Abstract
The aim of the present study was to identify predictors of outcome and complications in patients with small hepatocellular carcinoma (HCC) treated by percutaneous microwave ablation (MWA). Patients with non-previously treated small (≤ 3 cm) HCCs who underwent ultrasound (US)-guided percutaneous MWA between July 2016 and January 2019 were included. For each patient, the following variables were registered: age, sex, albumin, platelet count, INR/PT, PTT ratio, total bilirubin, liver status, etiology of liver disease, Child–Pugh classification, tumor dimension, margin, and hepatic segment, tumor subcapsular, perihilar or perivascular location, HCC focality, ascites. During follow-up, complications and outcomes were registered. Variables were then analyzed in relation to both outcomes and complications. 74 patients were included. Mean CT follow-up was 6.2 months (range 1–24 months). At least one complication occurred in 48% of patients, the majority being asymptomatic imaging findings not requiring intervention. One major complication was registered (duodenal perforation: 1.3%). The occurrence of complications was associated with HCC multifocality and abnormal INR/PT, duodenal wall edema with tumor dimension, portal vein thrombosis with Child Pugh score, perihepatic free fluid with abnormal platelet count and comorbidities. Incomplete response rate at 1 month was 18.9%. Local tumor progression and new HCC nodules rates were 13.5% and 27%, respectively. Incomplete response at 1 month was associated with both alcoholic etiology of liver disease and II segment tumor location, new HCC nodules with PBC. Despite the small series analyzed, significant factors related with complications and outcomes may be kept in mind when planning the best treatment for each patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver cancer is the second most common cause of cancer death worldwide [1].
Hepatocellular carcinoma (HCC) is the most predominant histological type and accounts for > 85% of all primary liver cancers [1].
The optimal curative therapy for patients with HCC is surgical resection or liver transplantation [2].
However, these therapies are often not feasible due to severe impairment of hepatic functional reserve, bilobar distribution of the tumors, extra-hepatic metastasis, involvement of the portal vein or liver donor paucity. Only 9–27% of patients with HCC have been reported to be eligible for surgical resection [2].
For this reason, various local ablative therapies, such as ethanol ablation, radiofrequency ablation (RFA) and microwave ablation (MWA), have been developed as an alternative to resection or liver transplantation [3].
These treatments play an important role as nonsurgical options that can achieve high local cure rates without significant reduction of the background liver function [4].
Percutaneous RFA has been proved to be more effective in terms of local cure when compared to ethanol injection [5]; moreover, survival outcomes for patients who achieved a complete response by RFA are comparable to that among patients treated by hepatic resection [6, 7]. RFA is now generally accepted as a curative treatment for very early or early stage HCC as defined by the Barcelona Clinic Liver Cancer (BCLC) treatment strategy [8].
MWA has shown to have several advantages when compared to other ablative modalities [9].
Microwaves radiate through all biological tissues, including charred, desiccated and high electrical impedance tissues, like the ones produced by ablation itself. These technical features permit to reduce procedure times, to achieve high temperatures in the target tumor obtaining larger volumes of cellular necrosis, and to be more efficient on lesions with cystic components, with a reduction in the heat-sink effect, and less intra-procedural pain [10, 11]. The MWA ablation zone has been considered less susceptible to the heat-sink effect when compared to RFA, as shown in animal models and clinical studies, especially for primary liver tumors [12,13,14]; however, this was not confirmed by other studies analyzing outcomes after MWA treatment of liver metastases [15, 16]. The use of MWA has spread in the last years and it’s being now commonly used by many institutions for the treatment of various neoplasms, including HCC.
Regardless of the treatment modality, HCC is a disease characterized by the burden of high recurrence rates.
Many studies have been performed on recurrence and complication rates after surgical resection, RFA or MWA of HCC [3, 4]. Some authors have searched for risk factors for complications and predictors of outcome after percutaneous thermal ablation of HCC, with the majority of the reports focusing on RFA [4, 17,18,19,20]. A smaller number of studies have focused on finding significant associations between various patient and/or tumor factors and safety or outcome in the treatment of small HCC by MWA [21, 22].
We carried out an analysis of patients and nodule characteristics that may be related with outcomes.
The aim of this study is to identify predictors of effectiveness and risk factors for complications in patients affected by small HCC nodules that were treated in our institution with percutaneous US-guided MWA.
Materials and methods
Population and tumor data
This retrospective study was conducted with the approval of our Internal Review Board.
Data regarding patients with ≥ 1 non-previously treated HCC nodule measuring up to 3 cm in maximum diameter who underwent percutaneous US-guided MWA of at our institution between July 2016 and January 2019 were collected. For this study, only 1 treated nodule per patient was analyzed. Eligible patients were at least 18 years of age with liver primary disease only. Patients whose preoperative CT or MRI exams could not be reviewed were excluded. We also excluded patients with nodules measuring > 3 cm or patients who already underwent surgical resection, trans-arterial chemoembolization or thermal ablation of the lesion that we treated with percutaneous US-guided MWA. For each patient, the following data were registered: age, sex, pre-procedural serum albumin (normal ≥ 3.4 g/dl, abnormal < 3.4 g/dl), blood platelet count (normal ≥ 100,000/µl of blood, abnormal < 100,000/µl), INR/PT value (normal ≤ 1.3, abnormal > 1.3), PTT ratio (normal ≤ 1.2, abnormal > 1.2), blood total bilirubin (normal ≤ 1.2 mg/dl, abnormal > 1.2 mg/dl), liver status (normal, hepatitis or cirrhosis), etiology of liver disease (alcohol, HBV, HCV, autoimmune hepatitis, non-alcoholic steato-hepatitis and PBC), Child–Pugh classification, comorbidities (none, diabetes, COPD, ESRD, HF/IHD). Images from the last exam performed before ablation, either computed tomography (CT) or magnetic resonance imaging (MRI), were reviewed for each patient, and the following data were registered: tumor diameter, tumor margin type, tumor segment, subcapsular, perihilar or perivascular tumor location, presence of ascites, and tumor focality (unifocal, multifocal). Tumor margin was defined irregular when an irregular contour involved > 50% of the lesion circumference. Nodules were classified as subcapsular when located ≤ 1 cm from hepatic capsule, perihilar when located ≤ 1 cm from hepatic hilum, and perivascular if located within 1 cm from a vessel measuring at least 2 mm. Regarding tumor focality, HCC was considered unifocal when the nodule that we treated was the only present within the liver, while it was defined multifocal when the liver presented > 1 nodule besides the target one.
MWA procedure
Informed consent was obtained from all patients before procedure.
An Anesthesiologist assisted the patient during the whole ablation session. Moderate sedation was achieved in each patient through intravenous injection of propofol, fentanyl and midazolam. Vital parameters (heart rate, respiratory rate, blood pressure), together with oxygen saturation and electrocardiographic tracing, were continuously monitored during the procedure.
All patients received an antibiotic prophylaxis according to an “ultra-short-term” scheme that consists in pre-procedural intravenous administration of 1 g cefazolin.
Lidocaine was injected to obtain local anesthesia in correspondence of the entrance site of the antenna that was positioned under US-guidance (Arietta V70, Hitachi Aloka Medical, Tokyo, Japan; Epic 7, Philips, The Best, Netherlands) in all cases.
The ablation system consisted of a microwave generator, capable of producing a power of 100 W at 2450 MHz, connected to a 13.5-gauge straight microwave antenna with a 2.8-cm radiating section by coaxial cable. Continuous perfusion with saline solution at 60 ml/min and at room temperature was provided by the system along the proximal part of the antenna to avoid any thermal damage.
Ablation power and time were decided according to data given by the manufacturer and to operator’s preference. The ablation field was assessed continuously by US during the whole procedure.
Ablation power and time were registered for each patient.
Outcome and analysis of predictors of outcomes and risk factors for complications
Each patient underwent a contrast-enhanced CT exam 1 month post-procedure to detect early complications and to assess MWA efficacy. The latter depended on the occurrence of a complete or incomplete response.
Complete response was defined as the absence of any enhancing tissue into or about the ablation field (Fig. 1), while incomplete response occurred when a enhancing area at the periphery of the ablative zone was seen (Fig. 2).
Computed tomography (CT) scans in a 56-year-old man with a hepatocellular carcinoma (HCC) nodule 20 mm in diameter in segment 8 of the liver. Pretreatment contrast-enhanced CT scan shows hyperattenuation of the nodule during arterial phase (a), rapid wash-out in the venous (b) and hypoattenuation in the delayed phase (c). At one month follow-up, CT shows uniform hypoattenuation in the ablated area, which indicates complete ablation (d–f)
Computed tomography (CT) scans in a 65-year-old man with a 15 mm hepatocellular carcinoma (HCC) nodule in segment 2 of the liver. Pretreatment contrast-enhanced CT scan shows hyperattenuation of the nodule during arterial phase (a), isoattenuation in the venous phase (b) and hypoattenuation in the delayed phase (c) (arrow head). At 1 month follow-up, CT shows hypoattenuation in the ablated area (arrow head) (d) with evidence of a residual enhancing lesion denoting incomplete response (arrow) (d–f)
The images at 1 month were also compared to the pre-procedural ones to assess the presence of a safe ablation volume margin, which occurred if the ablation volume resulted at least > 5 mm wider than the original lesion, in all planes.
Following our Institutional follow-up protocol, our patients underwent then a new contrast-enhanced CT exam at 3 months after procedure, and every 3 months thereafter, in order to detect late complications and the presence of local tumor progression and/or new HCC nodules.
According to the Standardization of Terminology and Reporting Criteria [18] local tumor progression was defined as the appearance of tumor tissue at the edge of the ablation zone after adequate intervention documented by contrast-enhanced follow-up study performed ≥ 3 months after treatment. A new HCC nodule was defined as appearance of a lesion with HCC features in a different area from the treated zone at least 3 months after intervention
Complications were classified according to CIRSE Quality Assurance Document and Standards for Classification of Complications [23]. Major complications were defined as an adverse event of grade ≥ 3 that required at least additional post-procedure therapy or prolonged hospital stay (< 48 h) with no post-procedure sequelae. Minor complications were defined as an adverse event of grade 1–2 that required at most a prolonged observation including overnight stay (as a deviation from the normal post-therapeutic course < 48 h), with no additional post-procedure therapy, nor any sequelae. Minor complications included any deviation from normality, including asymptomatic radiological findings at follow-up.
Statistical analysis
The association of 20 variables with the occurrence of complications during follow-up was investigated. These included: age; sex; albumin; platelets; INR/PT; PTT ratio; bilirubin; liver status; etiology of liver disease; Child–Pugh classification; comorbidities; tumor diameter; tumor margin type; tumor segment; subcapsular location; perihilar location; perivascular location; tumor focality; presence of ascites; presence of > 5 mm ablative margin at first follow-up exam.
The significance of 12 variables as predictors of outcome was then investigated. The variables were: age; sex; liver status; etiology of liver disease; tumor diameter; tumor margin type; tumor segment; subcapsular location; perihilar location; perivascular location; tumor focality; presence of > 5 mm ablative margin at first follow-up exam.
To evaluate categorical variables, contingency table, Pearson χ2-test and Fisher's Exact Test were used. To evaluate ordinal or continuous variables, Mann–Whitney U test was used.
SPSS v25.0.0 (IBM, Chicago, IL) was used for all statistical analyses. p values were considered significant when < 0.05.
Results
Patient and tumor-related factors
A total number of 74 patients with non-previously treated small (≤ 3 cm) HCCs underwent percutaneous US-guided MWA at our institution between July 2016 and January 2019.
Age, sex, liver status, etiology of liver disease, Child Pugh score and comorbidities of the population are reported in Table 1. The majority of patients presented with a single liver disease etiology (81%), while in 19% there were two concurrent causes of liver disease.
Table 2 reports the distribution of the population on the basis of normality or abnormality of the blood test values registered before intervention.
The diameter of the target HCC nodules, together with their segment and location (subcapsular, perivascular, perihilar) are reported by Table 3. Multiple nodules were present in the liver at the time of the diagnosis in 22/74 cases (29.7%), while the target lesion was the only HCC nodule in the remainder. Irregular margins were evident in 15/74 cases (20.2%). MWA was carried out with a power of 100 W in all cases, with a mean time of duration of 226 s (range 90–420 s).
Complications
Mean CT follow-up time was 6.2 months (range 1–24 months).
During follow-up at least one complication occurred in 36/74 patients (48%), the vast majority being minor. Minor complication rates were: asymptomatic perihepatic free fluid in 15/74 (20.2%); biliary system dilatation in 8/74 (10.8%); involvement of capsule by ablation volume in 8/74 cases (10.8%), artero-venous fistula (AVF) in 7/74 cases (9.4%); abdominal collection in 3/74 cases (4%); duodenal walls edema in 2/74 cases (2.7%), hemoperitoneum in 1 case (1.3%). One major complication occurred in one patient (duodenal perforation: 1/74; rate: 1.3%).
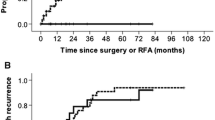
Mann–Whitney U test showed a significant association between duodenal wall edema and primary tumor diameter (17.29 ± 5.77 mm vs. 8.50 ± 2.12 mm; mean ± standard deviation for uncomplicated vs. complicated); portal vein thrombosis was significantly associated with Child Pugh score (5.50 ± 0.77 vs. 6.63 ± 0.92; mean ± standard deviation for uncomplicated vs. complicated). The box plots of these results are illustrated in Fig. 3. Chi-square test showed a significant association between: occurrence of perihepatic free fluid after intervention and both pre-procedural abnormal platelets count (p = 0.01) and comorbidities (p = 0.03); the occurrence of complications of any kind during follow-up with both HCC multifocality at the time of intervention (p = 0.02) and abnormal pre-procedural INR/PT (p = 0.02). Moreover, Fisher's Exact Test showed a significant association between the occurrence of portal vein thrombosis and both abnormal albumin (p = 0.02) and abnormal platelet count (p = 0.03).
Outcome
Incomplete response was registered in 14/74 cases (18.9%) at 1 month after procedure. Local tumor progression was recorded in 10/74 cases (13.5%) during follow-up at a mean time of 8.4 months after intervention (range 3–24 months). New HCC nodules were recorded in 20/74 cases (27%); the mean time to detect new tumors was 6.8 months (range 3–24 months).
Mann–Whitney U test didn’t show any significant association between variables and outcome.
Chi-square test showed a significant association between: incomplete response at one month, and both alcoholic etiology of liver disease (p = 0.01) and II segment HCC nodule location (p = 0.007); the appearance of new HCC nodules and primary biliary cirrhosis as etiology of liver disease (p = 0.02).
Chi-square test results for outcomes are illustrated in Fig. 4.
Bar charts derived from Chi-square test for outcome. Chi-square test showed a significant association between: incomplete response at 1 month and both alcoholic etiology of liver disease (a), and II segment HCC nodule location (b); the appearance of new HCC nodules and PBC as etiology of liver disease (c)
Discussion
The aim of the present study was to identify risk factors for the development of complications and predictors of outcomes in patients with small non-previously treated HCC nodules that underwent US-guided percutaneous MWA at our institution.
Despite few data available about potential factors implicated with outcome in patients with small HCC (≤ 3 cm) treated with MWA, many authors have tried to find a significant association between a number of variables and the outcome of patients with HCC treated with RFA. For example, absence of a > 5 mm safe ablative margin and tumors of large dimensions, with possible satellite nodules and microscopic infiltration, resulted to be significantly related with incomplete ablation; also, local tumor progression has been significantly associated to periportal location of tumor and patient age by some authors [24, 25].
In our population, we detected a local incomplete response at one month in 18.9% cases (14/74). Our results showed a significant association between incomplete response at one month and alcoholic cirrhosis (p = 0.01). This could reflect a more progressed stage of HCC-related pathological changes in the liver. As recently pointed out by Ganne-Carrié and Nahon, because of impaired surveillance and poor patient compliance, HCC is often detected late in patients with chronic alcoholic liver disease, leading to a more advanced and less responsive disease [26].
Also, a significant association was found between incomplete response at 1 month and II segment HCC nodule location. The II segment presents major challenges for percutaneous treatment with thermal ablation. First, it’s located just below the diaphragm, implying a greater degree of movement caused by respiratory acts. In addition, in cases in which the patient is positioned on his flank in order to ensure a better ultrasound window, the angle of attack on the lesion may be particularly sharp and the maneuver are less easy to be practically performed by the operator. Lastly, the proximity of this segment not only to the diaphragm but also to other organs (like the stomach) might lead to favor safety rather than a more aggressive ablation.
Local tumor progression was registered in 13.5% of our patients, a result in line with previous publications [22], but it wasn’t associated with any of the variables we analyzed.
The appearance of new HCC nodules at follow-up images, in a distant site in respect to the ablation site, was recorded in 27% patients (20/74). This rate is lower than others found in literature [22], but this is probably due to the difference in the mean follow-up time between studies. New distant HCC nodules were significantly associated with primary biliary cirrhosis. As pointed out by Jones et al. [27], HCC has a high incidence and is a rapid cause of death in male patients with stage III or IV PBC. This could imply that in this narrow cohort of patients a more aggressive treatment approach, such as OLT, should be considered in an earlier stage.
Interestingly, we didn’t find any significant association between outcome and subcapsular, perivascular or perihilar location of the target nodule. An absence of significant correlation between local tumor progression and subcapsular location of target HCC nodule is in line with the results reported by various authors, mostly for RFA [22, 28, 29], and with our previous experience [30], even though a correlation was reported in other studies [19, 31]. Zhang et al. concluded that local tumor progression is more frequent if lesions are in the proximity of major vessels [32] but other studies denied this relationship [33].
Both MWA and RFA may be considered safe and minimally invasive procedures, and are characterized by low overall complications rates, ranging from 10 to 30%. Moreover, the major complications rate is low in both procedures [21, 22, 34]. In this study, complications of any kind and grade, occurred at least once in 36/74 patients (48%) during follow-up. The complication rate we registered is relatively higher compared to what reported by other authors, and this is because we decided to consider as complications all cases of deviations from normality, even asymptomatic radiologic findings that could have been considered as paraphysiological sequelae by other authors. Examples are events as perihepatic fluid collection (15/74 patients; 20.2%), the creation of a non-hemodynamically significant AVF (7/74 cases; 9.4%), and segmental biliary ducts dilation (8/74 patients; 10.8%), which together represented a significant part of our total complication group. The rates of events universally considerable minor complications, which still didn’t require any special treatment, were lower: abdominal collection was registered in 3/74 cases (4%), duodenal walls edema in 2/74 cases (2.7%), and hemoperitoneum in 1 case (1.3%).
The occurrence of perihepatic free fluid after intervention was significantly associated with pre-procedural abnormal platelets count and with the presence of comorbidities of any type, while duodenal wall edema was significantly associated with primary tumor diameter, and portal vein thrombosis was significantly associated with Child Pugh score. Moreover, Fisher's Exact Test showed a significant association between the occurrence of portal vein thrombosis and abnormal values of albumin and platelet count before procedure.
Abnormal platelets count and comorbidities are entities that signify a worse hepatic function and a worse general condition of a patient, factors that may lead to develop more easily abdominal perihepatic free fluid after procedure, as a sign of temporary worsening of liver function.
Even though there was a statistically significant association between duodenal wall edema and primary tumor diameter, it is our opinion that the rarity of this complication in our population doesn’t leave safe space for any assumption.
Child Pugh score depends on the severity of cirrhosis, and the association between cirrhosis and portal vein thrombosis is well known. Cirrhotic patients having an odds ratio for venous thromboembolism of 1.7 in a recent meta-analysis [35], and the risk of developing portal vein thrombosis has been related to the severity of liver disease [36]. This not only explains the association of portal vein thrombosis to Child Pugh score, but also to abnormal values of albumin and platelets, which are an effect of a poor cirrhotic liver function. Among our population, a single major complication (duodenal perforation) occurred during follow-up, corresponding to a rate of 1.3%, which is in line with literature. No statistically significant association could be found for this event, given its rarity, in this study. The occurrence of complications of any kind and severity at least once during follow-up was significantly associated with multifocality of HCC liver disease at the time of intervention and abnormal pre-procedural INR/PT. This association is understandable cause both multifocality of disease and abnormal coagulation tests derive from a more advanced disease, which means a more compromised patient, in which any complication is more likely to occur. This study was aimed to investigate any significant association between several variables and the occurrence of complications and the outcome after intervention, but has several limitations including its retrospective nature, the small population number, and the follow-up, which may not be considered long. Moreover, no comparison was made with other treatments, like RFA. Larger studies are required to confirm or contradict our results. At the moment, we conclude that percutaneous US-guided MWA is a safe and effective treatment procedure in patients with small HCC nodules who are not suitable for surgical resection. Among the variables analyzed, only few significant associations were found in this study in relation to post-procedural complications and outcomes, but they may be kept in mind when planning the best treatment strategy for the patient.
Data availability
All data and materials as well as software application support the published claims and comply with field standards.
References
Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends—an update. Cancer Epidemiol Biomarkers Prev. 2016;25:16–27. https://doi.org/10.1158/1055-9965.EPI-15-0578.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011. https://doi.org/10.1002/hep.24199.
Jansen MC, van Hillegersberg R, Chamuleau RAFM, van Delden OM, Gouma DJ, van Gulik TM. Outcome of regional and local ablative therapies for hepatocellular carcinoma: a collective review. Eur J Surg Oncol. 2005. https://doi.org/10.1016/j.ejso.2004.10.011.
Tateishi R, Shiina S, Akahane M, Sato J, Kondo Y, Masuzaki R, et al. Frequency, risk factors and survival associated with an intrasubsegmental recurrence after radiofrequency ablation for hepatocellular carcinoma. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0059040.
Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999. https://doi.org/10.1148/radiology.210.3.r99fe40655.
Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology. 2008. https://doi.org/10.1002/hep.21933.
Chen MS, Li JQ, Zheng Y, Guo RP, Liang HH, Zhang YQ, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg. 2006. https://doi.org/10.1097/01.sla.0000201480.65519.b8.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018. https://doi.org/10.1016/S0140-6736(18)30010-2.
Ahmed M, Brace CL, Lee FT, Goldberg SN. Principles of and advances in percutaneous ablation. Radiology. 2011. https://doi.org/10.1148/radiol.10081634.
Carrafiello G, Laganà D, Mangini M, Fontana F, Dionigi G, Boni L, et al. Microwave tumors ablation: principles, clinical applications and review of preliminary experiences. Int J Surg. 2008. https://doi.org/10.1016/j.ijsu.2008.12.028.
Simon CJ, Dupuy DE, Mayo-Smith WW. Microwave ablation: principles and applications. Radiographics. 2005. https://doi.org/10.1148/rg.25si055501.
Bhardwaj N, Dormer J, Ahmad F, Strickland AD, Gravante G, West K, et al. Microwave ablation of the liver: a description of lesion evolution over time and an investigation of the heat sink effect. Pathology. 2011. https://doi.org/10.1097/PAT.0b013e32834c356c.
Dou JP, Yu J, Yang XH, Cheng ZG, Han ZY, Liu FY, et al. Outcomes of microwave ablation for hepatocellular carcinoma adjacent to large vessels: a propensity score analysis. Oncotarget. 2017. https://doi.org/10.18632/oncotarget.15672.
Correa-Gallego C, Fong Y, Gonen M, D’Angelica MI, Allen PJ, DeMatteo RP, et al. A retrospective comparison of microwave ablation vs. radiofrequency ablation for colorectal cancer hepatic metastases. Ann Surg Oncol. 2014. https://doi.org/10.1245/s10434-014-3817-0.
van Tilborg AAJM, Scheffer HJ, de Jong MC, Vroomen LGPH, Nielsen K, van Kuijk C, et al. MWA versus RFA for perivascular and peribiliary CRLM: a retrospective patient- and lesion-based analysis of two historical cohorts. Cardiovasc Intervent Radiol. 2016. https://doi.org/10.1007/s00270-016-1413-3.
Urbonas T, Anderson EM, Gordon-Weeks AN, Kabir SI, Soonawalla Z, Silva MA, et al. Factors predicting ablation site recurrence following percutaneous microwave ablation of colorectal hepatic metastases. HPB. 2019. https://doi.org/10.1016/j.hpb.2019.01.007.
Lee HY, Rhim H, Lee MW, Kim YS, Choi D, Park MJ, et al. Early diffuse recurrence of hepatocellular carcinoma after percutaneous radiofrequency ablation: analysis of risk factors. Eur Radiol. 2013. https://doi.org/10.1007/s00330-012-2561-8.
Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, et al. Image-guided tumorablation: standardization ofterminology and reporting criteria—a 10-year update. J Vasc Interv Radiol. 2014. https://doi.org/10.1016/j.jvir.2014.08.027.
Kono M, Inoue T, Kudo M, Chishina H, Arizumi T, Takita M, et al. Radiofrequency ablation for hepatocellular carcinoma measuring 2 cm or smaller: results and risk factors for local recurrence. Dig Dis. 2014. https://doi.org/10.1159/000367999.
Kikuchi L, Menezes M, Chagas AL, Tani CM, Alencar RSSM, Diniz MA, et al. Percutaneous radiofrequency ablation for early hepatocellular carcinoma: risk factors for survival. World J Gastroenterol. 2014. https://doi.org/10.3748/wjg.v20.i6.1585.
Kang TW, Lim HK, Lee MW, Kim YS, Rhim H, Lee WJ, et al. Aggressive intrasegmental recurrence of hepatocellular carcinoma after radiofrequency ablation: risk factors and clinical significance. Radiology. 2015. https://doi.org/10.1148/radiol.15141215.
Xu Y, Shen Q, Liu P, Xu Z, Wu P, Lu Z, et al. Microwave ablation for the treatment of hepatocellular carcinoma that met up-to-seven criteria: feasibility, local efficacy and long-term outcomes. Eur Radiol. 2017. https://doi.org/10.1007/s00330-017-4740-0.
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017. https://doi.org/10.1007/s00270-017-1703-4.
Kim YS, Rhim H, Cho OK, Koh BH, Kim Y. Intrahepatic recurrence after percutaneous radiofrequency ablation of hepatocellular carcinoma: analysis of the pattern and risk factors. Eur J Radiol. 2006. https://doi.org/10.1016/j.ejrad.2006.03.007.
Mulier S, Ni Y, Jamart J, Ruers T, Marchal G, Michel L. Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg. 2005. https://doi.org/10.1097/01.sla.0000171032.99149.fe.
Ganne-Carrié N, Nahon P. Hepatocellular carcinoma in the setting of alcohol-related liver disease. J Hepatol. 2019. https://doi.org/10.1016/j.jhep.2018.10.008.
Jones DEJ, Metcalf JV, Collier JD, Bassendine MF, James OFW. Hepatocellular carcinoma in primary biliary cirrhosis and its impact on outcomes. Hepatology. 1997. https://doi.org/10.1002/hep.510260508.
Teratani T, Yoshida H, Shiina S, Obi S, Sato S, Tateishi R, et al. Radiofrequency ablation for hepatocellular carcinoma in so-called high-risk locations. Hepatology. 2006. https://doi.org/10.1002/hep.21164.
Kang TW, Lim HK, Lee MW, Kim YS, Rhim H, Lee WJ, et al. Long-term therapeutic outcomes of radiofrequency ablation for subcapsular versus nonsubcapsular hepatocellular carcinoma: a propensity score matched study. Radiology. 2016. https://doi.org/10.1148/radiol.2016151243.
Ierardi AM, Giorlando F, Piacentino F, Fontana F, Novario R, Angileri SA, et al. Factors predicting outcomes of microwave ablation of small hepatocellular carcinoma. Radiol Medica. 2017. https://doi.org/10.1007/s11547-016-0694-6.
Yu J, Liang P, Yu XL, Cheng ZG, Han ZY, Mu MJ, et al. Local tumour progression after ultrasound-guided microwave ablation of liver malignancies: risk factors analysis of 2529 tumours. Eur Radiol. 2015. https://doi.org/10.1007/s00330-014-3483-4.
Zhang NN, Lu W, Cheng XJ, Liu JY, Zhou YH, Li F. High-powered microwave ablation of larger hepatocellular carcinoma: evaluation of recurrence rate and factors related to recurrence. Clin Radiol. 2015. https://doi.org/10.1016/j.crad.2015.06.092.
Kang TW, Lim HK, Lee MW, Kim YS, Choi D, Rhim H. Perivascular versus nonperivascular small HCC treated with percutaneous RF ablation: retrospective comparison of long-term therapeutic outcomes. Radiology. 2014. https://doi.org/10.1148/radiol.13130753.
Facciorusso A, Di Maso M, Muscatiello N. Microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma: a systematic review and meta-analysis. Int J Hyperth. 2016. https://doi.org/10.3109/02656736.2015.1127434.
Ambrosino P, Tarantino L, Di Minno G, Paternoster M, Graziano V, Petitto M, et al. The risk of venous thromboembolism in patients with cirrhosis: a systematic review and meta-analysis. Thromb Haemost. 2017. https://doi.org/10.1160/TH16-06-0450.
Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, et al. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004. https://doi.org/10.1016/j.jhep.2004.01.001.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by all authors. The manuscript was written by all authors, who also commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biondetti, P., Fumarola, E.M., Ierardi, A.M. et al. Percutaneous US-guided MWA of small liver HCC: predictors of outcome and risk factors for complications from a single center experience. Med Oncol 37, 39 (2020). https://doi.org/10.1007/s12032-020-01365-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-020-01365-x