Abstract
Hypoxanthine, the major oxypurine metabolite involved in purine’s salvage pathway in the brain, is accumulated in Lesch-Nyhan disease, an inborn error of metabolism of purine. The purpose of this study was to investigate the effects of hypoxanthine intrastriatal administration on infant and young adult rats submitted to stereotactic surgery. We analyzed the effect of hypoxanthine on neuroinflammatory parameters, such as cytokine levels, immunocontent of NF-κB/p65 subunit, iNOS immunocontent, nitrite levels, as well as IBA1 and GFAP immunocontent in striatum of infant and young adult rats. We also evaluate some oxidative parameters, including reactive species production, superoxide dismutase, catalase, glutathione peroxidase activities, as well as DNA damage. Wistar rats of 21 and 60 days of life underwent stereotactic surgery and were divided into two groups: control (infusion of saline 0.9 %) and hypoxanthine (10 μM). Intrastriatal administration of hypoxanthine increased IL-6 levels in striatum of both ages of rats tested, while TNF-α increased only in 21-day-old rats. Hypoxanthine also increased nuclear immunocontent of NF-κB/p65 subunit in striatum of both ages of rats. Nitrite levels were decreased in striatum of 21-day-old rats; however, the immunocontent of iNOS was increased in striatum of hypoxanthine groups. Microglial and astrocyte activation was seen by the increase in IBA1 and GFAP immunocontent, respectively, in striatum of infant rats. All oxidative parameters were altered, suggesting a strong neurotoxic hypoxanthine role on oxidative stress. According to our results, hypoxanthine intrastriatal administration increases neuroinflammatory parameters perhaps through oxidative misbalance, suggesting that this process may be involved, at least in part, to neurological disorders found in patients with Lesch-Nyhan disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Purines are a class of molecules that present several functions for the cellular biology, for instance nucleic acid synthesis, cofactor reactions, energy-consuming reactions, and cellular signaling. Hypoxanthine is the major purine metabolite involved in the purine’s salvage pathway in the brain. This mechanism is vital for the maintenance of physiologic purine levels. Deficiency of hypoxanthine-guanine phosphoribosyltransferase (HPRT, EC 2.4.2.8) activity leads to the inborn error of metabolism known as Lesch-Nyhan disease (LND), which is characterized by high levels of oxypurines, mainly hypoxanthine and uric acid [1–3].
HPRT is present in all tissues and distributed equally throughout the brain [4], although the symptoms presented by LND patients seem to be related more specifically to extrapyramidal effects and basal ganglia dysfunction [5]. LND patients present five times the normal concentration of hypoxanthine, but rather normal levels of xanthine in cerebrospinal fluid [6, 7]. However, brain tissue has relatively lower levels of xanthine oxidase; therefore, the production of uric acid from xanthine and hypoxanthine is narrow [8]. Histopathological studies showed that patients with LND present a decrease in brain volume and a white matter deficit more pronounced than gray matter [9], probably caused by a developmental deficiency rather than a degenerative one [10]. Symptomatology of LND patients is motor dysfunction (spasticity, dystonia), cerebral palsy, cognitive and behavioral disturbances, and self-mutilation behavior, as well as hyperuricemia [11, 12].
Central nervous system (CNS) has several mechanisms responsible for maintaining immune homeostasis. Microglia is the basic neuroinflammatory mediator, responding as the major brain’s immune cells. Neuroinflammation is characterized by activation of microglia and astrocyte with consequent release of many factors that modulate pro- and anti-inflammatory mediators, such as cytokines, chemokines, nitric oxide (NO), prostaglandins, growth factors, superoxide species, and nuclear factor-kappa B (NF-κB) translocation [13–15].
It is well established that high levels of reactive species induce oxidative stress, promoting several cellular injury as lipid, protein, and DNA damage [16]. It has been demonstrated the hypoxanthine/xanthine oxidase action as a source of oxidative stress in the vascular system [17]. Previous works have shown hypoxanthine’s capability to induce lipid peroxidation, reduce total radical-trapping antioxidant parameter, and also alter antioxidant enzymes [18, 19].
Since LND symptoms generally occur in early stage of life and the average life expectancy of patient with LND under treatment is early- to mid-20s [11], in the current research we aimed to evaluate hypoxanthine intrastriatal administration in infant and young adult rats. In order to verify whether high hypoxanthine levels could alter neuroinflammatory profile and its mechanism, in the present study we evaluated the effect of intrastriatal hypoxanthine administration on some neuroinflammatory parameters such as pro-inflammatory cytokines interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α), immunocontent of NF-κB, inducible nitric oxide synthase (iNOS), nitrite levels, as well as on microglial and astrocyte markers including ionized calcium-binding adapter molecule 1 (IBA1) and glial fibrillary acidic protein (GFAP). Some oxidative parameters such as reactive species generation, antioxidant enzymes activities, and DNA damage were also evaluated.
Materials and Methods
Animals and Reagents
Male Wistar rats of 21 (infant) and 60-day-old (young adult) were obtained from the Central Animal House of the Department of Biochemistry of the Universidade Federal do Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brazil. Animals were maintained under a standard dark–light cycle (lights on between 07:00 and 19:00 hours) at a room temperature of 22 ± 1 °C, with free access to a 20 % (w/w) commercial protein chow and water. Animal care followed the official governmental guidelines in compliance with the Federation of Brazilian Societies for Experimental Biology and was approved by the Ethical Committee of the Universidade Federal do Rio Grande do Sul, Brazil (#25717).
Acrylamide, bisacrylamide, SDS, and β-mercaptoethanol used in sodium dodecylsulfate polyacrylamide gel electrophoresis (SDS-PAGE) were purchased from Sigma Chemical Co. (St. Louis, MO, USA). Polyclonal antibodies were purchased from Santa Cruz Biotechnology, BD Biosciences, and Cell Signaling Technology. Anti-rabbit IgG peroxidase-conjugated and reagents to detect chemiluminescence (ECL) were purchased from Amersham Pharmacia Biotech (Piscataway, NJ, USA). Hybond-C nitrocellulose membranes were from Hybond-ECL (Hybond-ECL-nitrocellulose membrane, Amersham Biosciences, Freiburg, Germany). All other chemical reagents used for analysis were obtained from Sigma Aldrich Co., St. Louis, MO, USA.
Experimental Procedure
The model developed in this experimental study was based on the infusion of hypoxanthine directly into the right striatum, using a stereotactic apparatus, which is widely described in the current scientific literature [20–22]. In this technique, the coordinates specific to the right striatum for each age of rats were based on the stereotactic atlas coordinates developed by Paxinos and Watson [23] (coordinates relative from bregma for 21- and 60-day-old rats, respectively: AP −0.6 mm, ML −3.0 mm, V −4.0 mm from the dura; AP −0.5 mm, ML −2.5 mm, V −2.5 mm from the dura). In all experiments, the intrastriatal infusions of the drug occurred 2 days after surgery, to avoid any influence of anesthetic substances on the results, since studies show neuroprotective effect for xylazine and ketamine [24]. Later, a needle (0.9 mm) infusion was adjusted within the guide cannula placed in the animal and 2 μL of a solution of hypoxanthine (20 pmol/2 μL) or vehicle (saline 0.9 %) was administered in the right striatum of the animal 1 μL per minute. Thus, the animals were divided into two groups: (1) control (saline infusion); (2) hypoxanthine (hypoxanthine infusion). Animals were sacrificed by decapitation without anesthesia 30 min after the saline or hypoxanthine infusion, brain was dissected, and the structure analyzed was striatum. Hypoxanthine dose used in our study was chosen according to Puig and colleagues [25], being equivalent to that found in patients with Lesch-Nyhan disease. This model was used throughout all experiments described in this work.
Cytokines (IL-6 and TNF-α) Assay
Striatum was homogenized in 1:5 (w/v) saline (0.9 % NaCl). The homogenate was centrifuged at 800×g for 10 min at 4 °C, being the supernatant used for the technic. IL-6 and TNF-α levels in striatum were quantified by a rat high-sensitivity enzyme-linked immunoabsorbent assays (ELISA) with commercially available kits (InvitrogenTM, Life Technologies, Carlsbad, CA, USA) as described by Scherer et al. [26].
Cellular Fractionation for Cytosolic and Nuclear NF-κB/p65 Subunit
Cellular fractionation for cytosolic and nuclear NF-κB/p65 subunit was obtained as described by da Cunha et al. [27]. Striatum was homogenized in 300 μL hypotonic lysis buffer containing 10 mM HEPES (pH 7.9), 1.5 mM MgCl2, 10 mM KCl, 0.5 mM phenylmethylsulfonyl fluoride (PMSF), 1 mM dithiothreitol (DTT), 5 mM NaF, 1 mM sodium orthovanadate plus protease inhibitor cocktail. Samples homogenate were then lysed with 18 μL 10 % IGEPAL. The homogenate was centrifuged (14,000×g, 30 s, 4 °C), and supernatants containing the cytosolic fraction were stored at −80 °C. The nuclear pellet was resuspended in 200 μL ice-cold hypertonic extraction buffer (10 mM HEPES (pH 7.9), 0.40 M NaCl, 1.5 mM MgCl2, 10 mM KCl, 0.5 mM PMSF, 1 mM DTT, 5 mM NaF, 1 mM sodium orthovanadate, 0.25 mM EDTA, 25 % glycerol plus protease inhibitor cocktail). After 40 min of intermittent mixing, extracts were centrifuged (14,000×g, 10 min, 4 °C), and supernatants containing nuclear protein were secured. For electrophoresis analysis, aliquot samples were dissolved in 25 % (v/v) of a solution containing 40 % glycerol, 5 % mercaptoethanol, and 50 mM Tris–HCl, pH 6.8.
Western Blotting Analysis of NF-κB/p65 Subunit, iNOS, IBA1, and GFAP
Protein samples were separated by 10 % SDS-PAGE (30 μg/lane of total protein) and transferred (Trans-blot SD semidry transfer cell, BioRad) to nitrocellulose membranes for 1 h at 15 V in transfer buffer (48 mM Trizma, 39 mM glycine, 20 % methanol, and 0.25 % SDS). The blot was then washed for 10 min in Tris-buffered saline (TBS) (0.5 M NaCl, 20 mM Trizma, pH 7.5), followed by a 2-h incubation in blocking solution (TBS plus 5 % bovine serum albumin (BSA)). After incubation, the blot was washed twice for 5 min with blocking solution plus 0.05 % Tween-20 (T-TBS) and then incubated overnight at 4 °C in blocking solution containing the respective antibody anti-NF-κB p65 (1:1000; Santa Cruz Biotechnology), iNOS antibody diluted 1:1000 (Sigma-Aldrich), rabbit polyclonal anti-IBA1 (1:1000, Wako), anti-GFAP (1:2000, Cell Signaling Technology), and anti-β-actin (1:1000, Cell Signaling Technology). The blot was then washed twice for 5 min with T-TBS and incubated for 2 h in antibody solution containing peroxidase-conjugated anti-mouse IgG or peroxidase-conjugated anti-rabbit IgG diluted 1:2000. The blot was again washed twice for 5 min with T-TBS and twice for 5 min with TBS. The blot was developed using a chemiluminescence kit (Immobilon Western Chemiluminescent HRP Substrate, Millipore) and detected by ImageQuant LAS 4000 (GE Healthcare Life Sciences).
Nitrite Assay
For nitrite levels measurement, 100 μL of supernatant of striatum was mixed with 100 μL Griess reagent (1:1 mixture of 1 % sulfanilamide in 5 % phosphoric acid and 0.1 % naphthylethylenediamine dihydrochloride in water) and incubated in 96-well plates for 10 min at room temperature [28, 29]. The absorbance was measured on a microplate reader at a wavelength of 543 nm. Nitrite concentration was calculated using sodium nitrite standards.
Oxidative Stress Parameters Assays
Striatum was homogenized in 10 volumes (1:10, w/v) of 20 mM sodium phosphate buffer, pH 7.4, containing 140 mM KCl. Then the homogenates were centrifuged at 800×g for 10 min at 4 °C. The pellet was discarded, and the supernatant was used for the measurements of oxidative stress parameters as described by Schmitz and colleagues [30].
2′7′-Dichlorofluorescein Fluorescence Assay
Reactive oxygen species production was measured according to LeBel and colleagues [31] which is based on oxidation of 2′7′-dichlorofluorescein (H2DCF). Samples were incubated in a medium containing 100 μM 2′7′-dichlorofluorescein diacetate (H2DCF-DA) solution. The reaction produces dichlorofluorescein (DCF), a fluorescent compound which is measured at λ em = 488 nm and λ ex = 525 nm. Results were represented as nanomole DCF/milligram protein.
Superoxide Dismutase Assay
Superoxide dismutase (SOD) activity assay was performed according to Marklund [32]. SOD activity is measured through pyrogallol autoxidation, a process highly dependent on superoxide, which is a substrate for this enzyme. Hence, in the presence of SOD, pyrogallol autoxidation is inhibited, and the activity was then indirectly assayed at 420 nm. A calibration curve was performed with purified SOD as a standard. The results were represented as units per milligram of protein.
Catalase Assay
Catalase (CAT) activity was assayed based on the consumption of H2O2 at 240 nm in a reaction medium containing 20 mM H2O2, 0.1 % Triton X-100, 10 mM potassium phosphate buffer pH 7.0, and 0.1–0.3 mg protein/mL [33]. The results were represented as units per milligram of protein, being one CAT unit 1 μmol of H2O2 consumed per minute.
Glutathione Peroxidase Assay
Glutathione peroxidase (GPx) activity was measured utilizing tert-butyl-hydroperoxide as a substrate [34]. NADPH disappearance was monitored at 340 nm. The medium contained 2 mM glutathione, 0.15 U/mL glutathione reductase, 0.4 mM azide, 0.5 mM tert-butyl-hydroperoxide, and 0.1 mM NADPH. The specific activity is represented as units per milligram of protein, being one GPx unit 1 μmol of NADPH consumed per minute.
Single Cell Gel Electrophoresis (Comet Assay)
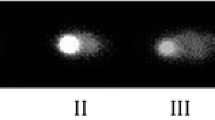
Alkaline comet assay was performed as described by Singh and colleagues [35] in accordance with general guidelines for the use of the comet assay [36, 37]. Striatum were homogenized in phosphate-buffered saline (PBS) and the samples were suspended in agarose and spread onto a glass microscope slide pre-coated with agarose, which set at 4 °C for 5 min. To maintain DNA as “nucleoids,” slides were incubated in ice-cold lyses solution (2.5 M NaCl, 100 mM EDTA, 10 mM Tris, pH 10.0, and 1 % triton X-100 with 10 % DMSO) removing cell proteins. Afterwards, slides were placed on a horizontal electrophoresis system, covered with fresh solution (300 mM NaOH plus 1 mM EDTA, pH > 13) for 20 min at 4 °C allowing DNA to unwind and express of alkali-labile sites. Electrophoresis was performed for 20 min (25 V; 300 mA; 0.9 V/cm). The slides were then neutralized, washed in bi-distilled water, and stained with silver staining protocol. Gels were analyzed in optical microscope after drying at room temperature overnight. One hundred cells (50 cells from each of the two replicate slides) were selected and evaluated. Cells received a scored according to the tail length, from 0 (no migration) to 4 (maximal migration) according to tail intensity [36]. Therefore, the damage index (DI) for cells ranged from 0 (all cells with no migration) to 400 (all cells with maximal migration). The slides were analyzed under blind conditions at least by two different individuals.
Protein Determination
Protein content of samples was measured by Lowry and colleagues [38] using bovine serum albumin as standard.
Statistical Analysis
Data were analyzed by Student’s t test was used to evaluate the different parameters. Analyses were performed using the Statistical Package for the Social Sciences (SPSS) software, in a PC-compatible computer. Differences were considered statistically significant if p < 0.05.
Results
Initially, we investigated the effect of hypoxanthine administration on immunocontent of cytosolic and nuclear fraction of NF-κB/p65 subunit. Panels a and b of Fig. 1 show that hypoxanthine administration significantly increased the immunocontent of nuclear fraction of NF-κB/p65 subunit in striatum of 21- [t(5) = 3.20; p < 0.05] and 60-day-old rats [t(5) = 6.39; p < 0.01], but no alteration was observed in cytosolic fraction of NF-κB/p65 subunit in rat striatum of 21- [t(5) = 1.09; p > 0.05] and 60-day-old [t(5) = 1.42; p > 0.05], as compared to control.
Effects of hypoxanthine intrastriatal administration on cytosolic and nuclear fraction of NF-κB/p65 subunit. a Striatum of 21-day-old rats and b striatum of 60-day-old rats. Results are expressed as percentage of control. Uniformity of gel loading was confirmed with β-actin as standard. Data are mean ± SD for six to seven animals in each group. Different from control, *p < 0.05, **p < 0.01 (Student’s t test). Hpx, hypoxanthine; NF-κB, nuclear factor-kappa B
Since NF-κB regulates the innate immune response, which is activated rapidly in response to a wide range of stimuli, including pro-inflammatory cytokines (IL-6 and TNF-α) [39], we evaluated the effect of hypoxanthine administration on cytokine levels (IL-6 and TNF-α) in striatum of 21- and 60-day-old rats. Figure 2a shows that hypoxanthine administration increased IL-6 in rat striatum of 21-day-old [t(5) = 3.92; p < 0.005] and of 60-day-old [t(5) = 3.77; p < 0,005] (Fig. 2b). TNF-α was significant increase in striatum of 21-day-old [t(5) = 2.57; p < 0.05], but not in 60-day-old rats [t(5) = 0.84; p > 0.05].
Effects of hypoxanthine intrastriatal administration on cytokines levels in striatum of infant and young adult rats. a IL-6 in 21-day-old rats; b IL-6 in 60-day-old rats; c TNF-α in 21-day-old rats; and d TNF-α in 60-day-old rats. Results are expressed as picogram per milligram of protein. Data are mean ± SD for five to six animals in each group. Different from control, *p < 0.05, **p < 0.01 (Student’s t test). Hpx, hypoxanthine; IL-6, interleukin-6; TNF-α, tumor necrosis factor alpha
Considering that NF-κB is associated with several inflammation mediators, including iNOS [40, 41], we evaluated the iNOS immunocontent and nitrite levels in striatum of infant and young adult rats. Figure 3a, b shows a significant increase in iNOS immunocontent in striatum of rats of both ages [21-day-old: t(6) = 2.64, p < 0.05; and 60-day-old: t(6) = 5.04, p < 0.001]. Figure 3c, d shows that hypoxanthine administration was able to diminished nitrite levels in striatum of infant rats [t(6) = 4.93; p < 0.001], but not in young adult rats [t(6) = 0.18; p > 0.05].
Effects of hypoxanthine intrastriatal administration on inducible nitric oxide synthase immunocontent and nitrite levels. a iNOS immunocontent in striatum of 21-day-old rats and b striatum of 60-day-old rats. Results are expressed as percentage of control. Uniformity of gel loading was confirmed with β-actin as standard. Data are mean ± SD for six to seven animals in each group. c Nitrite levels in striatum of 21-day-old rats and d striatum of 60-day-old rats. Results are expressed as micromole per milligram of protein. Data are mean ± SD for six to seven animals in each group. Different from control, *p < 0.05, ***p < 0.001 (Student’s t test). Hpx, hypoxanthine; iNOS, inducible nitric oxide synthase
In order to evaluate the effect of hypoxanthine on immune response of glial cells, we measured the immunocontent of IBA1 and GFAP with the aiming of analyze both microglia and astrocyte activation, respectively. Accordingly, we notice an increase in the immunocontent of IBA1 [t(6) = 4.20; p < 0.01] and GFAP [t(6) = 2.39; p < 0.05] in striatum of 21-day-old rats when compared to control group (Fig. 4a, c). However, there was no significant change in the immunocontent of both proteins in 60-day-old rats (Fig. 4b, d).
Effects of hypoxanthine intrastriatal administration on microglial and astrocyte activation. a IBA1 immunocontent in striatum of 21-day-old rats and b IBA1 immunocontent in striatum of 60-day-old rats. c GFAP immunocontent in striatum of 21-day-old rats and d GFAP immunocontent in striatum of 60-day-old rats. Results are expressed as percentage of control. Uniformity of gel loading was confirmed with β-actin as standard. Data are mean ± SD for six to seven animals in each group. Different from control, *p < 0.05, **p < 0.01 (Student’s t test). Hpx, hypoxanthine; IBA1, ionized calcium-binding adapter molecule 1; GFAP, glial fibrillary acidic protein
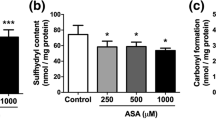
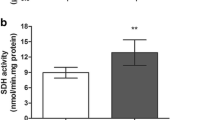
Since neuroinflammation is involved in oxidative stress and vice versa, we decided to evaluate hypoxanthine effect on some oxidative parameters in striatum of rats. Firstly, we measured reactive species production by oxidation of H2DCF, which is increased in infant [t(6) = 3.32; p < 0.01] and young adult rats [t(6) = 2.47; p < 0.05] (Fig. 5a, b). Regarding antioxidant status, previous studies from our group [18, 42] are important to highlight, due to the results obtained on SOD, CAT, and GPx activities in striatum of 60-day-old rats. In the present study, this led us to evaluate the same enzymes in striatum of 21-day-old rats. Figure 5c–e shows a decrease in the activities of SOD, CAT, and GPx [t(6) = 2.49; p < 0.05; t(6) = 2.24; p < 0.05; t(6) = 2.82; p < 0.05], respectively. We also analyze DNA damage detected a massive increase in DNA damage index in striatum of infant [t(6) = 21.08; p < 0.0001] and young adult [t(6) = 53.68; p < 0.0001] rats, when compared to control group (Fig. 5f, g).
Effects of hypoxanthine intrastriatal administration on oxidative parameters. a H2DCF oxidation in striatum of 21-day-old rats and b striatum of 60-day-old rats. Results are expressed as nanomole per milligram of protein. c SOD activity; d CAT activity; and e GPx activity in striatum of 21-day-old rats. Results are expressed as units per milligram of protein. f DNA damage index in striatum of 21-day-old rats and g striatum of 60-day-old rats. Results are expressed as DNA damage index. Data are mean ± SD for six to seven animals in each group. Different from control, *p < 0.05, **p < 0.01, ***p < 0.001 (Student’s t test). Hpx, hypoxanthine; H 2 DCF, 2′7′-dichlorofluorescein; SOD, superoxide dismutase; CAT, catalase; GPx, glutathione peroxidase
Discussion
Severe variation in purine salvage pathway as a result of HPRT activity deficiency causes LND, leading to hypoxanthine accumulation in patient’s urine, plasma, and cerebrospinal fluid [3]. Although the underlying mechanisms of brain dysfunction in LND are insufficiently understood, the accumulation of oxypurines, essentially hypoxanthine, has been proposed to contribute to the neurological dysfunction present in this disease [7]. A recent study showed that high hypoxanthine levels alter various transcription factors related in early development of neuronal dopamine and in pan-neuronal differentiation with elevated expression of neurotransmitter receptors for dopamine, adenosine, and serotonin in cellular model, as seen by Torres and Puig [43]
For a long time, CNS was considered to be “immune prerogative,” not being responsive or cooperate with inflammation. Nowadays, it is known that the CNS has a certain role in inflammation, and response to injury, infection or disease, resident CNS cells, mainly microglia, that generates inflammatory mediators that modulate the pro- and anti-inflammatory mediators (cytokines, chemokine, NO, PGs, growth factors, and the species of superoxide). These mediators upregulate adhesion molecules, increase permeability of the blood-brain barrier, facilitating the invasion of peripheral immune cells, inducing the release of potentially toxic molecules that can compromise brain cells [44]. A relation among neuroinflammation, oxidative stress, neurodegenerative disease, and others disorders has been suggested [45]. Based on these, the purpose of the present study was to evaluate pro-inflammatory cytokines levels, NF-κB/p65 subunit immunocontent, nitrite levels, iNOS immunocontent, as well as immunocontent of IBA1 and GFAP in striatum of 21- and 60-day-old rats subjected to intrastriatal administration of hypoxanthine. Some oxidative parameters such as reactive species generation, antioxidant enzymes activities, and DNA damage were also evaluated.
It is well known that NF-κB is activated in consequence of inflammation. Other member of the NF-κB family, NF-κB/p65, is situated in the cytoplasm bound to inhibitory proteins (IκB), hence inactivated. Activation induces nuclear translocation of NF-κB/p65, followed by transcriptional activation of specific target genes [46]. These translocations are often frequently taken as indicators of NF-κB activation and are related with cellular response to oxidants or to the inflammatory and acute immune response [15]. NF-κB has been associated with several inflammatory mediators such as IL-6 [47–49], TNF-α [50, 51], and iNOS [40, 41, 52]. In our study, there was an increase immunocontent nuclear NF-κB/p65 subunit in striatum of infant and young adult rats subjected to intrastriatal injection of hypoxanthine (Fig. 1). Cytokines are molecules involved in signal transmission between cells during the initiation of immune responses. Results showed that the hypoxanthine intrastriatal administration provoked an increase in pro-inflammatory cytokines, including IL-6 and TNF-α, in striatum of 21-day-old rats and only IL-6 increases in 60-day-old rats (Fig. 2). In agreement with our results, Gudbjornsson and colleagues [53] showed that hypoxanthine is related to inflammation of rheumatoid arthritis, which presents enhanced purine metabolism and diffusion of oxypurines. Although the mechanism(s) by which hypoxanthine acts on inflammation are not fully understood, our findings suggest that the increase in cytokines levels could be closely related to NF-κB activation.
Another relevant inflammatory mediator is NO. Oxidation products, nitrite, and nitrate are the main metabolites that can be used as an indicator of NO production [54]. NO is produced by converting the amino acid L-arginine to L-citrulline by the action of nitric oxide synthase (NOS). Inducible nitric oxide synthase (iNOS) is an isoform that is expressed via cytokines, endotoxins, and other inflammation mediators being expressed mainly in microglial cells, neutrophils, macrophages, fibroblasts, endothelial cells, and the vascular smooth muscle and mediates the production of large amounts of NO [55, 56]. To understand hypoxanthine mechanism on inflammation, we also evaluated nitrite levels in rats subjected to hypoxanthine administration. We observed that hypoxanthine decreases nitrite levels in striatum of 21-day-old rats but do not alter in 60-day-old (Fig. 3c, d). It has been shown that there is a relation between the formation of NO and synthesis of reactive species, such as superoxide and hydrogen peroxide [57]. Hydrogen peroxide can also react with NO generating peroxynitrite, a powerful cytotoxic substance [58], suggesting a diminished bioavailability of NO. This possibly explains the decrease in nitrite levels in striatum of infant rats.
Since iNOS is responsible for catalyzing the formation of NO through inflammatory stimuli and closely related to NF-κB activation, we also analyzed iNOS immunocontent. Results showed an increase in this enzyme immunocontent in striatum of 21- and 60-day-old rats (Fig. 3a, b). Increased protein expression of iNOS is an indicative of neuroinflammatory and neurodegeneration, which seems to be related to microglial activation [57, 59].
We also analyzed microglial and astrocyte activation, measuring IBA1 and GFAP immunocontent, respectively. Microglia, the major antigen presenting in CNS, can react promptly to antigens, releasing several inflammatory factors previous mentioned in this study such as NO, TNF-α, IL-6, and others. Excessive microglial activation is now known to corroborate to CNS disease by the liberation of cytotoxic factors leading to neuron damage [57, 60, 61]. Our results showed that hypoxanthine increased IBA1 immunocontent only in 21-day-old rats (Fig. 4a). Microglia can increase iNOS expression as well as NADPH oxidase, generating a great deal of NO and O2, which could act as inflammatory agents and promote microglial activation, as well as peroxynitrite synthesis, as mentioned earlier, a major cytotoxic metabolite [57, 60]. There was no change in IBA1 immunocontent in 60-day-old rats, this could be explained by the close relation between TNF-α and microglial activation [62].
Control of synapse formation, maturation, and elimination are astrocyte function, which are essential to development and maintenance of neural circuits. Together with microglia, astrocyte contributes to regulation of the neuroinflammation, being responsible for immune role of the CNS [63]. Loss of normal functions and gain of abnormal effects are some consequences of reactive astrocytes, being feature in a variety of disease processes [64]. Upregulation of intermediate filament proteins, particularly GFAP by reactive astrocytes, is probably the finest hallmark of reactive astrocytes and reactive gliosis measure [65]. Hypoxanthine was able to increase GFAP immunoreactivity in infant rats’ striatum, suggesting an astrogliosis event. No alteration was seen in young adult rats, perhaps by difference in the neurodevelopmental stage, meaning that infant rats are more bound to suffer from hypoxanthine administration and its neuroinflammatory effects.
Since one of the possible mechanism in which NF-κB may be acting as a pro-inflammatory signal is via oxidative stress [66] and hypoxanthine may have a oxidative effect [18, 19], we decide to analyze some oxidative parameters in both ages of rats. Our results showed an increase in reactive species production seen by H2DCF oxidation in infant and young adult rats; antioxidant enzyme deregulation in striatum of 21-day-old rats. Similar alteration was seen by Bavaresco and colleagues [42] in 60-day-old rats. It has been known that reactive oxygen species can attack directly the DNA producing single strand breaks [67]; in our study, we observed DNA damage, what may link hypoxanthine strongly to oxidative stress formation. This mechanism could explain the generation of inflammatory profile caused by hypoxanthine.
In summary, our findings demonstrated that intrastriatal administration of hypoxanthine presented an increase in pro-inflammatory cytokine levels, NF-κB, and iNOS, decreased nitrite levels, as well as altered microglial and astrocyte activation, suggesting that this substance may promote a pro-inflammatory status in striatum of infant and young adult rats by generation of oxidative stress. This study provides new basis elucidating hypoxanthine toxicity mechanisms on inflammatory and oxidative parameters, suggesting that this processes may be involved, at least in part, with disorders found in patients with LND.
References
Lesch M, Nyhan WL (1964) A familial disorder of uric acid metabolism and central nervous system function. Am J Med 36:561–570
Nyhan WL (1978) Ataxia and disorders of purine metabolism: defects in hypoxanthine guanine phosphoribosyl transferase and clinical ataxia. Adv Neurol 21:279–287
Jinnah H, Friedmann T (2001) Lesch-Nyhan disease and its variants. In: Scriver C, Beaudet A, Sly W, Valle D (eds) Metabolic molecular bases of inherited disease. Mc Graw-Hill, New York, pp 2537–2569
Jinnah HA, Hess EJ, Wilson MC, Gage FH, Friedmann T (1992) Localization of hypoxanthine-guanine phosphoribosyltransferase mRNA in the mouse brain by in situ hybridization. Mol Cell Neurosci 3:64–78. doi:10.1016/1044-7431(92)90010-Y
Visser J, Bär P, Jinnah H (2000) Lesch–Nyhan disease and the basal ganglia. Brain Res Rev 32:449–475. doi:10.1016/S0165-0173(99)00094-6
Harkness RA, McCreanor GM, Watts RWE (1988) Lesch-Nyhan syndrome and its pathogenesis: purine concentrations in plasma and urine with metabolite profiles in CSF. J Inherit Metab Dis 11:239–252. doi:10.1007/BF01800365
Rosenbloom FM, Kelley WN, Miller J, Henderson JF, Seegmiller JE (1967) Inherited disorder of purine metabolism. Correlation between central nervous system dysfunction and biochemical defects. JAMA 202:175–177
Schultz V, Lowenstein JM (1976) Purine nucleotide cycle. Evidence for the occurrence of the cycle in brain. J Biol Chem 251:485–492
Schretlen DJ, Varvaris M, Vannorsdall TD, Gordon B, Harris JC, Jinnah HA (2015) Brain white matter volume abnormalities in Lesch-Nyhan disease and its variants. Neurology 84:190–196. doi:10.1212/WNL.0000000000001128
Göttle M, Prudente CN, Fu R, Sutcliffe D, Pang H, Cooper D, Veledar E, Glass JD, Gearing M, Visser JE, Jinnah HA (2014) Loss of dopamine phenotype among midbrain neurons in Lesch-Nyhan disease. Ann Neurol. doi: 10.1002/ana.24191
Jinnah HA, Sabina RL, Van Den Berghe G (2013) Metabolic disorders of purine metabolism affecting the nervous system. Handb Clin Neurol 113:1827–1836. doi:10.1016/B978-0-444-59565-2.00052-6
Torres RJ, Puig JG (2008) The diagnosis of HPRT deficiency in the 21st century. Nucleosides Nucleotides Nucleic Acids 27:564–569. doi:10.1080/15257770802135778
Das Sarma J (2014) Microglia-mediated neuroinflammation is an amplifier of virus-induced neuropathology. J Neurovirol 20:122–136. doi:10.1007/s13365-013-0188-4
Ghirnikar RS, Lee YL, Eng LF (1998) Inflammation in traumatic brain injury: role of cytokines and chemokines. Neurochem Res 23:329–340
Dallot E, Méhats C, Oger S, Leroy M-J, Breuiller-Fouché M (2005) A role for PKCzeta in the LPS-induced translocation NF-kappaB p65 subunit in cultured myometrial cells. Biochimie 87:513–521. doi:10.1016/j.biochi.2005.02.009
Halliwell B (2007) Biochemistry of oxidative stress. Biochem Soc Trans 35:1147–1150. doi:10.1042/BST0351147
Oliveira PJ, Rolo AP, Palmeira CM, Moreno AJ (2001) Carvedilol reduces mitochondrial damage induced by hypoxanthine/xanthine oxidase: relevance to hypoxia/reoxygenation injury. Cardiovasc Toxicol 1:205–213
Bavaresco CS, Chiarani F, Wannmacher CMD, Netto CA, De Wyse ATS (2007) Intrastriatal hypoxanthine reduces Na+, K+-ATPase activity and induces oxidative stress in the rats. Metab Brain Dis 22:1–11. doi:10.1007/s11011-006-9037-y
Bavaresco CS, Zugno AI, Tagliari B, Wannmacher CMD, Wajner M, Wyse ATS (2004) Inhibition of Na+, K+-ATPase activity in rat striatum by the metabolites accumulated in Lesch-Nyhan disease. Int J Dev Neurosci 22:11–17. doi:10.1016/j.ijdevneu.2003.11.002
Engin E, Treit D (2007) The role of hippocampus in anxiety: intracerebral infusion studies. Behav Pharmacol 18:365–374. doi:10.1097/FBP.0b013e3282de7929
Zugno AI, Scherer EBS, Mattos C, Ribeiro CAJ, Wannmacher CMD, Wajner M, Wyse ATS (2007) Evidence that the inhibitory effects of guanidinoacetate on the activities of the respiratory chain, Na+, K+-ATPase and creatine kinase can be differentially prevented by taurine and vitamins E and C administration in rat striatum in vivo. Biochim Biophys Acta 1772:563–569. doi:10.1016/j.bbadis.2007.02.005
Tsenov G, Mátéffyová A, Mares P, Otáhal J, Kubová H (2007) Intrahippocampal injection of endothelin-1: a new model of ischemia-induced seizures in immature rats. Epilepsia 48(Suppl 5):7–13. doi:10.1111/j.1528-1167.2007.01282.x
Paxinos G, Watson C (2006) The rat brain in stereotaxic coordinates, sixth edition. Acad Press 170:547–612. doi:10.1016/0143-4179(83)90049-5
Ozden S, Isenmann S (2004) Neuroprotective properties of different anesthetics on axotomized rat retinal ganglion cells in vivo. J Neurotrauma 21:73–82. doi:10.1089/089771504772695968
Puig JG, Jimenez ML, Mateos FA, Fox IH (1989) Adenine nucleotide turnover in hypoxanthine-guanine phosphoribosyl-transferase deficiency: evidence for an increased contribution of purine biosynthesis de novo. Metabolism 38:410–418
Scherer EBS, Loureiro SO, Vuaden FC, da Cunha AA, Schmitz F, Kolling J, Savio LEB, Bogo MR et al (2014) Mild hyperhomocysteinemia increases brain acetylcholinesterase and proinflammatory cytokine levels in different tissues. Mol Neurobiol 50:589–596. doi:10.1007/s12035-014-8660-6
Da Cunha MJ, da Cunha AA, Loureiro SO, Machado FR, Schmitz F, Kolling J, Marques EP, Wyse ATS (2015) Experimental lung injury promotes changes in oxidative/nitrative status and inflammatory markers in cerebral cortex of rats. Mol Neurobiol 52:1590–1600. doi:10.1007/s12035-014-8961-9
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem 126:131–138
Da Cunha AA, Ferreira AGK, Loureiro SO, da Cunha MJ, Schmitz F, Netto CA, Wyse ATS (2012) Chronic hyperhomocysteinemia increases inflammatory markers in hippocampus and serum of rats. Neurochem Res 37:1660–1669. doi:10.1007/s11064-012-0769-2
Schmitz F, Pierozan P, Rodrigues AF, Biasibetti H, Coelho DM, Mussulini BH, Pereira MSL, Parisi MM, Barbé-Tuana F, de Oliveira DL, Vargas CR, Wyse ATS (2015) Chronic treatment with a clinically relevant dose of methylphenidate increases glutamate levels in cerebrospinal fluid and impairs glutamatergic homeostasis in prefrontal cortex of juvenile rats. Mol Neurobiol. doi: 10.1007/s12035-015-9219-x
LeBel CP, Ali SF, McKee M, Bondy SC (1990) Organometal-induced increases in oxygen reactive species: The potential of 2′,7′-dichlorofluorescin diacetate as an index of neurotoxic damage. Toxicol Appl Pharmacol 104:17–24. doi:10.1016/0041-008X(90)90278-3
Marklund S, Marklund G (1974) Involvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutase. Eur J Biochem 47:469–474. doi:10.1111/j.1432-1033.1974.tb03714.x
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126. doi:10.1016/S0076-6879(84)05016-3
Wendel A (1981) Glutathione peroxidase. Methods Enzymol 77:325–533. doi:10.1016/S0076-6879(81)77046-0
Singh NP, McCoy MT, Tice RR, Schneider EL (1988) A simple technique for quantitation of low levels of DNA damage in individual cells. Exp Cell Res 175:184–191. doi:10.1016/0014-4827(88)90265-0
Tice RR, Agurell E, Anderson D, Burlinson B, Hartmann A, Kobayashi H, Miyamae Y, Rojas E et al (2000) Single cell gel/comet assay: guidelines for in vitro and in vivo genetic toxicology testing. Environ Mol Mutagen 35:206–221
Hartmann A, Agurell E, Beevers C, Brendler-Schwaab S, Burlinson B, Clay P, Collins A, Smith A et al (2003) Recommendations for conducting the in vivo alkaline comet assay. 4th International Comet Assay Workshop. Mutagenesis 18:45–51
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Li Q, Verma IM (2002) NF-kappaB regulation in the immune system. Nat Rev Immunol 2:725–734. doi:10.1038/nri910
Morris KR, Lutz RD, Choi H-S, Kamitani T, Chmura K, Chan ED (2003) Role of the NF-kappaB signaling pathway and kappaB cis-regulatory elements on the IRF-1 and iNOS promoter regions in mycobacterial lipoarabinomannan induction of nitric oxide. Infect Immun 71:1442–1452
Guo G, Bhat NR (2006) Hypoxia/reoxygenation differentially modulates NF-kappaB activation and iNOS expression in astrocytes and microglia. Antioxid Redox Signal 8:911–918. doi:10.1089/ars.2006.8.911
Bavaresco CS, Chiarani F, Kolling J, Netto CA, de Souza Wyse AT (2008) Biochemical effects of pretreatment with vitamins E and C in rats submitted to intrastriatal hypoxanthine administration. Neurochem Int 52:1276–1283. doi:10.1016/j.neuint.2008.01.008
Torres RJ, Puig JG (2015) Hypoxanthine deregulates genes involved in early neuronal development. Implications in Lesch-Nyhan disease pathogenesis. J Inherit Metab Dis. doi: 10.1007/s10545-015-9854-4
Lucas S-M, Rothwell NJ, Gibson RM (2006) The role of inflammation in CNS injury and disease. Br J Pharmacol 147(Suppl):S232–S240. doi:10.1038/sj.bjp.0706400
Beal MF (1995) Aging, energy, and oxidative stress in neurodegenerative diseases. Ann Neurol 38:357–366. doi:10.1002/ana.410380304
Tak PP, Firestein GS (2001) NF-kappaB: a key role in inflammatory diseases. J Clin Invest 107:7–11. doi:10.1172/JCI11830
Libermann TA, Baltimore D (1990) Activation of interleukin-6 gene expression through the NF-kappa B transcription factor. Mol Cell Biol 10:2327–2334
Shimizu Y, van Seventer GA, Horgan KJ, Shaw S (1990) Costimulation of proliferative responses of resting CD4+ T cells by the interaction of VLA-4 and VLA-5 with fibronectin or VLA-6 with laminin. J Immunol 145:59–67
Son Y-H, Jeong Y-T, Lee K-A, Choi K-H, Kim S-M, Rhim B-Y, Kim K (2008) Roles of MAPK and NF-kappaB in interleukin-6 induction by lipopolysaccharide in vascular smooth muscle cells. J Cardiovasc Pharmacol 51:71–77. doi:10.1097/FJC.0b013e31815bd23d
Shakhov AN, Kuprash DV, Azizov MM, Jongeneel CV, Nedospasov SA (1990) Structural analysis of the rabbit TNF locus, containing the genes encoding TNF-beta (lymphotoxin) and TNF-alpha (tumor necrosis factor). Gene 95:215–221
Shakhov AN, Collart MA, Vassalli P, Nedospasov SA, Jongeneel CV (1990) Kappa B-type enhancers are involved in lipopolysaccharide-mediated transcriptional activation of the tumor necrosis factor alpha gene in primary macrophages. J Exp Med 171:35–47
Hughes JE, Srinivasan S, Lynch KR, Proia RL, Ferdek P, Hedrick CC (2008) Sphingosine-1-phosphate induces an antiinflammatory phenotype in macrophages. Circ Res 102:950–958. doi:10.1161/CIRCRESAHA.107.170779
Gudbjörnsson B, Zak A, Niklasson F, Hällgren R (1991) Hypoxanthine, xanthine, and urate in synovial fluid from patients with inflammatory arthritides. Ann Rheum Dis 50:669–672
Knowles RG, Moncada S (1994) Nitric oxide synthases in mammals. Biochem J 298(Pt 2):249–258
Lechner M, Lirk P, Rieder J (2005) Inducible nitric oxide synthase (iNOS) in tumor biology: the two sides of the same coin. Semin Cancer Biol 15:277–289. doi:10.1016/j.semcancer.2005.04.004
Moncada S (1993) The L-arginine: nitric oxide pathway, cellular transduction and immunological roles. Adv Second Messenger Phosphoprotein Res 28:97–99
Brown GC, Neher JJ (2010) Inflammatory neurodegeneration and mechanisms of microglial killing of neurons. Mol Neurobiol 41:242–247. doi:10.1007/s12035-010-8105-9
Borutaite V, Budriunaite A, Brown GC (2000) Reversal of nitric oxide-, peroxynitrite- and S-nitrosothiol-induced inhibition of mitochondrial respiration or complex I activity by light and thiols. Biochim Biophys Acta 1459:405–412
Ribeiro BMM, do Carmo MRS, Freire RS, Rocha NFM, Borella VCM, de Menezes AT, Monte AS, Gomes PXL et al (2013) Evidences for a progressive microglial activation and increase in iNOS expression in rats submitted to a neurodevelopmental model of schizophrenia: reversal by clozapine. Schizophr Res 151:12–19. doi:10.1016/j.schres.2013.10.040
Xu L, He D, Bai Y (2015) Microglia-mediated inflammation and neurodegenerative disease. Mol Neurobiol. doi: 10.1007/s12035-015-9593-4
Magni P, Ruscica M, Dozio E, Rizzi E, Beretta G, Maffei Facino R (2012) Parthenolide inhibits the LPS-induced secretion of IL-6 and TNF-α and NF-κB nuclear translocation in BV-2 microglia. Phytother Res 26:1405–1409. doi:10.1002/ptr.3732
Takeuchi H, Jin S, Wang J, Zhang G, Kawanokuchi J, Kuno R, Sonobe Y, Mizuno T et al (2006) Tumor necrosis factor-alpha induces neurotoxicity via glutamate release from hemichannels of activated microglia in an autocrine manner. J Biol Chem 281:21362–21368. doi:10.1074/jbc.M600504200
Guizzetti M, Zhang X, Goeke C, Gavin DP (2014) Glia and neurodevelopment: focus on fetal alcohol spectrum disorders. Front Pediatr 2:123–135. doi:10.3389/fped.2014.00123
Sofroniew MV (2009) Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci 32:638–647. doi:10.1016/j.tins.2009.08.002
Pekny M, Nilsson M (2005) Astrocyte activation and reactive gliosis. Glia 50:427–434. doi:10.1002/glia.20207
Li N, Karin M (1999) Is NF-{kappa}B the sensor of oxidative stress? FASEB J 13:1137–1143
Marnett LJ (2000) Oxyradicals and DNA damage. Carcinogenesis 21:361–370. doi:10.1093/carcin/21.3.361
Acknowledgments
This work was supported in part by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq-Brazil).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Biasibetti, H., Pierozan, P., Rodrigues, A.F. et al. Hypoxanthine Intrastriatal Administration Alters Neuroinflammatory Profile and Redox Status in Striatum of Infant and Young Adult Rats. Mol Neurobiol 54, 2790–2800 (2017). https://doi.org/10.1007/s12035-016-9866-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-9866-6