Abstract
The purpose of this study was to evaluate the impact of breast size on acute and late side effects in breast cancer (BC) patients treated with hypofractionated radiotherapy (Hypo-RT). In this study we analyzed patients over 50 years with a diagnosis of early BC, candidate for Hypo-RT after conservative surgery. Acute and late skin toxicities were evaluated in accordance with the RTOG scale. Multivariable logistic analysis was performed using dosimetric/anatomical factors resulted associated with toxicity outcome in univariable analysis. Among patients treated between 2009 and 2015, 425 had at least 5 years of follow-up. At RT end, acute skin toxicity ≥ G2 and edema ≥ G2 occurred in 88 (20.7%) and 4 (0.9%) patients, respectively. The multivariable analysis showed association of skin toxicity with boost administration (p < 0.01), treated skin area (TSA) receiving more than 20 Gy (p = 0.027) and breast volume receiving 105% of the prescription dose (V105%) (p = 0.016), but not breast size. At 5 years after RT, fibrosis ≥ G1 occurred in 89 (20.9%) patients and edema ≥ G1 in 36 (8.5%) patients. Fibrosis resulted associated with breast volume ≥ 1000 cm3 (p = 0.04) and hypertension (p = 0.04). As for edema, multivariable logistic analysis showed a correlation with hypertension and logarithm of age, but not with boost administration. Breast volume had an unclear impact (p = 0.055). A recurrent association was found between acute and late toxicities and breast V105%, which is correlated with breast size. This may suggest that a more homogenous RT technique may be preferred for patients with larger breast size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A recent systemic review of 17 randomized trial involving more than 10,000 patients confirmed the benefit of adjuvant radiotherapy (RT) on local control and overall survival for women with early breast cancer (BC) [1]. Shortened, hypofractionated radiotherapy (Hypo-RT) were compared to standard fractionation in many randomized trials and at a follow-up of 5–10 years’ equivalence in terms of local control, survival, and toxicity has been shown [2,3,4].
The first randomized trial was conducted in Canada where a dose of 42.4 Gy in 16 fractions against 50 Gy in 25 fractions were compared, resulting in equivalent local control and breast cosmesis [2]. The two most recent randomized studies, conducted in the UK, have demonstrated that hypofractionation offers a favorable tolerance and loco-regional tumor control [3, 4].
Moreover, the recent update of the American Society of Radiation Oncology evidence-based guidelines on RT for the whole breast confirmed that hypo-RT represents the new standard for patients with early-stage BC, regardless of age, chemotherapy administration, and breast size [5].
Nevertheless, its implementation in routine RT clinical practice across the world varies for numerous reason [6].
In the Canadian trial [2] large breast size was an exclusion criterion, whereas the results of START trials have not been stratified for this feature [3, 4].
Due to the lack of consensus, different parameters were used to define the breast size, such as clothing and bra size, or the distance between the lateral and medial field edge or the measurement of volumes that could be the planning or the clinical target volume (CTV), or the volume included in an isodose (50% or 90%). Moreover, if you evaluate planning target volume (PTV) to discriminate small breasts from large ones, the cutoff to consider is not well defined in literature [7].
Three-dimensional conformal radiation therapy (3D-CRT) still represents the standard of treatment for BC patients except for peculiar anatomical shapes and patients where intensity modulated [8], or volumetric techniques offer a real dosimetric or clinical advantage. The use of 3D-CRT in large breast size patients could increase dose inhomogeneity and subsequently late toxicity and cosmesis, as reported by retrospective studies [9,10,11,12]. The intensity-modulated radiotherapy (IMRT) and volumetric arc therapy (VMAT) techniques could improve dose homogeneity and this might translate as an improved toxicity profile [13,14,15,16,17,18].
In the recent randomized DBCG HYPO trial, BC patients received hypofractionated 3D-CRT with two tangential fields and a forward-planned field-in-field technique for homogeneous dose distribution, and the late toxicity in terms of induration was related to breast volume and not to the boost [19].
Based on this background, we evaluated the impact of breast size on long-term toxicity in our large series of patients with BC treated with 3D-CRT Hypo-RT and sequential boost.
Materials and methods
Patients, data collection, and radiation treatment
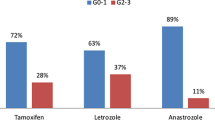
BC patients receiving hypofractionated whole-breast irradiation at Istituto Nazionale dei Tumori in Milan from April 2009 to December 2020, were considered for the study. Inclusion criteria were (a) breast conservative surgery (quadrantectomy) before RT; (b) early BC cases: pathological stage pT1-pT2 and pN0-pN1 according to TNM stage; (c) systemic therapy prescribed after multidisciplinary evaluation; (d) patients had to be at least 50 years old; (e) follow-up longer than 6 months. All patients underwent clinical examination before irradiation, weekly during the treatment and every 6 months after the course. Before starting RT, several clinical data including age, diabetes, hypertension, and information on medical treatments (type and adjuvant chemotherapy, hormonal deprivation, other concomitant drugs) were prospectively collected. Patients were stratified into two subgroups according to breast size: group A, presenting with breast size < 1000 cm3; group B, presenting with breast size ≥ 1000 cm3.
The planning Computed Tomography scan (5 mm slice thickness) from the level of the larynx to the upper abdomen was obtained in the supine position using “breast-board” or other personalized immobilization device with both arms raised above the head. CTV and PTV were defined according to ESTRO guidelines [20]. Organs at risk (OARs) (lungs, heart, and contralateral breast) were contoured. A 3D-CRT was planned both for whole-breast and boost irradiations. For the irradiation of the whole breast, two isocentric tangential fields were used and the plans were optimized using wedge filter, bolus, or the MLC. In general, two beams were used also for the boost irradiation. The whole breast was treated to a total dose of 42.4 Gy in 16 consecutive daily fractions, 2.65 Gy per fraction. The boost prescription followed a prospective prognostic factors policy based on previous published experience [2, 21]. The boost dose was 10 Gy in four fractions for grade III invasive BC and 16 Gy in eight fractions for patients with close (< 1 mm) or positive margins if a re-excision of the tumor bed could not be performed. The presence of surgical clips was recommended but not mandatory. In the absence of clips, the presence of a seroma or an architectural distortion area of the mammary gland structure was considered to identify the tumor bed. The dose was prescribed to the ICRU reference point and the dosimetric objective was to cover 95% of the PTV with at least 95% of the Prescribed Total Dose (PTD); in few cases of peculiar anatomical shape, we accepted 95% of the PTV to receive 90% of the PTD. For each patient, dose-volume histograms (DVHs) for the PTV and OARs were obtained. Dose constraints for OARs were the volume (V20) of the ipsilateral lung receiving 20 Gy < 20%; heart mean dose < 5 Gy or heart V20 < 10%. Dosimetric data were also collected with special focus on dose inhomogeneity defined as the absolute volumes of breast tissues exposed to the 105% of PTD, i.e., 44.52 Gy (V105%), and the treated skin area (TSA) receiving more than 20 Gy—treated skin was defined as a 5 mm layer from the skin surface.
Toxicity assessment
Acute skin toxicity was assessed during the treatment, at the end of RT, 2 weeks after the end of RT and then at 6 months. Late effects were assessed every year. Acute and late skin toxicities were evaluated in accordance with the RTOG grading scale. For this analysis, we considered late toxicity at 5 years because there was no significant difference in terms of toxicity with the previous follow-up.
Statistical analysis
Summary data were reported as frequencies and percentages, for categorical variables, or median and interquartile range, for continuous variables. Differences among groups of patients, at breast volume of 1000 cm3, were estimated with Chi-Squared test or Kruskal–Wallis test for categorical and continuous variables, respectively.
Correlation among continuous predictors was tested by Spearman test, while Chi Squared was used for categorical ones. Association between factors and toxicities was estimated in logistic univariable analysis. Specifically, those factors with a p value ≤ 0.2, hence showing a possible relation with the toxicity, were included in multivariable analysis. For variable selection, the number of toxicity events was considered, as well. To avoid the overfitting or paradoxical fitting, the variables included in the model did not exceed 10% of event occurrences [22, 23].
In multivariable logistic regression, Odds Ratios (ORs) were significant with p values ≤ 0.05. In case the linearity assumption did not hold, the predictor was transformed or split in classes. Therefore, in addition to the continuous type, age was grouped as < 70, 70–74,75–79, and 80 + , breast volume was split at 800 or 1000 cm3, V105% at 450 cm3, and TSA (> 20 Gy) at 200 cm3, considered the best thresholds for our dataset. Results were shown as OR and 95% CI in squared brackets. The analyses were carried out with R version 4.0.3.
Results
425 patients, treated between 2009 and 2015 at our institution, had at least 5 years of follow-up. The median follow-up was 78 months (range 67–89 months). Patients’ demographic and dosimetric characteristics are shown in Table 1. The median age was 73 (range 70–77 years). 355 patients had breast size < 1000 cm3 (group A) and 70 patients had breast size ≥ 1000 cm3 (group B). The boost was administered in 129 patients (30%), 98 patients of group A and 31 patients of group B, respectively. The median breast volume was 632 cm3 (range 438–784) in group A and 1129 cm3 (range 1056–1406) in group B, respectively. The median boost volume was 47.5 cm3 (range 28.1–75.2) in group A and 77.0 cm3 (range 51.2–100) in group B, respectively.
Table 2 shows the frequency distribution of toxicity at RT end and after 5 years. In Table 3 univariable and multivariable analyses are shown for skin toxicity and fibrosis at RT end and after 5 years, respectively. Frequency distribution of toxicity at 2 weeks after RT are displayed in the Supplementary Materials (Table S1), along with logistic regression results for skin toxicity and edema at 2 weeks and 5 years after RT, respectively, and for skin toxicity at RT end in the subgroup receiving boost.
At RT completion, toxicity ≥ G2 occurred in 88 (20.5%) patients for skin toxicity, 10 (2.3%) for asthenia, and 4 (0.9%) for both edema and fibrosis, only skin toxicity reporting significative Chi-Squared test (p = 0.07) for differences between A and B groups. The univariate logistic analysis (Table 3) showed a correlation between skin toxicity and boost administration (p < 0.01), breast volume (p = 0.01), breast V105% (p < 0.01), TSA (> 20 Gy) (p < 0.01), and all their subgroups. Among boost receiving patients, 40 (31%) showed skin toxicity and no more than 5 (3.88%) the other toxicities. Despite its significant association with breast size groups A and B, skin toxicity was correlated only to the boost size in univariate analysis (Tables 2, S2B).
At 2 weeks after RT, skin toxicity was recorded in 48 (10.77%) women and asthenia in 7 (1.6%), while the same patients than before suffered edema and fibrosis (4, 0.9%). No toxicity was associated with breast volume group (i.e., Chi-Squared test). Skin toxicity was related only to TSA (> 20 Gy) (p = 0.01) and edema only to breast V105% (p < 0.01) (Supplementary Materials Table S2A).
At 5 years after RT, toxicity ≥ G1 at skin occurred in 3 (0.7%) patients, edema in 36 (8.5%) patients, and 89 (20.9%) suffered fibrosis. No Chi-Squared test with p < 0.05 for these toxicities was found. Relation with fibrosis and edema in univariate logistic analysis was present for V105% at 450 cm3 (p < 0.01) and age (log scale, p = 0.03), respectively (Tables 3, S2A). However, some variables were associated with a p ≤ 0.2, i.e., breast volume ≥ 1000 cm3 and hypertension.
Correlation was present (rho = 0.59; p < 0.01) only among breast volume and breast V105%. Due to correlation, these variables could not appear in the same model simultaneously and the multivariable logistic model was performed and displayed only using breast volume predictor. Breast V105% was reported as a possible alternative, but its OR was estimated in a separate model with the same controlling covariates of breast size. Results were almost the same, if not differently specified.
In multivariable analysis skin toxicity at RT end was associated with the boost administration [OR 2.09 (1.17–3.42)] and TSA (> 20 Gy) ≥ 200 cm3 [OR 2.01 (1.08–3.74)]. As for breast volume, it was not significantly associated, but skin toxicity OR increase of 0.6% at breast V105% unit increase (cm3) [OR 1.006 (1.001–1.01)].
Being boost administration significative, the same analysis was performed among patients receiving boost. The size of boost volume resulted associated with skin toxicity at RT completion [OR 1.019 (1.008–1.033), Table S2B]. After 2 weeks, in the whole sample, the skin toxicity was weakly associated only to TSA (> 20 Gy) [OR 1.005 (1.00–1.011)] (Supplementary Materials Table S2A).
Multivariable analysis for late toxicity was performed on edema and fibrosis. Since the former had a non-linear relationship with age, but with its logarithmic transformation, here we referred to age classes. The OR association was higher for patients over 75 years old, with respect to the first age class. In addition, edema decreased in hypertensive patients [OR 0.40 (0.18–0.83)]. Breast volume was a potential affecting factor for edema [OR 2.31 (0.95–5.33)], however. On the other hand, fibrosis at 5 years from RT was associated with breast volume ≥ 1000 cm3 [OR 1.89 (1.01–3.47)]. Using breast V105% in place of breast volume, linearity assumption did not hold and the variable cutoff at 450 cm3 was used patients with breast V105% higher than 450 cm3 had almost twice and half OR of fibrosis [OR 2.39 (0.991–5.585)].
Discussion
The use of Hypo-RT in large breast size patients has always been a matter of discussion. Lots of randomized controlled trials have demonstrated the equivalent clinical efficacy of Conventional Fractionation (CF) and Hypo-RT in breast cancer patients [2,3,4, 24], but there are few data regarding long-term toxicity and cosmetic outcomes in large breast size patients. In this kind of patients, the use of Hypo-RT led to a widespread concern related to a possible increase of dose inhomogeneity, and consequently, of side effects [25].
Advances in RT techniques allowed mitigating dose inhomogeneity to the target volume. In the 3D-CRT the field-in-field technique is one of them developed to provide homogeneous dose distribution [26]. Also the introduction of IMRT and VMAT techniques in the treatment of large breast size decreases the dose inhomogeneity that probably is the responsible factor that influenced long-term toxicity and cosmetic outcomes [13,14,15,16,17,18].
Retrospective experiences have reported data only on the acute side effects of Hypo-RT in this specific setting.
Hannan et al. [27] compared patients with small or large breast size (chest wall separation > 25 cm or breast volume > 1500 cm3) treated with Hypo-RT and IMRT techniques. The authors confirmed that Hypo-RT also in large breast size patients had acceptable dosimetry with acute toxicity profile, comparable with data reported in the literature on CF.
Corbin et al. [28] published their prospectively collected data on large breast size patients treated with conventional or hypofractionated RT and forward-planned field-in-field technique. Despite the small sample size, they reported no significant differences in terms of acute toxicity between the two groups.
Patel et al. [29] reported data on acute toxicity of 502 women treated with Hypo 3D-CRT. They found that age > 64 years, BMI > 34 kg/m, breast volume > 1500 cm3, and breast V105% > 10% were significant independent predictors of grade 3 acute toxicity.
De Rose et al. [30] retrospectively analyzed patients with early-stage BC treated with 3-week hypofractionated VMAT to the whole breast (40.5 Gy) and SIB (48 Gy). They identified two cohort of patients based on breast size: 1000 cm3 was considered the cutoff to discriminate small and large breast size. The TSA receiving more than 20 Gy > 400 cm2 resulted as a significant predictor of both acute and late skin toxicities at 2 years; however, at 5 years, no breast size or dosimetric parameter suggested indications for increased toxicity. A worse cosmetic outcome was recorded at the 2-year follow-up for large breast size but was not confirmed at the 5-year follow-up. Nevertheless, this study had some limitations because only 352 had a 5-year follow-up and cosmesis was evaluated only by treating physicians during the follow-up.
In the HYPO trial [19], 882 patients who underwent breast-conserving surgery for node-negative breast cancer or ductal carcinoma in situ (DCIS), were randomly assigned to radiotherapy at a dose of either 50 Gy in 25 fractions or 40 Gy in 15 fractions. Smoking and a breast volume > 600 cm3 were associated with worse toxicity in the whole cohort, but there were no differences between Hypo- and CF RT. There were no significant late skin toxicity differences between large and small breast size patients.
At last, ASTRO Guidelines also suggest that the decision to offer Hypo-RT should be independent of breast size, provided that dose-homogeneity goals can be achieved.
There are few data about late toxicity in large breast size patients treated with Hypo-RT delivered with a 3D technique. To our knowledge, our study is the first assessing the impact of breast size on acute and long-term toxicity in a series of BC patients treated with Hypo and 3D-CRT. In our series of 425 patients, we reported at univariate analysis an association between acute skin toxicity and TSA (> 20 Gy) > 200 cm3 (p ≤ 0.01). The 20 Gy choice was made according to recent published literature [30]. Breast volume or breast V105% and boost had an impact only at RT end. Boost volume affected skin toxicity among those 129 patients receiving boost. No association with p < 0.05 was found for these toxicities, except for age (p = 0.03) and breast V105% (p < 0.01) with edema at 5 years after RT.
Multivariable logistic regression confirmed the TSA (> 20 Gy) ≥ 200 cm3 role in skin toxicity mainly at RT completion and after 2 weeks. However, the impact of breast V105%, boost administration, and size was present only after RT. After 5 years, prognostic factors increasing edema and fibrosis occurrence were breast volume ≥ 1000 cm3. Patients over 75 years old significantly experienced edema toxicity, while those administered with breast V105% ≥ 450 cm3 had fibrosis OR significantly higher than patients receiving less.
The strength of our study was the homogeneity of clinical and dosimetric data prospectively collected as reported in our previously studies [31, 32]. Moreover, each patient had at least 5 years of follow-up which is a sufficient time to assess late toxicity.
Our study has some limitations. We did not report cosmetic results because they were evaluated only by a single physician and not always the same person. Photographic findings were not available as we considered this evaluation non-objective and unrealistic. Furthermore, the series analyzed does not include patients under 50 years of age because hypofractionation in young patients was subsequently implemented, so in this setting the follow-up was not adequate.
Conclusion
Hypo-RT can be considered a safe treatment for large breast size patients too. A recurrent association was found between the toxicities (at the 3 time points) and the breast V105%, which is correlated with the breast size. This may suggest that a more homogenous RT technique may be preferred for patients with larger breast size (volumetric modulated RT or a field-in-field techniques usually give a more homogenous dose distribution than the tangential fields technique). More research is also needed to enlighten patients’ intrinsic characteristics that empower toxicities.
References
Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomized trials. Lancet. 2011;378(9804):1707e16.
Whelan TJ, Pignol JP, Levine MN, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010;362:513–20.
Bentzen SM, Agrawal RK, START Trialists’ Group, et al. The UK standardisation of breast radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet Oncol. 2008;9:331–41.
Bentzen SM, Agrawal RK, START Trialists’ Group, et al. The UK standardisation of breast radiotherapy (START) trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet. 2008;371:1098–107.
Smith BD, Bellon JR, Blitzblau R, et al. Radiation therapy for the whole breast: executive summary of an American society for radiation oncology (ASTRO) evidence-based guideline. Pract Radiat Oncol. 2018;8:145–52.
Ratosa I, Chirilă ME, Steinacher M, et al. Hypofractionated radiation therapy for breast cancer: preferences amongst radiation oncologists in Europe—results from an international survey. Radiother Oncol. 2020;155:17–26. https://doi.org/10.1016/j.radonc.2020.10.008 (Online ahead of print).
Ratosa I, Jenko A, Oblak I. Breast size impact on adjuvant radiotherapy adverse effects and dose parameters in treatment planning. Radiol Oncol. 2018;52:233–44.
Moody AM, Mayles WP, Bliss JM, et al. The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. Radiother Oncol. 1994;33:106–12.
Brierley JD, Paterson IC, Lallemand RC, Rostom RY. The influence of breast size on late radiation reaction following excision and radiotherapy for early breast cancer. Clin Oncol (R Coll Radiol). 1991;3:6–9.
Gray JR, McCormick B, Cox L, Yahalom J. Primary breast irradiation in large-breasted or heavy women: analysis of cosmetic outcome. Int J Radiat Oncol Biol Phys. 1991;21:347–54.
Goffman TE, Glatstein E. Hypofractionation redux? J Clin Oncol. 2004;22:589–91.
Vicini FA, Sharpe M, Kestin L, et al. Optimizing breast cancer treatment efficacy with intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2002;54:1336–44.
Michalski A, Atyeo J, Cox J, Rinks M, Morgia M, Lamoury G. A dosimetric comparison of 3D-CRT, IMRT, and static tomotherapy with a SIB for large and small breast volumes. Med Dosim. 2014;39:163–8.
Croog VJ, Wu AJ, McCormick B, Beal KP. Accelerated whole breast irradiation with intensity-modulated radiotherapy to the prone breast. Int J Radiat Oncol Biol Phys. 2009;73:88–93.
Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol. 2008;26:2085–92.
Hong L, Hunt M, Chui C, et al. Intensity-modulated tangential beam irradiation of the intact breast. Int J Radiat Oncol Biol Phys. 1999;44:1155–64.
Donovan E, Bleakley N, Denholm E, et al. Breast technology. Group randomised trial of standard 2D radiotherapy (RT) versus intensity modulated radio-therapy (IMRT) in patients prescribed breast radiotherapy. Radiother Oncol. 2007;82:254–64.
Formenti SC, Gidea-Addeo D, Goldberg JK, et al. Phase I-II trial of prone accelerated intensity modulated radiation therapy to the breast to optimally spare normal tissue. J Clin Oncol. 2007;25:2236–42.
Offersen BV, Alsner J, Nielsen HM, et al. Hypofractionated versus standard fractionated radiotherapy in patients with early breast cancer or ductal carcinoma in situ in a randomized phase III trial; the DBCG HYPO trial. J Clin Oncol. 2020;38(31):3615–25.
Offersen BV, Boersma LJ, Kirkove C, et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early-stage breast cancer. Radiother Oncol. 2015;114(1):3e10.
Jones HA, Antonini N, Hart AA, et al. Impact of pathological characteristics on local relapse after breast-conserving therapy: a subgroup analysis of the EORTC boost versus no boost trial. J Clin Oncol. 2009;27(30):4939e47.
Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87.
Hickey BE, James ML, Lehman M, et al. Hypofractionated radiation therapy for early breast cancer. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.
Franco P, Bartoncini S, Martini S, Iorio GC, Richard U. Do hypofraction and large breast size reciprocally fit in breast cancer radiotherapy? Ann Transl Med. 2019;7(Suppl 3):S146. https://doi.org/10.21037/atm.2019.06.26.
Onal C, Sonmez A, Arslan G, Oymak E, Kotek A, Efe E, Sonmez S, Dolek Y. Dosimetric comparison of the field-in-field technique and tangential wedged beams for breast irradiation. Jpn J Radiol. 2012;30(3):218–26. https://doi.org/10.1007/s11604-011-0034-7.
Hannan R, Thompson RF, Chen Y, et al. Hypofractionated whole-breast radiation therapy: does breast size matter? Int J Radiat Oncol Biol Phys. 2012;84:894–901.
Corbin KS, Dorn PL, Jain SK, et al. Hypofractionated radiotherapy does not increase scute toxicity in large-breasted women: results from a prospectively collected series. Am J Clin Oncol. 2014;37:322–6.
Patel AK, Ling DC, Richman AH, et al. Hypofractionated whole-breast irradiation in large-breasted women—is there a dosimetric predictor for acute skin toxicities? Int J Radiat Oncol Biol Phys. 2019;103:71–7.
De Rose F, Fogliata A, Franceschini D, et al. Hypofractionated whole breast irradiation and simultaneous integrated boost in large-breasted patients: long-term toxicity and cosmesis. Clin Breast Cancer. 2020;20(6):527–33. https://doi.org/10.1016/j.clbc.2020.06.005.
De Santis MC, Bonfantini F, Di Salvo F, et al. Factors influencing acute and late toxicity in the era of adjuvant hypofractionated breast radiotherapy. Breast. 2016;29:90–5. https://doi.org/10.1016/j.breast.2016.07.013.
La Rocca E, Meneghini E, Lozza L, et al. Older age and comorbidity in breast cancer: is RT alone the new therapeutic frontier? J Cancer Res Clin Oncol. 2020;146(7):1791–800. https://doi.org/10.1007/s00432-020-03243-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we do not have any conflict of interest.
Ethical approval
The present study has been reviewed and approved by the Internal Review Board of the Department of Radiation Oncology 1 of National Cancer Institute, Milan, Italy.
Research involving in human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Colciago, R.R., Cavallo, A., Magri, M.C. et al. Hypofractionated whole-breast radiotherapy in large breast size patients: is it really a resolved issue?. Med Oncol 38, 107 (2021). https://doi.org/10.1007/s12032-021-01550-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-021-01550-6