Abstract
The CORRECT trial demonstrated survival benefits with regorafenib monotherapy in patients with treatment-refractory, metastatic colorectal cancer (mCRC). However, the trial’s stringent eligibility criteria for regorafenib may limit its external validity. We aimed to examine treatment attrition rates and eligibility for regorafenib in routine practice. We identified patients at the British Columbia Cancer Agency diagnosed with mCRC who demonstrated disease progression or intolerable toxicity on 2 or more lines of systemic therapy. During the study timeframe, panitumumab and cetuximab were only used in the chemo-refractory setting. Data on clinicopathologic variables and patient outcomes were ascertained and analyzed. Eligibility was determined using the CORRECT trial criteria. A total of 391 patients were identified, among whom only 39% were eligible for regorafenib: 35% in the panitumumab group and 51% in the cetuximab group. The main reasons for ineligibility in all patients were Eastern Cooperative Oncology Group Performance Status (ECOG PS) > 1 (69%), an elevated total bilirubin (21%), and thromboembolic events in the past 6 months (10%). No difference in eligibility for regorafenib was observed between patients previously receiving panitumumab or cetuximab (P = 0.914; 95% CI 0.550–1.951). Kaplan–Meier analyses showed that regorafenib-eligible compared to regorafenib-ineligible patients had an increased median overall survival of 5.3 versus 2.1 months, respectively (P < 0.001). However, Cox proportional hazard analyses showed that only ECOG PS rather than trial eligibility was correlated with outcomes. The strict eligibility criteria disqualify most patients with treatment-refractory mCRC for regorafenib therapy. Future trials should broaden the eligibility criteria to improve external validity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is the third most common malignancy and the fourth leading cause of cancer-related deaths worldwide [1]. The global burden of the disease was estimated to be close to 700,000 deaths in 2017, and it is projected to increase particularly among low- to middle-income countries [1, 2]. The majority of deaths are attributable to metastatic disease [3], for which options are largely limited to palliative systemic therapy. In these cases, standard treatment typically involves the sequential and concomitant use of systemic agents such as fluoropyrimidine, oxaliplatin, irinotecan, and bevacizumab [4]. Patients who progress on standard chemotherapy with KRAS wild-type tumors are also offered panitumumab and cetuximab which represent monoclonal antibodies against the epidermal growth factor receptor (EGFR) [4]. These anti-EGFR therapies confer a significant increase in progression-free survival and overall survival (OS) [5, 6]. However, factors affecting the choice between the two anti-EGFR regimens in the chemo-refractory metastatic colorectal cancer (mCRC) setting are unclear, given that both agents demonstrate similar OS benefits and toxicity profiles [7, 8]. Some studies suggest preferential use of panitumumab despite the proven non-inferiority of cetuximab [9], which may be related to its economic advantages [10, 11]. Importantly, few treatment options currently exist upon disease progression, even among patients who continue to have a good performance status.
The CORRECT trial renewed optimism by demonstrating significant survival benefits with regorafenib monotherapy in patients with mCRC in the treatment-refractory setting, thus offering an additional line of treatment [12]. Regorafenib is an oral multi-kinase inhibitor that targets receptors involved in the tumor microenvironment as well as oncogenesis and angiogenesis [13]. The CORRECT trial showed that patients with treatment-refractory mCRC in the regorafenib group compared to the placebo group had an increased median OS of 6.4 months versus 5.0 months, respectively (hazard ratio [HR] 0.77; P = 0.0052; 95% CI 0.64–0.94) [12]. Despite promising results, this drug has not been uniformly funded in countries with socialized or universal healthcare because the true clinical utility of the agent remains unclear to some payers. In particular, the applicability of the trial results to routine practice is uncertain as randomized clinical trials (RCTs) often employ strict eligibility criteria to improve internal validity at the expense of external validity [14].
Therefore, our study aimed to retrospectively apply the eligibility criteria of the CORRECT trial to a population-based cohort of KRAS wild-type patients with chemo-refractory mCRC to determine the degree to which the trial criteria restrict eligibility of real-world patients for therapy and to identify clinical characteristics and treatment patterns, specifically comparing panitumumab and cetuximab, that may guide the appropriate use of regorafenib in the routine clinical setting.
Materials and methods
Study setting
The British Columbia Cancer Agency (BCCA) is a cancer control program that serves over 4.7 million residents in the province. Yearly, it receives over 20,000 patient referrals for newly diagnosed cancer. It operates out of six regional facilities distributed across the province to provide residents with comprehensive and equitable access to cancer care. Each of the facilities offers a full range of quality cancer care services including diagnostic and functional imaging, ambulatory care clinics, inpatient units, chemotherapy administration, radiation facilities, surgical suites, pain and symptom management and palliative care, and oncology clinical trial programs. The BCCA research ethics board approved this study before its conduct. No consent from patients was required because this study was considered of minimal risk, given its retrospective design.
Study population
Patients aged 18 years and older who were diagnosed with mCRC between 2009 and 2014, and who were referred to a BCCA regional facility for treatment were considered. Patients must have received and demonstrated radiographic evidence of progression on or intolerable toxicity to standard systemic therapies, which include fluoropyrimidine, oxaliplatin, irinotecan, and bevacizumab. To determine if specific treatment with panitumumab or cetuximab impacts eligibility for regorafenib therapy, only patients with KRAS wild-type tumors who received either anti-EGFR regimen were included. At the time of the study, anti-EGFR agents were only approved for use in the third line or chemo-refractory setting.
Study design
The primary aim of the study was to determine and compare eligibility for regorafenib monotherapy in patients who have failed anti-EGFR therapies. Eligibility was defined by the inclusion and exclusion criteria as outlined in the CORRECT trial. Patients that fully met the following criteria were considered eligible: (1) histologically or cytologically confirmed metastatic colorectal adenocarcinoma; (2) Eastern Cooperative Oncology Group performance status (ECOG PS) ≤ 1; (3) adequate bone marrow, liver, and renal function; (4) no prior treatment with regorafenib; (5) no history of other major malignancies within the last 5 years; (6) no significant cardiac disease; (7) no history of arterial or venous thrombotic or embolic events in the last 6 months; (8) no ongoing, uncontrolled infection; (9) no symptomatic brain metastasis or meningeal tumors unless previously treated and clinically stable; (10) no seizure disorder requiring medical treatment; (11) no severe dehydration; (12) no symptomatic interstitial lung disease; (13) no mal-absorptive condition; (14) no history of organ allograft; and (15) no active wound, ulcer, or bone fracture. The secondary aim of the study was to measure overall survival from the date of the last treatment cycle received by the patient to the date of death from any cause.
To ascertain eligibility and OS, a retrospective chart review of patients with mCRC was conducted. Data on patient demographics, clinicopathologic variables, and patient outcomes were obtained from the BC Cancer Registry. This provincial database prospectively collects and houses clinical information on patients diagnosed with all gastrointestinal cancers, and who are referred to BCCA for care.
Statistical analysis
Baseline patient characteristics and eligibility were analyzed in the form of descriptive statistics. OS was estimated using the Kaplan–Meier method, and the log-rank test was used to measure differences in outcomes between the regorafenib-eligible and regorafenib-ineligible groups. Hazard ratios and 95% confidence intervals (CIs) were calculated using Cox proportional hazard models to identify predictors of survival. Analyses included the entire patient cohort, but they were also secondarily stratified into patients receiving either panitumumab or cetuximab to identify treatment-specific effects on eligibility and survival. Statistical significance was set at P < 0.05. All statistical analyses were performed using SPSS version 24.0.
Results
A total of 391 patients with treatment-refractory mCRC progressing on an anti-EGFR therapy were identified from the provincial database. All patients had KRAS wild-type tumors and received at least one cycle of an EGFR inhibitor: 298 patients received panitumumab and 93 patients received cetuximab. For the entire study cohort, the median age at diagnosis was 61 years (range 22–84), 247 (63%) were male, and 305 (78%) were Caucasian. Further, 237 (61%) had a primary tumor located in the colon, and all of the primary tumors were histologically confirmed adenocarcinoma. The patients’ burden of disease at diagnosis was high: 267 (68%) had regional lymph node involvement and 225 (58%) had distant metastasis. The most common sites of metastasis were the liver (66%), lungs (21%), and intra-abdominal lymph nodes (6%). Regarding treatment, 291 (74%) patients previously received 5 or more systemic therapy agents. Panitumumab or cetuximab (100%), fluoropyrimidine (99%), and irinotecan (97%) were the most frequently prescribed treatments.
Comparing anti-EGFR treatment groups, patients who received panitumumab had a statistically significant increase in age (P < 0.001) and the presence of distant metastasis (P = 0.024) at diagnosis. There was also a difference in ECOG PS (P = 0.011), with a greater proportion of patients treated with panitumumab having poorer performance relative to the cetuximab group. The remaining clinical characteristics were found to be similar between the two treatment groups. Other baseline patient characteristics and treatment-stratified analyses are summarized in Table 1.
Applying the eligibility criteria of the CORRECT trial to our study cohort, a total of 153 (39%) patients were eligible for regorafenib monotherapy: 106 (35%) in the panitumumab group and 47 (51%) in the cetuximab group (Fig. 1a). Logistic regression analysis controlling for covariates, such as age at diagnosis, presence of distant metastasis, and ECOG PS, indicated that the difference in eligibility between panitumumab- and cetuximab-treated patients was not statistically significant (P = 0.914; 95% CI 0.550–1.951). The top reasons rendering ineligibility in all patients were ECOG PS > 1 (69%), total bilirubin > 1.5 × upper limit of normal (ULN) (21%), arterial or venous thrombotic or embolic event in the past 6 months (10%), and AST > 2 × ULN (9%). Treatment-stratified analyses of reasons for ineligibility are summarized in Fig. 1b.
a Of the 391 patients, a total of 153 patients were considered eligible for regorafenib: 106 in the panitumumab group and 47 in the cetuximab group. b Main reasons for regorafenib eligibility were ECOG PS > 1, total bilirubin > 1.5 × ULN, AST > 2 × ULN, and thrombotic or embolic events in the past 6 months
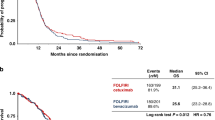
Interestingly, Kaplan–Meier survival analysis showed that trial eligibility alone predicted far better patient outcomes. Patients who were eligible for regorafenib had an increased median OS compared to ineligible patients (5.3 vs 2.1 months; P < 0.001) (Fig. 2a). However, after accounting for covariates in our Cox proportional hazard model, only ECOG PS ≤ 1, rather than trial eligibility, predicted better patient outcomes (Fig. 2b). The cumulative hazard of all patients with an ECOG PS ≤ 1 versus an ECOG PS > 1 was 0.53 (P = 0.001; 95% CI 0.370–0.767) (Fig. 2c). Further stratifying the analysis to compare individual ECOG PS levels, patients with a poor ECOG PS (3 or 4) had a statistically significant increase in cumulative hazard compared to patients with good (0 or 1) and moderate (2) ECOG PS. However, no difference in survival was observed between patients with ECOG PS 0 and 1 (HR 1.395; P = 0.150; 95% CI 0.887–2.195), and ECOG PS 1 and 2 (HR 1.406; P = 0.103; 95% CI 0.933–2.119) (Fig. 2d). Comparing the treatment groups, no difference in survival was observed between patients treated with panitumumab and cetuximab (3.3 vs 3.3 months; P = 0.303) (not shown).
a Median OS of all patients from the last treatment cycle to death from any cause is 5.3 and 2.1 months in the regorafenib-eligible and regorafenib-ineligible groups, respectively (P < 0.001). Cox regression analysis of the cumulative hazard of all patients, b who were eligible versus ineligible for regorafenib for whom the value was 0.97 (P = 0.871; 95% CI 0.666–1.412), c those with an ECOG PS ≤ 1 versus > 1 for whom the value was 0.53 (P = 0.001; 95% CI 0.370–0.767), and d patients with a higher ECOG PS level had a statistically significant cumulative hazard compared to patients with good and moderate PS. However, no difference was observed in patients with ECOG PS 0 and 1 (HR 1.395; P = 0.150; 95% CI 0.887–2.195), and ECOG PS 1 and 2 (HR 1.406, P = 0.103; 95% CI 0.933–2.119)
Discussion
CORRECT was a phase III RCT that demonstrated the efficacy of regorafenib monotherapy in the setting of treatment-refractory mCRC [12]. Because RCTs tend to use strict eligibility criteria to improve internal validity at the expense of external validity [14], many payers of socialized or universal healthcare systems are neither comfortable nor quick to adopt emerging therapies, such as regorafenib, due to uncertainties about their true applicability to real-world patients [15]. Consequently, it is important to determine if RCT results remain valid in routine clinical practice to help inform drug funding decisions. Our study aimed to evaluate the CORRECT trial’s external validity by retrospectively applying its eligibility criteria to a population-based cohort of patients with treatment-refractory mCRC. Specifically, our interest focused on patients with KRAS wild-type tumors who have progressed on an anti-EGFR therapy. To our knowledge, few factors are known to guide the choice between the two anti-EGFR regimens. Identifying potential differences in the eligibility for subsequent treatments based on receipt of panitumumab or cetuximab may inform overall decision making.
Our study determined that the majority of patients (61%) were not eligible to receive regorafenib had it been available during the study timeframe. This suggests that regorafenib cannot be offered to a large proportion of patients due to the stringent inclusion and exclusion criteria, and that the results of the CORRECT trial may not be fully generalizable. This may explain why continued uncertainty exists regarding its funding in some jurisdictions. The most commonly cited reason for ineligibility in all patients was ECOG PS > 1. Interestingly, studies have shown that the assessment of patient performance status is often subject to bias and interobserver variability [16]. To this end, if the ECOG PS criteria were broadened to include patients with a moderate PS of 2, the external validity of the trial would be improved. In our cohort, for instance, refining the ECOG PS cut-off to 2 would result in an absolute increase in eligibility by 23%. It should be noted, however, that our study cohort largely consisted of patients with heavily pretreated metastatic disease. This may potentially account for a poorer average performance status and explain why a higher ECOG PS cut-off of 2 would significantly increase eligibility.
Furthermore, in our study cohort, simply being eligible for regorafenib therapy was correlated with better patient outcomes. This suggests that patients with prognostically unfavorable disease were likely excluded from the CORRECT trial, which further underscores the importance of finding additional treatment options for regorafenib-ineligible patients. After controlling for ECOG PS, trial eligibility no longer significantly correlated with an increased median OS. Instead, meeting the criterion of ECOG PS ≤ 1 became a key and independent predictor of increased survival.
Comparing the treatment groups, no significant difference was observed in the median OS between the panitumumab and cetuximab groups. This is expected and consistent with previous studies that showed both anti-EGFR therapies produced similar safety profiles and survival benefits [7]. It should, however, be noted that this study was not designed to be a head-to-head comparison of the biological therapies, and that the survival analyses between the two therapies in this study should be considered with caution.
The results of this study should be interpreted in the context of its limitations. This study is retrospective in design and assesses eligibility for regorafenib therapy at only one point in time. In reality, a patient’s eligibility status can change over time depending on an unpredictable disease trajectory. Additionally, it is assumed that eligibility alone determines the use or non-use of regorafenib, and that all patients who are eligible will initiate therapy. This is an oversimplification of a complex process. In practice, treatment decisions are made by accounting for additional patient and physician factors.
In summary, the majority of patients in our study cohort with treatment-refractory mCRC who have progressed on an anti-EGFR therapy were not candidates for regorafenib monotherapy as defined by the CORRECT eligibility criteria. Additionally, treatment with either anti-EGFR regimen did not yield a difference in eligibility for the agent. Using less restrictive eligibility criteria that include patients with moderate performance status while maintaining patient safety should be considered in order to enhance the external validity of future trials.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2016;66:683–691.
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER cancer statistics review, 1975–2014, National Cancer Institute, Bethesda; 2014.
Wolpin BM, Mayer RJ. Systemic treatment of colorectal cancer. Gastroenterology. 2008;134(5):1296–310.
Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ, Juan T, Sikorski R, Suggs S, Radinsky R, Patterson SD. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(10):1626–34.
Karapetis CS, Khambata-Ford S, Jonker DJ, O’callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359(17):1757–65.
Price TJ, Peeters M, Kim TW, Li J, Cascinu S, Ruff P, Suresh AS, Thomas A, Tjulandin S, Zhang K, Murugappan S. Panitumumab versus cetuximab in patients with chemotherapy-refractory wild-type KRAS exon 2 metastatic colorectal cancer (ASPECCT): a randomised, multicentre, open-label, non-inferiority phase 3 study. Lancet Oncol. 2014;15(6):569–79.
Fakih M, Vincent M. Adverse events associated with anti-EGFR therapies for the treatment of metastatic colorectal cancer. Curr Oncol. 2010;17(Suppl 1):18.
Kennecke HF, Chen L, Blanke CD, Cheung WY, Schaff K, Speers C. Panitumumab (Pmab) versus cetuximab (Cmab)/irinotecan (Iri) therapy among patients with KRAS wild-type (wt) metastatic colorectal cancer (MCRC). J Clin Oncol. 2012;30:640.
Pettigrew M, Kavan P, Surprenant L, Lim HJ. Comparative net cost impact of the utilization of panitumumab versus cetuximab for the treatment of patients with metastatic colorectal cancer in Canada. J Med Econ. 2016;19(2):145–57.
Graham CN, Maglinte GA, Schwartzberg LS, Price TJ, Knox HN, Hechmati G, Hjelmgren J, Barber B, Fakih MG. Economic analysis of panitumumab compared with cetuximab in patients with wild-type KRAS metastatic colorectal cancer that progressed after standard chemotherapy. Clin Ther. 2016;30(6):1376–91.
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, Humblet Y, Bouché O, Mineur L, Barone C, Adenis A. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. The Lancet. 2013;381(9863):303–12.
Wilhelm SM, Dumas J, Adnane L, Lynch M, Carter CA, Schütz G, Thierauch KH, Zopf D. Regorafenib (BAY 73-4506): a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int J Cancer. 2011;129(1):245–55.
Rothwell PM. Factors that can affect the external validity of randomised controlled trials. PLOS Clin Trial. 2006;19(1):e9.
Mason AR, Drummond MF. Public funding of new cancer drugs: is NICE getting nastier?. Eur J Cancer. 2009;45(7):1188–92.
Sørensen JB, Klee M, Palshof T, Hansen HH. Performance status assessment in cancer patients. An inter-observer variability study. Br J Cancer. 1993;67(4):773–5.
Funding
The research was supported financially by the Mach-Gaensslen Foundation of Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval
Ethics approval was obtained from the BCCA Research Ethics Board. Being a retrospective study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Angeles, A., Hung, W. & Cheung, W.Y. Eligibility of real-world patients with chemo-refractory, K-RAS wild-type, metastatic colorectal cancer for palliative intent regorafenib monotherapy. Med Oncol 35, 114 (2018). https://doi.org/10.1007/s12032-018-1176-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-018-1176-6