Abstract
The present study investigated the correlation between interleukin-6 (IL-6) and tumor necrosis factor alpha (TNF-α) levels in cerebrospinal fluid (CSF) and subarachnoid hemorrhage (SAH) progression. A meta-analysis was further conducted from pooled data to analyze the clinical value of IL-6 and TNF-α in SAH diagnosis. In our case-control study, a total of 57 SAH patients were assigned to two groups, CVS group (n = 27) and non-CVS group (n = 30), based on the presence of cerebral vasospasm (CVS). In addition, 65 healthy subjects were enrolled as controls. IL-6 and TNF-α levels in CSF were measured in all the study subjects by enzyme-linked immunosorbent assay (ELISA). For meta-analysis, an exhaustive literature search was conducted to identify relevant published articles and strict inclusion and exclusion criteria were applied to select studies for the present meta-analysis. Data extracted from these studies was analyzed using STATA 12.0 software. IL-6 and TNF-α levels in CSF of SAH patients were markedly higher than those of healthy controls (all P < 0.001). Further, CVS patients showed elevated IL-6 and TNF-α levels in CSF compared to non-CVS patients (all P < 0.001). The increase in IL-6 and TNF-α levels in CSF correlated with the increasing disease severity, based on Hunt-Hess grade, in SAH patients (all P < 0.05). Our meta-analysis also confirmed that IL-6 and TNF-α CSF levels were markedly higher in SAH patients compared to healthy controls (all P < 0.001). Ethnicity-stratified analysis showed that both IL-6 and TNF-α CSF levels were elevated in Asian SAH patients, compared to their healthy counterparts (all P < 0.05). The TNF-α CSF levels were significantly higher in Caucasian SAH patients (P < 0.001), but the IL-6 CSF levels showed no such differences compared to the healthy controls (P = 0.219). Subgroup analysis based on the presence of CVS showed that both IL-6 and TNF-α CSF levels were markedly higher in CVS patients than those in non-CVS patients (all P < 0.05). Our results provide strong evidence that IL-6 and TNF-α CSF levels are elevated in SAH patients and may participate in SAH development. Thus, these two cytokines could be important biomarkers for early diagnosis and disease monitoring in SAH patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) is an acute cerebrovascular event and a fatal neurosurgical emergency that can have devastating effects on the central nervous system and profound impact on the vital functions of several other organs [1]. SAH is a major cause of morbidity and mortality worldwide and accounts for 25 % of stroke-related mortalities. Overall, SAH represents 5 % of all stroke cases and affects up to 30,000 individuals each year in North America [2, 3]. Cerebral vasospasm (CVS) is the morphological narrowing of cerebral arteries and is a frequent complication associated with aneurismal SAH, causing significant morbidity and mortality [4]. The onset and etiology of CVS are difficult to establish, and SAH patients frequently display delayed onset of CVS, resulting in delayed cerebral ischemia (DCI) [5]. Although the exact pathophysiology of SAH has remained elusive, previous studies provide a clue that infiltration of red blood cells into subarachnoid space and cerebral cisterns, accompanied by their subsequent lysis, produces pronounced immune responses mediated by proinflammatory cytokines [6]. Currently, there are no validated biomarkers for diagnosis or monitoring of preclinical vasospasms, but two prominent areas of investigation for novel biomarker discovery include neuroimaging and biochemical markers in body fluids, such as serum/plasma and cerebrospinal fluid (CSF) [7]. Elevated inflammatory responses mediated by increased cytokine release in CSF and plasma correlate with adverse clinical outcomes in SAH patients [8, 9]. The levels of cytokines and cytokine receptors increase significantly in CSF following SAH, but a precise relationship between SAH progression and the inflammatory markers in CSF remains unclear [10].
A variety of factors influence cytokine levels in body fluids. For example, dynamic exercise causes a transient increase in serum concentration of various immunomodulatory proteins, including proinflammatory cytokines interleukin-6 (IL-6) and tumor necrosis factor alpha (TNF-α) [11, 12]. IL-6 is a cytokine prominently involved in inflammation and host response to infections and also plays a significant role in the regulation of metabolism, tissue regeneration, and neural development [13]. On the other hand, TNF-α was first described by Carswell et al. in 1975 as a serum protein component that was capable of inducing cell death in cancer cell lines in vitro and completely eliminating transplanted sarcomas in vivo in a mouse xenograft model [14, 15]. TNF-α is a critical cytokine involved in initiating inflammatory responses and may play a central role in generation of oxidative stress and apoptosis of endothelial cells, widely observed in SAH [6]. In clinical studies, ongoing inflammation is detected by measuring the levels of inflammatory markers in plasma or in the CSF [7, 10, 16]. Increased IL-6 level in CSF is linked to the higher incidence of CVS and is associated with worse patient outcomes [17]. SAH severity, according to the Hunt-Hess grade, correlates with increasing levels of inflammatory cytokines, especially TNF-α, and the levels of inflammatory cytokines are associated with correspondingly poorer outcomes in SAH patients [18]. Nevertheless, multiple previous studies attempting to correlate IL-6 and TNF- α levels in CSF with SAH outcomes reported conflicting results [19–21]. In this report, IL-6 and TNF-α CSF levels were examined in a case-control study involving carefully selected SAH patients. In addition, a meta-analysis was performed to verify the results of our case-control study and further analyze the pooled data on IL-6 and TNF-α levels in CSF of SAH patients.
Materials and Methods
Ethics Statement
This study was approved by the Institutional Review Board of the First Hospital of Jilin University. All participants were enrolled in this study after signing written informed consents. All the study procedures were in accordance with the Declaration of Helsinki [22].
Study Participants
Between September 2010 and August 2014, a total of 57 SAH patients (33 males and 24 females; mean age 57.9 ± 9.5 years, range 30 to 75 years; average body mass index [BMI] 19.6 ± 2.7 kg/cm2) were recruited at the Department of Neurosurgery, the First Hospital of Jilin University. SAH diagnosis was confirmed by cranial computed tomography (CT) scan, and all patients were diagnosed as intracranial aneurysm based on computed tomography angiography (CTA) or magnetic resonance angiography (MRA), with intra-arterial digital subtraction angiography (DSA). Patients were excluded if they had the following diseases: infections, heart diseases, autoimmune diseases, malignant tumors, and hematonosis. Patients receiving drugs or treatments that affect immune functions were also excluded. The disease severity in SAH patients was assessed at admission using Hunt-Hess grade, neurological examination, and the onset of headache [23]. Of the 57 SAH patients, 10 patients were classified as neurological grade I, 25 as neurological grade II, 14 as neurological grade III, and 8 as neurological grade IV or V. Based on the presence of CVS, SAH patients were divided into two groups: CVS group (n = 27) and non-CVS group (n = 30). The diagnostic criteria for CVS were as follows: (1) symptom fluctuation or disease aggravation after treatment; (2) drowsiness or patient became progressively confused and entered into coma; (3) presence of focal signs; (4) increased intracranial pressure; (5) patients were confirmed as mild CVS (120~140 cm/s), moderate CVS (141~200 cm/s), and severe CVS (141~200 cm/s) based on the middle cerebral artery (MCA) blood flow measured by transcranial Doppler (TCD) ultrasonography, and the flow velocity ratio for MCA and internal carotid artery (ICA) was more than 3; and (6) rebleeding after SAH [24]. In addition, 65 healthy controls (35 males and 30 females; mean age 59.2 ± 10.6 years, range 32 to 73 years; average BMI 20.5 ± 3.1 kg/cm2), without any history of steroids and immunosuppressive drugs, were enrolled as healthy group at the same medical center. Importantly, no significant differences in age, gender, and BMI were observed between the SAH group and healthy controls.
Sample Collection
CSFs (3 mL) from SAH patients and healthy controls were collected by routine lumbar puncture on the second day of admission and during the physical examination, respectively. The collected samples were centrifuged at 800g for 10 min to remove cells and stored at −70 °C until further analysis. The levels of IL-6 and TNF-α in the CSF were measured by enzyme-linked immunosorbent assay (ELISA) using a commercially available ELISA kit (R&D Systems, Minneapolis, MN) and following all the manufacturers’ instructions.
Statistical Analysis
All statistical analyses were performed using STATA version 12.0 software (Stata Corporation, College Station, TX, USA). Categorical data were expressed as numbers and percentages and were analyzed by χ 2 test. Continuous variables with normal distribution were expressed as mean ± standard deviation (SD). The t test was used to measure the differences between two groups of continuous variables. A P value of <0.05 was considered as statistically significant.
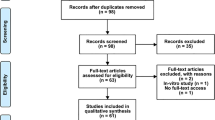
A comprehensive search was conducted to identify relevant published studies using the databases PubMed (1966~2015) and Chinese Biomedical Literature Database (CBM, 1978~2015). The search strategy included medical subject headings (MESH) terms and keywords as follows: (“subarachnoid hemorrhage” or “SAH” or “primary subarachnoid hemorrhage” or “acute hemorrhagic cerebrovascular disease”) and (“cerebrospinal fluid” or “CSF”) and (“interleukin” or “IL”) and (“tumor necrosis factor” or “TNF”). The cross-references of selected articles were manually reviewed to identify other relevant studies. The standard mean difference (SMD) with 95 % confidence intervals (95 %CI) was estimated by fixed effects model or random effects model to evaluate the association between CSF levels of IL-6 and TNF-α and SAH severity. Z test was employed to detect the significance of the pooled effect size [25].
Results
Cranial CT Images in SAH Patients and Healthy Controls
The cranial CT images in SAH patients and healthy controls are shown in Fig. 1a, b. The cranial CT scan of SAH patients showed a high-density shadow in sulci and cisterns.
Association of TNF-α and IL-6 Levels in CSF with Hunt-Hess Grade
Table 1 shows significantly higher IL-6 and TNF-α levels in CSF of SAH patients (Hunt-Hess grade I~V) compared to healthy controls (all P < 0.05). Further, Hunt-Hess grade II SAH patients showed higher IL-6 and TNF-α levels in CSF compared to Hunt-Hess grade I patients (IL-6: t = 2.32, P = 0.026; TNF-α: t = 2.81, P = 0.008). The CSF levels of both IL-6 and TNF-α were elevated in Hunt-Hess grade III SAH patients compared to Hunt-Hess grade II SAH patients (IL-6: t = 2.39, P = 0.022; TNF-α: t = 2.16, P = 0.037). In addition, Hunt-Hess grade IV~V SAH patients also showed higher CSF levels of IL-6 and TNF-α than Hunt-Hess grade III SAH patients (IL-6: t = 2.10, P = 0.048; TNF-α: t = 2.09, P = 0.049).
IL-6 and TNF-α CSF Levels in SAH Patients and Healthy Controls
The mean IL-6 levels in CSF of SAH patients and healthy controls were 325.31 ± 25.68 and 13.05 ± 4.16 pg/mL, respectively, revealing significant differences between the two groups (t = 96.65, P < 0.001) (Fig. 2a). Additionally, mean TNF-α levels in CSF of SAH patients and healthy controls were 49.68 ± 7.02 and 12.47 ± 2.15 pg/mL, respectively, showing that TNF-α levels in CSF of SAH patients were significantly higher than those of the healthy controls (t = 40.64, P < 0.001) (Fig. 2b).
IL-6 and TNF-α CSF Levels in CVS Patients and Non-CVS Patients
Within the SAH patient group, the mean IL-6 and TNF-α levels in CSF of CVS patients were 362.56 ± 30.14 and 56.12 ± 8.15 pg/mL, respectively. On the other hand, mean IL-6 and TNF-α levels in CSF of non-CVS patients were 291.79 ± 21.67 and 43.88 ± 6.01 pg/mL, respectively. The result showed that IL-6 and TNF-α levels in CSF of CVS patients were markedly higher than those of non-CVS patients (L-6: t = 10.25, P < 0.001; TNF-α: t = 6.50, P < 0.001) (Fig. 3a, b).
Results of Meta-Analysis
Following an exhaustive literature search and study selection process, 13 studies finally met our inclusion criteria for the present meta-analysis [26–38]. Our meta-analysis results showed that both IL-6 and TNF-α levels in CSF of SAH patients were markedly higher than those of the healthy controls (IL-6: SMD = 4.63, 95 %CI = 2.56~6.70, P < 0.001; TNF-α: SMD = 7.78, 95 %CI = 4.23~11.32, P < 0.001) (Fig. 4a, b). Ethnicity-stratified analysis further revealed that both IL-6 and TNF-α levels in CSF of SAH patients were significantly elevated in Asian SAH patients compared to their healthy controls (IL-6: SMD = 3.32, 95 %CI = 1.18~5.46, P = 0.002; TNF-α: SMD = 11.34, 95 %CI = 6.14~16.53, P < 0.001). In addition, subgroup analysis based on ethnicity further showed that CSF levels of TNF-α in Caucasian SAH patients were significantly higher than those in their corresponding healthy controls (TNF-α: SMD = 3.02, 95 %CI = 2.23~3.82, P < 0.001), but a similar association was not observed for IL-6 CSF levels and SAH in Caucasians (IL-6: SMD = 10.39, 95 %CI = −6.19~26.97, P = 0.219) (Fig. 5a, b). Subgroup analysis based on the presence of CVS in SAH patients showed that CSF levels of both IL-6 and TNF-α were markedly higher in CVS patients than those in non-CVS patients (IL-6: SMD = 2.45, 95 %CI = 1.17~3.73, P < 0.001; TNF-α: SMD = 0.92, 95 %CI = 0.09~1.74, P = 0.029) (Fig. 6a, b).
Ethnicity-stratified analysis for the difference of IL-6 and TNF-α CSF levels between SAH patients and healthy controls. a IL-6 CSF level of SAH patients was significantly higher than that of healthy controls in Asians. b TNF-α CSF level in SAH patients was markedly higher than that in healthy controls in Asians and Caucasians
Forest plots of the comparison of the IL-6 and TNF-α CSF levels between cerebral vasospasm (CVS) patients and non-CVS patients. a IL-6 CSF level of CVS patients was significantly higher than that of non-CVS patients. b TNF-α CSF level of CVS patients was markedly higher than that of non-CVS patients
Discussion
IL-6 and TNF-α are proinflammatory cytokines that regulate multiple physiological processes [39, 40]. Evidence shows that IL-6 and TNF-α play an important role in cerebral tissue injury, but the underlying mechanism is poorly understood [7, 12]. We performed a case-control study and a meta-analysis to carefully examine the relationship between SAH and CSF levels of IL-6 and TNF-α. In our study, IL-6 CSF level was sharply increased in SAH patients compared to healthy controls, suggesting that inflammatory responses mediated by IL-6 may play an important role in SAH progression. Further, our results showed that CSF levels of IL-6 were higher in Hunt-Hess grade I-IV SAH patients compared to healthy controls and CSF levels of IL-6 increased with the disease grade. Collectively, these results suggested that elevated IL-6 CSF level may influence SAH progression and may predict poor clinical outcomes in SAH patients. Approximately, 25 % of SAH patients require temporary external CSF drainage to treat hydrocephalus and this offers a unique opportunity to study the changes in brain physiology and pharmacology in patients by using these CSF samples [9]. Previous studies showed that IL-6 concentrations are elevated in CSF of patients following SAH and in patients with poor Glasgow Outcome Scale (GOS), compared to patients with moderate or good GOS, indicating that higher IL-6 levels in CSF correlate with worse clinical outcomes [9, 41]. Data also suggests that when the possibility of infection is eliminated by thorough examination, IL-6 may be a valuable early diagnostic indicator in SAH patients [10]. A potential mechanism for the chronic CSF obstruction due to increased IL-6 levels could be microgliosis and scar formation within CSF. Consistent with this, a previous study reported that increased IL-6 levels in CSF significantly elevated the number of glial fibrillary acidic protein (GFAP)-immunoreactive astrocytes and ionized calcium-binding adaptor molecule-1 (Iba-1)-reactive microglia, causing a massive reactive gliosis, which resulted in widespread cerebral hypertrophy [42, 43]. Astrocytosis and microgliosis, along with the increased expressions of GFAP and Iba-1, play key roles in the development of neonatal and acquired communicating hydrocephalus [44]. Importantly, an increase in IL-6 levels in both peripheral and central circulation is associated with pronounced inflammation response in SAH patients [9].
Our findings also revealed that TNF-α levels in CSF of SAH patients were higher than those of healthy controls and TNF-α CSF levels increased with disease severity, suggesting that elevated TNF-α level in CSF may be associated with SAH progression. SAH is a common occurrence in accidents that cause cerebrovascular injuries, and inflammation rapidly occurs in subarachnoid space following SAH [45]. TNF-α is a key cytokine in the inflammatory cascade and plays an important role in the host defense against infections [46]. TNF-α level also correlates with delayed complications of SAH such as DCI [6]. Current theories behind the evolution of DCI involve impaired fibrinolytic activity, activation of inflammatory cascade, and endothelial dysfunction leading to microthrombi formation, all of which involve TNF-α activity [6]. TNF-α stimulates the expression of intercellular adhesion molecule-1 (ICAM-1) in arachnoid cells and lymphocyte function-associated antigen-1 (LFA-1) in T lymphocytes, respectively [45]. The result suggests that arachnoid cells assist T lymphocyte invasion into the subarachnoid space following SAH and this physiological response is sensitive to TNF-α levels. Chou et al. demonstrated that elevated TNF-α level following SAH is linked to poor long-term outcome, after accounting for the Hunt-Hess grade, suggesting that TNF-α may hold significant promise as a clinical biomarker to predict SAH outcome [18]. Our findings are consistent with previous studies. We show that elevated IL-6 and TNF-α CSF levels are associated with SAH development and correlate with Hunt-Hess grade. In addition, we conducted a meta-analysis and found that IL-6 and TNF-α CSF levels in SAH patients were higher than those in healthy controls, confirming that higher IL-6 and TNF-α CSF levels are intimately associated with SAH development and progression.
Further, our case-control study and accompanying meta-analysis results also confirmed that SAH patients with CVS exhibited sharply elevated IL-6 and TNF-α levels in CSF, compared to non-CVS patients. CVS is the most common cause of acute focal cerebral ischemia following SAH and is defined as development of new focal neurologic deficits in SAH patients, which occurs in approximately one third of SAH patients [7, 47]. TNF-α activity correlates with oxidative stress, cell death, and recruitment of other inflammatory mediators [48]. TNF-α levels increase within 2–3 days following SAH, and elevated TNF-α levels correlate with poor 3- and 6-month outcomes in SAH patients, potentially leading to CVS in many cases [49]. It is also known that patients with CVS exhibit higher IL-6 CSF levels on days 4 and 5 following SAH; thus, elevated IL-6 levels in CSF could be a potential early biomarker for CVS [50]. Taken together, these results indicated that both TNF-α and IL-6 play important roles in the development of CVS following SAH and could be developed as reliable biomarkers for early detection.
Subgroup analyses based on ethnicity were conducted to explore factors influencing our meta-analysis results. The ethnicity-stratified analysis showed that TNF-α level in CSF of SAH patients was markedly higher than that of healthy controls in Asians and Caucasians. On the other hand, IL-6 level in CSF was elevated in SAH patients, compared to healthy controls, only in Asians, but such an association was not observed in Caucasians. These differences in ethnic groups could be attributed to geographical, environmental, and genetic factors.
Limitations of this study should be noted while interpreting our results. First, lack of access to original data of the studies selected for meta-analysis limited our further assessment of potential interactions. Second, the meta-analysis included 13 studies that were performed in Caucasians and Asians, with other ethnicities not represented in the studies, which may result in selection bias and limit the universal applicability of the results. Further, 4 out of 5 selected studies in Asian SAH patients were from China, with only one study from Korea. Thus, the findings in Asian population may not be applicable to all Asians and further studies are required on the associations of IL-6 and TNF-α CSF levels with SAH in Asian population from different geographical locations. Moreover, studies published in language other than English and Chinese were not included in our meta-analysis.
In conclusion, our findings strongly suggest that both IL-6 and TNF-α levels in CSF are associated with SAH and may directly be involved in the development and progression of SAH. Therefore, the two cytokines could be important biomarkers of early diagnosis and disease monitoring in SAH patients.
References
Diringer MN, Bleck TP, Claude Hemphill J 3rd et al (2011) Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit Care 15:211–240
Connolly ES Jr, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737
Sehba FA, Pluta RM, Zhang JH (2011) Metamorphosis of subarachnoid hemorrhage research: from delayed vasospasm to early brain injury. Mol Neurobiol 43:27–40
Testai FD, Aiyagari V, Hillmann M et al (2011) Proof of concept: endogenous antiangiogenic factors predict the occurrence of symptomatic vasospasm post subarachnoid hemorrhage. Neurocrit Care 15:416–420
Vergouwen MD, Vermeulen M, van Gijn J et al (2010) Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke 41:2391–2395
Hanafy KA, Grobelny B, Fernandez L et al (2010) Brain interstitial fluid TNF-alpha after subarachnoid hemorrhage. J Neurol Sci 291:69–73
Lad SP, Hegen H, Gupta G et al (2012) Proteomic biomarker discovery in cerebrospinal fluid for cerebral vasospasm following subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 21:30–41
Muroi C, Frei K, El Beltagy M et al (2008) Combined therapeutic hypothermia and barbiturate coma reduces interleukin-6 in the cerebrospinal fluid after aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol 20:193–198
Singh N, Hopkins SJ, Hulme S et al (2014) The effect of intravenous interleukin-1 receptor antagonist on inflammatory mediators in cerebrospinal fluid after subarachnoid haemorrhage: a phase II randomised controlled trial. J Neuroinflammation 11:1
Hopkins SJ, McMahon CJ, Singh N et al (2012) Cerebrospinal fluid and plasma cytokines after subarachnoid haemorrhage: CSF interleukin-6 may be an early marker of infection. J Neuroinflammation 9:255
Timmerman KL, Amonette WE, Markofski MM et al (2015) Blunted IL-6 and IL-10 response to maximal aerobic exercise in patients with traumatic brain injury. Eur J Appl Physiol 115:111–118
Sarrafzadeh A, Schlenk F, Gericke C et al (2010) Relevance of cerebral interleukin-6 after aneurysmal subarachnoid hemorrhage. Neurocrit Care 13:339–346
Wang Y, Li G, Su YM et al (2014) Interleukin-6 promotor polymorphisms and coronary vasospastic angina in Han Chinese. Int J Clin Exp Med 7:2858–2864
Carswell EA, Old LJ, Kassel RL et al (1975) An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci U S A 72:3666–3670
Park KM, Bowers WJ (2010) Tumor necrosis factor-alpha mediated signaling in neuronal homeostasis and dysfunction. Cell Signal 22:977–983
McMahon CJ, Hopkins S, Vail A et al (2013) Inflammation as a predictor for delayed cerebral ischemia after aneurysmal subarachnoid haemorrhage. J Neurointerv Surg 5:512–517
Muroi C, Bellut D, Coluccia D et al (2011) Systemic interleukin-6 concentrations in patients with perimesencephalic non-aneurysmal subarachnoid hemorrhage. J Clin Neurosci 18:1626–1629
Chou SH, Feske SK, Atherton J et al (2012) Early elevation of serum tumor necrosis factor-alpha is associated with poor outcome in subarachnoid hemorrhage. J Investig Med 60:1054–1058
Pickard JD, Murray GD, Illingworth R et al (1989) Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial. BMJ 298:636–642
Jayaraman T, Paget A, Shin YS et al (2008) TNF-alpha-mediated inflammation in cerebral aneurysms: a potential link to growth and rupture. Vasc Health Risk Manag 4:805–817
Aoki T, Kataoka H, Shimamura M et al (2007) NF-kappaB is a key mediator of cerebral aneurysm formation. Circulation 116:2830–2840
Holt GR (2014) Declaration of Helsinki—the world’s document of conscience and responsibility. South Med J 107:407
Rosen DS, Macdonald RL (2005) Subarachnoid hemorrhage grading scales: a systematic review. Neurocrit Care 2:110–118
Bacigaluppi S, Zona G, Secci F et al. (2015) Diagnosis of cerebral vasospasm and risk of delayed cerebral ischemia related to aneurysmal subarachnoid haemorrhage: an overview of available tools. Neurosurg Rev
Chen H, Manning AK, Dupuis J (2012) A method of moments estimator for random effect multivariate meta-analysis. Biometrics 68:1278–1284
Mathiesen T, Andersson B, Loftenius A et al (1993) Increased interleukin-6 levels in cerebrospinal fluid following subarachnoid hemorrhage. J Neurosurg 78:562–567
Osuka K, Suzuki Y, Tanazawa T et al (1998) Interleukin-6 and development of vasospasm after subarachnoid haemorrhage. Acta Neurochir (Wien) 140:943–951
Fassbender K, Hodapp B, Rossol S et al (2001) Inflammatory cytokines in subarachnoid haemorrhage: association with abnormal blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry 70:534–537
Kwon KY, Jeon BC (2001) Cytokine levels in cerebrospinal fluid and delayed ischemic deficits in patients with aneurysmal subarachnoid hemorrhage. J Korean Med Sci 16:774–780
Hendryk S, Jarzab B, Josko J (2004) Increase of the IL-1 beta and IL-6 levels in CSF in patients with vasospasm following aneurysmal SAH. Neuroendocrinol Lett 25:141–147
Zhang ZL, Yu QQ, He XY (2005) Study of serum and cerebrospinal fluid interleukin-6 levels in patients with subarachnoid hemorrhage. Stroke Nerv Dis 12:33–35
Schoch B, Regel JP, Wichert M et al (2007) Analysis of intrathecal interleukin-6 as a potential predictive factor for vasospasm in subarachnoid hemorrhage. Neurosurgery 60:828–836, discussion 828–836
Ni W, Gu YX, Song DL et al (2011) The relationship between IL-6 in CSF and occurrence of vasospasm after subarachnoid hemorrhage. Acta Neurochir Suppl 110:203–208
Lee JH, Park DH, Back DB et al (2012) Comparison of cerebrospinal fluid biomarkers between idiopathic normal pressure hydrocephalus and subarachnoid hemorrhage-induced chronic hydrocephalus: a pilot study. Med Sci Monit 18:PR19–PR25
Liu ZW, Kong WL, Shi XF et al (2012) Study of cerebrospinal fluid interleukin-6 levels in patients with aneurysmatic subarachnoid hemorrhage. Chin J Clin (Electronic Edition) 06:1140–1143
Liu BG, Gong XH, He LM et al (2012) Measurement of IL-1β, IL-6 and TNF-α levels in cerebrospinal fluid of patients with aneurysmal subarachnoid hemorrhage and its significance. J Clin Res 29:404–406
Jiang JQ, Zhao XW, Guo ZW et al (2013) Changes of cerebrospinal fluid and serum cytokine levels in the elderly patients with subarachnoid hemorrhage. Chin J Gerontol 33:2288–2289
Xie X, Wu X, Cui J et al (2013) Increase ICAM-1 and LFA-1 expression by cerebrospinal fluid of subarachnoid hemorrhage patients: involvement of TNF-alpha. Brain Res 1512:89–96
Vecchione C, Frati A, Di Pardo A et al (2009) Tumor necrosis factor-alpha mediates hemolysis-induced vasoconstriction and the cerebral vasospasm evoked by subarachnoid hemorrhage. Hypertension 54:150–156
Pradilla G, Chaichana KL, Hoang S et al (2010) Inflammation and cerebral vasospasm after subarachnoid hemorrhage. Neurosurg Clin N Am 21:365–379
Fassbender K, Hodapp B, Rossol S et al (2001) Inflammatory cytokines in subarachnoid haemorrhage: association with abnormal blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry 70:534–537
Wostrack M, Reeb T, Martin J et al (2014) Shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: the role of intrathecal interleukin-6. Neurocrit Care 21:78–84
Chakrabarty P, Jansen-West K, Beccard A et al (2010) Massive gliosis induced by interleukin-6 suppresses Abeta deposition in vivo: evidence against inflammation as a driving force for amyloid deposition. FASEB J 24:548–559
Deren KE, Packer M, Forsyth J et al (2010) Reactive astrocytosis, microgliosis and inflammation in rats with neonatal hydrocephalus. Exp Neurol 226:110–119
Xie X, Wu X, Cui J et al (2013) Increase ICAM-1 and LFA-1 expression by cerebrospinal fluid of subarachnoid hemorrhage patients: involvement of TNF-alpha. Brain Res 1512:89–96
Mariette X, Matucci-Cerinic M, Pavelka K et al (2011) Malignancies associated with tumour necrosis factor inhibitors in registries and prospective observational studies: a systematic review and meta-analysis. Ann Rheum Dis 70:1895–1904
Jung CS, Lange B, Zimmermann M et al (2013) CSF and serum biomarkers focusing on cerebral vasospasm and ischemia after subarachnoid hemorrhage. Stroke Res Treat 2013:560305
Beeftink MM, Ruigrok YM, Rinkel GJ et al (2011) Relation of serum TNF-alpha and TNF-alpha genotype with delayed cerebral ischemia and outcome in subarachnoid hemorrhage. Neurocrit Care 15:405–409
Przybycien-Szymanska MM, WW Ashley Jr. (2015) Biomarker discovery in cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis
Schoch B, Regel JP, Wichert M et al (2007) Analysis of intrathecal interleukin-6 as a potential predictive factor for vasospasm in subarachnoid hemorrhage. Neurosurgery 60:828–836, discussion 828–836
Acknowledgments
We would like to acknowledge the reviewers for their helpful comments on this paper.
Conflict of Interest
The authors have declared that no competing interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, W., Guan, Y., Zhao, G. et al. Elevated IL-6 and TNF-α Levels in Cerebrospinal Fluid of Subarachnoid Hemorrhage Patients. Mol Neurobiol 53, 3277–3285 (2016). https://doi.org/10.1007/s12035-015-9268-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9268-1