Abstract
Cerebral palsy (CP) is a neuromuscular disease due to injury in the infant’s brain. The CP disorder causes many neurologic dysfunctions in the patient. Various treatment methods have been used for the management of CP disorder. However, there has been no absolute cure for this condition. Furthermore, some of the procedures which are currently used for relief of symptoms in CP cause discomfort or side effects in the patient. Recently, stem cell therapy has attracted a huge interest as a new therapeutic method for treatment of CP. Several investigations in animal and human with CP have demonstrated positive potential of stem cell transplantation for the treatment of CP disorder. The ultimate goal of this therapeutic method is to harness the regenerative capacity of the stem cells causing a formation of new tissues to replace the damaged tissue. During the recent years, there have been many investigations on stem cell therapy. However, there are still many unclear issues regarding this method and high effort is needed to create a technology as a perfect treatment. This review will discuss the scientific background of stem cell therapy for cerebral palsy including evidences from current clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lesions or anomalies of the brain happening in the early stages of its development can lead to a group of heterogeneous non-progressive motor dysfunction syndromes called cerebral palsy [1]. Above 100,000 Americans less than 18 years of age are supposed to have some neurologic dysfunctions attributed to cerebral palsy [2]. Cerebral palsy can be caused by brain injury in prenatal or postnatal periods. Several birth complications such as low birth weight, uterine growth retardation, asphyxia, intracranial hemorrhage, and trauma can induce this disease [3]. In the most of cerebral palsy (CP) patients, there is a white matter injury in periventricular, subcortical, and callosal areas of the brain [4]. The different subtypes of CP include spastic, ataxic, dyskinetic, and unclassified [5]. Various methods have been used for the treatment of CP which include physical and occupational therapy [6]; using the caste and orthoses [7]; medications that aimed to decrease the effects of CP such as abnormal muscle tone, sleep disorder, and agitation and to prevent seizer [8]; surgery which includes diverse surgeries on bone, muscles, tendons, and nerves that can facilitate training and rehabilitation [9], hyperbaric oxygen that delivers oxygen at greater than atmospheric pressure; Adeli suit therapy [10]; and patterning, electrical stimulation, and conductive education [11]. However, none of the abovementioned treatments is of absolute cure for CP and some of them may cause discomfort or several side effects in the patients. Recently, stem cell therapy has attracted huge interest as a new treatment for CP. Many clinical trials on patients with CP who use this method of treatment have shown great efficacy. It seems that cell therapy will create a revolution in the management of CP and the conventional therapeutic methods may be substituted by this novice strategy.
Stem Cell
Stem cells are cells with the ability to differentiate into few (like multipotent adult stem cells) or any (like pluripotent embryonic stem cells) cell types while able to self-renew to produce more stem cells [12, 13]. Wilson in the nineteenth century introduced the term “stem cell” as a synonym for a mitotically quiescent primordial germ cell [14]. The stem cells (SCs) are characterized by self-renewability that is the capability to both multiply them and make new SCs more differentiated than the mother cells. SCs are classified according to the developmental step of the animal from which a stem cell is separated from. In this classification, stem cell is defined as embryonic stem cells (ESCs) and adult stem cells (ASCs) including mesenchymal stem cells, hemopoietic stem cells, and neural stem cells [15]. Regarding to differentiating ability, SCs are characterized as totipotent, pluripotent cells such as ESCs, and multipotent cells such as ASCs, which are able to create more classified types of cell lineages [13]. Scientific investigators have been working to find and recognize the molecular and cellular pathways that involve SCs. Deep understanding of the pathophysiological mechanisms related to SCs will be the only way to obtain them in a laboratory and use the achieved results in the treatment of neurological disorders like CP [16].
Cell-Based Therapy in Neurological Diseases
Cell-based therapy and gene transfer to the diseased brain have been provided to explore the possibility of developing new powerful therapeutic methods for a spectrum of human neurological disorders. Indeed, the lack of appropriate cell types for cell therapy in patients with the neurological disorders has caused the development of this therapeutic procedure [17]. The main sources of stem cells for neurotherapy include ESCs, stem cells from the fetal or adult central nervous system, or other tissues such as bone marrow and cord blood (Fig. 1) [18–20]. The clinical effect significance of stem cells occurs through neural replacement, remyelination, and neuroprotection.
Sources of stem cells in neurological disease [19]
Cellular Signaling Pathways for Brain Growth and Repair
The stem cell niches in the CNS are placed in distinct anatomic regions. They have been found in the dentate gyrus of the hippocampus and in the subventricular zone along the lateral ventricles. The neural stem cells present in CNS niches are able to proliferate along neuronal or glial lineages [21]. The stem cell-based natural repair happens through the stages of multiplication, differentiation, migration, and neosynaptogenesis [22, 23]. The cell proliferation is induced by growth factors such as FGF-2 (fibroblast growth factor-2) and EGF-1 (epidermal growth factor-1) [24–26]. Signaling has a vital role in the renovation of embryonic and adult stem cells. In the developing neocortex [27], sonic hedgehog (Shh) helps to neural progenitor cell proliferation. During neurogenesis, radial glial cells of the ventricular zone (VZ) are the main neocortical progenitors that produce neurons through both symmetric and asymmetric divisions. Shh and Notch signaling can cooperate to regulate neurogenic part of neocortical progenitors [28]. Differentiation along neuronal lines happens under the effect of the Shh, while the notch pathway stimulates proliferation towards a glial lineage. The Shh is a secreted glycoprotein which increases the proliferation of neural progenitors [29, 30]. The Notch is a transcription factor that makes active CBF1. The Notch which is often expressed in proliferating regions of the developing CNS plays an important role in this process. In fact, in vivo activation of the Notch improves radial glial morphology at E12.5/E14.5, while constitutive activation is associated with an extra formation of oligodendrocyte progenitor cells (OPCs). In addition, other studies have demonstrated that postnatal Notch-expressing progenitors develop to disperse astrocytes and periventricular cells. Therefore, stem cell differentiation depends on the interactions between different signaling pathways, some which induce specific lineage production and some which stop [31–33].
Stem Cell Therapy as a Novice Procedure for the Treatment of CP
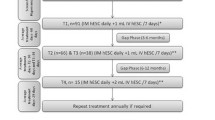
Unsatisfactory results in conventional methods for the treatment of CP have compelled the scientists to seek for the new therapeutic procedures. One of these novice procedures is the stem cell therapy. Several studies in animal models have already shown potential benefits of stem cell transplantation for the treatment of CP [34]. Recently, several practitioners have been trying to treat CP patients with stem cells and a spectrum of positive results has been demonstrated in their clinical trials [35–38]. During the last years, the diverse types of stem cells derived from different origins, with special dosage, have been used in various clinical trials. Several techniques of cell delivery have been tested in the patients with different complications and etiologies of cerebral palsy. A group of scientists believes that patients who are in acute phase of some kinds of CP like hypoxic-ischemic brain injuries are better candidates for cell therapy because of the presence of the chemotactic signals and vascular permeability. The problem in this phase is lack of time for doing appropriate processes on cells before culture [39]. Furthermore, some researchers consider the age as an important factor in success of cell therapy for CP. They suppose trials in younger ages will lead to better results [40]. The investigation about mentioned parameters may be useful for clarifying different aspects of stem cell therapies for the treatment of the cerebral palsy. Several studies in animal models have already shown potential benefits of stem cell transplantation for the treatment of CP [34, 37]. Recently, several practitioners have been trying to treat CP patients with stem cells and a spectrum of positive results has been found in their clinical trials [35–38]. Currently, scientists at the Duke University have started a phase I study with autologous umbilical cord blood transplantation in full-term newborns with moderate-to-severe CP derived from hypoxic-ischemic encephalopathy. The newborns have been followed for evaluation of neurodevelopmental outcomes and have been also observed with magnetic resonance imaging [39]. During the last years, the diverse types of stem cells derived from different origins, with special dosage, have been used in various clinical trials. Several techniques of cell delivery have been tested in the patients with different complications and etiologies of cerebral palsy. A group of scientists believes that the patients who are in acute phase of some kinds of CP like hypoxic-ischemic brain injury are better candidates for cell therapy because of the presence of the chemotactic signals and vascular permeability. The problem in this phase is the lack of time for doing appropriate processes on cells before culturing them [39]. Furthermore, some researchers consider the age as an important factor in success of cell therapy for CP. They suppose that the trials in younger ages will lead to good results [40]. The investigation of the abovementioned parameters may be useful for clarifying different aspects of stem cell therapies for the treatment of the cerebral palsy.
Different Mechanisms by Which Stem Cells May Help for the Repair of the Brain in CP
Cell transdifferentiation is differentiation of stem cells into mature neurons. Indeed, the first hypothesis, concerning the mechanism of stem cell therapy in CP, was the direct transformation of stem cells into mature neurons. However, investigations on animals with CP showed that the functional recovery in animals with CP can also happen without the presence of cells with neural labeling in the damaged area of the brain [41, 42]. Furthermore, the transdifferentiation of ASCs with mesodermal origin into cells which are derived from ectodermal layer is still under investigation. In addition, in vitro studies showed that the transdifferentiation of stem cells into neural cells is detected by the presence of special markers of neurons and glial cell [43]. However, the electrophysiological features of these transdifferentiated cells are not well documented yet. Due to these matters, other mechanisms for the repair of brain in CP patients have been suggested [41, 44, 45].
Release of Trophic Factors
The stem cells may play an important role in generation or release of neurotrophic factors [46]. The studies on animal models with CP showed that there was an increase of 15 % in generation of trophic factors after transplantation of umbilical cord blood stem cells (UCBSCs) to the animal. The scientists believe that in a hypoxic-ischemic brain, although the release of trophic factor happens naturally but the transplantation of stem cells can increase its generation [41].
Induction of Endogenous Neurogenesis
The investigations on animals with CP revealed that the transplantation of stem cells to animal causes a decrease in the production of microglial and an increase in the neurogenesis. The scientists believed that transplanted stem cells modulate the inflammatory cascade of the brain after injury and enhance the production of neurons [47].
Modulation of the Inflammatory Process
The stem cells can stop the activity of immune cells in the patient with CP. Recent studies on animals with CP have demonstrated that various sources of stem cells can stop the activation of various immune cells. For instance, neural stem cells (NSCs) in a CP animal model decreased inflammatory cytokines and improved neuroprotection [20]. Furthermore, intravenous injection of HUCBSC enhanced the neuron survival and decreased the infiltration of white blood cells and the secretion proinflammatory proteins in the damaged brain in the model with CP [20, 41].
Stimulation of Angiogenesis
The new blood vessels can be produced through the transdifferentiation of the stem cells into the blood vessels and also by release of trophic factors [48]. Some studies on the adult rats with CP have demonstrated the enhancement of the blood vessels in the penumbra just a few days after delivery of stem cells. In addition, transdifferentiation of the grafted stem cells into blood vessels has been detected. Other evidences from CP animal models have shown that the stem cells derived from the bone marrow stroma can improve the angiogenesis in the ischemic area by enhancing the endogenous levels of vascular endothelial growth factor [49]. Evidences from transplantation of NSCs to a rat with hypoxic-ischemic brain injury showed that angiogenic signals were produced to induce the generation of a neovascularized parenchyma at the region of the porencephalic cyst [41].
The endometrial stem cell is one of the stem cells which its angiogenic potential has been approved in several studies. The 3-dimensional (3D) culture gives the possibility of quantification of cell proliferation and angiogenesis from endometrial stromal cells. The culture of human endometrial stem cells in the fibrin matrix leads to the proliferation of endometrial stromal stem cells and angiogenesis [50–54]. Also, another research has been shown that human endometrial stem cells are a new source for neural cells [55–60]. These documents show that human endometrium has a number of candidate stem/progenitor cell for the treatment of CP.
Stimulating of Neuroplasticity
The enhancing of the efferent and afferent connections between the brain and zones of the injury causes an increase in the local synaptic activity [41]. The expression of synaptic proteins have been recently detected in adult rats with CP passing stem cell transplantation, indicating the generation of synaptic contacts. Confirming this possibility, a recent investigation indicated that intracerebral delivery of NSC in CP rats enhanced the number of axon terminals in the sensorimotor cortex, corpus callosum, and ipsilateral striatum/thalamus and also increased the development of axons in the injured hemisphere [41, 61].
Sources of Stem Cells Which Have Been Used to Achieve Their Role in the Treatment of CP
Umbilical Cord Blood
Investigations indicated that umbilical cord blood (UCB) contains many types of stem cells which may be helpful in the treatment of CP such as hematopoietic stem cells [44], embryonic-like stem cells, endothelial stem cells, epithelial stem cells, and mesenchymal stem cells [62]. The UCB studies demonstrated that the transplanted UCB stem cells can move to the injured regions in the traumatic brain of the CP rat. The reason of homing of the UCB stem cells into the brain lesion may be specific chemo-attractants being discharged and unregulated on the injured area, and the impaired bloodbrain barrier in the damaged brain helps in the penetration of donor cells to the central nervous system [63]. The benefits of using cord blood stem cells for CP include the availability, high tolerance to HLA mismatch, and reduced graft versus host disease [64].
Bone Marrow
Several studies have used the bone marrow as a source for hemopoietic and mesenchymal stem cells for the treatment of CP [39, 65]. The use of bone marrow (BM)-derived cells is not always satisfactory because of the high risk of viral exposure, the significant reduction in the cell population, and the proliferative/differentiation capacity along with age. In addition, it needs a painful invasive procedure to achieve a BM sample [39].
Brain
The subventricular zone of the lateral ventricles and the subgranular region of the hippocampal dentate gyrus have the NSCs and the astrocyte stem cells. The embryonic nervous system of animal models has been used as this source [66]. The disadvantage of this method is small population of donor cells [67].
Embryo
The inner cell mass of blastocyst-stage embryos also has been used in investigations as a source in stem cell therapy for CP because of having cells that possess the capability to develop into neurons [41].
Types of Stem Cells Which Have Been Used for the Treatment of CP
Hematopoietic Stem Cells
This type of stem cell has been used in the various clinical trials for the treatment of CP [68]. The mononuclear stem cells are hematopoietic cells which have the ability of self-renewal, differentiation, and migration. They are abundantly placed in the bone marrow and defined as CD 34+ cells. They are hypothesized to act in neurogenesis and angiogenesis. In the human clinical trials on the CP patients, there has been an acceptable reduction of disability scale after the delivery of bone marrow-derived hematopoietic stem cell into the carotid artery of the CP patients [69]. The researchers hypothesized that the improvement in the treated patients was due to increased angiogenesis or to internal milieu, which is helpful for starting the reparative process. However, they had no method to prove this opinion since there was no mean available to observe the stem cells homing capability or survival or integration into the host cytoarchitecture. Several studies have already indicated the benefit of the mononuclear stem cell transplantation in animal models and clinical trials with CP. These findings showed that the mononuclear stem cells have the ability of neurogenesis and angiogenesis by modulating the host environment [70].
Mesenchymal Stem Cells
The mesenchymal stem cells can be isolated from the bone marrow or cord blood [71]. The mesenchymal stem cells are great candidates for cell transplantation because they can be easily accessible; the isolation is uncomplicated and the cells can increase to clinical scales in a relatively short period of time. They can also be maintained with minimal loss of potency. Furthermore, the human clinical trials of the mesenchymal stem cells (MSCs) have demonstrated no adverse reactions to allogeneic MSC grafts and they also have wide-ranging differentiation capacity. Moreover, this cell type has an increased capacity to express neuronal phenotypes in vitro and in vivo [72]. Some studies showed that the MSC can increase the endogenous generation of new neuronal cells through inhibition of microglial inflammatory activity. The therapeutic possibility of mesenchymal stem cells has been recently investigated in an experimental model of the CP animals. It showed a promotion of neurological function with the decrease of brain tissue injury after delivery of the stem cells. The researchers found delivered cells in the cortex and the hippocampus, 7 days after cell delivery demonstrating the astrocytic differentiation, without neuronal development [41]. Different human trials have shown positive results in the use of mesenchymal stem cells for the management of CP [41, 73].
Neural Stem Cell
The NSCs have the ability of self-renewal and limited capacity to produce cells of neuronal and glial lineages [21, 74]. Evidences achieved from a case study on a CP mouse showed that multipotent astrocytic stem cells from the subventricular zone of mice moved to the cortical and the periventricular ischemic region and indicated signs of neuronal and astrocytic differentiation in CP animals passed intracerebral transplantation. In comparison, when transplantation was done in healthy animals, the cells remained in the region of transplantation and kept their astrocytic profile. The investigations have shown that the NSC can move and survive in injured brain regions and can be stimulated to differentiate in vivo and in vitro into neurons, oligodendrocytes, and astrocytes [75]. Researches on the animal models with CP showed that when the NSCs grafted into the contra lateral hemisphere of the hypoxic brain injury, the NSC moved across the corpus callosum and other interhemispheric commissures to the infarcted region. However, when grafted into the ipsilateral hemisphere, the cells stayed at the site of injury. In both examinations, the NSCs developed in the ischemic zone, expressing markers for neurons, oligodendrocytes, astrocytes, and neural progenitor cells [76]. Furthermore, the same research group showed the inflammatory mechanisms related to the movement of the NSC in response to brain hypoxic-ischemic injury [77].
Embryonic Stem Cells
These cells have the capacity to differentiate into neurons by specific culture methods [78]. In a study on a rat with CP, transplantation of ESCs which had been differentiated into neurons in vitro led to promoted spatial memory in cerebral palsy rat. But, although the number of neuronal cells was enhanced in the ischemic hippocampus, there was no obvious correlation between the outcomes and neuronal repopulation, differentiation, or release of trophic factors by the transplanted cells. The evidences of the investigations also indicated that symmetry can happen after delivery of human ESCs in CP rat. However, the researcher found no change on the structural brain damage [79].
Methods of Cell Delivery Which Can Be Used for the CP Patients
Various methods of cell delivery have been used for cell therapy in CP patients: (1) intravenous method which is safe and non-invasive but has the risk of cell migration to the other organs, (2) intra-arterial method with the advantages of the better targeting of the injured regions possible but has the danger of embolism and ischemia [80], (3) intracranial method which makes the migration of transplanted cells easier but it is very invasive [65], (4) intraperitoneal [81], and (5) subcutaneous methods which are both easy and none invasive but cells have to migrate a long distance in these techniques [64].
The Effectiveness of the Stem Cell Therapy on CP Complications
Stem cell therapy has been effective for different complications of CP such as muscle tone, abnormal movements, speech, cognition, balance, and gross motor function [82]. The improvement mechanism is the repair of the brain injury areas, which are responsible for the promoted tasks. This repair may happen due to differentiation of transplanted stem cells into neural cells or secondary to induction of neurogenesis or angiogenesis. This results in an increase of blood flow to the damaged regions [83–86].
Reverse Reactions Which May Happen in Stem Cell Therapy
There have been no major immediate or delayed adverse reactions in the patients who have passed various procedures of cell therapy with different kinds of cells. In no patient’s laboratory and clinical findings of tissue-destructive autoimmune reactions were detected [63, 83].
Supplementary Approaches Which Can Facilitate Cell Therapy in CP
The stem cells can be mobilized by processes in which endogenous stem and progenitor cells are moved. Delivering cytokines such as granulocyte colony stimulatory factor (GCSF) or chemokines such as SDF-1, trophic and growth factor like brain-derived neurotrophic factor (BDNF) or glial-derived neurotrophic factor (GDNF) into the brain can help to this purpose [87, 88]. These approaches may be used together to enhance recovery [89]. Some cases of CP, like hypoxic-ischemic brain injuries, may associate with massive tissue necrosis, yielding to a porencephalic cyst. Such condition provides an impaired microenvironment for homing of transplanted cells because of lack of blood supply and enough extracellular matrixes. In some situations, the utilization of biodegradable scaffolds in the necrotic cavity will be useful in order to ease the creation of connections between graft and host tissue [41, 90, 91].
Summary
In this article, the stem cells which are unspecialized cells with the ability to differentiate into other cells [13, 15] were discussed and their role in the treatment of cerebral palsy was investigated [44, 92]. Furthermore, other treatments which are used for CP were mentioned. It is obvious that although several procedures have been used for the treatment of CP, but none of them have had satisfactory results [93]. The stem cell therapy as a new therapeutic method for the treatment of CP can solve a lot of problems in this way. According to recent investigations, various types of stem cells can act in the process of brain repair through different mechanisms. For instance, the NSCs have the ability of self-renewal and modulation of inflammatory process while hematopoietic and endometrial stem cells have the ability of angiogenesis or neurogenesis. The MSCs can modulate the activity of immune cells or act through cell differentiation [20, 41, 47, 94].
Traditional treatments such as using the braces are too difficult for the patient to be tolerated [7]. Drug therapy will just reduce the symptoms and will not be an absolute cure for the disease. Some of the new procedures such as the electrical stimulation have not shown positive results [11], and some others like hyperbaric oxygen delivery which has been somewhat effective may result in dangerous complications such as pneumothorax [95]. The stem cell therapy as a new therapeutic method for the treatment of CP can solve a lot of problems in this way. According to recent investigations, various types of stem cells can act in the process of brain repair through different mechanisms. For instance, the NSCs have the ability of self-renewal and modulation of inflammatory process while hematopoietic and endometrial stem cells have the ability for angiogenesis or neurogenesis. The MSCs can modulate the activity of immune cells or act through cell transdifferentiation [96, 97].
The clinical trials have shown that the stem cell therapy can have influences on any complications of CP like loss of motor control, speech control, abnormal muscle tone, and cognitive problems without causing considerable reverse immediate or delayed reactions [44]. In previous studies, various types of stem cells from diverse origins and through different techniques have been transplanted in CP patients. The results indicated that each of the subtypes of the mentioned parameters has its own advantages and disadvantages for cell therapy. Regarding the source of stem cells, UCBSCs showed good results for achieving treatment of CP because of availability, high tolerance to HLA mismatch between donor and recipient, and reduction of graft versus host disease [64]. The using of BM-derived cells is not always satisfactory because of invasiveness and high risk of viral exposure and the significant reduction in the cell population and the proliferative/differentiation capacity along with age [94]. Using the brain as a source provided a limited number of cells for immunological matches [18]. Regarding the type of stem cells, the mesenchymal stem cells are great candidates for cell transplantation because they can be easily accessible; the isolation is uncomplicated and the cells can increase to clinical scales in a relatively short period of time. They can also be maintained with minimal loss of potency [39]. Regarding the NSCs, they have been very helpful in animal models and preclinical trials for the treatment of CP [98], but accessibility of very small population of them makes immunological matches difficult for cell therapy [18]. The hematopoietic stem cells are also good choices for brain repair because of their ability for induction of angiogenesis and neurogenesis [99], but aspirating the bone marrow of the patient for achieving these cells is painful and increases the risk of infection [100, 101]. Concerning the ESCs, although neurological functions and the population of neurons in the injured zone have enhanced after cell delivery in animal models but no changes in the structural brain injury have been detected. Regarding the method of cell delivery, recent studies demonstrate that intravenous injection of the stem cells is a safe method but it has the risk of migration of cells to other organs [102, 103]. Intracranial cell delivery is an invasive method but the migration of the stem cells is easier in this procedure. Intra-arterial injection of stem cells allowed better targeting the injured organ but there was the risk of embolism and ischemia. Intraperitoneal and subcutaneous injections of the stem cells are easy and safe methods but the stem cells have to migrate a long distance. According to the evidences from previous trials, using appropriate cytokines or chemokines and growth factors with the stem cell transplantation will play the role of supplementary therapy and maximize the effects of stem cell therapy [44, 104, 105]. The results of investigations indicated that some factors like the age of the patients and the time interval between the establishment of injury and cell delivery in CP patients influenced the results of cell therapy [40] Cell transplantation in young ages has good results [64]. Concerning the transplantation time, regardless of the lacking time for doing appropriate process before cell culture, transplantation in acute phase has good results because of the presence of chemotactic signals.
In conclusion, further investigation is needed to answer several questions about this novice treatment and establish it as a perfect procedure for management of CP. The emphasis of this review is that the stem cell therapy can be considered as a substitution for current therapeutic methods of CP which have just limited effects on this disease and some of them may result in dangerous reverse reactions.
Reference
Smithers-Sheedy H, Badawi N, Blair E, Cans C, Himmelmann K, Krageloh-Mann I, McIntyre S, Slee J, Uldall P, Watson L, Wilson M (2014) What constitutes cerebral palsy in the twenty-first century? Dev Med Child Neurol 56(4):323–328. doi:10.1111/dmcn.12262
Katz RT (2003) Life expectancy for children with cerebral palsy and mental retardation: implications for life care planning. NeuroRehabilitation 18(3):261–270
Krigger KW (2006) Cerebral palsy: an overview. Am Fam Physician 73(1):91–100
Share JB (1976) Review of drug treatment for Down’s syndrome persons. Am J Ment Defic 80(4):388–393
Pakula AT, Van Naarden BK, Yeargin-Allsopp M (2009) Cerebral palsy: classification and epidemiology. Phys Med Rehabil Clin N Am 20(3):425–452. doi:10.1016/j.pmr.2009.06.001
Verschuren O, Ketelaar M, Gorter JW, Helders PJ, Uiterwaal CS, Takken T (2007) Exercise training program in children and adolescents with cerebral palsy: a randomized controlled trial. Arch Pediatr Adolesc Med 161(11):1075–1081. doi:10.1001/archpedi.161.11.1075
Autti-Ramo I, Suoranta J, Anttila H, Malmivaara A, Makela M (2006) Effectiveness of upper and lower limb casting and orthoses in children with cerebral palsy: an overview of review articles. Am J Phys Med Rehabil 85(1):89–103
Garvey MA, Giannetti ML, Alter KE, Lum PS (2007) Cerebral palsy: new approaches to therapy. Curr Neurol Neurosci Rep 7(2):147–155
Bose K, Yeo KQ (1975) The role of surgery in cerebral palsy. Singap Med J 16(4):249–255
Anttila H, Suoranta J, Malmivaara A, Makela M, Autti-Ramo I (2008) Effectiveness of physiotherapy and conductive education interventions in children with cerebral palsy: a focused review. Am J Phys Med Rehabil 87(6):478–501. doi:10.1097/PHM.0b013e318174ebed
Liptak GS (2005) Complementary and alternative therapies for cerebral palsy. Ment Retard Dev Disabil Res Rev 11(2):156–163. doi:10.1002/mrdd.20066
Xu XL, Yi F, Pan HZ, Duan SL, Ding ZC, Yuan GH, Qu J, Zhang HC, Liu GH (2013) Progress and prospects in stem cell therapy. Acta pharmacol Sinica 34(6):741–746. doi:10.1038/aps.2013.77
Lodi D, Iannitti T, Palmieri B (2011) Stem cells in clinical practice: applications and warnings. J Exp Clin Cancer Res CR 30:9. doi:10.1186/1756-9966-30-9
Taylor SE, Smith RK, Clegg PD (2007) Mesenchymal stem cell therapy in equine musculoskeletal disease: scientific fact or clinical fiction? Equine Vet J 39(2):172–180
Biehl JK, Russell B (2009) Introduction to stem cell therapy. J Cardiovasc Nurs 24(2):98–103 . doi:10.1097/JCN.0b013e318197a6a5quiz 104-105
Mouhieddine TH, Kobeissy FH, Itani M, Nokkari A, Wang KK (2014) Stem cells in neuroinjury and neurodegenerative disorders: challenges and future neurotherapeutic prospects. Neural Regen Res 9(9):901–906. doi:10.4103/1673-5374.133129
Kim SU, De Vellis J (2009) Stem cell-based cell therapy in neurological diseases: a review. J Neurosci Res 87(10):2183–2200
Schwartz PH (2006) The potential of stem cell therapies for neurological diseases. Expert Rev Neurother 6(2):153–161
Lindvall O, Kokaia Z (2006) Stem cells for the treatment of neurological disorders. Nature 441(7097):1094–1096. doi:10.1038/nature04960
Karussis D, Petrou P, Kassis I (2013) Clinical experience with stem cells and other cell therapies in neurological diseases. J Neurol Sci 324(1–2):1–9. doi:10.1016/j.jns.2012.09.031
Yazdankhah M, Farioli-Vecchioli S, Tonchev AB, Stoykova A, Cecconi F (2014) The autophagy regulators Ambra1 and Beclin 1 are required for adult neurogenesis in the brain subventricular zone. Cell Death Dis 5:e1403. doi:10.1038/cddis.2014.358
Toni N, Sultan S (2011) Synapse formation on adult-born hippocampal neurons. Eur J Neurosci 33(6):1062–1068. doi:10.1111/j.1460-9568.2011.07604.x
Masoudian N, Riazi GH, Afrasiabi A, Modaresi SM, Dadras A, Rafiei S, Yazdankhah M, Lyaghi A, Jarah M, Ahmadian S, Seidkhani H (2015) Variations of glutamate concentration within synaptic cleft in the presence of electromagnetic fields: an artificial neural networks study. Neuroch Res 40(4):629–642. doi:10.1007/s11064-014-1509-6
Oyagi A, Hara H (2012) Essential roles of heparin-binding epidermal growth factor-like growth factor in the brain. CNS Neurosci Ther 18(10):803–810. doi:10.1111/j.1755-5949.2012.00371.x
Harirchian MH, Tekieh AH, Modabbernia A, Aghamollaii V, Tafakhori A, Ghaffarpour M, Sahraian MA, Naji M, Yazdankhah M (2012) Serum and CSF PDGF-AA and FGF-2 in relapsing-remitting multiple sclerosis: a case-control study. Eur J Neur 19(2):241–247. doi:10.1111/j.1468-1331.2011.03476.x
Adeeb N, Mortazavi MM (2014) The role of FGF2 in spinal cord trauma and regeneration research. Brain and behav 4(2):105–107. doi:10.1002/brb3.207
Mashayekhi F, Azari M, Moghadam LM, Yazdankhah M, Naji M, Salehi Z (2009) Changes in cerebrospinal fluid nerve growth factor levels during chick embryonic development. J Clinic Neurosci 16(10):1334–1337. doi:10.1016/j.jocn.2009.03.023
Richa E (2011) The correlation between the granulocyte content in infused stem cells and side effects of the infusion. Blood Transfus 9(3):346. doi:10.2450/2011.0103-10
Mathai KI, Shashivadhanan SS, Sahoo PK (2008) The role of stem cells in neural injury—emerging paradigms. Indian J surg 70(5):212–214. doi:10.1007/s12262-008-0061-5
Platel J-C, Stamboulian S, Nguyen I, Bordey A (2010) Neurotransmitter signaling in postnatal neurogenesis: the first leg. Brain Res Rev 63(1):60–71
Magnusson JP, Goritz C, Tatarishvili J, Dias DO, Smith EM, Lindvall O, Kokaia Z, Frisen J (2014) A latent neurogenic program in astrocytes regulated by Notch signaling in the mouse. Science (New York, NY) 346(6206):237–241. doi:10.1126/science.346.6206.237
Imayoshi I, Sakamoto M, Yamaguchi M, Mori K, Kageyama R (2010) Essential roles of Notch signaling in maintenance of neural stem cells in developing and adult brains. J Neurosci 30(9):3489–3498
Ables JL, DeCarolis NA, Johnson MA, Rivera PD, Gao Z, Cooper DC, Radtke F, Hsieh J, Eisch AJ (2010) Notch1 is required for maintenance of the reservoir of adult hippocampal stem cells. J Neurosci 30(31):10484–10492
Chen A, Siow B, Blamire AM, Lako M, Clowry GJ (2010) Transplantation of magnetically labeled mesenchymal stem cells in a model of perinatal brain injury. Stem Cell Res 5(3):255–266
Hansson L-E, Nyrén O, Hsing AW, Bergström R, Josefsson S, Chow W-H, Fraumeni JF Jr, Adami H-O (1996) The risk of stomach cancer in patients with gastric or duodenal ulcer disease. N Engl J Med 335(4):242–249
Ramirez F, Steenblock DA, Payne AG, Darnall L (2006) Umbilical cord stem cell therapy for cerebral palsy. Med Hypotheses Res 3(2):679–686
Papadopoulos KI, Low SS, Aw TC, Chantarojanasiri T (2011) Safety and feasibility of autologous umbilical cord blood transfusion in 2 toddlers with cerebral palsy and the role of low dose granulocyte-colony stimulating factor injections. Restor Neurol Neurosci 29(1):17–22. doi:10.3233/rnn-2011-0572
Carroll JE, Mays RW (2011) Update on stem cell therapy for cerebral palsy. Expert Opin Biol Ther 11(4):463–471. doi:10.1517/14712598.2011.557060
Malgieri A, Kantzari E, Patrizi MP, Gambardella S (2010) Bone marrow and umbilical cord blood human mesenchymal stem cells: state of the art. Int J Clin Exp Med 3(4):248–269
Harris DT (2009) Non-haematological uses of cord blood stem cells. Br J Haematol 147(2):177–184. doi:10.1111/j.1365-2141.2009.07767.x
Paula S, Greggio S, DaCosta JC (2010) Use of stem cells in perinatal asphyxia: from bench to bedside. J pedi 86(6):451–464. doi:10.2223/JPED.2035
Mancias-Guerra C, Marroquin-Escamilla AR, Gonzalez-Llano O, Villarreal-Martinez L, Jaime-Perez JC, Garcia-Rodriguez F, Valdes-Burnes SL, Rodriguez-Romo LN, Barrera-Morales DC, Sanchez-Hernandez JJ, Cantu-Rodriguez OG, Gutierrez-Aguirre CH, Gomez-De Leon A, Elizondo-Riojas G, Salazar-Riojas R, Gomez-Almaguer D (2014) Safety and tolerability of intrathecal delivery of autologous bone marrow nucleated cells in children with cerebral palsy: an open-label phase I trial. Cytotherapy 16(6):810–820. doi:10.1016/j.jcyt.2014.01.008
Faghihi F, Mirzaei E, Ai J, Lotfi A, Sayahpour FA, Ebrahimi-Barough S, Joghataei MT (2016) Differentiation potential of human chorion-derived mesenchymal stem cells into motor neuron-like cells in two- and three-dimensional culture systems. Mol Neurobiol 53(3):1873. doi:10.1007/s12035-015-9172-8
Fan HC, Ho LI, Chi CS, Cheng SN, Juan CJ, Chiang KL, Lin SZ, Harn HJ (2015) Current proceedings of cerebral palsy. Cell transpl 24(3):471–485. doi:10.3727/096368915x68693119
Feng M, Lu A, Gao H, Qian C, Zhang J, Lin T, Zhao Y (2015) Safety of allogeneic umbilical cord blood stem cells therapy in patients with severe cerebral palsy: a retrospective study. Stem Cells Int 325652. doi:10.1155/2015/325652
Ghosh B, Zhang C, Smith GM (2014) Bridging between transplantation therapy and neurotrophic factors in Parkinson's disease. Front Biosci (Elite ed) 6:225–235
Kassis I, Vaknin-Dembinsky A, Karussis D (2011) Bone marrow mesenchymal stem cells: agents of immunomodulation and neuroprotection. Curr Stem Cell Res Ther 6(1):63–68
Bliss T, Guzman R, Daadi M, Steinberg GK (2007) Cell transplantation therapy for stroke. Stroke 38(2 Suppl):817–826. doi:10.1161/01.str.0000247888.25985.62
Ai J, Kiasat-Dolatabadi A, Ebrahimi-Barough S, Ai A, Lotfibakhshaiesh N, Norouzi-Javidan A, Saberi H, Arjmand B, Aghayan HR (2014) Polymeric scaffolds in neural tissue engineering: a review. Arch Neurosci 1(1):15–20
Ai J, Tabatabaei FS, Larijani B (2009) A possible cell therapy for critical limb ischemia in women by using endometrial adult stem cells. Ther Crit Limb Isch 5:1–2
Esfandiari N, Khazaei M, Ai J, Bielecki R, Gotlieb L, Ryan E, Casper RF (2007) Effect of a statin on an in vitro model of endometriosis. Fertil Steril 87(2):257–262. doi:10.1016/j.fertnstert.2006.06.040
Ebrahimi-Barough S, Hoveizi E, Yazdankhah M, Ai J, Khakbiz M, Faghihi F, Tajerian R, Bayat N (2016) Inhibitor of PI3K/Akt signaling pathway small molecule promotes motor neuron differentiation of human endometrial stem cells cultured on electrospun biocomposite polycaprolactone/collagen scaffolds. Mol Neurobiol. doi:10.1007/s12035-016-9828-z
Esfandiari N, Ai J, Nazemian Z, Javed MH, Gotlieb L, Casper RF (2007) Expression of glycodelin and cyclooxygenase-2 in human endometrial tissue following three-dimensional culture. Am J Reprod Immunol 57(1):49–54. doi:10.1111/j.1600-0897.2006.00445.x
Ai J, Esfandiari N, Casper R (2009) Detection of aromatase in human endometrial tissue cultured in three-dimensional fibrin matrix in vitro. IJRM 7(3):105–109
Mobarakeh ZT, Ai J, Yazdani F, Sorkhabadi SMR, Ghanbari Z, Javidan AN, Mortazavi-Tabatabaei SAR, Massumi M, Barough SE (2012) Human endometrial stem cells as a new source for programming to neural cells. Cell Biol Int Rep 19(1):7–14
Ebrahimi-Barough S, Javidan AN, Saberi H, Joghataei MT, Rahbarghazi R, Mirzaei E, Faghihi F, Shirian S, Ai A, Ai J (2015) Evaluation of motor neuron-like cell differentiation of hEnSCs on biodegradable PLGA nanofiber scaffolds. Mol Neurobiol 52(3):1704–1713
Bayat N, Ebrahimi-Barough S, Ardakan MM, Ai A, Kamyab A, Babaloo H, Ai J (2016) Differentiation of human endometrial stem cells into Schwann cells in fibrin hydrogel as 3D culture. Mol Neurobiol. doi:10.1007/s12035-016-9730-8
Hoveizi E, Ebrahimi-Barough S, Tavakol S, Sanamiri K (2016) In vitro differentiation of human iPS cells into neural like cells on a biomimetic polyurea. Mol Neurobiol.doi: 10.1007/s12035–015–9663-7
Navaei-Nigjeh M, Amoabedini G, Noroozi A, Azami M, Asmani MN, Ebrahimi-Barough S, Saberi H, Ai A, Ai J (2014) Enhancing neuronal growth from human endometrial stem cells derived neuron-like cells in three-dimensional fibrin gel for nerve tissue engineering. J Biomed Mater Res A 102(8):2533–2543
Hoveizi E, Tavakol S, Ebrahimi-Barough S (2015) Neuroprotective effect of transplanted neural precursors embedded on PLA/CS scaffold in an animal model of multiple sclerosis. Mol Neurobiol 51(3):1334–1342
Tan J, Zheng X, Zhang S, Yang Y, Wang X, Yu X, Zhong L (2014) Response of the sensorimotor cortex of cerebral palsy rats receiving transplantation of vascular endothelial growth factor 165-transfected neural stem cells. Neural Regener Res 9(19):1763–1769. doi:10.4103/1673-5374.141785
Titomanlio L, Kavelaars A, Dalous J, Mani S, El Ghouzzi V, Heijnen C, Baud O, Gressens P (2011) Stem cell therapy for neonatal brain injury: perspectives and challenges. Ann Neurol 70(5):698–712. doi:10.1002/ana.22518
Ruff CA, Faulkner SD, Fehlings MG (2013) The potential for stem cell therapies to have an impact on cerebral palsy: opportunities and limitations. Dev Med Child Neurol 55(8):689–697. doi:10.1111/dmcn.12166
Harris DT (2008) Cord blood stem cells: a review of potential neurological applications. Stem Cell Rev 4(4):269–274. doi:10.1007/s12015-008-9039-8
Seledtsov VI, Kafanova MY, Rabinovich SS, Poveshchenko OV, Kashchenko EA, Fel'de MA, Samarin DM, Seledtsova GV, Kozlov VA (2005) Cell therapy of cerebral palsy. Bull Exp Biol Med 139(4):499–503
Chou CH, Fan HC, Hueng DY (2015) Potential of neural stem cell-based therapy for Parkinson's disease. Parkinsons Dis 2015:571475. doi:10.1155/2015/571475
Chen G, Wang Y, Xu Z, Fang F, Xu R, Wang Y, Hu X, Fan L, Liu H (2013) Neural stem cell-like cells derived from autologous bone mesenchymal stem cells for the treatment of patients with cerebral palsy. J Transl Med 11:21. doi:10.1186/1479-5876-11-21
Tso D, McKinnon RD (2015) Cell replacement therapy for central nervous system diseases. Neural Regen Res 10(9):1356–1358. doi:10.4103/1673-5374.165209
Tao H, Han Z, Han ZC, Li Z (2016) Proangiogenic features of mesenchymal stem cells and their therapeutic applications. Stem cells intern 2016:1314709. doi:10.1155/2016/1314709
Castorina A, Szychlinska MA, Marzagalli R, Musumeci G (2015) Mesenchymal stem cells-based therapy as a potential treatment in neurodegenerative disorders: is the escape from senescence an answer? Neur Regen Res 10(6):850–858. doi:10.4103/1673-5374.158352
Damien P, Allan DS (2015) Regenerative therapy and immune modulation using umbilical cord blood-derived cells. Biol Blood Marrow Transplant 21(9):1545–1554. doi:10.1016/j.bbmt.2015.05.022
Zhao F, Qu Y, Liu H, Du B, Mu D (2014) Umbilical cord blood mesenchymal stem cells co-modified by TERT and BDNF: a novel neuroprotective therapy for neonatal hypoxic-ischemic brain damage. Int J Dev Neurosci 38:147–154. doi:10.1016/j.ijdevneu.2014.06.014
Taran R, Mamidi MK, Singh G, Dutta S, Parhar IS, John JP, Bhonde R, Pal R, Das AK (2014) In vitro and in vivo neurogenic potential of mesenchymal stem cells isolated from different sources. J Biosci 39(1):157–169
Scardigli R, Capelli P, Vignone D, Brandi R, Ceci M, La Regina F, Piras E, Cintoli S, Berardi N, Capsoni S, Cattaneo A (2014) Neutralization of nerve growth factor impairs proliferation and differentiation of adult neural progenitors in the subventricular zone. Stem Cells 32(9):2516–2528. doi:10.1002/stem.1744
Deierborg T, Roybon L, Inacio AR, Pesic J, Brundin P (2010) Brain injury activates microglia that induce neural stem cell proliferation ex vivo and promote differentiation of neurosphere-derived cells into neurons and oligodendrocytes. Neurosci 171(4):1386–1396. doi:10.1016/j.neuroscience.2010.09.045
Dadwal P, Mahmud N, Sinai L, Azimi A, Fatt M, Wondisford FE, Miller FD, Morshead CM (2015) Activating endogenous neural precursor cells using metformin leads to neural repair and functional recovery in a model of childhood brain injury. Stem cell reports 5(2):166–173. doi:10.1016/j.stemcr.2015.06.011
Hosseini SM, Samimi N, Farahmandnia M, Shakibajahromi B, Sarvestani FS, Sani M, Mohamadpour M (2015) The preventive effects of neural stem cells and mesenchymal stem cells intra-ventricular injection on brain stroke in rats. N Am J Med Sci 7(9):390–396. doi:10.4103/1947-2714.166216
Smith DK, He M, Zhang CL, Zheng JC (2016) The therapeutic potential of cell identity reprogramming for the treatment of aging-related neurodegenerative disorders. Prog Neurobiol. doi:10.1016/j.pneurobio.2016.01.006
Gennai S, Monsel A, Hao Q, Liu J, Gudapati V, Barbier EL, Lee JW (2015) Cell-based therapy for traumatic brain injury. Br J Anaesth 115(2):203–212. doi:10.1093/bja/aev229
Bennet L, Tan S, Van den Heuij L, Derrick M, Groenendaal F, van Bel F, Juul S, Back SA, Northington F, Robertson NJ, Mallard C, Gunn AJ (2012) Cell therapy for neonatal hypoxia-ischemia and cerebral palsy. Ann Neurol 71(5):589–600. doi:10.1002/ana.22670
Dalous J, Pansiot J, Pham H, Chatel P, Nadaradja C, D'Agostino I, Vottier G, Schwendimann L, Vanneaux V, Charriaut-Marlangue C, Titomanlio L, Gressens P, Larghero J, Baud O (2013) Use of human umbilical cord blood mononuclear cells to prevent perinatal brain injury: a preclinical study. Stem cells develop 22(1):169–179. doi:10.1089/scd.2012.0183
Mathewson MA, Lieber RL (2015) Pathophysiology of muscle contractures in cerebral palsy. Phys Med Rehabil Clin N Am 26(1):57–67. doi:10.1016/j.pmr.2014.09.005
Berger R, Soder S (2015) Neuroprotection in preterm infants. BioMed Res Inter 2015:257139. doi:10.1155/2015/257139
Li L, Harms KM, Ventura PB, Lagace DC, Eisch AJ, Cunningham LA (2010) Focal cerebral ischemia induces a multilineage cytogenic response from adult subventricular zone that is predominantly gliogenic. Glia 58(13):1610–1619. doi:10.1002/glia.21033
Gonzales-Portillo GS, Sanberg PR, Franzblau M, Gonzales-Portillo C, Diamandis T, Staples M, Sanberg CD, Borlongan CV (2014) Mannitol-enhanced delivery of stem cells and their growth factors across the blood-brain barrier. Cell Transplant 23(4–5):531–539. doi:10.3727/096368914x678337
Chicha L, Smith T, Guzman R (2014) Stem cells for brain repair in neonatal hypoxia-ischemia. Childs Nerv Syst 30(1):37–46. doi:10.1007/s00381-013-2304-4
Cuchiara ML, Horter KL, Banda OA, West JL (2013) Covalent immobilization of stem cell factor and stromal derived factor 1alpha for in vitro culture of hematopoietic progenitor cells. Acta Biomater 9(12):9258–9269. doi:10.1016/j.actbio.2013.08.012
Zeng W, Wen C, Wu Y, Li L, Zhou Z, Mi J, Chen W, Yang M, Hou C, Sun J, Zhu C (2012) The use of BDNF to enhance the patency rate of small-diameter tissue-engineered blood vessels through stem cell homing mechanisms. Biomat 33(2):473–484. doi:10.1016/j.biomaterials.2011.09.066
Shamosi A, Mehrabani D, Azami M, Ebrahimi-Barough S, Siavashi V, Ghanbari H, Sharifi E, Roozafzoon R, Ai J (2016) Differentiation of human endometrial stem cells into endothelial-like cells on gelatin/chitosan/bioglass nanofibrous scaffolds. Artif Cells Nanomed Biotechnol 16:1–11
Yu JH, Seo JH, Lee JY, Lee MY, Cho SR (2016) Induction of neurorestoration from endogenous stem cells. Cell Transplant. doi:10.3727/096368916x690511
Kang M, Min K, Jang J, Kim SC, Kang MS, Jang SJ, Lee JY, Kim SH, Kim MK, An SA, Kim M (2015) Involvement of immune responses in the efficacy of cord blood cell therapy for cerebral palsy. Stem Cells Dev 24(19):2259–2268. doi:10.1089/scd.2015.0074
Sharpe K, Di Pietro N, Illes J (2016) In the know and in the news: how science and the media communicate about stem cells, autism and cerebral palsy. Stem Cell Rev 12(1):1–7. doi:10.1007/s12015-015-9627-3
Purandare C, Shitole DG, Belle V, Kedari A, Bora N, Joshi M (2012) Therapeutic potential of autologous stem cell transplantation for cerebral palsy. Case Rep Transplant 2012:825289. doi:10.1155/2012/825289
Ai J, Mehrabani D (2010) Are endometrial stem cells novel tools against ischemic heart failure in women? A hypothesis. IRCMJ 12(1):73–75
Mukherjee A, Raison M, Sahni T, Arya A, Lambert J, Marois P, James PB, Parent A, Ballaz L (2014) Intensive rehabilitation combined with HBO2 therapy in children with cerebral palsy: a controlled longitudinal study. Undersea Hyperb Med 41(2):77–85
Coulson-Thomas VJ, Coulson-Thomas YM, Gesteira TF, Kao WW (2016) Extrinsic and intrinsic mechanisms by which mesenchymal stem cells suppress the immune system. Ocul Surf. doi:10.1016/j.jtos.2015.11.004
Stagg J, Galipeau J (2013) Mechanisms of immune modulation by mesenchymal stromal cells and clinical translation. Curr Mol Med 13(5):856–867
Sd P, Greggio S, DaCosta JC (2010) Use of stem cells in perinatal asphyxia: from bench to bedside. J Pediatr 86(6):451–464
Srivastava P, Bhasin A, Mohanty S, Sharma S, Kiran U, Bal C, Gaikwad S, Singh M, Bhatia R, Tripathi M (2011) Restorative therapy using autologous bone marrow derived mononuclear cells infusion intra-arterially in patients with cerebral palsy: an open label feasibility study. Neurol Asia 16(3):231–239
Vawda R, Fehlings MG (2013) Mesenchymal cells in the treatment of spinal cord injury: current & future perspectives. Curr Stem Cell Res T 8(1):25–38
Phinney DG, Isakova IA (2014) Mesenchymal stem cells as cellular vectors for pediatric neurological disorders. Brain Res 1573:92–107. doi:10.1016/j.brainres.2014.05.029
Hosseini SM, Farahmandnia M, Razi Z, Delavarifar S, Shakibajahromi B (2015) 12 hours after cerebral ischemia is the optimal time for bone marrow mesenchymal stem cell transplantation. Neur Reg Res 10(6):904–908. doi:10.4103/1673-5374.158354
Chen L, Cui X, Wu Z, Jia L, Yu Y, Zhou Q, Hu X, Xu W, Luo D, Liu J, Xiao J, Yan Q, Cheng L (2014) Transplantation of bone marrow mesenchymal stem cells pretreated with valproic acid in rats with an acute spinal cord injury. Biosci Tren 8(2):111–119
Borlongan CV, Glover LE, Tajiri N, Kaneko Y, Freeman TB (2011) The great migration of bone marrow-derived stem cells toward the ischemic brain: therapeutic implications for stroke and other neurological disorders. Prog Neurobiol 95(2):213–228. doi:10.1016/j.pneurobio.2011.08.005
Zhao Y, Lai W, Xu Y, Li L, Chen Z, Wu W (2013) Exogenous and endogenous therapeutic effects of combination Sodium Ferulate and bone marrow stromal cells (BMSCs) treatment enhance neurogenesis after rat focal cerebral ischemia. Metab Brain Dis 28(4):655–666. doi:10.1007/s11011-013-9425-z
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiasatdolatabadi, A., Lotfibakhshaiesh, N., Yazdankhah, M. et al. The Role of Stem Cells in the Treatment of Cerebral Palsy: a Review. Mol Neurobiol 54, 4963–4972 (2017). https://doi.org/10.1007/s12035-016-0030-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-0030-0