Abstract
The health-related quality of life (HRQL) is generally accepted as an important parameter for patients undergoing oncologic surgery. We conducted this prospective, randomized study to compare the effect of narrow gastric tube (NGT) reconstruction and whole-stomach (WS) reconstruction on the long-term HRQL in patients after esophagectomy. One hundred and four patients undergoing esophagectomy were enrolled in our study from 2007 to 2008, with 52 in NGT group and 52 in WS group. A questionnaire with reference to the European Organization for Research and Treatment of Cancer QLQ-C30 and QLQ-OES18 was used to assess the HRQL at 3 weeks, 6 months, 1, 2, 3, 4, and 5 years after esophagectomy. Data collection and follow-up were performed regularly. No significant difference was found between NGT group and WS group in the patients’ baseline characteristics. Patients in NGT group had decreased risk of postoperative reflux esophagitis by comparison with those in WS group. The 5-year cumulative survival rate was 42 % (NGT) and 27 % (WS), respectively. Compared with WS group, a significant increased survival rate (P = 0.027) was found in NGT group. Additionally, patients had lower dysphagia scores (better) in NGT group than those in WS group at 5 years after esophagectomy (P < 0.05). However, the scores of the other scales did not show statistical difference at 5-year follow-up. NGT is a better option for the reconstruction after esophagectomy because of decreased risk of postoperative complication, increased survival rate, and better HRQL, and NGT should be preferred to be recommended for patients undergoing esophagectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer ranks the sixth most common cause of cancer death worldwide. Even after surgery, the overall survival is only 42 % at 5 years [1]. The surgical trauma associated with an esophagectomy for esophageal cancer is perhaps the greatest among all general thoracic surgical operations. In such a disease with high incidence of postoperative complications, survival alone may not be able to adequately describe the outcome. More attention has been paid to patients’ health-related quality of life (HRQL). HRQL is generally accepted as an additional outcome parameter in patients undergoing oncologic surgery, especially for patients with a comparatively poor prognosis. Esophagectomy severely impacts on physical, emotional, and social health and has highly negative consequences for the patient’s HRQL [2–5].
The method of narrow gastric tube (NGT) reconstruction was first proposed by Akiyama in 1972 [6]. It has been widely applied nowadays and contributes to about 90 % of all procedures of esophagectomy worldwide [7]. Currently, both the NGT and whole stomach (WS) are utilized for esophagectomy. Theoretically, the WS interferes with physiological structure of the patient which seriously affects the postoperative quality of life. Surgeons have performed such operations with NGT gradually owing to the advantages of quicker recovery, less complications, and probably better HRQL. There are quite a few studies in the literature investigating the application of NGT reconstruction [8, 9]. Because of a small sample size and lack of randomized comparison, results of these studies require further investigation. Our previous study compared the methods of NGT and WS reconstruction after esophagectomy and concluded that patients with NGT reconstruction have lower rate of complications, quicker recovery, and better HRQL. However, the follow-up was short and the long-term result still remains unclear. The present study is to compare the effect of NGT and WS reconstruction on survival rate and HRQL at 5 years after esophagectomy.
Patients and methods
Patient enrollment
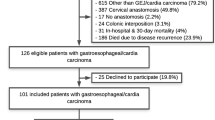
Participants in this study included 104 of 112 patients, 81 men and 23 women (median age 60.09 years; age range 44–74 years) who underwent surgery for esophageal cancer at the Department of Thoracic Surgery, the First Affiliated Hospital of Chongqing Medical University (Chongqing, China), between 2007 and 2008. The patients were evaluated by esophagography, esophagoscopy, bronchoscopy, computed tomography (CT), and positron emission tomography (PET). Patients with tumors infiltrating into adjacent organs or with distant metastases were excluded from this study. Patients who received either preoperative radiotherapy or chemotherapy before operations were also excluded. All patients were randomized into two groups by opaque envelop method: a narrow gastric tube reconstruction, NGT group (n = 52), and a whole-stomach reconstruction, WS group (n = 52). The demographic information of the two groups is listed in Table 1.
Surgery
All operations followed the principles of radical resection of esophagus. The lesser curvature of the stomach was resected, and gastric tube was reconstructed from the distal aspect of the lesser curvature by applying linear staplers. Gastric conduit (3–4 cm in diameter) was constructed based on the preservation of gastroepiploic vessels of the greater curvature of the stomach. For patients with tumor located in the upper one-third of the esophagus, the tubular stomach was pulled upward to the left cervical part through the posterior mediastinal route and hand-sewn two-layer anastomosis was performed. For patients with tumor located in the lower two-thirds of the esophagus, a stapled intrathoracic anastomosis was performed. For patients in WS group, whole stomach was used. The dissection and handling of the stomach and esophagus were consistent with that of the NGT group. A pyloroplasty was done routinely. The postoperative chemotherapy with docetaxel and cisplatin was provided to all patients.
HRQL assessment
A questionnaire with reference to the EORTC QLQ-C30 and the QLQ-OES18 was designed, and participants were required to complete the questionnaire at regular intervals after surgery (3 weeks, 6 months, 1, 2, 3, 4, and 5 years). The EORTC QLQ-C30 core questionnaire incorporates five functional scales, a global health scale, and three symptom scales, each containing between two and five items [9]. The revised scales of the QLQ-OES18 were correlated with scales in the QLQ-C30 to examine the relationship between the disease-specific symptoms and generic aspects of QOL. All scale and item scores are linearly transformed such that scales range from 0 to 100. In the functional scales, a high score is equivalent to better function, whereas in the symptom scales and single items, a high score means more symptoms.
Statistical analyses
The statistical software program SPSS was used for all statistical analyses. Nominal data were calculated with the Chi-square test. Tests of differences between groups were performed using unpaired t tests. A P value of <0.05 was regarded as statistically significant.
Results
Baseline characteristics
One hundred and four patients (81 males and 23 females) were included, and 103 were followed until death or the end of the study period. The follow-up rate was 99 %. The average age was 60.09 ± 6.78 years. There were no differences in patient and cancer characteristics between the two groups [10].
Postoperative complications and hospital mortality
Postoperative reflux esophagitis were significantly more frequent in WS group (n = 3, 5.8 %) than in NGT group (n = 11, 21.2 %) (P = 0.04). For other items, differences were not significant (P > 0.05) (Table 2). All patients in NGT group recovered with no operative death. In WS group, one patient died of ulcerative hemorrhage and another died of pneumonia. There was no local recurrence of tumor in both groups.
Overall survival
During the follow-up period of 5 years, 70 of the 104 patients died (33 in NGT group and 37 in WS group). The overall survival at 5 years was 36 %. The 5-year survival of patients in the NGT group was 42 % and of patients in the WS group was 27 % (P = 0.027) (Fig. 1). Patients in NGT group achieved a significantly better 5-year survival.
HRQL investigation
Questionnaires were sent to patients at 3 weeks, 6 months, 1, 2, 3, 4, and 5 years after surgery. Patients in NGT group had significantly less reflux than those in WS group at 3 weeks, 6 months, and 1 year. However, this difference fades out during the observation period of 4 and 5 years. For the nausea, difference was not significant at 3 weeks, 6 months, 1, and 5 years, with exception at 2, 3, and 4 years. For the dysphagia, difference was significant at 6 months; this difference resolved during the observation period of 2–4 years but reoccurred at 5 years (P = 0.02) (Fig. 2). All the 25 items are listed in Table 3.
Discussion
Despite its association with a significant risk of morbidity, esophagectomy is the only established curative treatment option for esophageal cancer. Currently, 5-year survival after esophagectomy for cancer is 30–45 % [11]. More than half of the operated patients will develop functional disorders after surgery [12], generally reflux, dysphagia, and intrathoracic stomach syndrome. These problems play an important role in the recovery after surgery, identified as a negative factor for long-term survival and quality of life [13, 14].
The procedure of isoperistaltic narrow gastric tube reconstruction was proposed by Akiyama in 1972 [6] and is nowadays routinely applied by 90 % of European, 80 % of Asian, and 79 % of North American surgeons [7]. The following are advantages of tubular stomach we analyzed: (1) After tubulization, the stomach is usually long enough (30–35 cm) to be pulled up to the neck, which can decrease the tension in the site of anastomosis [15]. (2) The acid secretion is suppressed because of the truncal vagotomy and degradation of gastric mucosal blood supply [16]. (3) Gastric tube is laid in posterior mediastinum. There is no room for expansion so that the interference with the heart and lung is less. (4) The diameter of gastric tube and esophagus is similar. It is equivalent to the normal physiological channel and can decrease the thoracic gastric retention [17]. A recent meta-analysis reviewed most of the available studies on gastric function after esophagectomy in the literature and concluded that the gastric tube reconstruction compared with whole stomach is more preferred because of less reflux, delayed gastric emptying, intrathoracic stomach syndrome, and better quality of life [18].
However, there were no studies in the literature comparing methods of reconstruction with regard to survival, which is another important indicator for patients undergoing oncologic surgery. Previously, studies [10, 19] have paid attention to this point but failed to reveal any significant difference on survival between groups at 1 and 2 years of follow-up. As the follow-up goes by, we proved for the first time in the literature that narrow gastric tube is superior to whole-stomach reconstruction after oncologic esophagectomy in view of better survival (P = 0.027) at 5-year follow-up. The following are reasons we inferred: (1) Survival diminished markedly with increasing number of regional lymph nodes positive for cancer [1]. Tubulization of the stomach makes it easier to skeletonize the lesser curvature for lymph node clearance. (2) There are more patients with cancer located in lower third and cardia in NGT group (28 vs. 21, Table 1). It is reported that survival improves as the tumor location moves distally in the esophagus [1]. (3) The application of immunohistochemical staining has markedly improved the sensitivity of micrometastatic disease than the routine hematoxylin and eosin staining alone [20]. The clinical significance of micrometastases in patients with esophageal cancer has been proved. Narrow gastric tube allows a wider resection of the stomach, and more R0 resection without micrometastases could be expected. Survival is reported to decrease with the resection margin status, particularly from R0 to either R1 or R2 [1].
Results of HRQL questionnaire showed that patients with NGT reconstruction presented significantly less symptom of dysphagia. This is a coincidence with the previous study [21], which explained that the persistent digestive tract symptoms may severely impact the postoperative HRQL. Dysphagia is the most often-cited symptom associated with an anastomotic stricture. The recurrence of dysphagia defeats one of the main aims of surgery: to restore normal swallow function to improve the patient’s quality of life. Interestingly, difference of dysphagia occurred only twice during the follow-up period: 6 months and 5 years after surgery. We speculated that it indicates the two different mechanisms of stricture: a benign stricture related to reflux, ischemia, or inflammation (6 months after surgery) [22] and a malignant stricture of endoluminal or locoregional tumor recurrence (5 years after surgery) [23]. After tubulization, the tension in the site of anastomosis decreased, which can enhance the vascularization in the site of anastomosis and facilitate the healing process [24]. Acid secretion is also suppressed because of the truncal vagotomy and degradation of gastric mucosal blood supply. The symptom of reflux is therefore significantly less severe at 3 weeks, 6 months, and 1 year in NGT group (Table 3). This contributes to less benign stricture in NGT group early after surgery (6 months after surgery). As years go by, problems related to functional disorders do not significantly impair long-term quality of life, which is mainly influenced by tumor recurrence. Dysphagia related to malignant process of endoluminal or locoregional tumor recurrence becomes patients’ primary complaint. Patients in NGT group have a significantly better survival at 5 years after surgery, which is correlated with their less severe symptoms of dysphagia.
In conclusion, this prospective randomized study indicates that NGT may be a better alternative choice for the reconstruction after esophagectomy in view of decreased risk of postoperative complication, increased survival rate, and better HRQL. This surgical technique merits wider application and greater refinement.
References
Rice T, Rush V, Apperson Hansen C, et al. Worldwide esophageal cancer collaboration. Dis Esophagus. 2009;22(1):1–8.
McLarty AJ, Deschamps C, Trastek VF, et al. Esophageal resection for cancer of the esophagus: long-term function and quality of life. Ann Thorac Surg. 1997;63(6):1568–72.
Schmidt CE, Bestmann B, Kuchler T, et al. Quality of life associated with surgery for esophageal cancer: differences between collar and intrathoracic anastomoses. World J Surg. 2004;28(4):355–60.
Blazeby JM, Farndon JR, Donovan J, Alderson D. A prospective longitudinal study examining the quality of life of patients with esophageal carcinoma. Cancer. 2000;88(8):1781–7.
Brooks JA, Kesler KA, Johnson CS, et al. Prospective analysis of quality of life after surgical resection for esophageal cancer: preliminary results. J Surg Oncol. 2002;81(4):185–94.
Lauschke H, Tolba R, Hirner A. History of surgical esophageal replacement. Chirurg. 2001;72(8):973–7.
Judith B, Daan PL, Sjoerd GE, et al. International servery on esophageal cancer: part I surgical techniques. Dis Esophagus. 2009;22:195–202.
Akiyama H, Miyazono H, Tsurumaru M, et al. Use of the stomach as an esophageal substitute. Ann Surg. 1978;188(5):606–10.
Yamamoto S, Makuuchi H, Shimada H, et al. Clinical analysis of reflux esophagitis following esophagectomy with gastric tube reconstruction. J Gastroenterol. 2007;42(5):342–5.
Zhang C, Wu QC, Hou PY, et al. Impact of the method of reconstruction after oncologic oesophagectomy on quality of life–a prospective, randomised study. Eur J Cardiothorac Surg. 2011;39:109–14.
Collard JM, Otte JB, Reynaert M, Kestens PJ. Quality of life three years or more after esophagectomy for cancer. J Thorac Cardiovasc Surg. 1992;104:391–4.
Koichiro S, Satoshi I, Masafumi S, et al. Chest pain and ST segment depression caused by expansion of gastric tube used for esophageal reconstruction. Intern Med. 2005;44(3):217–21.
Tetsuya T, Terunal A, Takao S, et al. Marked reversible ST-T abnormalities induced by cardiac compression from a retrosternal gastric tube used to reconstruct the esophagus after tumor resection. Int Heart J. 2006;47(3):475–82.
Walther B, Johansson J, Johnsson F, et al. Cervical or thoracic anastomosis after esophageal resection and gastric tube reconstruction: a prospective randomized trial comparing sutured neck anastomosis with stapled intrathoracic anastomosis. Ann Surg. 2003;238(6):803–12.
Bonavina L, Anselmino M, Ruol A, et al. Functional evaluation of the intrathoracic stomach as an oesophageal substitute. Br J Surg. 1992;79:529–32.
Domergue J, Veyrac M, Huin-Yan S, et al. pH monitoring for 24 hours of gastroesophageal reflux and gastric function after intrathoracic gastroplasty after esophagectomy. Surg Gynecol Obstet. 1990;171:107–10.
Gutschow C, Collard JM, Romagnoli R, Salizzoni M, Holscher A. Denervated stomach as an esophageal substitute recovers intraluminal acidity with time. Ann Surg. 2001;233:509–14.
Poghosyan T, Gaujoux S, Chirica M, et al. Functional disorders and quality of life after esophagectomy and gastric tube reconstruction for cancer. J Visc Surg. 2011;148(5):e327–35.
Zhang M, Wu QC, Li Q, et al. Comparison of the health-related quality of life in patients with narrow gastric tube and whole stomach reconstruction after oncologic esophagectomy: a prospective randomized study. Scand J Surg. 2013;102(2):77–82.
Takeuchi H, Kawakubo H, Saikawa Y, Omori T, Kitagawa Y. Clinical significance of micrometastases in patients with esophageal cancer. Nihon Geka Gakkai Zasshi. 2013;114(1):9–12.
Egberts JH, Schniewind B, Bestmann B, et al. Impact of the site of anastomosis after oncologic esophagectomy on quality of life: a prospective, longitudinal outcome study. Ann Surg Oncol. 2008;15(2):566–75.
van Heijl M, Gooszen JA, Fockens P, et al. Risk factors for development of benign cervical strictures after esophagectomy. Ann Surg. 2010;251:1064–9.
Sutcliffe RP, Forshaw MJ, Tandon R, et al. Anastomotic strictures and delayed gastric emptying after esophagectomy: incidence, risk factors and management. Dis Esophagus. 2008;21:712–7.
Blazeby JM, Conroy T, Hammerlid E, et al. Clinical and psychometric validation of an EORTC questionnaire module, the EORTC QLQ-OES18, to assess quality of life in patients with oesophageal cancer. Eur J Cancer. 2003;39(10):1384–94.
Acknowledgments
We are grateful for all the help or support given to us.
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical standard
All procedures in the study were performed in accordance with ethical standards of our institutional according to ethical standard of Declaration of Helsinki 1964. Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Min Zhang and Qiang Li have equally contributed to this work
Rights and permissions
About this article
Cite this article
Zhang, M., Li, Q., Tie, HT. et al. Methods of reconstruction after esophagectomy on long-term health-related quality of life: a prospective, randomized study of 5-year follow-up. Med Oncol 32, 122 (2015). https://doi.org/10.1007/s12032-015-0568-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-015-0568-0