Abstract
Therapeutic hypothermia (TH) is the most potent therapeutic strategy for global cerebral ischemia (GCI), usually induced by cardiac arrest. TH has been shown both to suppress the delayed neuronal cell death in the vulnerable hippocampal CA1 subregion and to improve neurological outcomes in experimental animals after GCI. However, given the multiple adverse effects resulting from TH, application of such a therapy is typically limited. In recent years, methylene blue (MB) has emerged as a potential therapeutic drug for the treatment of neurodegenerative diseases. In this study, we investigated the beneficial effects of mild TH combined with MB treatment after GCI. We report that both the neuronal survival in the hippocampal CA1 region and the hippocampus-dependent spatial learning and memory in the combined treatment animals were enhanced compared to those in the single treatment animals. Mechanistic studies revealed that combined TH and MB treatment significantly attenuated mitochondrial dysfunction induced by GCI in the hippocampus CA1 region. The combined treatment also markedly suppressed GCI-induced reactive gliosis and inflammation and reduced oxidative stress while enhancing the antioxidant capacity of hippocampal CA1 neurons. Finally, combining TH and MB synergistically attenuated the intrinsic cytochrome c/caspase-3 apoptotic pathway induced by GCI. Our results suggest that TH and MB act synergistically to protect the ischemic brain and suppress cognitive impairment caused by GCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Representing about 2% of the total body weight, the human brain consumes about 20% of the oxygen and 25 to 50% of the body’s glucose [1, 2]. Brain neurons have the highest energy needs, requiring continuous delivery of oxygen and glucose from cerebral blood flow [3]. However, blood supply of oxygen and glucose to the brain tissue is drastically reduced during global cerebral ischemia (GCI), usually resulting from cardiac arrest, severe hypotensive shock, asphyxia, and complex cardiac surgery [4–8]. In these situations, a transient period of GCI causes selective cell death in the vulnerable hippocampal CA1 pyramidal cell layer days after reperfusion, which is known as delayed apoptotic neuronal death [7, 9, 10]. Following neuronal cell loss, one of the major disabilities in survivors of GCI is cognitive impairment.
To date, no pharmacological treatments are effective to promote recovery in patients with a GCI. Therapeutic hypothermia (TH) is the only strategy that has been reported to benefit adult cardiac arrest patients, with the patients usually being cooled to the range of 32–34 °C for 12–24 h [11, 12]. However, the practical induction of hypothermia, including phases of induction, duration of therapy, and rewarming, is labor-intensive and time-consuming. Importantly, recent meta-analysis suggests that the benefit of TH on survival and neurological outcome after cardiac arrest is still inconclusive and controversial [11, 13]. Additional limitations of TH include significant side effects such as pneumonia, renal tubular dysfunction, arrhythmia, seizures, and imbalance of electrolytes and blood sugar [14–16]. Therefore, it is important to develop new treatment therapies for protection of the brain after GCI.
Methylene blue (MB), a century-old drug for the treatment of malaria, has recently been shown to be neuroprotective against various neurodegenerative disorders [17–19]. Recent works by our laboratory and others have demonstrated the beneficial effects of MB in ischemic brain injuries, including the neuroprotective and functional improvement effects in experimental stroke and GCI models [20–23]. Accumulating evidence from clinical and animal studies also suggests that combination therapies are more effective than a single approach. As such, the combined treatment with effective drugs and therapies may become a paradigm in preventing ischemic brain injury such as GCI. Intriguingly, MB in combination with other therapies has been reported to exert greater synergistic efficacy [24–29]. Therefore, the MB-containing regimens could also represent a promising alternative therapy combination against GCI-induced neurological deficits.
By utilizing a well-established rat model of GCI, the present study was designed to elucidate whether MB, combined with an improved TH treatment, could synergistically protect the hippocampal neurons from ischemic reperfusion-induced injury and alleviate cognitive impairment. This work was also performed to further refine the potential underlying mechanisms of combination treatment.
Materials and Methods
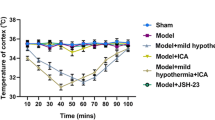
Global Cerebral Ischemia
Sprague Dawley male rats (aged 3 months and weighing 250–300 g) were used for the current study. The animals were randomly divided into six groups: sham control (sham, without ischemia), GCI (rats underwent global cerebral ischemia, no methylene blue, no hypothermia), GCI + Veh (GCI plus vehicle saline treatment), GCI + MB (GCI plus methylene blue treatment), GCI + TH (GCI plus hypothermia treatment), and GCI + MB + TH. The experimental design is shown in Fig. 1a. The GCI model was developed using the four-vessel occlusion (4-VO) method [30] with some modifications. Briefly, under anesthesia with sodium pentobarbital (50 mg/kg, i.p.), the right and left alar foramina of the first cervical vertebrae were exposed through a midline incision behind the occipital bone. The vertebral arteries were permanently occluded by bipolar electrocauterization. Thereafter, the bilateral common carotid arteries (CCAs) were isolated and a silastic ligature was loosely secured around each artery, and the incision was closed with wound clips. Twenty-four hours later, the animals were re-anesthetized with isofluorane and the CCAs were exposed and occluded for 25 min with aneurysm clips to induce GCI. A relatively long duration of ischemia was induced in this study to evaluate the difference between single treatment and the combined treatment. Isofluorane was discontinued after initiation of the ischemia. Successful GCI was ensured by monitoring the bilateral pupil dilation, unresponsiveness to light, and loss of righting reflex of each subject after CCA occlusion. After the procedure, the clips were released and arterial blood flow was confirmed before the skin was sutured. Rectal temperature of the subject was kept at 37 ± 0.5 °C during and after ischemia via an infrared lamp and a thermal blanket, except after surgery in TH groups. Sham-operated animals underwent identical surgical procedures as with ischemic animals except for the occlusion of CCAs. All animal procedures were approved by the institutional animal use committee and conformed to the local and international guidelines on the ethical use of animals. All efforts were made to minimize the pain or distress and reduce the number of animals used in the experiments.
Effect of methylene blue and hypothermia on neuronal survival in the CA1 region of the hippocampus after GCI. a Schematic experimental design of methylene blue (MB) and hypothermia (HT) treatment, at 2 h after GCI. b Representative images of immunofluorescent labeling for NeuN in the ischemic hippocampus 12 days after GCI. Scale bar = 200 μm. c Quantitative analyses of neuronal survival in hippocampal CA1 pyramidal layer. The number of surviving neurons was quantified as percentage changes versus sham control group. * P < 0.05 versus sham control, # P < 0.05 versus ischemic control (GCI) or vehicle control (Veh) group, and $ P < 0.05 versus MB or HT treatment group. Data shown are means ± SE from 8 to 12 animals in each group
Methylene Blue and Hypothermia Treatment
Two hours after GCI, mild hypothermia was induced and rectal temperature was maintained at 35 ± 0.5 °C for 2 h. Temperature was consistently controlled by using an automated temperature control system including a Humidifier Cooling Electric Fan, ice packs, and a rectal probe as described previously [31]. After the experiment, the animals were gradually warmed up to normothermia over a period of 1 h with an overhead infrared lamp and a heating pad. For methylene blue (MB) treatment, 2 h after GCI, MB (Fisher Scientific, Pittsburgh, PA) or vehicle (0.9% saline) was administered with 3-day release ALZET Osmotic pumps (1003D, DURECT Corporation, Cupertino, CA) at doses of 0.5 mg/kg/day as described in our previous work [21]. The minipumps were implanted subcutaneously under the upper back skin of the animals.
Histological Analysis
Immunofluorescent labeling for NeuN and TUNEL was performed to evaluate neuronal viability in the ischemic hippocampus, using a procedure previously described [32]. Briefly, animals 12 days after GCI were transcardially perfused with ice-cold phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (PFA) in PBS, under deep anesthesia. Brains were collected, soaked in PFA overnight, and cryoprotected in 30% sucrose solution at 4 °C until they sank to the bottom. Rat brain specimens were frozen in OTC compound, and coronal brain slices (25 μm thick) were prepared using a Leica microtome. Free-floating sections were incubated with a mouse anti-NeuN monoclonal antibody (1:500; EMD Millipore) to detect surviving neurons. The morphologically healthy CA1 pyramidal cells displaying round soma and distinct nuclei as appeared in sham-operated animals were counted as surviving neurons. TUNEL labeling was performed on free-floating brain sections using a Click-iT® Plus TUNEL assay kit (Thermo Fisher Scientific) following the manufacturer’s protocol. All the images were obtained using a Zeiss LSM 510 Meta confocal laser scanning microscope (Carl Zeiss Inc., Germany). For quantitative analyses of neuronal survival and apoptotic cell death, the number of healthy CA1 neurons and TUNEL-positive cells per 250 μm length of medial CA1 pyramidal cell layer was counted bilaterally in three to five representative brain sections from each animal. Cell counts from the right and left hippocampus on each of the examined sections were averaged to provide a single value for each brain. A mean ± SE (n = 8–12) was calculated from the data in each group and quantified as percentage changes versus sham control.
Barnes Maze Task
The Barnes Maze task was adapted to examine hippocampus-dependent spatial learning and memory in rats as described previously by our laboratory [33]. Briefly, trial tests were performed on days 9, 10, and 11 after GCI. During a 180-s test, latency of each animal to locate the hidden escape box (escape latency) was recorded. On day 12 after GCI, the escape box was removed, and the time spent in the target quadrant (quadrant occupancy) was recorded in a 90-s period. The platform was extensively cleaned with 70% ethanol between each test. The behavioral traces in the Barnes Maze task were monitored using an overhead camera controlled by computer and analyzed afterwards using ANY-maze video tracking software (Stoelting Co., Wood Dale, IL).
Immunofluorescence Staining and Confocal Microscopy
As described previously [32], free-floating sections were blocked with 10% normal donkey serum for 1 h followed by overnight primary antibody incubation at 4 °C. The following primary antibodies were used for this study: anti-Iba1, superoxide dismutase 2 (SOD2), and thioredoxin-2 (TRX2, Proteintech Group [10]), anti-4-HNE (Abcam Inc.), and anti-GFAP (Cell Signaling). Sections were then washed and incubated with appropriate Alexa Fluor donkey anti-mouse/rabbit secondary antibodies for 1 h at room temperature. The sections were washed, mounted, and coverslipped in Vectashield mounting medium with DAPI (H-1200, Vector Laboratories, Inc.). The changes of mitochondrial membrane potential (MMP) was measured using MitoTracker Red Staining as described [33]. Briefly, MitoTracker® Red CMXRos (50 ng/ml in 100 μl of saline, Life Technologies) was administered via tail vein injection 5 min before scarification. The brains were perfused and fixed, and coronal brain slices (25 μm thick) were prepared as described above. After washing with 0.1% PBS-Triton X-100 and briefly with distilled water, the sections were mounted and sealed in Vectashield mounting medium with DAPI. The images were then obtained on a Zeiss LSM 510 Meta confocal laser scanning microscope (Carl Zeiss Inc., Germany) using either ×40 oil immersion Neofluar objective with the image size set at 1024 × 1024 pixels. The captured images were viewed and analyzed using LSM 510 Meta imaging software, and representative fluorescent images were selected for presentation.
Brain Homogenates and Subcellular Fractionation
Animals were sacrificed by rapid decapitation under deep anesthesia with sodium pentobarbital 3 days after GCI. Brain was immediately removed from the cranium and placed on an ice pad, and the hippocampal CA1 regions were quickly separated and frozen in dry ice. The cytosolic protein fractions were prepared as previously described [32]. Briefly, tissues were homogenized in ice-cold homogenization buffer containing 10 mM HEPES (pH 7.9), 0.6% NP-40, 12 mM β-glycerophosphate, and inhibitors of proteases and enzymes (Thermo Scientific, Rockford, IL) with a Teflon-glass homogenizer. The homogenates were centrifuged at 17,000×g for 20 min at 4 °C to yield cytosolic fractions in the supernatants. Protein concentrations were determined by the Modified Lowry Protein Assay Reagent Kit (Pierce, Rockford, IL), and supernatants were aliquoted and stored at −80 °C until use.
ELISA Assay
The cytoplasmic contents of proinflammatory cytokines and cytochrome c were determined by ELISA technique as described previously [33]. In brief, hippocampus protein samples were diluted with bicarbonate/carbonate coating buffer (Sigma-Aldrich), loaded in PVC ELISA microplate (Corning) and incubated overnight. The plate wells were then washed, blocked, and probed with specific antibodies to IL-1β, IL-6, and cytochrome c for 4 h at 37 °C, respectively. Afterwards, the plate wells were washed and incubated with HRP-conjugated secondary antibodies for 1 h at room temperature. Finally, the plates were developed with TMB substrate and absorbance was read at 370 nm on a spectrophotometer (Bio-Rad). The values were calculated and normalized to the corresponding protein content and expressed as percentage changes compared to the control group.
Protein Carbonyl Content Assay
The levels of oxidative modification of proteins in the hippocampus CA1 region were measured using the OxyBlot Protein Oxidation Detection Kit (EMD Millipore Corporation) following the manufacturer’s protocol. Briefly, protein was denatured in sodium dodecyl sulfate (SDS) and derivatized to 2,4-dinitrophenylhydrazone (DNP) by incubation with 2,4-dinitrophenylhydrazine (DNPH). Electrophoresis was carried out on 4–20% SDS-PAGE, and the separated proteins were transferred onto PVDF membranes. The membranes were then incubated with anti-DNP primary antibody, followed by incubation with HRP-conjugated anti-rabbit secondary antibody. Bound antibodies were visualized by enhanced chemiluminescence (ECL; Amersham Biosciences). The membranes were stripped and reprobed with a monoclonal primary antibody against GAPDH (1:5000, Proteintech Group). The level of protein carbonylation was normalized to the corresponding GAPDH and expressed as percentage changes versus sham control.
Total Antioxidant Capacity Assay
The total antioxidant capacity in the hippocampus region was determined using an antioxidant assay kit (Cayman Chemical) as described recently [33]. The antioxidant capacity of the sample relies on the ability to inhibit the oxidation of 2,2′-azino-di-(3-ethylbenzthiazoline-6-sulfonic acid (ABTS) by metmyoglobin. Briefly, diluted protein samples or trolox standards were mixed with metmyoglobin and hydrogen peroxide working solution to start the reaction, according to the manufacturer’s instructions. The absorbance was measured at 450 nm on a spectrophotometer (Bio-Rad) after a 5-min incubation, and the standard was plotted as a function of trolox. Total antioxidant capacities of the samples were determined by comparison to the standard curve, and the results were reported as percentage changes compared to the sham control.
Caspase Activity Assay
Caspase-3 activity was measured in the hippocampal proteins using a fluorometric substrate Ac-DEVD-AMC (AnaSpec, Fremont, CA) as previously described by our laboratory [21, 33]. In brief, the reaction was initiated by mixing the protein homogenate and caspase-3 substrate in protease assay buffer and incubated at 37 °C for 1 h. The fluorescence AMC was determined on a fluorescence spectrophotometer (Perkin Elmer) with excitation at 360 nm and emission at 460 nm. Data were calculated as changes in fluorescent units per microgram of protein and presented as percentage changes compared to sham control.
Statistical Analysis
All results were expressed as mean ± SE and analyzed by using SigmaStat 3.5 software (SPSS, Inc., Chicago, IL). The data were examined by one-way or two-way analysis of variance (ANOVA) followed by post hoc comparison with Student-Newman-Keuls’ or Dunnett’s post hoc tests. Probability values less than 0.05 were reported as statistically significant.
Results
Effect of MB and TH on Neuronal Survival in Hippocampal CA1 Region after GCI
Twelve days after GCI, histological analysis was performed to evaluate the level of neuronal survival in hippocampal CA1 subfields. As shown in Fig. 1b, c, a 25-min GCI followed by reperfusion led to severe cell loss in CA1 cell layers in GCI control and vehicle (Veh)-treated GCI animals compared with the sham controls. Examination of NeuN-positive cells from either MB- or TH-treated animals revealed that the single-treatment animals that underwent GCI displayed significant neuronal survival in the hippocampal CA1 region as compared to the GCI or Veh group. Intriguingly, quantitative analysis of the number of surviving neurons indicated that the neuroprotection was markedly greater in the MB-TH combined treatment group than in the MB or TH single-treatment group.
Effect of MB and TH on Impaired Spatial Learning and Memory Following GCI
Hippocampus-dependent spatial learning and memory was examined in Barnes Maze task performed on days 9–12 following GCI. As shown in Fig. 2a (upper panel) and Fig. 2b, the trial tests on day 11 revealed that GCI control and Veh-treated animals spent more time (escape latency) to find the hidden escape box, compared to sham control rats. In addition, in the probe tests on day 12 after GCI, ischemic animals spent significantly shorter time (quadrant occupancy) in the target quadrant where the escape box was located, as compared to sham control (lower panel in Fig. 2a, c). By contrast, single MB or TH treatment could significantly decrease escape latencies to find the escape box in the training trials and increase quadrant occupancy in the probe tests. Importantly, MB-TH-combined treatment further increased the performance on hippocampal-dependent learning and memory tests, as evidenced by the shortest escape latency and longest quadrant occupancy in the ischemic animals with combination treatment (Fig. 2a–c).
Effect of methylene blue and hypothermia on hippocampus-dependent spatial learning and memory following GCI. a Representative tracks of the indicated animals in the trial tests (up panel) on day 11 and probe tests (low panel) on day 12 after GCI are shown, respectively. b, c Statistical analyses of the escape latency and quadrant occupancy of the animals in each group. * P < 0.05 versus sham control, # P < 0.05 versus ischemic control (GCI) or vehicle control (Veh) group, and $ P < 0.05 versus MB or HT treatment group. Data shown are means ± SE from 8 to 12 animals in each group
Effect of MB and TH on Mitochondrial Dysfunction Induced by GCI in the Hippocampus CA1 Region
We next examined whether MB and TH have the additive effects to prevent GCI-induced changes in mitochondrial function. We first examined mitochondrial membrane potential (MMP) using MitoTracker Red fluorescent dye and confocal microscopy, as shown in Fig. 3a, b. Quantitative analysis of MitoRed fluorescence intensities showed markedly decreased fluorescence signal associated with MMP in the cytoplasm of CA1 neurons 3 days after GCI (GCI control and Veh vs. Sham), suggesting mitochondrial depolarization and collapse of MMP induced by GCI. Intriguingly, treatment with either MB or TH could partially and significantly increase fluorescence intensity associated with MMP, compared with GCI- and Veh-treated controls. Additionally, MB-TH-combined treatment synergistically preserved the fluorescence intensity, compared with single MB or TH treatment. Secondly, we measured the cytochrome c oxidase (CCO) activity associated with mitochondrial function, using the mitochondrial fraction samples from CA1 regions. As shown in Fig. 3c, a similar protective pattern as in MMP was observed in single MB- or TH-treated animals compared to GCI/Veh controls, and this effect was potentiated by combination treatment, indicating a synergistic effect of MB plus TH in preservation of mitochondrial function and the presence of healthy mitochondria.
Effect of methylene blue and hypothermia on mitochondrial dysfunction in the hippocampus CA1 neurons 3 days after GCI. a Representative confocal microscopy images of fluorescent MitoTracker Red staining for MMP tests. DAPI was used for nuclear counterstain of the CA1 cell layer. Staining images are representative of four to five individual animals in each group. Scale bar = 20 μm. b The MitoTracker fluorescence intensity associated with MMP was quantified and expressed as percentage changes compared with the sham control. c Cytochrome c oxidase (CCO) activity was detected in the mitochondrial fractions from each group, and the value was expressed as percentage changes relative to sham control. * P < 0.05 versus sham, # P < 0.05 versus GCI or Veh control group, and $ P < 0.05 versus MB or HT treatment group. Data are means ± SE from four to five animals in each group
Effect of MB and TH on Reactive Gliosis and Proinflammatory Cytokine Production Induced by GCI in the Hippocampus CA1 Region
Microglial and astrocytic gliosis and inflammation were then evaluated at the later reperfusion time points, 3 and 12 days after GCI. Brain sections were immunostained for detection of Iba1 (a marker for microglial activation) and GFAP (a marker for reactive astrocytosis). Figure 4a presents typical confocal microscopy images showing remarkable activation of microglia and astrocytes in the hippocampal CA1 subfield 12 days after GCI. In addition, the production of proinflammatory cytokines, IL-1β and IL-6, were determined by ELISA assays in CA1 proteins collected 3 days after GCI (Fig. 4b, c). The data clearly showed that single treatment of MB or TH could effectively attenuate ischemia reperfusion-evoked microglial and astroglial activation (Fig. 4a), as well as the elevated levels of IL-1β and IL-6 (Fig. 4b, c). Interestingly, when animals were treated with both MB and TH, ischemia reperfusion-induced reactive gliosis and proinflammatory cytokine levels were almost completely blocked at days 12 and 3 after GCI, respectively.
Effect of methylene blue and hypothermia on microglial and astroglial activation, and proinflammatory cytokines produced by GCI in the hippocampus CA1 region. a Typical confocal microscopy images of Iba1 (green) and GFAP (red) staining taken from the medial CA1 region 12 days after GCI. Brain sections were counterstained with DAPI (blue). Scale bar = 20 μm. Staining images are representative of 8–12 individual animals in each group. b, c The concentrations of proinflammatory cytokines IL-1β and IL-6 were determined by ELISA assays using hippocampal CA1 proteins collected 3 days after GCI. Data are means ± SE (n = 4–5) expressed as percentage changes versus sham controls. * P < 0.05 versus sham, # P < 0.05 versus GCI or Veh control group, and $ P < 0.05 versus MB or HT treatment group
Effect of MB and TH on the Levels of Oxidative Status After GCI in the Hippocampus CA1 Region
We then examined the level of protein carbonyl, a novel biomarker for oxidative stress [34], and the total antioxidant capacity in hippocampus CA1 protein samples collected 3 days after GCI. As shown in Fig. 5a, b, relative to the changes in the GCI/Veh control groups, both the single treatment group (MB or TH) and the combination treatment group (MB + TH) had significant changes reflected in the decreased level of protein carbonyl content and increased level of antioxidant capacity, with moderate and greater effects in single and combined groups, respectively. Furthermore, immunofluorescent labeling for lipid peroxidation (4-HNE) and mitochondrial antioxidants (TRX2 and SOD2) was performed in the hippocampal CA1 region 3 days after GCI. The results in Fig. 5c revealed that, in agreement with the effects of MB/TH in maintaining cellular redox homeostasis status, combination of both treatments resulted in a remarkable decrease in the level of 4-HNE and increase in the levels of TRX2 and SOD2, respectively, compared with GCI/Veh control and single-treatment groups.
Effect of methylene blue and hypothermia on oxidative stress status in the hippocampus CA1 region 3 days after GCI. a The levels of oxidative modification of proteins in the hippocampus CA1 region were measured using a protein carbonyl immunoblot kit. b Total antioxidant capacity in the hippocampus CA1 of each group was examined using an antioxidant assay kit. c Representative microscopy images of immunofluorescent labeling for 4-HNE, TRX2, and SOD2 in the hippocampal CA1 region 3 days after GCI. Scale bar = 20 μm. Results are means ± SE from four to five animals in each group. * P < 0.05 versus sham, # P < 0.05 versus GCI or Veh control group, and $ P < 0.05 versus MB or HT treatment group
Effect of MB and TH on Cytosolic Levels of Cytochrome c, Caspase-3, and Neuronal Apoptosis Induced by GCI in the Hippocampus CA1 Region
Finally, we investigated the changes of the intrinsic mitochondrial apoptotic pathway following GCI and MB-TH treatments. The cytosolic distribution of cytochrome c (Cyt c) was examined by ELISA assay, and caspase-3 activity was determined using specific fluorometric substrates at day 3 after GCI. As shown in Fig. 6a, b, ischemia reperfusion induced significant elevations in cytosolic Cyt c level and caspase-3 activity compared with sham control, and these increases could be attenuated by either MB or TH treatment. Notably, MB-TH-combined treatment exerted additive effect in inhibition of Cyt c release and caspase-3 activation, as compared to single MB or TH treatment. Subsequently, the extent of apoptotic neuronal death in hippocampal CA1 was investigated by TUNEL staining 12 days after GCI. As presented in Fig. 6c, d, cell counting and statistical evaluation demonstrated that single MB or TH treatment could moderately decrease the number of TUNEL-positive cells in the hippocampal CA1 region, compared with GCI/Veh control groups. Furthermore, MB and TH in combination had a synergistic inhibitory effect on the level of neuronal apoptosis following GCI. These observations suggest that MB and TH can work together to inhibit the intrinsic mitochondrial apoptotic pathway and attenuate delayed neuronal death following GCI and reperfusion.
Effect of methylene blue and hypothermia on cytosolic level of cytochrome c, caspase-3 activity, and apoptotic cell death induced by GCI. a The content of cytochrome c (Cyt c) in the cytosolic protein samples of hippocampal CA1 region was examined by ELISA assay at 3 days after GCI. b The change of caspase-3 activity in cytosolic proteins was examined using specific fluorometric substrates at 3 days after GCI. c Representative fluorescent microscopy image of TUNEL staining in the hippocampal CA1 region 12 days after GCI. Scale bar = 20 μm. d The numbers of TUNEL-positive cells in the medial hippocampal CA1 region from the indicated animals were counted and statistically evaluated. Results are means ± SE from four to five animals in a, b, and 8–12 animals in c, d, in each group. * P < 0.05 versus sham, # P < 0.05 versus GCI or Veh control group, and $ P < 0.05 versus MB or HT treatment group
Discussion
Using a well-established 4-VO GCI model, the current study first demonstrated that combination treatment with MB and TH, initiated 2 h after GCI insult, exhibited synergistic neuroprotective properties against the delayed neuronal cell death in the hippocampal CA1 region. Previous studies suggest that TH must be applied immediately or within hours after GCI and must be sustained for at least 1 h in order to obtain neuroprotective effects [35, 36]. The treatment window and profile of TH also rely on the ischemic duration or severity. It should be noted that, to examine the potential combined effects of certain therapies compared with the single treatment, a relatively prolonged duration of ischemia (25 min vs. the standard 10–15 min) was adopted in this study to induce more severe neuronal damage. The key findings are that the extent of hippocampus neuronal survival, improved strikingly by combination treatment, was correlated with the improvement of neurological function following GCI. The underlying mechanism of MB-TH-combined treatment on reducing apoptotic neuronal loss and cognitive deficits is likely due to the multifactorial beneficial effects as illustrated in our study: (1) preservation of mitochondrial membrane integrity and restoration of mitochondrial function, (2) suppression of oxidative stress and preservation of antioxidant capacity, (3) reductions in reactive gliosis and neuroinflammation, and (4) attenuation of intrinsic mitochondrial apoptotic pathway in the hippocampal CA1 region. These observations suggest an efficient additive action of TH and MB in the treatment of delayed brain injury following global ischemia.
In this GCI model, hippocampal CA1 cell death usually occurs 3–4 days after ischemic insult, which provides an extended and valuable therapeutic time window for the application of therapies. Although a relatively short duration (2 h) and a higher temperature (35 vs. 32–34 °C) of TH was combined with MB in the current work, the beneficial effects of combination treatment were still present. Our findings thus suggest that the improved TH therapy combined with MB not only exerted enhanced benefits through synergic action but could also potentially decrease the many side effects caused by the longer period of TH, as mentioned above.
Mitochondrial dysfunction in the hippocampal CA1 region plays a pivotal role in the pathogenesis of neuronal death following GCI [10, 21, 37]. Our previous work shows that MB has neuroprotective and functional improvement effects against GCI, at least via improving mitochondrial function [21]. The current study has now extended our past knowledge to include the synergistic influence with mild TH on mitochondrial MMP and activity and showed that TH-MB combination therapy could favorably influence mitochondrial function. Since mitochondria are important regulators of the delayed cell death in response to GCI [38–40], the strategies to improve mitochondrial integrity and function, as shown by the combination treatment herein, are of vital importance in protecting the vulnerable hippocampal CA1 neurons.
We found that the hypothermic animals with MB treatment exhibited a significantly increased activity of cytochrome c oxidase, the terminal complex of the electron transport chain where over 90% of oxygen is consumed [41], compared to the singly MB- or TH-treated animals. This data thus suggests that the combination treatment has an ameliorative affect on brain energy metabolism especially during the late ischemic reperfusion stage. This observed beneficial impact is important, as the reductions of energy metabolism and the oxidative metabolism of glucose, at later reperfusion stages, are observed in ischemia-susceptible neurons and persist for several days after GCI [42]. The progressive failure of energy production in the CA1 subfield is suggested to be coincident with the eventual cell death in hippocampal CA1 pyramidal neuron populations [10]. However, an important mechanism underlying the therapeutic benefits of TH is the reduction of cerebral glucose and oxygen metabolism during the initial phase of reperfusion [12, 43], alluding to the importance of stemming the overproduction of dangerous oxidative free radicals occurring primarily in the early hours after reperfusion [32]. Recently, important findings from Dr. Yang’s group [22, 44] showed that MB can act as an alternative electron donor, shuttling electrons from early energy substrates to Cyt C and increasing energy production while simultaneously bypassing potential electron leakage in the presence of damaged electron transport chain (ETC) components upstream of CCO. This complementary action of MB to increase energy production, thereby maintaining healthy neuronal function, is of vital importance in supporting the therapeutic action of TH. By preventing excessive free radical production while supporting ATP production, we believe that combination therapy can confer additional protection to the mitochondria, greatly improving long-term neuronal survival, as indeed indicated in this study.
Brain neurons are more susceptible to oxidative stress as compared to other body tissues [45, 46]. Enhanced free radicals and oxidative neuronal damage are well accepted for their great contribution to the cell loss and poor neurologic outcome following GCI. Accumulating research findings support that dysfunctional mitochondria and reactive glial cells act as reservoir of reactive oxygen species (ROS) generation [45]. Iron overload caused by ischemia induces mitochondrial depolarization and respiratory chain breakdown thereby generating subsequent deleterious oxidative stress. In addition, reactive microglia and astrocytes enhance inflammation and oxidative damage after ischemia via increased production and release of cytokines and ROS [47, 48]. Oxidative stress can also attack mitochondria and glial cells in a positive feedback manner [49, 50]. Importantly, TH has been shown to attenuate oxidative damage in a variety of experimental models of brain injuries, such as traumatic brain injury [51, 52], neonatal hypoxic-ischemic encephalopathy [53–55], and stroke [56–59], as well as cardiac arrest and global ischemia [60–63]. Oxidative stress is induced by disturbed equilibrium between oxidative status and antioxidant homeostasis. In the current work, we provided novel evidence in the changes of decreased oxidative stress and increased endogenous antioxidant potential by MB and TH, suggesting that redox homeostasis status was substantially restored following combination treatment.
Mitochondrial dysfunctions, activation of caspase-3, and finally apoptosis have been recognized as pathological causes for delayed neuronal death of hippocampal CA1 neurons after GCI insult [9, 10]. This type of cell death of CA1 pyramidal neurons, usually occurring several days after an initial ischemic attack in rodents and humans, is well accepted as neuronal apoptosis [7, 9, 10]. Previous studies from ours and others have indicated that both TH and MB are able to induce neuroprotection associated with reduced mitochondrial dysfunction and the inhibition of caspase-3 activity following cardiac arrest or GCI [21, 64]. The present results extend these previous findings by detailing the combinatorial benefits in inhibiting the intrinsic mitochondrial apoptotic pathway following the combined therapy with TH and MB over the two treatment components in isolation.
While MB has significant therapeutic potential, it must be noted that there are several considerations to be made when designing treatment paradigms. Higher doses of MB have significant adverse effects including cardiovascular effects, headaches, vomiting, diarrhea, and blue urine [65, 66]. MB functions as a photosensitizer, inducing formation of ROS upon exposure to light that can result in damage to the epidermis [67]. MB can also induce serotonin syndrome in the presence of a selective serotonin reuptake inhibitor (SSRI) [68]. In addition, those with glucose-6-phosphate dehydrogenase (G6PD) deficiency are at risk for anemia when administered MB [69]. These considerations must be taken into account when translating MB to GCI in clinical trials.
In conclusion, the novel finding of the synergistic effect of MB plus TH against delayed apoptotic cell death evoked by the GCI indicates that the combination treatment can function in concert to exert beneficial effects. As summarized in Fig. 7, the neuroprotective effects of this treatment appears to involve mediation by preservation of mitochondrial integrity and function, antioxidant preservation against oxidative stress, inhibition of reactive gliosis and inflammation, and attenuation of Cyt c release and mitochondrial apoptotic pathway. Therefore, combination treatment with MB and TH may serve as a potential therapy to treat GCI-induced neuronal death and cognitive deficits.
Schematic summary of the combination treatment of therapeutic hypothermia (TH) and methylene blue (MB). Mitochondrial damage, reactive gliosis, and oxidative stress contribute to the delayed cell death (apoptosis) in hippocampal CA1 neurons following global cerebral ischemia (GCI). Oxidative stress can act as positive feedback, attacking mitochondria and glial cells. MB and HT work synergistically to attenuate these detrimental effects and improve neurological outcome
References
Belanger M, Allaman I, Magistretti PJ (2011) Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation. Cell Metab 14(6):724–738. doi:10.1016/j.cmet.2011.08.016
Kennedy C, Sokoloff L (1957) An adaptation of the nitrous oxide method to the study of the cerebral circulation in children; normal values for cerebral blood flow and cerebral metabolic rate in childhood. J Clin Invest 36(7):1130–1137. doi:10.1172/JCI103509
Mergenthaler P, Lindauer U, Dienel GA, Meisel A (2013) Sugar for the brain: the role of glucose in physiological and pathological brain function. Trends Neurosci 36(10):587–597. doi:10.1016/j.tins.2013.07.001
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K (2002) Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 346(8):557–563. doi:10.1056/NEJMoa003289
Wolman RL, Nussmeier NA, Aggarwal A, Kanchuger MS, Roach GW, Newman MF, Mangano CM, Marschall KE et al (1999) Cerebral injury after cardiac surgery: identification of a group at extraordinary risk. Multicenter Study of Perioperative Ischemia Research Group (McSPI) and the Ischemia Research Education Foundation (IREF) Investigators. Stroke; a journal of cerebral circulation 30(3):514–522
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K et al (1996) Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 335(25):1857–1863. doi:10.1056/NEJM199612193352501
Harukuni I, Bhardwaj A (2006) Mechanisms of brain injury after global cerebral ischemia. Neurol Clin 24(1):1–21. doi:10.1016/j.ncl.2005.10.004
Weitzdoerfer R, Pollak A, Lubec B (2004) Perinatal asphyxia in the rat has lifelong effects on morphology, cognitive functions, and behavior. Semin Perinatol 28(4):249–256
Lipton P (1999) Ischemic cell death in brain neurons. Physiol Rev 79(4):1431–1568
Abe K, Aoki M, Kawagoe J, Yoshida T, Hattori A, Kogure K, Itoyama Y (1995) Ischemic delayed neuronal death. A mitochondrial hypothesis. Stroke; a journal of cerebral circulation 26(8):1478–1489
Kim YM, Yim HW, Jeong SH, Klem ML, Callaway CW (2012) Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms?: a systematic review and meta-analysis of randomized and non-randomized studies. Resuscitation 83(2):188–196. doi:10.1016/j.resuscitation.2011.07.031
Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Bbttiger BW, Callaway C, Clark RS et al (2010) Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a scientific statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke (Part II). International emergency nursing 18(1):8–28. doi:10.1016/j.ienj.2009.07.001
Nielsen N, Friberg H, Gluud C, Herlitz J, Wetterslev J (2011a) Hypothermia after cardiac arrest should be further evaluated—a systematic review of randomised trials with meta-analysis and trial sequential analysis. Int J Cardiol 151(3):333–341. doi:10.1016/j.ijcard.2010.06.008
Perbet S, Mongardon N, Dumas F, Bruel C, Lemiale V, Mourvillier B, Carli P, Varenne O et al (2011) Early-onset pneumonia after cardiac arrest: characteristics, risk factors and influence on prognosis. Am J Respir Crit Care Med 184(9):1048–1054. doi:10.1164/rccm.201102-0331OC
Nielsen N, Sunde K, Hovdenes J, Riker RR, Rubertsson S, Stammet P, Nilsson F, Friberg H (2011b) Adverse events and their relation to mortality in out-of-hospital cardiac arrest patients treated with therapeutic hypothermia. Crit Care Med 39(1):57–64. doi:10.1097/CCM.0b013e3181fa4301
Sunde K (2013) Therapeutic hypothermia in cardiac arrest. Revista espanola de cardiologia 66(5):346–349. doi:10.1016/j.rec.2012.10.004
Jiang Z, Duong TQ (2016) Methylene blue treatment in experimental ischemic stroke: a mini review. Brain circulation 2(1):48–53. doi:10.4103/2394-8108.178548
Schirmer RH, Adler H, Pickhardt M, Mandelkow E (2011) Lest we forget you—methylene blue. Neurobiol Aging 32(12):2325 e2327–2325 e2316. doi:10.1016/j.neurobiolaging.2010.12.012
Oz M, Lorke DE, Petroianu GA (2009) Methylene blue and Alzheimer’s disease. Biochem Pharmacol 78(8):927–932. doi:10.1016/j.bcp.2009.04.034
Ahmed ME, Tucker D, Dong Y, Lu Y, Zhao N, Wang R, Zhang Q (2016) Methylene blue promotes cortical neurogenesis and ameliorates behavioral deficit after photothrombotic stroke in rats. Neuroscience 336:39–48. doi:10.1016/j.neuroscience.2016.08.036
Lu Q, Tucker D, Dong Y, Zhao N, Zhang Q (2016) Neuroprotective and functional improvement effects of methylene blue in global cerebral ischemia. Mol Neurobiol 53(8):5344–5355. doi:10.1007/s12035-015-9455-0
Wen Y, Li W, Poteet EC, Xie L, Tan C, Yan LJ, Ju X, Liu R et al (2011) Alternative mitochondrial electron transfer as a novel strategy for neuroprotection. J Biol Chem 286(18):16504–16515. doi:10.1074/jbc.M110.208447
Fang Q, Yan X, Li S, Sun Y, Xu L, Shi Z, Wu M, Lu Y et al (2016) Methylene blue ameliorates ischemia/reperfusion-induced cerebral edema: an MRI and transmission electron microscope study. Acta Neurochir Suppl 121:227–236. doi:10.1007/978-3-319-18497-5_41
Rodriguez P, Zhao J, Milman B, Tiwari YV, Duong TQ (2016) Methylene blue and normobaric hyperoxia combination therapy in experimental ischemic stroke. Brain and behavior 6(7):e00478. doi:10.1002/brb3.478
Dormoi J, Briolant S, Desgrouas C, Pradines B (2013) Impact of methylene blue and atorvastatin combination therapy on the apparition of cerebral malaria in a murine model. Malar J 12:127. doi:10.1186/1475-2875-12-127
Zoungrana A, Coulibaly B, Sie A, Walter-Sack I, Mockenhaupt FP, Kouyate B, Schirmer RH, Klose C et al (2008) Safety and efficacy of methylene blue combined with artesunate or amodiaquine for uncomplicated falciparum malaria: a randomized controlled trial from Burkina Faso. PLoS One 3(2):e1630. doi:10.1371/journal.pone.0001630
Xu CH, Yu LK, Cao L, Yang R, Yan J, Liu ZC, Wang Y (2016) Value of radial probe endobronchial ultrasound-guided localization of solitary pulmonary nodules with the combination of ultrathin bronchoscopy and methylene blue prior to video-assisted thoracoscopic surgery. Molecular and clinical oncology 5(2):279–282. doi:10.3892/mco.2016.913
Coulibaly B, Zoungrana A, Mockenhaupt FP, Schirmer RH, Klose C, Mansmann U, Meissner PE, Muller O (2009) Strong gametocytocidal effect of methylene blue-based combination therapy against falciparum malaria: a randomised controlled trial. PLoS One 4(5):e5318. doi:10.1371/journal.pone.0005318
D'Amico F (2005) A polychromatic staining method for epoxy embedded tissue: a new combination of methylene blue and basic fuchsine for light microscopy. Biotechnic & histochemistry : official publication of the Biological Stain Commission 80(5–6):207–210. doi:10.1080/10520290600560897
Zhang QG, Wang RM, Scott E, Han D, Dong Y, Tu JY, Yang F, Reddy Sareddy G et al (2013) Hypersensitivity of the hippocampal CA3 region to stress-induced neurodegeneration and amyloidogenesis in a rat model of surgical menopause. Brain : a journal of neurology 136(Pt 5):1432–1445. doi:10.1093/brain/awt046
Oh JS, Kim SW, Cho HJ, Kyong YY, Oh YM, Choi SM, Choi KH, Park KN (2013) Combination treatment with 17beta-estradiol and therapeutic hypothermia for transient global cerebral ischemia in rats. Am J Emerg Med 31(1):154–160. doi:10.1016/j.ajem.2012.06.033
Zhang QG, Raz L, Wang R, Han D, De Sevilla L, Yang F, Vadlamudi RK, Brann DW (2009) Estrogen attenuates ischemic oxidative damage via an estrogen receptor alpha-mediated inhibition of NADPH oxidase activation. The Journal of neuroscience : the official journal of the Society for Neuroscience 29(44):13823–13836. doi:10.1523/JNEUROSCI.3574-09.2009
Lu Y, Wang R, Dong Y, Tucker D, Zhao N, Ahmed ME, Zhu L, Liu TC et al (2017) Low-level laser therapy for beta amyloid toxicity in rat hippocampus. Neurobiol Aging 49:165–182. doi:10.1016/j.neurobiolaging.2016.10.003
Dalle-Donne I, Rossi R, Giustarini D, Milzani A, Colombo R (2003) Protein carbonyl groups as biomarkers of oxidative stress. Clinica chimica acta; international journal of clinical chemistry 329(1–2):23–38
Andresen M, Gazmuri JT, Marin A, Regueira T, Rovegno M (2015) Therapeutic hypothermia for acute brain injuries. Scandinavian journal of trauma, resuscitation and emergency medicine 23:42. doi:10.1186/s13049-015-0121-3
Zhang H, Zhou M, Zhang J, Mei Y, Sun S, Tong E (2008) Therapeutic effect of post-ischemic hypothermia duration on cerebral ischemic injury. Neurol Res 30(4):332–336. doi:10.1179/174313208X300279
Racay P, Tatarkova Z, Chomova M, Hatok J, Kaplan P, Dobrota D (2009) Mitochondrial calcium transport and mitochondrial dysfunction after global brain ischemia in rat hippocampus. Neurochem Res 34(8):1469–1478. doi:10.1007/s11064-009-9934-7
Dave KR, Saul I, Busto R, Ginsberg MD, Sick TJ, Perez-Pinzon MA (2001) Ischemic preconditioning preserves mitochondrial function after global cerebral ischemia in rat hippocampus. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 21(12):1401–1410. doi:10.1097/00004647-200112000-00004
Li PA, Kristian T, He QP, Siesjo BK (2000) Cyclosporin A enhances survival, ameliorates brain damage, and prevents secondary mitochondrial dysfunction after a 30-minute period of transient cerebral ischemia. Exp Neurol 165(1):153–163. doi:10.1006/exnr.2000.7459
Cafe C, Torri C, Gatti S, Adinolfi D, Gaetani P, Rodriguez YBR, Marzatico F (1994) Changes in non-synaptosomal and synaptosomal mitochondrial membrane-linked enzymatic activities after transient cerebral ischemia. Neurochem Res 19(12):1551–1555
DiMauro S, Schon EA (2003) Mitochondrial respiratory-chain diseases. N Engl J Med 348(26):2656–2668. doi:10.1056/NEJMra022567
Sims NR (1992) Energy metabolism and selective neuronal vulnerability following global cerebral ischemia. Neurochem Res 17(9):923–931
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J et al (2013) Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med 369(23):2197–2206. doi:10.1056/NEJMoa1310519
Yang SH, Li W, Sumien N, Forster M, Simpkins JW, Liu R (2015) Alternative mitochondrial electron transfer for the treatment of neurodegenerative diseases and cancers: methylene blue connects the dots. Prog Neurobiol. doi:10.1016/j.pneurobio.2015.10.005
Uttara B, Singh AV, Zamboni P, Mahajan RT (2009) Oxidative stress and neurodegenerative diseases: a review of upstream and downstream antioxidant therapeutic options. Curr Neuropharmacol 7(1):65–74. doi:10.2174/157015909787602823
Floyd RA, Carney JM (1992) Free radical damage to protein and DNA: mechanisms involved and relevant observations on brain undergoing oxidative stress. Ann Neurol 32(Suppl):S22–S27
Sofroniew MV (2009) Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci 32(12):638–647. doi:10.1016/j.tins.2009.08.002
Green SP, Cairns B, Rae J, Errett-Baroncini C, Hongo JA, Erickson RW, Curnutte JT (2001) Induction of gp91-phox, a component of the phagocyte NADPH oxidase, in microglial cells during central nervous system inflammation. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 21(4):374–384. doi:10.1097/00004647-200104000-00006
Urrutia PJ, Mena NP, Nunez MT (2014) The interplay between iron accumulation, mitochondrial dysfunction, and inflammation during the execution step of neurodegenerative disorders. Front Pharmacol 5:38. doi:10.3389/fphar.2014.00038
Witte ME, Geurts JJ, de Vries HE, van der Valk P, van Horssen J (2010) Mitochondrial dysfunction: a potential link between neuroinflammation and neurodegeneration? Mitochondrion 10(5):411–418. doi:10.1016/j.mito.2010.05.014
Madden LK, DeVon HA (2015) A systematic review of the effects of body temperature on outcome after adult traumatic brain injury. The Journal of neuroscience nursing : journal of the American Association of Neuroscience Nurses 47(4):190–203. doi:10.1097/JNN.0000000000000142
Bayir H, Adelson PD, Wisniewski SR, Shore P, Lai Y, Brown D, Janesko-Feldman KL, Kagan VE et al (2009) Therapeutic hypothermia preserves antioxidant defenses after severe traumatic brain injury in infants and children. Crit Care Med 37(2):689–695. doi:10.1097/CCM.0b013e318194abf2
Zhao M, Zhu P, Fujino M, Zhuang J, Guo H, Sheikh I, Zhao L, Li XK (2016) Oxidative stress in hypoxic-ischemic encephalopathy: molecular mechanisms and therapeutic strategies. Int J Mol Sci 17(12). doi:10.3390/ijms17122078
Toader AM, Filip A, Decea N, Muresan A (2013) Neuroprotective strategy in an experimental newborn rat model of brain ischemia and hypoxia: effects of resveratrol and hypothermia. Clujul medical 86(3):203–207
Shankaran S (2012) Therapeutic hypothermia for neonatal encephalopathy. Curr Treat Options Neurol 14(6):608–619. doi:10.1007/s11940-012-0200-y
Cai L, Thibodeau A, Peng C, Ji X, Rastogi R, Xin R, Singh S, Geng X et al (2016) Combination therapy of normobaric oxygen with hypothermia or ethanol modulates pyruvate dehydrogenase complex in thromboembolic cerebral ischemia. J Neurosci Res 94(8):749–758. doi:10.1002/jnr.23740
Briyal S, Gulati A (2010) Endothelin-A receptor antagonist BQ123 potentiates acetaminophen induced hypothermia and reduces infarction following focal cerebral ischemia in rats. Eur J Pharmacol 644(1–3):73–79. doi:10.1016/j.ejphar.2010.06.071
Ji X, Luo Y, Ling F, Stetler RA, Lan J, Cao G, Chen J (2007) Mild hypothermia diminishes oxidative DNA damage and pro-death signaling events after cerebral ischemia: a mechanism for neuroprotection. Frontiers in bioscience : a journal and virtual library 12:1737–1747
Karibe H, Chen SF, Zarow GJ, Gafni J, Graham SH, Chan PH, Weinstein PR (1994) Mild intraischemic hypothermia suppresses consumption of endogenous antioxidants after temporary focal ischemia in rats. Brain Res 649(1–2):12–18
Deng G, Yonchek JC, Quillinan N, Strnad FA, Exo J, Herson PS, Traystman RJ (2014) A novel mouse model of pediatric cardiac arrest and cardiopulmonary resuscitation reveals age-dependent neuronal sensitivities to ischemic injury. J Neurosci Methods 222:34–41. doi:10.1016/j.jneumeth.2013.10.015
Ostadal P, Mlcek M, Kruger A, Horakova S, Skabradova M, Holy F, Svoboda T, Belohlavek J et al (2013) Mild therapeutic hypothermia is superior to controlled normothermia for the maintenance of blood pressure and cerebral oxygenation, prevention of organ damage and suppression of oxidative stress after cardiac arrest in a porcine model. J Transl Med 11:124. doi:10.1186/1479-5876-11-124
Guerra-Wallace MM, Casey FL 3rd, Bell MJ, Fink EL, Hickey RW (2013) Hyperoxia and hypoxia in children resuscitated from cardiac arrest. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 14(3):e143–e148. doi:10.1097/PCC.0b013e3182720440
Zhang H, Zhang JJ, Mei YW, Sun SG, Tong ET (2011) Effects of immediate and delayed mild hypothermia on endogenous antioxidant enzymes and energy metabolites following global cerebral ischemia. Chin Med J 124(17):2764–2766
Gong P, Hua R, Zhang Y, Zhao H, Tang Z, Mei X, Zhang M, Cui J et al (2013) Hypothermia-induced neuroprotection is associated with reduced mitochondrial membrane permeability in a swine model of cardiac arrest. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 33(6):928–934. doi:10.1038/jcbfm.2013.33
Ginimuge PR, Jyothi SD (2010) Methylene blue: revisited. J Anaesthesiol Clin Pharmacol 26(4):517–520
Ramirez Rivera J, Garayua JE (2006) Methemoglobinemia: life-threatening hazard of multiple drug ingestions. Boletin de la Asociacion Medica de Puerto Rico 98(2):118–121
Tardivo JP, Del Giglio A, de Oliveira CS, Gabrielli DS, Junqueira HC, Tada DB, Severino D, de Fatima TR et al (2005) Methylene blue in photodynamic therapy: from basic mechanisms to clinical applications. Photodiagn Photodyn Ther 2(3):175–191. doi:10.1016/S1572-1000(05)00097-9
Gillman PK (2006) Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia 61(10):1013–1014. doi:10.1111/j.1365-2044.2006.04808.x
Vincer MJ, Allen AC, Evans JR, Nwaesei C, Stinson DA (1987) Methylene-blue-induced hemolytic anemia in a neonate. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne 136(5):503–504
Acknowledgment
This study was supported by Research Grant NS086929 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, USA; an American Heart Association Grant-in-Aid 15GRNT25240004; and a science and technology project of Xuzhou city, Jiangsu (KC15SH093).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animal procedures were approved by the institutional animal use committee and conformed to the local and international guidelines on the ethical use of animals.
Conflict of Interest
The authors declare that there is no conflict of interest.
Additional information
Lei Li and Rongli Yang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, L., Yang, R., Li, P. et al. Combination Treatment with Methylene Blue and Hypothermia in Global Cerebral Ischemia. Mol Neurobiol 55, 2042–2055 (2018). https://doi.org/10.1007/s12035-017-0470-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0470-1