Abstract
Dendritic cells (DCs)-based tumor vaccines have shown to be the promising methods for inducing therapeutic antitumor response. However, DCs alone rarely carry curative antitumor activity, and the immunosuppressive microenvironment may contribute to this defect of DC vaccinal function. Irradiation in combination with DCs has been shown to promote immune-mediated tumor destruction in preclinical studies. However, little is known about how irradiation alters the tumor microenvironment, and what host pathways modulate the activity of administrated DCs. In this study, BALB/c mice and the 4T1 breast cancer cell line were used in a tumor-bearing model. The tumor-bearing mice were irradiated locally up to 10 Gy for 3 consecutive days or a single dose of 30 Gy using a cesium source. Studies of dynamic change of the tumor microenvironment in irradiated versus untreated tumors revealed that there was no obvious change on IL-10, IL-6 and TGF-β expression or production, whereas increased TNF-α level within the first 2 weeks of irradiation. The increased TNF-α level is exactly right timing window for DCs injection, corresponding to the significant elevation of intratumoral CD8+ T infiltration and the regression of tumor size. With attention to scheduling, combination X-ray with DCs i.t. injection may offer a practical strategy to improve treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiotherapy is one of the most important methods against cancer. Accumulating data show that high energy X-ray radiotherapy involves antitumor immunity. X-ray can enhance the immunogenicity of tumor cells by releasing the “dangerous signals,” such as HMGB-1 and hsp70 [1, 2], and by up-regulates the expression of adhesion molecules, such as VCAM-1 and ICAM-1 [3, 4]. So, it has become clear that irradiation can already render tumors and their microenvironment more immunogenic [5]. Furthermore, irradiation can up-regulate cell death receptors in tumor cells such as Fas/CD95 and MHC-I, which can trigger tumor cell apoptosis or MHC-1-mediated immunity [6, 7]. Thus, radiotherapy not only causes the destruction of signaling molecules, but also plays important role in regulation of antitumor immunity of our body. However, in a clinical setting immune responses elicited by radiation alone result in little protective immunity, as local relapse occurs often [8, 9]. Lately, increasing evidence demonstrates that cancer immunotherapy and its synergy with radiotherapy could have a good prospect [10–12].
DCs-based immunotherapy against tumors has been studied [13–17]. Intratumorally, injection of DCs alone induces little curative antitumor effects as the immunosuppressive tumor microenvironment compromises DCs functions. The manipulation of the tumor microenvironment is necessary to potentiate the effect of DCs immunity [17, 18]. Studies have shown that persistent antitumor memory by combining radiotherapy and DCs injection could be obtained [19, 20]. Tumor locally irradiation could enhance the ability of DCs to capture tumor antigens, migrate to the draining lymph node and present processed antigens to T cells [21]. However, little is known about the mechanisms, by which irradiation alter the tumor microenvironment, and the host pathways that modulate the activity of administrated DCs. The activation of T cells by DCs can only be achieved in the presence of inflammatory or “dangerous signals.” It has been reported that certain solid tumors could release proinflammatory cytokines, such as IL-6, IL-17, IL-1β and TNF-α, when expose to ionizing radiation [22]. Several inflammatory cytokines are considered to be key factors that lead to tumor recurrence and metastasis in radiotherapy [23–25], and these cytokines alone or combined with irradiated tumor cells could promote injected DCs maturation and induce stimuli critical for eliciting effective antigen presentation [26, 27]. Additionally, these inflammatory mediators also increase the permeability of the local vasculature that leads to the recruitment of circulating lymphocytes, including antigen-presenting cells and effector T cells into surrounding tissues. In this study, we aimed to investigate the mechanisms of the synergic effect of irradiation and DCs administration in treatment of tumors.
Here, we report that irradiation modulates an inflammatory microenvironment within tumors and the exactly right timing window for DCs injection after local irradiation.
Materials and methods
Mice and tumor cell line
BALB/c and C57BL/6 mice (6–8 week old) were purchased from Animal Center of Hebei Medical University. The mice were housed under specific pathogen-free conditions in the central animal facility of Hebei Medical University. All animal procedures were approved and performed in accordance with the animal guidelines of the Animal Care and Use Committee of Hebei Medical University. 4T1 cell line was purchased from American Type Culture Collection (Manassas, VA) and maintained according to the recommendations of the supplier.
Irradiation
4T1 cell line or tumor-bearing mice were irradiated with a linear accelerator (Elekta Synergy) at dose rate of 2.78 Gy/min according to the normal source-skin distance (SSD) method [28].
Generation of bone marrow-derived DCs and in vitro antigen pulsing
The differentiation of DCs from BABL/c mice bone marrow was induced by incubation with IL-4 (10 ng/ml, peproTech) and GM-CSF (10 ng/ml, peproTech) for 5 days. On day 6, cultured DCs were loaded with X-ray (30 Gy) irradiated 4T1 tumor cells lysate at the concentration of 50 μg/ml/106 for 18 h. Then DCs were treated with PBS or LPS (100 ng/ml, E. coli 0127: B8, Sigma-Aldrich) for another 36 h for maturation.
Tumor challenge and treatment
4T1 cells (1 × 105 in 0.1 ml of serum-free RPMI 1640) were subcutaneously inoculated into the right flank of BALB/c mice. Seven days later, the mice were randomly divided into 6 groups. Untreated group, 10 Gy × 3 group (10 Gy X-ray was locally applied on tumor daily for 3 consecutive days), 30 Gy group (single dose of 30 Gy irradiation on day 7), 10 Gy × 3 + DC group (after 48 h of final irradiation, DCs were injected intratumorally at the dosage of 1 × 106/mouse/100 μl), 30 Gy + DC group. One week later, the mice received another DCs injection. Tumor size was measured with a caliper, and tumor volume was calculated using the formula (A × B 2)/2, where A is the larger and B the shorter of the two measurements.
Isolation of tumor-infiltrating T lymphocytes
Tumor-infiltrating lymphocytes (TIL) were isolated from tumor tissues with a method described previously and modified slightly [29]. Tumors were dissected by removing surrounding normal tissue, weighted, minced into ~1-mm pieces, digested with an enzymatic solution containing 0.2 mg/ml DNase, 850 U/ml collagenase type II in supplement-free RPMI 1640 at 37 °C for 45 min, then passed through a 40-μm filter and washed several times. The cells then were suspended in serum-free RPMI 1640 and were overlaid with 75–100% Ficoll and centrifuged for 20 min at 2000g. Leukocytes were collected from the interphase, washed, counted, and then the CD3+ T cells were sorted with the method of magnetic separation (CD3ε MicroBead Kit, mouse, Miltenyi Biotec.)
Fluorescence-activated cell sorting (FACS) analysis
For surface marker analysis, DCs were incubated with anti-CD11c-FITC (BD Pharmingen, clone: G235-2356), PE-conjugated anti-CD86, ICAM-1 (BD Pharmingen, clone: R35-95,clone:3E2), and MHC II (eBioscience) and subjected for FACS analysis using a Becton–Dickinson FACScan (San Jose, CA). For the analysis of IFN-γ, CD127 and CD44 expression in CD8+ T, activated Ag-specific T cells were labeled with anti-IFN-γ-FITC (clone Pharmingen), anti-CD127-FITC and anti-CD44-FITC (eBioscience), anti-CD8-PE (Pharmingen). For Treg cells detection, anti-CD4-FITC (Pharmingen) and anti-CD25-PE (Pharmingen) were used. All the cell labeling methods were referred to our previous work [29].
Real-time reverse transcription PCR (qRT-PCR)
Total RNA was extracted from aliquots of 106 tumor-infiltrating leukocytes using TRIzol (Invitrogen Life Technologies, Carlsbad, CA) according to the manufacturer’s instructions. Primers for CXCL16 (5′ CCTTGTCTCTTGCGTTCTTCC 3′ forward and 5′ TCCAAAGTACCCTGCGGTATC 3′ reverse) and for CXCR6 (5′CCCTGTACTTTATGCCTTTG3′ forward and 5′ CTTGGAACTGTCCTCAGAAG3′ reverse) were synthesized by Invitrogen for qRT-PCR analysis. Data were analyzed using the 2−ΔΔCT method.
Cytokine detection by ELISA
To quantify the levels of IL-6, TGF-β, IL-10 and TNF-α from tumors, 500-milligram tumors were homogenized in 0.5 ml PBS containing protease inhibitors (Sigma). For T cells IFN-γ release assay, splenic T cells (2 × 106) were cultured with DCs pulsed with irradiated or nonirradiated 4T1 lysates in 24-well culture plates at various ratios. After 48 h, supernatants were collected and quantified for IFN-γ content. The amount of cytokines was determined using ELISA kit (BD Pharmingen, San Diego, CA).
CTL assays
Splenic lymphocytes or tumor-infiltrating lymphocytes from treated or nontreated tumor-bearing mice were stimulated with irradiated 4T1 lysate (50 μg/ml) and 20 ng/ml IL-2 for 5 days. The CTL responses of splenic lymphocytes were measured using a standard colorimetric assay (CytoTox 96, Non-Radioactive Cytotoxicity Assay, Promega, USA), according to the method described previously [22]. Percentage of lysis was calculated as (experimental release − spontaneous release)/(maximum release − spontaneous release) × 100.
In vivo neutralization experiments
4T1 tumor-bearing mice were treated with indicated irradiation doses (as described in “Tumor challenge and treatment”). Two days after irradiation, animals were treated with intravenous injection of anti-TNF-α antibody (20 μg/mouse, 500-P64, peprotech, USA) or PBS and then intratumoral injection of DCs as mentioned in “Fluorescence-activated cell sorting (FACS) analysis.”
Statistical analysis
For statistical analysis, we used Student’s t test or X 2 test, and a 95% confidence limit was considered to be significant, defined as P < 0.05. Results are typically presented as mean ± SD of data from four to five mice.
Results
DCs pulsed by X-ray radiated 4T1 extracts enhance T cell antigen presentation in vitro
To examine whether irradiation has an effect on tumor cells, and subsequently stimulate DCs capacity in promoting T cell antigen presentation, we pulsed wild-type mice bone marrow DCs with or without irradiated 4T1 breast tumor cell lysate. The results show that 30 Gy X-ray irradiated 4T1 lysate (50 μg/ml) alone had no detectable effect on day 5 DCs MHC II, CD86 and ICAM-1 expression (data not shown); however, subsequent LPS matured DCs had increased IL-12p70 expression (Supplementary Fig. 1). We also observed an increased secretion of IFN-γ from irradiated 4T1-lysate-pulsed DCs and increased allogenic T cell proliferation compared to that of nonirradiated 4T1 lysate and PBS-pulsed DCs (Supplementary Fig. 1).
Local irradiation improves intratumorally DC vaccination therapy for tumor in vivo
Since the DCs pulsed by X-ray irradiated 4T1 extract showed an enhanced immunity in vitro, we next aimed to examine whether tumor irradiation therapy improve DC vaccination in vivo. Mice were subcutaneously inoculated 1 × 105 4T1 tumor cells; seven days later (the size of tumor was about 210 mm3), the tumors were X-ray irradiated and followed by DC vaccination intratumorally at day 2 or day 9. Figure 1a outlines the treatment schema, and Fig. 1b shows the tumor growth curve. The results show that all untreated and DCs only treated mice died at week 7; however, 20–40% of mice treated with X-ray irradiation followed by DC vaccination survived beyond 15 weeks with tumors size less than 300 mm3 (Fig. 1c).
Irradiation only or combined with DCs significantly slowed tumor growth in vivo. a Groups of six mice each were implanted 4T1 in the right flank as describe in Materials and Methods, and the tumor diameters were measured on a regular basis. Mice were then treated with a dose of 10 Gy for 3 consecutive days on days 7, 8, 9 or a single dose of 30 Gy on day 9 after tumor implantation. Then tumor lysate-pulsed DCs intratumorally injected on days 11 and 18. b Statistical analysis comparing tumor growth on days 10–35 was done using the ANOVA test (*P < 0.05). c Statistical analysis comparing tumor-bearing mice percent survival at 14 weeks after tumor inoculation was done using the Log-rank (Mantel–Cox) test (**P < 0.01)
Irradiation-induced tumor cell TNF-α is essential to the antitumor immunity of DCs
Next, we examined the cytokines expression in tumors. In consistent with the in vitro observation, X-ray irradiation had little effect on the expression of IL-10, IL-6 in tumors (data not shown). However, TNF-α level in irradiated tumors markedly increased and TGF-β markedly decreased from day 2 to day 11 post irradiation, thereafter the TNF-α or TGF-β level was back to the control level at day 21 (Fig. 2). To verify the crucial role of TNF-α in the irradiation-mediated DC antitumor immunity, we injected anti-TNF-α through tail vein prior to intratumorally injected DCs. The ELISA showed TNF-α level in the irradiated tumor beds was decreased following anti-TNF-α neutralization antibody injection (Fig. 3a). Figure 3b shows that administration of anti-TNF-α abolished the antitumor immunity of DCs. Our results showed that the increased TNF-α at the first 2 weeks after radiation is important for DCs playing an effective antitumor immunity.
TNF-α and TGF-β level within the tumor mass 2 and 11 days after irradiation. 4T1 tumor-bearing mice subjected to treatment with irradiation of a dose of 10 Gy for 3 consecutive days on days 7, 8, 9 or a single dose of 30 Gy on day 9 after tumor implantation. Control groups of mice received no treatment. After 2, 11 and 21 days of irradiation, tumor tissues were harvested and weighted. Then the tumors were prepared homogenate to analyze TGF-β (a) and TNF-α (b) production with ELISA. Data are reported as the average relative expression or concentration of cytokine (pg) per gram tumor tissue ±SE of triplicate samples. *P < 0.05, **P < 0.01 versus untreated group
Inhibition of TNF-α abolished the depressed tumor growth caused by irradiation combined with DCs injection. The antitumor effect was relieved by treatment with a-TNF-α neutralizing antibody (a). TNF-α neutralizing antibody inoculation decreased TNF-α level of tumors (b). Data are reported as the average relative expression or concentration of cytokine (pg) per gram tumor tissue ±SE of triplicate samples. **P < 0.01 versus untreated group
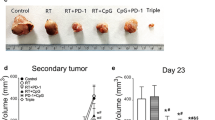
Treatment with irradiation followed DCs injection induces sustained and systemic immunity in mice
To investigate whether the mice treated with X-ray radiation followed DCs administration establish a systemic antitumor immunity, we rechallenged the mice with no or small measureable tumors at week 10 by a second injection of 1 × 105 4T1 tumor cells to the left flank 2 cm away from the original tumors. We observed ~60% of rechallenged mice were resistant to tumor cell rechallenge and survived for 10 weeks, whereas all-control mice with single inoculated of tumor cells appeared recurrence after one week of tumor inoculation and all died of tumors within 6 weeks (Fig. 4a). Splenocytes from these survived mice showed a higher cytolysis activity to target tumor cells (Fig. 4b). In addition, the CD8+ T cells from rechallenged mice showed a higher level of CD127 and IFN-γ expression compared to that CD8+ T cells from naive mice (Fig. 4c, d).
Long-lasting and systemic immunity was occurred when mice treated with irradiation combined with i.t. DCs injection. a–d To assay the efficacy of radiation therapy and DC vaccine combinatorial therapy, a a lethal dose 5 × 105 4T1 cells was inoculated (subcutaneously) into naive mice or mice cured by combinatorial therapy 10 weeks after initial tumor inoculation on the opposite flank. Mice were monitored weekly for the appearance of tumors. All naive tumor-bearing mice died between weeks 3 and 4. b Bulk splenocytes were prepared 3 weeks after the rechallenge experiment described in (a) and restimulated in vitro with 4T1 lysate. Subsequently, splenocytes (effector) were incubated for 4 h with the 4T1 tumor cells at indicated effector: target ratios, and cytotoxic T lymphocyte (CTL) activity was determined by a standard colorimetric assay. As negative control, splenocytes from naive mice were assayed for CTL activity against the 4T1 tumor cells. Data are representative of two independent experiments (three per group). c The splenic cells from rechallenge mice for 3 weeks were stimulated with 4T1 lysate for 18 h; then interferon (IFN)-γ-producing, CD127 and CD44-expressing CD8+ T cells were detected. One representative experiment of three independent experiments is shown. d Statistical analysis comparing IFN-γ production or CD127 and CD44 expression on CD8+ T cell at 3 weeks after tumor inoculation was done using the ANOVA test, (*P < 0.05, **P < 0.01; three per group). Each bar represents the mean standard deviation of tumor samples from three independent experiments
Together, these results indicate that a persistent, systemic antitumor immunity that was established in mice cured by therapy combining intratumoral DC vaccine injection and X-irradiation.
Irradiation followed by DC vaccination promotes the effector T cells accumulation, increases the ratio of CD8+ T/Treg and tumor-specific CTL activity within tumors
Next, we were interested in whether the induced sustained systemic antitumor immunity affects the trafficking of effector T cells into solid tumors. We performed real-time PCR to observe a dynamic mRNA expression of CXCL16 (a chemokine released by tumor cells or stromal cells and could recruit CD8+ T cell) and CXCR6, the ligand for CXCL16, in tumor-derived lymphocytes. At the first 11 days after irradiation, CXCL16 or CXCR6 mRNAs expression was higher to a various extent than that of control, whereas no substantial differences were observed on the expression of CXCL16 and CXCR6 at day 21 after irradiation or following TNF-α neutralization at day 11 after irradiation (Fig. 5). These results indicate that there is an optimal time window of inducing proinflammatory microenvironment after irradiation that is favorable for the infiltration and the antitumor capacity of tumor-specific cytotoxic T cells.
Tumor irradiation increases CXCL16 and CXCR6 mRNAs expression. Irradiation changed the expression of CXCL16 in tumors or CXCR6 in immune infiltrates of tumors. Mice were inoculated s.c. in right flank with 4T1 tumor cells on day 0. Tumors were locally irradiated on days 7 to 9 at the dose of 10 Gy or at a single dose of 30 Gy, respectively. TNF-α neutralizing antibody was injected via tail vein 2 days later. Tumors were harvested and weighed on days 4, 11 and 21 after final irradiation. Data are reported as the relative expression ±SE of four mice per group. This experiment was repeated two times with similar results (*P < 0.05, **P < 0.01)
Further, we analyzed the tumor-infiltrated cell types by FACS and observed a dramatic increase of CD8+ T but not Treg lymphocytes after irradiation regardless of DCs administration (Fig. 6a–d). The ratio of CD8/Treg was significantly increased after combination treatment of irradiation and DCs injection (P < 0.01, Fig. 6e). Tumor-infiltrating cytotoxic T cells showed a higher cytolysis on 4T1 tumor cells as well as irradiated 4T1 (Fig. 6f).
Characterization of the immune infiltrates within irradiated, DCs injected or treated with irradiation combined with i.t. DCs injection versus untreated s.c. 4T1 tumors. Mice were inoculated s.c. in right flank with 4T1 tumor cells on day 0. Tumor-bearing mice were treated with local irradiation only, DCs injection only, irradiation (10 Gy × 3 or 30 Gy) combined with DCs injection, respectively. Tumors were harvested and weighed on day 19 after final irradiation. Then tumors described in “Materials and methods” were mechanically disaggregated to single cell suspensions, stained for CD4 and CD25 or CD8 and analyzed by flow cytometry (a, c). The data are presented as number of CD8+ T cells × 106 per gram tumor for each individual tumor (b). The data are presented as number of CD4+ CD25+ T cells × 105 per gram tumor for each individual tumor (d). The data are shown as the ratio of CD8+ T cells to CD4+ CD25+ T cells (e). Data represent cumulative results of two experiments. Lysis activity of tumor infiltrates against 4T1 or irradiated 4T1 in vitro. Tumor infiltrates were obtained as described in “Materials and methods,” then were incubated for 4 h with 4T1 tumor cells or 4T1 irradiated with 30 Gy at effector: target ratio of 100:1. The cytotoxic T lymphocyte (CTL) activity was determined by a standard colorimetric assay (f). Data are representative of two independent experiments (three mice per group). The differences of treated versus PBS are statistically significant (**P < 0.01; *P < 0.05)
Taken together, our results indicate that combination of irradiation and DCs treatment enhances the infiltration and activation of tumor-specific CD8+ T cells and facilitates tumor regression.
Discussion
DC-based tumor vaccines have shown to be one of the promising methods for inducing therapeutic antitumor response. However, DCs alone rarely cause curative antitumor effects, and this has been attributed to various factors including the existence of an immunosuppressive microenvironment within solid tumors. Current studies suggest that a variety of soluble factors and cell types in the tumor microenvironment not only influences endogenous DCs infiltrating the tumors, but also moderates the dialogue between DCs and naive T cells [30]. Therefore, exploration of novel strategies aiming to reverse the derepressed microenvironment and subsequently to enhance the potency of DC-based vaccine is pertinent.
It has been reported that irradiated tumor cells are good source of antigens for DC uptake and presentation [31]. Irradiation-induced tumor cell releasing HMGB1 and HSP70 that could active DCs by binding TLR4 [32, 33]. In this report, we demonstrate that X-ray radiated enhances DC vaccination capacity by activating more naive T cells both in vitro and in vivo. Consequently, X-ray combined DCs obviously inhibited the growth of tumors in vivo and prolonged the survival time of tumor-bearing mice (Fig. 1).
Induction of a proinflammatory microenvironment within solid tumors has been shown to augment DCs function by providing maturation stimuli important for cross-priming rather than cross-tolerance [30]. It had been demonstrated that combination of irradiation and anti-PD-L1 antibody therapies achieved effective tumor control by enhancing CTLs effector functions, which, in turn, negatively regulates the accumulation of MDSCs (myeloid-derived suppressor cells) through TNF signaling [34]. In this study, we showed that local irradiation combined with DCs administration results in a decreased TGF-β and an increased TNF-α level within the irradiated tumor bed (Fig. 2, 3a). Reducing the TNF-α level with anti-TNF-α neutralizing antibody could significantly dull the combined treatment of advantage (Fig. 3b). In addition, the high levels of CD127 and IFN-γ expression on CD8+ T cells from rechallenged mice showed long-lasting and systemic immunity in combined treatment mice had established (Fig. 4). Consequently, our data showed that a high TNF-α level time window was essential for DCs activity to give play to antitumor effect.
Recently, Filatenkov et al. demonstrated that CD8+ T cell infusion after irradiation could significantly improve tumor-bearing mice survival [35, 36]. CXCL16 has been shown to induce strong chemotaxis of activated CD8 T cells, which express high levels of CXCR6 [28]. In this report, we observed that irradiation strikingly up-regulates CXCL16/CXCR6 expression on tumor cells or tumor-infiltrated leukocytes (Fig. 5). This finding is in accordance with the recruitment of CD8+ T in irradiated tumor mass (Fig. 6a, b). Bos et al. [37] reported that transient regulatory T cell ablation could enhance radiotherapy. The behavior of the Treg cells was different from that of the CD8+ T cells during irradiation, since their number was not substantially decreased by radiation, suggesting that Treg cells may represent more radioresistant lymphocytes (Fig. 6c, d). Although irradiation could not decrease the numbers of regulatory T cell, the inhibitory effect maybe weakened with higher ratio of CD8+ T and Treg, as well as higher CTL lysis activity against 4T1 or irradiated 4T1in tumor microenvironment (Fig. 6e, f).
Together, our findings demonstrate that intratumoral DCs injection within 2 weeks of irradiation is critical for fully activating their antitumor effect and implicate a novel strategy for cancer treatment.
References
Schmid TE, Multhoff G. Radiation-induced stress proteins-the role of heat shock proteins (HSP) in anti-tumorresponses. Curr Med Chem. 2012;19:1765–70.
Pasi F, Paolini A, Nano R, Di Liberto R, Capelli E. Effects of single or combined treatments with radiation and chemotherapy on survival and danger signals expression in glioblastoma cell lines. Bio Med Res. 2014;2014:453–97.
Handschel J, Prott FJ, Sunderkötter C, Metze D, Meyer U, et al. Irradiation induces increase of adhesion molecules and accumulation of beta2-integrin-expressing cells in humans. Int J Radiat Oncol Biol Phys. 1999;45:475–81.
Lugade AA, Sorensen EW, Gerber SA, Moran JP, Frelinger JG, et al. Radiation-induced IFN-gamma production within the tumor microenvironment influences antitumor immunity. J Immunol. 2008;180:3132–9.
Frey B, Rubner Y, Kulzer L, Werthmoller N, Weiss EM, et al. Antitumor immune responses induced by ionizing irradiation and further immune stimulation. Cancer Immunol Immunother. 2014;63:29–36.
Friedman EJ. Immune modulation by ionizing radiation and its implications for cancer immunotherapy. Curr Pharm Des. 2002;8:1765–80.
Garnett CT, Palena C, Chakraborty M, Tsang KY, Schlom J, et al. Sublethal irradiation of human tumor cells modulates phenotype resulting in enhanced killing by cytotoxic T lymphocytes. Cancer Res. 2004;64:7985–94.
Mantel F, Flentje M, Guckenberger M. Stereotactic body radiation therapy in there-irradiation situation-a review. Radiat Oncol. 2013;8:7–20.
Hodge JW, Ardiani A, Farsaci B, Kwilas AR, Gameiro SR. The tipping point for combination therapy: cancer vaccines with radiation, chemotherapy, or targeted small molecule inhibitors. Semin Oncol. 2012;39:323–39.
Serre R, Benzekry S, Padovani L, Meille C, Andre N, et al. Mathematical modeling of cancer immunotherapy and its synergy with radiotherapy. Cancer Res. 2016;76(17):4931–40.
Morris ZS, Guy EI, Francis DM, Gressett MM, Werner LR, et al. In situ tumor vaccination by combining local radiation and tumor-specific antibody or immunocytokine treatments. Cancer Res. 2016;76(13):3929–41.
Derer A, Frey B, Fietkau R, Gaipl US. Immune-modulating properties of ionizing radiation: rationale for the treatment of cancer by combination radiotherapy and immune checkpoint inhibitors. Cancer Immunol Immunother. 2016;65(7):779–86.
Radford KJ, Tullett KM, Lahoud MH. Dendritic cells and cancer immunotherapy. Curr Opin Immunol. 2014;27:26–32.
Baek S, Lee SJ, Kim MJ, Lee H. Dendritic cell (DC) vaccine in mouse lung cancer minimal residual model; comparison of monocyte-derived DC vs. hematopoietic stem cell derived-DC. Immune Netw. 2012;12:269–76.
Van Lint S, Wilgenhof S, Heirman C, Corthals J, Breckpot K, et al. Optimized dendritic cell-based immunotherapy for melanoma: the TriMix-formula. Cancer Immunol Immunother. 2014;63:959–67.
Wimmers F, Schreibelt G, Sköld AE, Figdor CG, De Vries IJ, et al. Paradigm shift in dendritic cell-based immunotherapy: from in vitro generated monocyte-derived DCs to naturally circulating DC subsets. Front Immunol. 2014;11:165–77.
Hunn MK, Bauer E, Wood CE, Gasser O, Dzhelali M, et al. Dendritic cell vaccination combined with temozolomide retreatment: results of a phase I trial in patients with recurrent glioblastoma multiforme. J Neurooncol. 2015;21:319–29.
Rossowska J, Pajtasz-Piasecka E, Anger N, Wojas-Turek J, Kicielińska J, et al. Cyclophosphamide and IL-12-transduced DCs enhance the antitumor activity of tumor antigen-stimulated DCs and reduce Tregs and MDSCs number. J Immunother. 2014;37:427–39.
Byun JW, Lee HS, Song SU, Lee SW, Kim SK, et al. Combined treatment of murine fibrosarcoma with chemotherapy (Paclitaxel), radiotherapy, and intratumoral injection of dendritic cells. Ann Dermatol. 2014;26:53–60.
Lugade AA, Sorensen EW, Gerber SA, Moran JP, Frelinger JG, et al. Radiation-induced IFN-γ production within the tumor microenvironment influences antitumor immunity. J Immunol. 2008;180:3132–9.
Teitz-Tennenbaum S, Li Q, Okuyama R, Davis MA, Sun R, et al. Mechanisms involved in radiation enhancement of intratumoral dendritic cell therapy. J Immunother. 2008;31:345–58.
Ao X, Zhao L, Davis MA, Lubman DM, Lawrence TS, et al. Radiation produces differential changes in cytokine profiles in radiation lung fibrosis sensitive and resistant mice. J Hematol Oncol. 2009;2:6–18.
Lee EJ, Park HJ, Lee IJ, Kim WW, Ha SJ, et al. Inhibition of IL-17A suppresses enhanced-tumor growth in low dose pre-irradiated tumor beds. PLoS ONE. 2014;9:e106423.
Demaria S, Bhardwaj N, McBride WH, Formenti SC. Combining radiotherapy and immunotherapy: a revived partnership. Int J Radiat Oncol Biol Phys. 2005;63:655–66.
Barker HE, Paget JT, Khan AA, Harrington KJ. The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nat Rev Cancer. 2015;15(7):409–25.
Strauss L, Bergmann C, Szczepanski M, Gooding W, Johnson JT, et al. A unique subset of CD4+ CD25highFoxp3+ T cells secreting interleukin-10 and transforming growth factor-β1 mediates suppression in the tumor microenvironment. Clin Cancer Res. 2007;13:4345–54.
Ahn E, Kim H, Han KT, Sin JI. A loss of antitumor therapeutic activity of CEA DNA vaccines is associated with the lack of tumor cells’ antigen presentation to Ag-specific CTLs in a colon cancer model. Cancer Lett. 2015;356:676–85.
Matsumura S, Wang B, Kawashima N, Braunstein S, Badura M, et al. Radiation-induced CXCL16 release by breast cancer cells attracts effector T cells. J Immunol. 2008;181:3099–107.
Song S, Wang Y, Wang J, Lian W, Liu S, et al. Tumour-derived IL-10 within tumour microenvironment represses the antitumour immunity of Socs 1-silenced and sustained antigen expressing DCs. Eur J Cancer. 2012;48:2252–9.
Lin A, Schildknecht A, Nguyen LT, Ohashi PS. Dendritic cells integrate signals from the tumor microenvironment to modulate immunity and tumor growth. Immunol Lett. 2010;127:77–84.
Larsson M, Fonteneau JF, Bhardwaj N. Dendritic cells resurrect antigens from dead cells. Trends Immunol. 2001;22:141–8.
Saenz R, Futalan D, Leutenez L, Eekhout F, Fecteau JF, et al. TLR4-dependent activation of dendritic cells by an HMGB1-derived peptide adjuvant. J Transl Med. 2014;12:211.
Chen T, Guo J, Han C, Yang M, Cao X. Heat shock protein 70, released from heat-stressed tumor cells, initiates antitumor immunity by inducing tumor cell chemokine production and activating dendritic cells via TLR4 pathway. J Immunol. 2009;182:1449–59.
Deng L, Liang H, Burnette B, Beckett M, Darga T, et al. Irradiation and anti–PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest. 2014;124:687–95.
Filatenkov A, Baker J, Müller AM, Ahn GO, Kohrt H, et al. Treatment of 4T1 Metastatic Breast cancer with combined hypofractionated irradiation and autologous T-cell infusion. Radiat Res. 2014;182:163–9.
Balermpas P, Rödel F, Weiss C, Rödel C, Fokas E. Tumor-infiltrating lymphocytes favor the response to chemoradiotherapy of head and neck cancer. Oncoimmunology. 2014;3:e27403.
Bos PD, Plitas G, Rudra D, Lee SY, Rudensky AY. Transient regulatory T cell ablation deters oncogene-driven breast cancer and enhances radiotherapy. J Exp Med. 2013;210:2435–46.
Acknowledgements
This work was supported by a grant from the National Natural Science Foundation of China (81071710). We are grateful to Xuehui Yang for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shuxia Song has received research grants from the National Natural Science Foundation of China (81071710). Authors declare that they have no conflict of interest.
Ethical approval
The mice were housed under specific pathogen-free conditions in the central animal facility of Hebei Medical University. All animal procedures were approved and performed in accordance with the animal guidelines of the Animal Care and Use Committee of Hebei Medical University.
Additional information
Lijia Chang and Zhengzheng Zhang have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. 1
Irradiated 4T1 lysate pulsed DCs had advantage on antigen presentation. (A) Irradiated 4T1-lysate could not enhance DCs to secrete IL-12. (B) Naïve splenic cells were stimulated in vitro by irradiated versus non-irradiated 4T1 lysate pulsed-DCs at various ratios. In control samples containing splenic cells alone, DCs alone, and splenic cells co-cultured with unpulsed-DCs no IFN-γ secretion were detected. Data are reported as the average concentration of IFNγ (pg/ml) per 1×106 responders per 48 h ± SE of triplicate samples. *, P<0.05 (TIFF 100 kb)
Rights and permissions
About this article
Cite this article
Chang, L., Zhang, Z., Chen, F. et al. Irradiation enhances dendritic cell potential antitumor activity by inducing tumor cell expressing TNF-α. Med Oncol 34, 44 (2017). https://doi.org/10.1007/s12032-016-0864-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-016-0864-3