 33342 (Invitrogen, Rockville, MD). The slides were analyzed using confocal laser microscopy (LSM 780 NLO, Zeiss, Germany).
Results
GFP-Adenovirus Transduction-Induced Reactive Gliosis and SVCT2 Expression in Astrocytes of the Cerebral Cortex, Callosum Corpus and Hippocampus
Adenoviral infection in the brain and spinal cord induced activation of astrocytes with the typical molecular and morphological features of reactive astrocytes, manifested as an increase in the expression of intermediate filaments, such as vimentin and GFAP (Pekny et al., 2014). We, therefore, investigated whether SVCT2 expression (red) was induced in reactive astrocytes (GFAP positive, blue) of the brain after injection with GFP-adenovirus (green) (Fig. 1). Strong expression of GFP was observed at the pial surface of the cerebral cortex and cells from the callosum corpus (Fig. 1c–m). Immunostaining against GFAP revealed a high density of astrocytes in the area near the site of viral infection at the cerebral cortex, such that defining an independent cell was difficult due to overlapping in the astrocytic processes (Fig. 1c, f; arrows). Similarly, intense immunoreactivity of SVCT2 was detected in a polarized distribution below the transduced pial surface (Fig. 1d, g, asterisks), presenting strong co-localization with those areas where most of the GFAP signal was observed (Fig. 1e, h–i; arrowheads). In the callosum corpus, we observed numerous cells that expressed GFP and just a few that were not efficiently transduced with the adenovirus (Fig. 1j; arrows and arrowheads, respectively). GFAP staining revealed the presence of numerous fibrous astrocytes scattered throughout the callosum corpus (Fig. 1j). Immunostaining against SVCT2 showed a similar pattern than previously observed, where SVCT2 is expressed in both GFP-positive and GFP-negative cells (Fig. 1k; arrows and arrowheads, respectively). However, co-localization analysis of SVCT2 and GFAP showed that a high number of fibrous astrocytes are SVCT2-positive (Fig. 1l–m). Normal brains without GFP-adenovirus injection were used as controls (Fig. 1j1–l1). Finally, we detected co-localization of SVCT2 and GFAP in astrocytes (GFP-Ad negative) at the marginal zone (layer I) of the cerebral cortex (Fig. 1n–q; arrows and inset). Normal brains without GFP-adenovirus injection were used as controls. A weak immunoreaction for GFAP and SVCT2 was detected in astrocytes at the marginal zone (Fig. 1n1–q1).
Expression of SVCT2 in astrogliosis generated by adenoviral transduction in the brain. a Schematic representation of GFP-adenovirus (GFP-Ad) packaging in the 293A cell line. b Intracerebroventricular injection of GFP-Ad and immunohistochemical analysis in the cerebral cortex and the corpus callosum (inset). c–q. Frontal sections of rat brains were transduced with GFP-Ad (green) and immunostained with anti-SVCT2 and anti-GFAP antibodies followed by secondary antibodies labeled with Cy3 (red) or Cy5 (blue), respectively. Topro-3 was used for nuclear staining (blue). Adenoviral transduction and GFP expression induced an increase in GFAP immunostaining in the marginal layer of the cerebral cortex (arrowheads in c and f), reflecting a high degree of reactive gliosis generated by the virus. SVCT2 was detected in those areas with higher GFAP immunoreactivity (asterisks in d and g, and arrowheads in e and h–i). The corpus callosum transduced with GFP-Ad presented numerous fibrous astrocytes both negative and positive for GFP and co-localizing with GFAP and SVCT2 (arrows and arrowheads in j–m). Normal brains without Ad-GFP injection were used as controls (j1–l1). Co-distribution of SVCT2 and GFAP was also observed in astrocytes (Ad-GFP negative) in the marginal zone. Normal brains without Ad-GFP injection were used as controls (n1–q1). Cx cerebral cortex, CC corpus callosum. Magnification in c–h and j–q, ×200. In i, ×420
In order to evaluate if reactive gliosis and SVCT2 induction after transduction of GFP-adenovirus is conserved in other areas near the callosum corpus, we performed a similar analysis in the hippocampus (Fig. 2a–f). An intense immunoreactivity to GFAP was observed, revealing a high number of stellate cells with overlapping cellular processes (Fig. 2a, d; arrows). Intense immunoreactivity of SVCT2 was also observed in this area, displaying a stellate form in many cases (Fig. 2b, e; arrows), and a ring type concentration in the cellular body in others (Fig. 2e; arrowheads). Co-localization analysis showed that most astrocytes expressed SVCT2 (Fig. 2c, f; arrows), and just a few SVCT2-positive cells were negative for GFAP (Fig. 2f; arrowheads). Normal brains without GFP-adenovirus injection were used as controls (d1–f1).
Adenoviral transduction in the corpus callosum stimulates intense reactive astrogliosis positive for SVCT2 in the hippocampus. a–c. Frontal sections of rat brains transduced with GFP-adenovirus (GFP-Ad, green) and immunostained with anti-SVCT2 and anti-GFAP antibodies followed by secondary antibodies labeled with Cy3 (red) or Cy5 (blue), respectively. d–f Magnifications of the insets in a–c, respectively. Increased immunoreactivity of GFAP was observed in the hippocampus near the Ad-GFP transduction zone in the corpus callosum. Most reactive astrocytes showed an intense co-localization with anti-SVCT2 (arrows), and only few cells were positive for anti-SVCT2 but not for anti-GFAP (arrowheads). Normal brains without Ad-GFP injection were used as controls (d1–f1). CC corpus callosum. Magnification in a–c, ×200. In d–f, ×400
Together these data confirmed the presence of pronounced reactive gliosis after injection of GFP-adenovirus, characterized by increased immunostaining for GFAP in areas surrounding the sites of adenoviral transduction, such as the cerebral cortex and hippocampus, or in the same zone of adenoviral transduction, such as the callosum corpus. In these samples, numerous reactive astrocytes presented a typical stellate morphology with thick overlapping processes that were SVCT2-positive, suggesting an induction of this transporter in response to the astrocytic activation. Moreover, some astrocytes from areas of white matter near the pial surface of the cerebral cortex also expressed SVCT2, although they were away from the area of adenoviral transduction.
Astrogliosis Generated During the Intracerebral Injection of Microbial Neuraminidase-Induced SVCT2 Expression in Astrocytes of the Cerebral Cortex
Next, we studied if similar SVCT2 induction was observed in astrocytes after injection (3 days) of low doses of neuraminidase into only one lateral ventricle (Fig. 3a). For this, we performed a co-localization analysis between SVCT2 (green) and two markers of reactive gliosis, vimentin (red) and GFAP (blue) (Fig. 3b–q). Intracerebroventricular injection of neuraminidase produces an intense co-localization between GFAP and vimentin in the marginal astrocytes of the cortex (Cx) (Fig. 3b, f; arrows). In contrast, GFAP, but not vimentin was detected in cells localized throughout the thickness of the cerebral cortex (Fig. 3b, f; arrowheads). Similarly, SVCT2 showed a strong immunoreactivity in areas near the external cortex, co-localizing with vimentin (Fig. 3c, g; arrows). However, no co-localization between SVCT2 and the glial markers was detected in the remaining areas within the cerebral cortex (Fig. 3c–e, g–i; arrowheads). Normal brains without neurominidase injection were used as controls (Fig. 3b1–d1). A similar analysis performed at the level of the ependymal wall from the lateral ventricle, opposite to the site of neuraminidase injection (non-injected lateral ventricle) (Fig. 3j–q; arrows), showed an integral ependymal wall (Ep) that was positive for vimentin. In addition, the SVZ was positive for GFAP with just a few cells also double positive for vimentin (Fig. 3j, n; arrowheads). Moreover, SVCT2 exhibited a strong pattern of co-localization with vimentin at the ependymal wall (Fig. 3k, o; Ep), and few cells at the neurogenic niche from the SVZ were positive for SVCT2, GFAP, and vimentin expression (Fig. 3k–m, o–q; arrowheads).
SVCT2 is induced in reactive astrogliosis generated by intracerebroventricular injection of neuraminidase. Frontal sections of rat brains injected with neuraminidase (3 days) and immunostained with anti-SVCT2, anti-GFAP and anti-vimentin antibodies followed by secondary antibodies labeled with Cy2 (green), Cy3 (red) or Cy5 (blue), respectively. a Schematic representation of the site of neuraminidase injection at the level of the lateral ventricle. b–e Region of the cerebral cortex showing gliosis that was positive for GFAP and vimentin at the marginal zone, together with expression of SVCT2 (arrows). Normal brains without neurominidase injection were used as controls (b1–d1). f-i. Magnifications of the insets in b–e, respectively. j–m. Region of the non-injected lateral ventricle showing an intense co-localization between SVCT2 and vimentin in the intact ependymal wall (Ep), but without co-localization between SVCT2 and GFAP in the subventricular zone (SVZ) or brain parenchyma. n–q Magnifications of j–m, respectively. In these images, it is possible to observe the neurogenic niche and lateral ventricle, showing co-localization between SVCT2 and vimentin in the Ep, and co-localization between SVCT2 and GFAP in astrocytes at the SVZ (arrowheads). Cx cerebral cortex, LV lateral ventricule, Ep ependymal wall, SVZ subventricular zone. Magnification in b–e and j–m, ×250. In f–i and n–q, ×450
SVCT2 Was Induced in Reactive Astrocytes of the Corpus Callosum at 5 and 10 days Following Cortical Injury
Rats were subjected to cortical injury, and induction of SVCT2 expression was evaluated in brain samples at 5 and 10 days post-injury (Fig. 4a). In the damaged cerebral hemisphere, a strong immunoreactivity against GFAP (red) was detected in the corpus callosum at 5 days post-trauma, with overlapping astrocytic processes and, consequently, poor definition of individual astrocytic domains (Fig. 4b, e). A positive signal for SVCT2 (green) was detected in ependymal cells in the lateral ventricle (Ep), and in also in some GFAP + cells in the corpus callosum (Fig. 4c–d, f–g; arrows). In contrast, a similar analysis performed in the corpus callosum from the opposite hemisphere to which the injury was induced (i.e., control cortex), showed a weaker immunostaining against GFAP and a negative signal for SVCT2 (Fig. 4h–j). Although no significant changes in GFAP immunoreactivity were detected in astrocytes in the corpus callosum at 10 days post-trauma (Fig. 4k, n), a clear increase in the expression of SVCT2 and its co-localization with the glial marker were observed (Fig. 4l–m, o–p; arrows). Together our data indicate that reactive gliosis at the corpus callosum, produced by cortical injury, also induces SVCT2 expression in reactive astrocytes.
Expression of SVCT2 is induced in reactive astrocytes in the corpus callosum from brains subjected to cortical injury. Frontal sections of the lateral ventricle and corpus callosum from rat brains, which were damaged with a pin at the cerebral cortex and then maintained 5 and 10 days post-injury (5-DPI and 10-DPI, respectively). Brain samples were immunostained with anti-GFAP and anti-SVCT2 antibodies followed by secondary antibodies labeled with Cy2 (green) and Cy3 (red), respectively. a. Schematic representation of the cortical injury protocol. b–f, k–o General view of the traumatized region, showing immunostaining against GFAP and SVCT2 in astrocytes at the corpus callosum from 5-DPI and 10-DPI animals, respectively. g Magnification of the inset in d. h–j Corpus callosum in the opposite hemisphere to which the injury (control cortex) was induced at 5-DPI. At 5-DPI, the corpus callosum from the injured hemisphere presented a strong immunoreactivity against GFAP, corresponding to intense reactive astrogliosis with increased expression of SVCT2 in reactive astrocytes (arrows). No increase in GFAP immunostaining or SVCT2 induction was detected in the corpus callosum from the non-injured hemisphere at 5-DPI (h–j). k–p GFAP and SVCT2 expression is mostly evident in the corpus callosum from 10-DPI animals (k, l, and n, o). M. GFAP/SVCT2 merged images. p Magnification of the inset in m. GFAP/SVCT2 colocalization (arrows). CC corpus callosum, CP choroid plexus, LV lateral ventricle, Ep ependymal wall. Magnification in b–c, e–f, h–j, k–l, and n–o, ×180. In d and m, ×350. In g and p, ×480
SVCT2 Expression in Reactive Astrocytes Is Observed in Kindled Hippocampal and Cerebral Cortex Slices
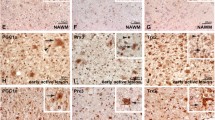
In order to analyze if the reactive astrogliosis generated in the in vivo kindling model of epilepsy is accompanied with an SVCT2 induction, we evaluated the co-localization of SVCT2, GFAP, and vimentin in these samples (Fig. 5). In the hippocampus of the control brain, we detected many thin astrocytes positive for GFAP (Fig. 5i; insert and arrow). Vimentin showed a low level of expression in GFAP-positive cells (Fig. 5j; insert and arrow); a high intensity of immunoreactivity was associated with capillaries (Fig. 5j; arrowhead). However, only a few cells were triple positive for GFAP, vimentin, and SVCT2 (Fig. 5k–l; arrows and insert). Kindled brains also showed a more intense immunoreaction to GFAP as well as typical hypertrophic morphology of the reactive astrocytes in the hippocampus and cerebral cortex as compared to that observed in the control animals (Fig. 5a, e; insert and arrow). Similar to the control samples, vimentin immunoreaction was principally associated with capillaries in both brain regions analyzed (Fig. 5b, f; arrowheads) and not in the reactive astrogliosis (Fig. 5b; arrow and insert). However, in the kindling model, we detected an intense immunofluorescence for SVCT2 in many hypertrophic reactive astrocytes of the hippocampus and cerebral cortex (Fig. 5c–d, g–h; arrow in insert). Thus, in the hippocampus and cerebral cortex of kindled animals, intense astrogliosis is accompanied with an induction in SVCT2 expression.
Reactive astrogliosis present in epileptic brain is accompanied with an intense expression of SVCT2. Kindled hippocampal and cerebral cortex slices were immunostained with anti-SVCT2, anti-GFAP and anti-vimentin antibodies followed by secondary antibodies labeled with Cy2 (green), Cy3 (red) or Cy5 (white), respectively. a–h In the kindled brain, numerous reactive hypertrophic astrocytes with an intensely positive immunoreaction for GFAP and SVCT2 were detected (inserts and arrows). i–l Control brain showing a poor colocalization between SVCT2 and the reactive astrogliosis marker (GFAP, arrows). In both control and kindled brains, a high immunoreactivity for vimentin was associated with capillaries and not reactive astrogliosis (arrowheads). Magnification in a–l, ×200. Insets, ×450
SVCT2 Is Induced in Astrocytes Maintained in Culture for Long Periods
It has been reported that astrocytes at 22 DIV, but not 7 DIV, uptake AA by a mechanism that requires sodium (Astuya et al., 2005). By means of immunocytochemical analysis, we determined the expression of SVCT2 in primary cultures of cortical astrocytes maintained for 15 DIV. These cultures showed the expression of GFAP and vimentin, but not SVCT2 (Fig. 6a–d). Next, we determined the expression of SVCT2 and its subcellular localization in primary cultures of cortical astrocytes maintained for 30 DIV (Fig. 6e–j). These cultures conserved the expression of GFAP (Fig. 6e; white) and the facilitative glucose transporter, GLUT1, that also mediates uptake of DHA (Fig. 6h; green), which is in agreement with previous reports (Astuya et al., 2005; Cisternas et al., 2013). However, these cultures also presented positive immunostaining against SVCT2 (green) near the nucleus and in the plasma membrane (Fig. 6f–g; asterisks and arrows, respectively). These cells were also positive for the marker of reactive gliosis, vimentin (Fig. 6i–j; white). These results indicate that astrocytes maintained in culture for long periods express markers of reactive astrogliosis, but also express SVCT2, which is properly localized at the plasma membrane.
Cortical astrocytes maintained in culture for long periods express SVCT2 and markers of reactive gliosis. Rat brain astrocytes cultured for 15 days (a–d) and 30 days in vitro (DIV) (e–j) were immunostained using anti-GFAP, anti-vimentin, anti-SVCT2 and anti-GLUT1 antibodies followed by secondary antibodies labeled with Cy2 (gray) and Cy3 (green). Hoechst was used for nuclear staining (blue). Under these conditions, cortical astrocytes expressed GFAP/vimentin and conserved the expression of the facilitative glucose transporter, GLUT1. The expression of SVCT2 was induced in 30 DIV astrocytes (f–g, asterisks and arrows, respectively). Scale bars in a–j: 10 μM
Reactive Astrogliosis in the Brain of AD Patients Is Not Related with Induction of SVCT2 Expression
Second harmonic generation (SHG) and two photon excited fluorescence imaging were conducted in post-mortem human brain tissue samples obtained from healthy and AD patients. This technology allowed us to detect the presence of amyloid plaques in the brains of AD patients (Fig. 7a; arrow), and their absence in the brains of healthy controls (Fig. 7h). Immunostaining against GFAP showed moderate, focalized reactive astrogliosis, with the astrocytic processes intimately associated with the amyloid plaques (Fig. 7b, e; arrows). SVCT2 immunoreactivity was detected in the neuropil from the brain parenchyma surrounding the amyloid plaques (Fig. 7c, f; arrows). However, no apparent co-localization of SVCT2 and GFAP was evident (Fig. 7d, g; arrows and insert). In contrast, control samples showed positive immunostaining against GFAP in astrocytes dispersed throughout the brain parenchyma without overlapping cellular processes (Fig. 7i). Similar to the AD samples, SVCT2 distribution was observed at the neuropil, and no evident co-localization with GFAP was observed in control brain samples (Fig. 7j–k; insert). Our results indicate that moderate astrogliosis observed in post-mortem human brain tissue samples from AD patients does not induce expression of SVCT2 in reactive astrocytes surrounding the amyloid plaque. Furthermore, SVCT2 is not expressed in astrocytes of human brain tissue from healthy patients, which is consistent with that observed in other species, such as rat and mouse.
SVCT2 is not induced in the focal astrogliosis observed in brain samples obtained from AD patients. a–k Frontal sections of the cerebral cortex in post-mortem biopsies from healthy (control) and AD patients were immunostained with anti-SVCT2 and anti-GFAP antibodies followed by secondary antibodies labeled with Cy2 (green) and Cy3 (red), respectively. Samples were analyzed using second harmonic generation and two photon excited fluorescence imaging for detection of amyloid plaques. In the brains of AD patients, GFAP-positive reactive astrocytes surrounded and isolated amyloid plaques from the neuronal parenchyma (arrows). However, astrocytes did not show positive immunostaining against SVCT2 (arrows and insert). No amyloid plaques were detected in the brains from control patients, and GFAP immunoreactivity showed that astrocytes are scattered throughout the parenchyma without any apparent formation of cell aggregates, and no co-localization with SVCT2 (insert). Scale bars in a–k: 20 μM
Discussion
Here, we have demonstrated for the first time that the sodium/vitamin C co-transporter, SVCT2, is expressed in reactive astrocytes positive for GFAP and/or vimentin in different brain regions from animals subjected to neuroinflammation induced by viral or bacterial infection, brain injury due to parenchymal damage and in the kindled brain. In addition, we detected expression of SVCT2 in astrocytes maintained in culture for long periods (1 month), which promotes activation of these cells. Finally, we reported that SVCT2 induction was not observed in focal astrogliosis surrounding amyloid plaques in brain tissue samples obtained from AD patients.
Growing evidence indicates that defects in astrocyte function and/or altered cooperation between astrocytes and neurons may produce neuronal death, and it has been proposed that an increase or re-establishment of astrocytic functions might represent an important neuroprotective strategy [26,27,28,29]. These neuroprotective strategies are related, among others, with an increase in the antioxidant capacity of reactive astrocytes in vitro.
SVCT2 protein is widely expressed and mediates uptake of the reduced form of vitamin C, AA, which is a potent, soluble antioxidant [2, 5, 30, 31]. In the CNS, the expression and function of SVCT2 in neurons allow the maintenance of intracellular AA concentrations of ~ 10 mM, which constitutes the major non-enzymatic antioxidant in these cells [32]. By contrast, glutathione is the main antioxidant molecule in astrocytes from normal brain, and AA concentrations of ~ 1 mM have been detected [32]. These low intracellular levels of AA are due to the absence of SVCT2 in most astrocytes under physiological conditions [7, 19, 20, 33]. In this context, it has been reported that SVCT2 is expressed in astrocytes at the neurogenic niche from lateral ventricle [34], similar to that observed in the present work. In addition, in situ hybridization studies have shown that some astrocytes at the marginal zone from the entorhinal cortex are positive for SVCT2 mRNA expression [19]. In our analysis, astrocytes from the marginal zone were the only GFAP-positive cells that co-localized with SVCT2 in a region of the cerebral cortex that was negative for GFP-adenovirus transduction. These cells may need effective antioxidant mechanisms to survive severe inflammation, as marginal (subpial) astrocytes that are part of the limiting glia from the brain are especially prominent in patients which have survived episodes of purulent or granulomatous meningitis, indicating that these cells are essential to avoid dissemination of pathogenic agents into the brain parenchyma [28].
In situ expression of SVCT2 in other subpopulations of parenchymal astrocytes has only been reported at the mRNA level after ischemia/reperfusion injury generated by occlusion of the middle cerebral artery [20]. Moreover, it has been determined that cultures of astrocytes maintained for 22 DIV, but not 7 DIV, express SVCT2 mRNA and exhibit the ability to uptake AA by a sodium-dependent mechanism that was sensitive to quercetin [33]. Overall, this suggests that SVCT2 expression is inducible in activated reactive astrocytes and modulated by signs of injury and inflammation.
Physiologically, astrocytes regulate blood flow, delivery of energy substrates, synapsis, and plasticity [28]. Astrogliosis or astrocytic activation refers to a set of molecular, cellular, and functional changes that astrocytes suffer during different pathologies of the nervous system, such as brain and spinal cord infections, traumatic injury, epilepsy, infarct, some brain tumors, and neurodegenerative diseases (e.g., AD, amyotrophic lateral sclerosis, Parkinson’s disease (PD), and Huntington’s disease (HD) [35]. It has been proposed that astrocytic activation is not an all-or-nothing process, but at least three degrees of reactive astrogliosis can be defined (mild to severe, severe and diffuse, or severe with formation of a compact glial scar) that are generated as a consequence of the severity of the insult [28]. Moreover, it has been reported that certain viral and bacterial infections as well as ependymal denudation (EpD) after intracerebroventricular injection of neuraminidase, induce a strong overexpression of GFAP and other genes, a pronounced hypertrophy of the body and cellular processes, and the formation of a dense glial scar to isolate and protect the neuronal parenchyma against inflammatory cells and infectious agents [36]. Therefore, it is considered that these insults trigger the most severe form of reactive astrogliosis. Our analysis with GFP-adenovirus showed a high intensity of GFAP immunostaining in areas, such as the marginal layer from cerebral cortex and hippocampus, which are near the zone of effective viral transduction (i.e., pial surface and corpus callosum, respectively), revealing the presence of a glial scar. Similarly, in the brains injected with neuraminidase, an intense co-localization between GFAP and vimentin was detected in the areas of external cortex. Similar results were obtained in the corpus callosum at 5 and 10 days following cortical injury. The appearance of reactive astrogliosis and a glial scar observed after CNS trauma varies depending on different factors, from severe reactive astrogliosis and prominent glial scar throughout the area where the injury occurred into the surrounding areas that decreases in severity in areas distant to the injury site. In this context, we not only detected an induction of SVCT2 expression in reactive astrocytes present in the injury area at 5 days post-injury, but also observed a space-time diffusion of the reactive astrogliosis toward the opposite hemisphere at 10 days following cortical injury. This phenomenon was accompanied with an induction of SVCT2 expression by astrocytes. Using hippocampal and cerebral cortex samples from the kindling model, a model of mesial temporal lobe epilepsy [37] and a form of chronic and permanent epileptic state [38], we detected numerous hypertrophic reactive astrocytes positive for GFAP with decreased vimentin levels. However, an intense co-localization of GFAP and SVCT2 was observed in these reactive astrocytes present not only in the hyppocampus but also in the cerebral cortex, indicating that the severe and prominent astrogliosis present in these samples is associated with SVCT2 induction in reactive astrocytes. The areas containing the glial scar showed different levels of expression and localization of SVCT2, indicating that expression of the transporter is induced in reactive astrocytes as a physiological response to severe reactive astrogliosis.
Antioxidant protection exerted by reactive astrocytes may be important to prevent neurodegeneration observed in diseases, such as AD, HD, ALS, and PD. In our study, no association was detected between the SVCT2 expression and the characteristic astrogliosis, a focal process that has been previously described as surrounding the amyloid plaques [35], in brain material from AD patients. The samples used in this study may have presented with mild reactive astrogliosis where astrocytes do not express SVCT2, similar to that observed in normal brains. Studies in mouse models of AD have shown that reactive astrocytes migrate towards Aβ peptides, internalizing and reducing their deposits [39,40,41]. Moreover, co-cultures of neurons and astrocytes have confirmed that astrocytes are able to internalize Aβ peptides, which induces oxidative stress, depletion of glutathione content, and neuronal death by an astrocyte-dependent mechanism [42]. In this regard, selective overexpression of nuclear factor erythroid 2-related factor 2 (Nfr2) in astrocytes, a factor that regulates the expression of antioxidant enzymes related to glutathione metabolism (heme-oxygenases and NAD(P)H quinone oxidoreductases), preserves neuronal viability in the brain from mice with ALS, PD, and HD [43,44,45]. Therefore, we propose that SVCT2 induction constitutes an interesting therapeutic strategy to allow AA uptake by activated astrocytes in order to enhance their antioxidant capacity to reduce the deleterious effects of intracellular ROS production and, thus, the negative consequences for neuronal viability.
The mechanism by which SVCT2 is upregulated in brain tissue is poorly understood. It has been observed that SVCT2 mRNA levels increase in neurons and astrocytes following oxidative damage due to ischemia and reperfusion [20]; however, other studies have shown that the increase in SVCT2 occurs only in neurons [46, 47] or in endothelial cells and neurons [48]. Thus, we propose that there is a differential mechanism in CNS cells, which regulates SVCT2 expression in the different cell types. In C2C12 cells, it has been determined that the activation of NFκB and AP-1 would increase SVCT2 expression under conditions of oxidative stress generated by hydrogen peroxide [49]. Interestingly, activation of the JNK pathway as well as p38 MAPKs and NFκB, has been proposed to favor increased SVCT2 expression in neuronal cultures treated with ethanol [50].
Under pathophysiological conditions or oxidative damage, astrocytes generate different cytokines, including TNFalpha [51], resulting in the activation of NFκB and reactive gliosis. This mechanism could operate in most of the pathologies described in this study; however, in patients with AD (Fig. 7) and in animal models with aging pathologies, there would be no increase in SVCT2 [51].
Together, our data suggest that SVCT2 induction in severe reactive astrogliosis is a necessary event for oxidative defense and cellular protection. This mechanism would not only potentiate astrocyte survival, but also promote the maintenance of neuronal viability, favoring a faster and more effective recovery of damaged brain tissue. Moreover, SVCT2 expression in reactive astrogliosis may be considered a transversal event for many CNS pathologies characterized by severe reactive astrogliosis and the presence of a dense glial scar, constituting a putative marker for activated astrocytes and also a therapeutic target for future clinical treatments to protect the damaged brain.
References
May JM, Qu ZC, Mendiratta S (1998) Protection and recycling of alpha-tocopherol in human erythrocytes by intracellular ascorbic acid. Arch Biochem Biophys 349(2):281–289. https://doi.org/10.1006/abbi.1997.0473
Nualart F, Mack L, Garcia A, Cisternas P, Bongarzone ER, Heitzer M, Jara N, Martinez F et al (2014) Vitamin C transporters, recycling and the bystander effect in the nervous system: SVCT2 versus gluts. J Stem Cell Res Ther 4(5):209. https://doi.org/10.4172/2157-7633.1000209
Rice ME, Lee EJ, Choy Y (1995) High levels of ascorbic acid, not glutathione, in the CNS of anoxia-tolerant reptiles contrasted with levels in anoxia-intolerant species. J Neurochem 64(4):1790–1799
Nualart FJ, Rivas CI, Montecinos VP, Godoy AS, Guaiquil VH, Golde DW, Vera JC (2003) Recycling of vitamin C by a bystander effect. J Biol Chem 278(12):10128–10133. https://doi.org/10.1074/jbc.M210686200
Tsukaguchi H, Tokui T, Mackenzie B, Berger UV, Chen XZ, Wang Y, Brubaker RF, Hediger MA (1999) A family of mammalian Na+-dependent L-ascorbic acid transporters. Nature 399(6731):70–75. https://doi.org/10.1038/19986
García L, Salazar K, Millan C, Rodriguez F, Montecinos H, Caprile T, Silva C, Cortes C et al (2005) Sodium vitamin C cotransporter SVCT2 is expressed in hypothalamic glial cells. Glia 50(1):32–47. https://doi.org/10.1002/glia.20133
Mun GH, Kim MJ, Lee JH, Kim HJ, Chung YH, Chung YB, Kang JS, Hwang YI et al (2006) Immunohistochemical study of the distribution of sodium-dependent vitamin C transporters in adult rat brain. J Neurosci Res 83(5):919–928. https://doi.org/10.1002/jnr.20751
Qiu S, Li L, Weeber EJ, May JM (2007) Ascorbate transport by primary cultured neurons and its role in neuronal function and protection against excitotoxicity. J Neurosci Res 85(5):1046–1056. https://doi.org/10.1002/jnr.21204
Salazar K, Cerda G, Martinez F, Sarmiento JM, Gonzalez C, Rodriguez F, Garcia-Robles M, Tapia JC et al (2014) SVCT2 transporter expression is post-natally induced in cortical neurons and its function is regulated by its short isoform. J Neurochem 130(5):693–706. https://doi.org/10.1111/jnc.12793
Garcia-Krauss A, Ferrada L, Astuya A, Salazar K, Cisternas P, Martinez F, Ramirez E, Nualart F (2016) Dehydroascorbic acid promotes cell death in neurons under oxidative stress: a protective role for astrocytes. Mol Neurobiol 53(9):5847–5863. https://doi.org/10.1007/s12035-015-9497-3
Caprile T, Salazar K, Astuya A, Cisternas P, Silva-Alvarez C, Montecinos H, Millan C, de Los Angeles Garcia M et al (2009) The Na+-dependent L-ascorbic acid transporter SVCT2 expressed in brainstem cells, neurons, and neuroblastoma cells is inhibited by flavonoids. J Neurochem 108(3):563–577. https://doi.org/10.1111/j.1471-4159.2008.05788.x
Silva-Alvarez C, Salazar K, Cisternas P, Martinez F, Liour S, Jara N, Bertinat R, Nualart F (2016) Apical polarization of SVCT2 in apical radial glial cells and progenitors during brain development. Mol Neurobiol. https://doi.org/10.1007/s12035-016-0081-2
Oyarce K, Silva-Alvarez C, Ferrada L, Martinez F, Salazar K, Nualart F (2017) SVCT2 is expressed by cerebellar precursor cells, which differentiate into neurons in response to ascorbic acid. Mol Neurobiol. https://doi.org/10.1007/s12035-016-0366-5
Meredith ME, Harrison FE, May JM (2011) Differential regulation of the ascorbic acid transporter SVCT2 during development and in response to ascorbic acid depletion. Biochem Biophys Res Commun 414(4):737–742. https://doi.org/10.1016/j.bbrc.2011.09.146
Portugal CC, Socodato R, Canedo T, Silva CM, Martins T, Coreixas VS, Loiola EC, Gess B et al (2017) Caveolin-1-mediated internalization of the vitamin C transporter SVCT2 in microglia triggers an inflammatory phenotype. Sci Signal 10(472). https://doi.org/10.1126/scisignal.aal2005
Angelow S, Haselbach M, Galla HJ (2003) Functional characterisation of the active ascorbic acid transport into cerebrospinal fluid using primary cultured choroid plexus cells. Brain Res 988(1–2):105–113
Ulloa V, Garcia-Robles M, Martinez F, Salazar K, Reinicke K, Perez F, Godoy DF, Godoy AS et al (2013) Human choroid plexus papilloma cells efficiently transport glucose and vitamin C. J Neurochem. https://doi.org/10.1111/jnc.12295
Gess B, Lohmann C, Halfter H, Young P (2010) Sodium-dependent vitamin C transporter 2 (SVCT2) is necessary for the uptake of L-ascorbic acid into Schwann cells. Glia 58(3):287–299. https://doi.org/10.1002/glia.20923
Nualart F, Salazar K, Oyarce K, Cisternas P, Jara N, Silva-Alvarez C, Pastor P, Martinez F et al (2012) Typical and atypical stem cells in the brain, vitamin C effect and neuropathology. Biol Res 45(3):243–256. https://doi.org/10.4067/S0716-97602012000300006
Berger UV, Lu XC, Liu W, Tang Z, Slusher BS, Hediger MA (2003) Effect of middle cerebral artery occlusion on mRNA expression for the sodium-coupled vitamin C transporter SVCT2 in rat brain. J Neurochem 86(4):896–906
Cisternas P, Silva-Alvarez C, Martinez F, Fernandez E, Ferrada L, Oyarce K, Salazar K, Bolanos JP et al (2014) The oxidized form of vitamin C, dehydroascorbic acid, regulates neuronal energy metabolism. J Neurochem 129(4):663–671. https://doi.org/10.1111/jnc.12663
Alvarez-Ferradas C, Morales JC, Wellmann M, Nualart F, Roncagliolo M, Fuenzalida M, Bonansco C (2015) Enhanced astroglial Ca2+ signaling increases excitatory synaptic strength in the epileptic brain. Glia 63(9):1507–1521. https://doi.org/10.1002/glia.22817
Steward O, Torre ER, Tomasulo R, Lothman E (1991) Neuronal activity up-regulates astroglial gene expression. Proc Natl Acad Sci U S A 88(15):6819–6823
Shi LH, Luo F, Woodward DJ, McIntyre DC, Chang JY (2007) Temporal sequence of ictal discharges propagation in the corticolimbic basal ganglia system during amygdala kindled seizures in freely moving rats. Epilepsy Res 73(1):85–97. https://doi.org/10.1016/j.eplepsyres.2006.08.008
Morales JC, Alvarez-Ferradas C, Roncagliolo M, Fuenzalida M, Wellmann M, Nualart FJ, Bonansco C (2014) A new rapid kindling variant for induction of cortical epileptogenesis in freely moving rats. Front Cell Neurosci 8:200. https://doi.org/10.3389/fncel.2014.00200
Barres BA (2008) The mystery and magic of glia: a perspective on their roles in health and disease. Neuron 60(3):430–440. https://doi.org/10.1016/j.neuron.2008.10.013
Belanger M, Magistretti PJ (2009) The role of astroglia in neuroprotection. Dialogues Clin Neurosci 11(3):281–295
Sofroniew MV, Vinters HV (2010) Astrocytes: biology and pathology. Acta Neuropathol 119(1):7–35. https://doi.org/10.1007/s00401-009-0619-8
De Keyser J, Mostert JP, Koch MW (2008) Dysfunctional astrocytes as key players in the pathogenesis of central nervous system disorders. J Neurol Sci 267(1–2):3–16. https://doi.org/10.1016/j.jns.2007.08.044
Savini I, Rossi A, Pierro C, Avigliano L, Catani MV (2008) SVCT1 and SVCT2: key proteins for vitamin C uptake. Amino Acids 34(3):347–355. https://doi.org/10.1007/s00726-007-0555-7
Burzle M, Hediger MA (2012) Functional and physiological role of vitamin C transporters. Curr Top Membr 70:357–375. https://doi.org/10.1016/B978-0-12-394316-3.00011-9
Rice ME (2000) Ascorbate regulation and its neuroprotective role in the brain. Trends Neurosci 23(5):209–216
Astuya A, Caprile T, Castro M, Salazar K, Garcia Mde L, Reinicke K, Rodriguez F, Vera JC et al (2005) Vitamin C uptake and recycling among normal and tumor cells from the central nervous system. J Neurosci Res 79(1–2):146–156. https://doi.org/10.1002/jnr.20326
Pastor P, Cisternas P, Salazar K, Silva-Alvarez C, Oyarce K, Jara N, Espinoza F, Martinez AD et al (2013) SVCT2 vitamin C transporter expression in progenitor cells of the postnatal neurogenic niche. Front Cell Neurosci 7:119. https://doi.org/10.3389/fncel.2013.00119
Allaman I, Belanger M, Magistretti PJ (2011) Astrocyte-neuron metabolic relationships: for better and for worse. Trends Neurosci 34(2):76–87. https://doi.org/10.1016/j.tins.2010.12.001
Granados-Duran P, Lopez-Avalos MD, Grondona JM, Gomez-Roldan Mdel C, Cifuentes M, Perez-Martin M, Alvarez M, Rodriguez de Fonseca F et al (2015) Neuroinflammation induced by intracerebroventricular injection of microbial neuraminidase. Front Med 2:14. https://doi.org/10.3389/fmed.2015.00014
Cole-Edwards KK, Musto AE, Bazan NG (2006) c-Jun N-terminal kinase activation responses induced by hippocampal kindling are mediated by reactive astrocytes. J Neurosci : Off J Soc Neurosci 26(32):8295–8304. https://doi.org/10.1523/JNEUROSCI.1986-05.2006
Kandratavicius L, Balista PA, Lopes-Aguiar C, Ruggiero RN, Umeoka EH, Garcia-Cairasco N, Bueno-Junior LS, Leite JP (2014) Animal models of epilepsy: use and limitations. Neuropsychiatr Dis Treat 10:1693–1705. https://doi.org/10.2147/NDT.S50371
Wyss-Coray T, Loike JD, Brionne TC, Lu E, Anankov R, Yan F, Silverstein SC, Husemann J (2003) Adult mouse astrocytes degrade amyloid-beta in vitro and in situ. Nat Med 9(4):453–457. https://doi.org/10.1038/nm838
Nagele RG, D'Andrea MR, Lee H, Venkataraman V, Wang HY (2003) Astrocytes accumulate A beta 42 and give rise to astrocytic amyloid plaques in Alzheimer disease brains. Brain Res 971(2):197–209
Pihlaja R, Koistinaho J, Malm T, Sikkila H, Vainio S, Koistinaho M (2008) Transplanted astrocytes internalize deposited beta-amyloid peptides in a transgenic mouse model of Alzheimer’s disease. Glia 56(2):154–163. https://doi.org/10.1002/glia.20599
Abramov AY, Canevari L, Duchen MR (2004) Calcium signals induced by amyloid beta peptide and their consequences in neurons and astrocytes in culture. Biochim Biophys Acta 1742(1–3):81–87. https://doi.org/10.1016/j.bbamcr.2004.09.006
Vargas MR, Johnson DA, Sirkis DW, Messing A, Johnson JA (2008) Nrf2 activation in astrocytes protects against neurodegeneration in mouse models of familial amyotrophic lateral sclerosis. J Neurosci : Off J Soc Neurosci 28(50):13574–13581. https://doi.org/10.1523/JNEUROSCI.4099-08.2008
de Vries HE, Witte M, Hondius D, Rozemuller AJ, Drukarch B, Hoozemans J, van Horssen J (2008) Nrf2-induced antioxidant protection: a promising target to counteract ROS-mediated damage in neurodegenerative disease? Free Radic Biol Med 45(10):1375–1383. https://doi.org/10.1016/j.freeradbiomed.2008.09.001
Joshi G, Johnson JA (2012) The Nrf2-ARE pathway: a valuable therapeutic target for the treatment of neurodegenerative diseases. Recent Pat CNS Drug Discov 7(3):218–229
Iwata N, Okazaki M, Xuan M, Kamiuchi S, Matsuzaki H, Hibino Y (2014) Orally administrated ascorbic acid suppresses neuronal damage and modifies expression of SVCT2 and GLUT1 in the brain of diabetic rats with cerebral ischemia-reperfusion. Nutrients 6(4):1554–1577. https://doi.org/10.3390/nu6041554
Portugal CC, da Encarnacao TG, Socodato R, Moreira SR, Brudzewsky D, Ambrosio AF, Paes-de-Carvalho R (2012) Nitric oxide modulates sodium vitamin C transporter 2 (SVCT-2) protein expression via protein kinase G (PKG) and nuclear factor-kappaB (NF-kappaB). J Biol Chem 287(6):3860–3872. https://doi.org/10.1074/jbc.M111.260166
Gess B, Sevimli S, Strecker JK, Young P, Schabitz WR (2011) Sodium-dependent vitamin C transporter 2 (SVCT2) expression and activity in brain capillary endothelial cells after transient ischemia in mice. PLoS One 6(2):e17139. https://doi.org/10.1371/journal.pone.0017139
Savini I, Rossi A, Catani MV, Ceci R, Avigliano L (2007) Redox regulation of vitamin C transporter SVCT2 in C2C12 myotubes. Biochem Biophys Res Commun 361(2):385–390. https://doi.org/10.1016/j.bbrc.2007.07.007
Tian H, Ye X, Hou X, Yang X, Yang J, Wu C (2016) SVCT2, a potential therapeutic target, protects against oxidative stress during ethanol-induced neurotoxicity via JNK/p38 MAPKs, NF-kappaB and miRNA125a-5p. Free Radic Biol Med 96:362–373. https://doi.org/10.1016/j.freeradbiomed.2016.03.039
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, Bennett ML, Munch AE et al (2017) Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541(7638):481–487. https://doi.org/10.1038/nature21029
Acknowledgements
This work was partially supported by a FONDECYT grant 1140477 and CONICYT PIA ECM-12 grant (both to Francisco Nualart), the National Institutes of Health grant (R01 NS065808) to Ernesto R. Bongarzone, grants 1130491 from FONDECYT, CONICYT-Chile, and CID 1/2006 from DIPUV to Christian Bonansco, Fondecyt grant 11140405 to Katterine Salazar and Fondecyt grant 11150678 to Fernando Martínez. The funders had no role in the study design, data collection, data analysis, decision to publish, or preparation of the manuscript. We thank Ms. Ximena Koch for technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salazar, K., Martínez, F., Pérez-Martín, M. et al. SVCT2 Expression and Function in Reactive Astrocytes Is a Common Event in Different Brain Pathologies. Mol Neurobiol 55, 5439–5452 (2018). https://doi.org/10.1007/s12035-017-0762-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0762-5