Abstract
Oxidative stress plays a critical role in neuronal injury and is associated with various neurological diseases. Here, we explored the potential protective effect of neuroserpin against oxidative stress in primary cultured hippocampal neurons. Our results show that neuroserpin inhibits H2O2-induced neurotoxicity in hippocampal cultures as measured by WST, LDH release, and TUNEL assays. We found that neuroserpin enhanced the activation of AKT in cultures subjected to oxidative stress and that the AKT inhibitor Ly294002 blocked this neuroprotective effect. Neuroserpin increased the expression of the anti-apoptotic protein BCL-2 and blocked the activation of caspase-3. Neuroserpin did not increase the level of neuroprotection over levels seen in neurons transduced with a BCL-2 expression vector, and an inhibitor of Trk receptors, K252a, did not block neuroserpin’s effect. Taken together, our study demonstrates that neuroserpin protects against oxidative stress-induced dysfunction and death of primary cultured hippocampal neurons through the AKT-BCL-2 signaling pathway through a mechanism that does not involve the Trk receptors and leads to inhibition of caspase-3 activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroserpin was first discovered as a secreted protein from axons of dorsal root ganglia (Stoeckli et al. 1989). It was later found that neuroserpin was expressed in the central nervous system (Hastings et al. 1997; Osterwalder et al. 1996), detected from an early stage in neuronal development of the mouse (E10), increasing to a maximal level perinatally before declining to a moderate level in the adult (Krueger et al. 1997). Biochemical evidence showed that neuroserpin strongly inhibits the serine protease tissue plasminogen activator (tPA) (Hastings et al. 1997; Osterwalder et al. 1998). It is a less effective inhibitor of urokinase plasminogen activator, trypsin, and NGF-γ and acts predominantly as a substrate for plasmin (Hastings et al. 1997; Osterwalder et al. 1998). The expression pattern of neuroserpin is largely similar to tPA supporting a role for neuroserpin to regulate the activity of tPA in physiological and pathological situations (Lee et al. 2015; Miranda and Lomas 2006; Robinson et al. 2015). Consistent with this view, neuroserpin has been proposed to regulate tPA levels and modulate neuronal migration (Krueger et al. 1997), neurite growth (Hill et al. 2000; Navarro-Yubero et al. 2004; Parmar et al. 2002), synaptogenesis (Borges et al. 2010), and synaptic plasticity in the adult brain (Berger et al. 1999; Madani et al. 2003; Wannier-Morino et al. 2003). However, some effects of neuroserpin have been reported to be independent of inhibition of tPA (Lee et al. 2008; Madani et al. 2003; Wu et al. 2010).
Neuroserpin can reduce N-methyl-d-aspartate (NMDA)-mediated excitotoxicity and ischemia-induced plasmin-mediated cell death in in vivo and primary neuronal culture models (Lebeurrier et al. 2005; Wu et al. 2010). Administration of recombinant neuroserpin into the brain reduced infarct size by about 60 % in a rat middle cerebral artery occlusion model of cerebral ischemia, while cleaved neuroserpin lacking tPA inhibitory activity had no effect (Yepes et al. 2000). In addition to ischemic death, neuroserpin administration has been found to reduce lesion size following excitotoxic insult with NMDA in mice (Lebeurrier et al. 2005). Neuroserpin is elevated in the cerebrospinal fluid of patients with Alzheimer’s disease (AD) (Fabbro and Seeds 2009; Nielsen et al. 2007). Neuroserpin forms a complex with amyloid beta (Aβ) peptides to reduce the aggregation of the peptides and attenuates the Aβ toxicity in cell culture (Kinghorn et al. 2006). Furthermore, Aβ42 injected into the brains of mice is cleared more rapidly in neuroserpin-deficient mice than in wild-type mice, and the knockout of the neuroserpin gene leads to decreased Aβ40 and Aβ42 levels, fewer and smaller amyloid plaques, and reduced memory deficits, in a mouse model of the disease (Fabbro et al. 2011). Consistent with the hypothesis that inhibition of tPA by neuroserpin underlies these changes, there was a greater level of tPA accumulation in the plaques of the neuroserpin knockout mice. Hence neuroserpin has been recognized as a potential regulator in the pathogenesis of AD.
Oxidative stress is a condition in which the balance between production of reactive oxygen species (ROS) and level of antioxidants is significantly disturbed and results in damage to cells by ROS (Gandhi and Abramov 2012). The generation of excessive ROS and oxidative damage is believed to be involved in the pathogenesis of neurodegenerative disorders including AD, Parkinson’s disease (PD), and Huntington’s disease (HD) (Melo et al. 2011). ROS mediates neurotoxicity in each of these diseases through modification of hallmark proteins by oxidation (Li et al. 2013). In AD, extracellular deposits of Aβ and intracellular neurofibrillary tangles are two major hallmark proteins. It has been reported that oxidative stress also stimulates the production of Aβ probably through increased expression and activation of beta- and gamma-secretase, two enzymes critical for the production of Aβ (Radi et al. 2014). In fact, oxidative damage precedes Aβ deposition which further contributes to oxidative stress and neurodegeneration in AD brains and transgenic mouse models of AD (Butterfield and Boyd-Kimball 2004). In PD, post-translational modifications of alpha-synuclein by ROS have been implicated in increasing the aggregation and toxicity of alpha-synuclein (Li et al. 2013), while anti-oxidants were found to inhibit its aggregation (Radi et al. 2014). Thus, oxidative stress is a promising therapeutic target for treating neurodegenerative diseases.
In this study, we have investigated the neuroprotective role and mechanism of action of neuroserpin using a model of induced oxidative stress. We demonstrate for the first time that recombinant neuroserpin acts extracellularly to protect against hydrogen peroxide-induced neurotoxicity through the AKT signaling pathway in a primary hippocampal culture model. We further show that neuroserpin rescued the dysfunction caused by oxidative stress by modulating the expression of the mitochondria apoptotic pathway proteins BCL-2 and caspase-3.
Materials and Methods
Reagents
Ly294002 was purchased from Cell Signaling Technology (Danvers, Massachusetts, USA). Recombinant rat neuroserpin (residues 19–410) was cloned into pET28a (Novagen, Merck Limited, Auckland, New Zealand), adding an N-terminal 6·His-tag and thrombin tag removal cleavage site. Recombinant neuroserpin was produced in Escherichia coli BL21(DE3) pRIL cells (Stratagene, La Jolla, CA, USA) at 18 °C and purified by Ni-NTA affinity chromatography, anion-exchange chromatography (UNO Q1; Bio-Rad Laboratories, Hercules, CA, USA), and gel filtration (Superdex 75 HR 10/30; Pharmacia, GE Healthcare Life Sciences, Auckland, New Zealand). Adenovirus expressing β-galactosidase (LacZ) and BCL-2 were purchased from Vector Biolabs (Malvern, PA, USA). Monoclonal rabbit anti-cleaved active caspase-3 antibody (1:3000), monoclonal mouse anti-p-AKT antibody (1:3000), polyclonal rabbit anti-β-actin antibody (1:10,000), polyclonal rabbit anti-t-AKT antibody (1:5000), and polyclonal rabbit anti-BCL-2 antibody (1:3000) were from Cell Signaling Technology and used at the dilutions shown in brackets. Trk receptor family inhibitor, K252a (Sigma, St. Louis, MO, USA), was used at the concentration of 100 nM.
Animals
Pregnant rats (Sprague Dawley) were purchased from Taconic Farms, Inc., Derwood, MD. All animals were given food and water ad libitum in a humidity- and temperature-controlled room under a 12-h light/dark cycle. All animal procedures were approved by the Animal Care and Use Committee, NICHD, NIH.
Primary Neuronal Culture
Embryonic day 18 (E18) hippocampal neuronal cultures were prepared as described previously (Qin et al. 2014). Briefly, the hippocampus was dissected and digested with 2 mg/ml papain in 2 ml for 30 min at 37 °C and the papain then inactivated with 10 % FBS (3 ml). The digest was triturated to dissociate the tissue and then passed through a cell strainer to remove any intact tissue clumps. The cells were then centrifuged for 5 min at 1500×g and the supernatant discarded. The cell pellet was suspended in DMEM 1000 units/ml penicillin, 1000 units/ml streptomycin, and 5 % FBS. The cells were then plated on poly-l-lysine (Sigma, St. Louis, MO, USA; cat. no. P4707) coated 96-well or 12-well plates at a density of 1 × 106 cells/ml. For TUNEL assay, the cells were plated on 24-well plates with coverslips (Electron Microscopy Sciences, Hatfield, PA, USA) at a density of 5 × 105 cells/ml, and the coverslips were precoated with poly-l-lysine (Sigma). The medium was replaced by Neurobasal medium with 2 % B27 (Invitrogen, Carlsbad, CA, USA) the following day. As the hippocampal cultures were derived from E18 embryos, at the stage when neurogenesis is about to end and gliogenesis has not yet started, and cultured in Neurobasal medium which is optimized to support growth of neurons rather than glial cells, the cultures contain primarily neurons. For all the experiments, the culture medium per well was 0.1 ml for the 96-well plate, 0.5 ml for the 24-well plate, and 1 ml for the 12-well plate. After culture, the neurons were treated with recombinant neuroserpin or transduced with adenovirus expressing Bcl-2 or LacZ (MOI 20) (Vector Biolabs, Philadelphia, PA, USA) in the presence or absence of 100 μM H2O2.
WST-1 Assay for Cell Viability
The viability of the cells was determined by the WST-1 Cell Proliferation Reagent (Clontech, Mountain View, CA, USA) assay in a 96-well plate. The WST assay is a water-soluble version of the standard MTT assay for cell viability. After the different treatments, 10 μl of premixed WST-1 was added to each well and the plate was maintained in a 37 °C incubator for 1–2 h. The absorbance of the samples was then measured at 440 nm using a multi-well plate reader.
Lactate Dehydrogenase Release Assay for Cell Cytotoxicity
The cytotoxicity of cells after various treatments was evaluated by the extent of the release of lactate dehydrogenase (LDH). This was achieved with a CytoTox 96 Non-Radioactive Cytotoxicity Assay kit according to the manufacturer’s instructions (Promega, Madison, WI, USA).
TUNEL Assay
The TUNEL assay was performed as described previously (Cheng et al. 2013). Briefly, primary cultured hippocampal neurons grown on slides were fixed and permeabilized after the various treatments. An in situ cell death detection kit TUNEL (Roche, Indianapolis, IN, USA) was used to stain the cells. After staining, coverslips were mounted over the slides, which were then imaged under the fluorescence microscope. The cell nuclei were stained with DAPI. The percentage of cell death was determined by the ratio of the number of TUNEL-positive cells to DAPI-stained cells. At least 500 cells were counted in each treatment.
Western Blotting
Western blots were performed as described previously (Cheng et al. 2015). Briefly, protein lysates were prepared using T-Protein Extraction Reagent (Pierce, Rockford, IL, USA) supplemented with 1× Complete Inhibitor Cocktail (Roche), centrifuged at 15,000×g for 10 min at 4 °C, and the protein concentrations in the supernatants were determined using a Bio-Rad Protein Assay (Bio-Rad, Hercules, CA, USA). Twenty micrograms of protein were added to NuPAGE LDS sample buffer (Invitrogen, Carlsbad, CA, USA) and denatured at 70 °C for 10 min. Then, the denatured samples were ran on 4–12 % SDS-PAGE gels (Invitrogen, Carlsbad, CA, USA) and then transferred onto nitrocellulose membrane (Millipore, Billerica, MA, USA). After blocking with 5 % nonfat milk at room temperature for 1 h, the membrane was incubated with the primary antibodies overnight diluted in PBS supplemented with 1 % Tween 20. After washing, the membrane was incubated with fluorophore-conjugated anti-mouse or anti-rabbit antibodies (Amersham, Piscataway, NJ, USA) and visualized using an Odyssey infrared imaging system (LI-COR Inc., Lincoln, NE, USA). Band intensities were quantified using Odyssey software version 2.1. The expression level for each target protein was normalized to expression levels of β-actin.
Statistical Analysis
Data were analyzed by one-way analysis of variance (ANOVA) followed by Tukey post hoc multiple comparisons tests where noted. Significance was set at p < 0.05.
Results
Neuroserpin Protects Hippocampal Neurons Against Oxidative Stress
To determine whether neuroserpin is neuroprotective against oxidative stress, we treated primary hippocampal cultures with 0.215, 2.15, 21.5, and 215 nM of neuroserpin for 1 h, followed by incubation with 100 μM H2O2 for 24 h. Effects were quantitated using assays reporting cell viability (reduction of WST-1), cell cytotoxicity (LDH), and DNA fragmentation that results from apoptotic signaling (TUNEL assay). The cell viability of cultures challenged with H2O2 decreased approximately by 50 % compared to the untreated group (Fig. 1a). However, pretreatment with neuroserpin rescued this oxidative stress-induced decrease in a dose-dependent manner, suggesting a neuroprotective effect of neuroserpin against oxidative stress (Fig. 1a, ANOVA between all the groups; F (5, 93) = 49.06, p < 0.05). The LDH release assay confirmed the neuroprotective effect with neuroserpin dose-dependently attenuating the cytotoxicity caused by oxidative stress (Fig. 1b, F (5, 96) = 91.37, p < 0.05). Furthermore, neuroserpin alone did not significantly affect neuronal cell viability (Fig. 1c, F (4, 45) = 2.097, p > 0.05) or cytotoxicity (Fig. 1d, F (4, 45) = 0.3384, p > 0.05).
Purified recombinant neuroserpin protects against H2O2−induced neurotoxicity in primary cultured rat hippocampal neurons. Neurons were pretreated with varying concentrations of neuroserpin or vehicle alone for 1 h then further treated with H2O2 (100 μM) for 24 h. Cell health was then quantified using assays reporting cell viability (reduction of WST) and cell cytotoxicity (LDH). Neurons were also treated with neuroserpin alone. a, b Neuroserpin inhibited the H2O2−induced decrease in cell viability and increase of cytotoxicity. Data are from three independent experiments, n = 15. Values are mean ± SEM, one-way ANOVA followed by Tukey test. *p < 0.05 compared to the control group, # p < 0.05 compared to the H2O2 group. c. d Neuroserpin alone had no significant effect on the cell viability and cytotoxicity. Data are from two independent experiments, n = 10. Values are mean ± SEM, one-way ANOVA analysis
Results from the TUNEL assay further confirmed a neuroprotective effect. Treatment with 100 μM H2O2 increased the number of apoptotic cells in the primary hippocampal cultures (Fig. 2). Pretreatment with 21.5 nM neuroserpin significantly reduced the number of apoptotic cells (Fig. 2a, b, F (3, 20) = 45.73, p < 0.05).
Neuroserpin reduces apoptotic cell death triggered by H2O2 in cultured rat hippocampal neurons. a Neurons were pretreated with 21.5 nM neuroserpin or vehicle for 1 h, exposed to H2O2 (100 μM) for 24 h, and apoptotic cells detected using a TUNEL assay. Photomicrographs show neurons stained by TUNEL (green) and DAPI (blue) after various treatments. b The bar graphs represent the quantification of the dead cells as a percentage of the total number of cells determined by DAPI staining. Data are from three independent experiments, n = 6. Values are mean ± SEM, one-way ANOVA analysis followed by Tukey test. *p < 0.05 compared to the untreated control group, #p < 0.05 compared to the H2O2-only group
The AKT Signaling Pathway Mediates the Neuroprotective Effect of Neuroserpin
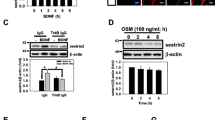
Treatment of hippocampal cultures with 100 μM H2O2 for 24 h increased the phosphorylation of AKT, consistent with a previous study showing that 24 h of oxidative stress increased the phosphorylation of AKT in neurons (Uranga et al. 2013). While neuroserpin alone had no effect on AKT activation (Fig. 3a, F (2, 6) = 1.34, p > 0.05), pretreatment of cultures with 21.5 nM neuroserpin enhanced the activation of AKT induced by oxidative stress (Fig. 3b, F (2, 6) = 33.6, p < 0.05). To determine whether the enhanced activation of AKT plays a role in the neuroprotective effect of neuroserpin, we used the PI3 kinase inhibitor, Ly294002, which has been shown to block PI3 kinase-dependent AKT phosphorylation and kinase activity (Cheng et al. 2013; Gharbi et al. 2007). We treated the neurons with vehicle or 10 μM Ly294002 in the presence or absence of neuroserpin for 1 h, challenged cultures with 100 μM H2O2 for 24 h, and measured LDH levels to quantitate cell toxicity. As shown in Fig. 3c, Ly294002 alone had no effect on cell cytoxicity. However, it reduced the neuroprotective effect of neuroserpin (F (4, 45) = 95.72, p < 0.05).
Neuroserpin pretreatment enhances activation of AKT signaling pathways in cultured rat hippocampal neurons. a Top panel: Neurons were treated with vehicle and 21.5 nM neuroserpin for 1 h or 24 h. Protein lysates were analyzed by Western blotting using antibodies specific for phosphorylated AKT (p-AKT) and total AKT (t-AKT). A representative Western blot is shown. Bottom panel: Bar graphs showing the quantification of p-AKT normalized to t-AKT. Data are from two independent experiments. Values are mean ± SEM, one-way ANOVA followed by Tukey test. b Top panel: Neurons were pretreated with 21.5 nM neuroserpin or vehicle for 1 h and then exposed to H2O2 (100 μM) for 24 h. Protein lysates were analyzed by Western blotting using antibodies specific for phosphorylated AKT (p-AKT) and total AKT (t-AKT). A representative Western blot is shown. Bottom panel: Bar graphs showing the quantification of p-AKT normalized to t-AKT. Data are from three independent experiments. Values are mean ± SEM, one-way ANOVA followed by Tukey test. *p < 0.05 compared to the untreated control group, #p < 0.05 compared to the H2O2 group. c Neurons were pretreated with 10 μM Ly294002 or vehicle in the presence or absence of neuroserpin (21.5 nM) for 1 h and then exposed to 100 μM H2O2 for 24 h before analysis of cytotoxicity using LDH assays. Data are from two independent experiments, n = 10. Values are mean ± SEM, one-way ANOVA followed by Tukey test. *p < 0.05 compared to the H2O2 group, #p < 0.05 compared to the NS + H2O2 group
Neuroserpin Attenuates H2O2-Induced Changes in BCL-2 and Caspase-3
We further investigated the mechanism underlying neuroserpin’s effects on oxidative stress by analysis of the anti-apoptotic AKT downstream signaling pathway protein BCL-2 and the pro-apoptotic enzyme caspase-3. Primary hippocampal cultures were treated with vehicle or 100 μM H2O2 for 24 h. As shown in Fig. 4a, b, the level of BCL-2 in the cultures decreased significantly after treatment with H2O2 compared to the control group. Pretreatment with 21.5 nM neuroserpin significantly inhibited this decrease (F (3, 12) = 7.639, p < 0.05), while treatment with neuroserpin alone had no effect. To see if neuroserpin could enhance the neuroprotective effect mediated by BCL-2, primary hippocampal cultures were transduced with 20 MOI of adenovirus expressing LacZ or BCL-2 for 24 h. BCL-2 transduction significantly reduced the cytotoxicity caused by 100 μM H2O2 (Fig. 4c, F (4, 45) = 62.92, p < 0.05). Pretreatment with 21.5 nM neuroserpin did not enhance this neuroprotective effect. These results suggest that neuroserpin-induced neuroprotection in the hippocampal cultures was dependent on BCL-2. We also found that cultures challenged with 100 μM H2O2 showed increased activation of caspase-3. Pretreatment with 21.5 nM neuroserpin significantly inhibited H2O2-induced activation of caspase-3 (Fig. 4d, e, F (3, 8) = 19.15, p < 0.05).
BCL-2 and caspase-3 are involved in the neuroprotective effect of neuroserpin. Neurons were pretreated with 21.5 nM neuroserpin or vehicle for 1 h and then exposed to H2O2 (100 μM) for 24 h. Protein lysates were analyzed by Western blotting using antibodies specific for BCL-2 and active caspase-3. a Representative Western blot of immunoreactive BCL-2. Duplicate samples of each test condition were analyzed. Actin served as internal control for protein loading. b Bar graphs showing the quantification of BCL-2 normalized to actin. Data are from two independent experiments. Values are mean ± SEM, one-way ANOVA followed by Tukey test, n = 4. *p < 0.05 compared to the untreated control group, #p < 0.05 compared to the H2O2 group. c Primary cultured hippocampal neurons were treated with LacZ or BCL-2 adenovirus for 24 h followed by 21.5 nM neuroserpin or vehicle for 1 h and then exposed to H2O2 (100 μM) for 24 h. Cytotoxicity was measured by LDH release assay after various treatments in the neurons. Data are from two independent experiments, n = 10. Values are mean ± SEM, one-way ANOVA followed by Tukey test. *p < 0.05 compared to the BCL-2-negative group. NS, not significant. d Representative Western blot of active caspase-3. Duplicate samples of each test condition were analyzed. Actin served as internal control for protein loading. e Bar graphs showing the quantification of active caspase-3 normalized to actin. Data are from two independent experiments, n = 3. Values are mean ± SEM, one-way ANOVA followed by Tukey test. *p < 0.05 compared to the control group, #p < 0.05 compared to the H2O2 group. Csp-3, caspase-3
Neuroserpin’s Neuroprotective Effect Is Not Mediated Through Trk Receptors
One possible pathway through which neuroserpin could stimulate PI3K/AKT activity and neuronal survival is through transactivation of Trk receptors. To investigate this possibility, we pretreated cultures with the Trk receptors inhibitor, K252a. Pretreatment did not block neuroserpin’s inhibitory effect on H2O2-induced cell death (Fig. 5, F (4, 45) = 53.47, p < 0.05).
Neuroserpin’s neuroprotective effect is not mediated through Trk receptors. Neurons were pretreated with 100 nM K252a or vehicle in the presence or absence of neuroserpin (21.5 nM) for 1 h and then exposed to 100 μM H2O2 for 24 h before analysis of cytotoxicity using LDH assays. Results suggested that neuroserpin’s neuroprotective effect is not mediated through Trk receptors. Data are from two independent experiments, n = 10. Values are mean ± SEM, one-way ANOVA followed by Tukey test
Discussion
Oxidative stress has been proposed to be a major contributor to neuronal synaptic dysfunction and neuronal loss in aging and a number of neurodegenerative disorders including Alzheimer’s disease (de la Monte and Wands 2006; Joseph et al. 2005; Mancuso et al. 2007; Shi and Gibson 2007). Our results demonstrate that neuroserpin protects against H2O2-induced oxidative stress in primary cultures of rat hippocampal neurons. More detailed analysis of the cellular mechanisms underlying this effect identified a role for PI3 kinase-dependent activation of the AKT signaling pathway. PI3K/AKT is an established mediator of the survival response against oxidative stress (Cheng et al. 2013; Duarte et al. 2008; Uranga et al. 2013). Consistent with previous studies, AKT was activated in response to oxidative stress, through the activity of PI3 kinase, its upstream activator. Activation of this pathway in neurons subjected to oxidative injury has largely been associated with neuronal survival (Choi et al. 2012; Lee et al. 2009; Wang et al. 2012). We found that neuroserpin enhanced H2O2-induced AKT levels and that the protective effect was blocked following inhibition of PI3 kinase. Our results support a role for neuroserpin as an activator of this neuroprotective pathway. We also examined the effects of H2O2 and neuroserpin on levels of the “anti-death” protein BCL-2 and the “pro-death” enzyme caspase-3. BCL-2 is a pro-survival/anti-apoptotic protein that is localized to the outer mitochondrial membrane where it prevents the release of cytochrome c from mitochondria by inhibiting apoptosis-induced mitochondrial pore formation (Yang et al. 1997). Translocation of cytochrome c from the mitochondria to the cytoplasm is a key event in the activation of caspase-3 and the induction of apoptosis (Garrido et al. 2006). Neuroserpin pretreatment significantly reduced both the H2O2-mediated decrease in BCL-2 levels and the increase in caspase-3. These changes would act synergistically to increase neuronal survival and are consistent with the neuroprotective effect of neuroserpin towards oxidative stress seen in this study.
How neuroserpin transduces a survival signal to activate the PI3 kinase/AKT pathway and triggers neuroprotection is not clear. One possibility is through activation of the low-density lipoprotein receptor-related protein-1 (LRP-1) receptor. The LRP receptor is a member of the LDL receptor family that endocytoses a diverse range of ligands and regulates a number of signaling pathways (Bacskai et al. 2000; Hayashi et al. 2007; Herz and Strickland 2001; Hu et al. 2006; Mantuano et al. 2008a; Mantuano et al. 2008b). Recently, activation of LRP-1 by the protease inhibitor α-2-macroglobulin or tPA has been shown to transactivate Trk receptors and stimulate AKT activity (Shi et al. 2009). Given the established roles for Trk receptors in nerve cell survival and inhibition of apoptosis (Zhang et al. 2000; Zhang et al. 2010) and the capability of neuroserpin to bind to the LRP-1 receptor, either as part of a complex with tPA or in association with an unidentified accessory molecule (Makarova et al. 2003), neuroserpin-mediated transactivation of the TrkA receptor is one possible pathway that may underlie the neuroprotective response. However, inhibition of Trk receptor activation failed to block neuroserpin’s inhibitory effect on H2O2-induced cell death suggesting it was not involved. Another possibility is that neuroserpin regulates responses to ROS through a tPA-independent mechanism (Ma et al. 2012). Neuroserpin also has 20 methionine residues, which could act to scavenge free radicals and mediate its neuroprotective function (Mohsenifar et al. 2007).
Interestingly, one of the underlying mechanisms mediating aging and Aβ neurotoxicity is oxidative stress. Aβ has been found to increase levels of H2O2 in neurons, which is thought to lead to an imbalance between ROS and the cells’ oxidant defenses (Behl et al. 1994; Thomas et al. 1996). The response of hippocampal cultures pretreated with neuroserpin to stimulate the natural protective mechanisms of neurons suggests that it may function to reduce the levels of neuronal degeneration during age-dependent stresses such as oxidative stress. A similar mechanism may contribute to neuroserpin’s protective effects following excitotoxic glutamate-induced neuronal death (Lebeurrier et al. 2005), which also involves the production of ROS (Cheng et al. 2013). It should be noted that other mechanisms have been proposed for neuroserpin’s neuroprotective effects including interaction with Aβ to form off-pathway nontoxic oligomers (Kinghorn et al. 2006) and inhibition of tPA-mediated intracellular calcium flux through NMDA receptors (Lebeurrier et al. 2005). Also, in the case of AD, there is evidence that reduced neuroserpin levels leads to fewer and smaller amyloid plaques and reduced memory deficits (Fabbro et al. 2011).
Neuroserpin has been also reported to be neuroprotective in focal ischemic stroke (Cinelli et al. 2001) and more recently in an in vitro ischemic model following oxygen-glucose deprivation and reoxygenation (OGD/R) (Wang et al. 2015). In both models, the neuroprotective effects of neuroserpin were attributed to effects on nonneuronal cells, either microglial cells or astrocytes. The astrocyte study also reported that while OGD/R treatment upregulated levels of pAKT, neuroserpin administration had little effect. While our study used a well-established rat hippocampal culture model that is highly enriched in neurons, we cannot exclude effects of neuroserpin on glial cells that may be present.
In summary, our study demonstrates for the first time that extracellular neuroserpin plays a neuroprotective role against H2O2-induced oxidative stress in primary hippocampal neuronal cultures. These effects are mediated by the PI3 kinase/AKT signaling pathways with neuroserpin attenuating the H2O2-mediated reduction in BCL-2, a pro-survival protein, and blocking the H2O2-mediated activation of the pro-apoptotic caspase, caspase-3. Together with the previously reported anti-excitotoxic effect of neuroserpin, these studies support further investigations into the involvement of neuroserpin in aging and neurodegenerative diseases.
References
Bacskai BJ, Xia MQ, Strickland DK, Rebeck GW, Hyman BT (2000) The endocytic receptor protein LRP also mediates neuronal calcium signaling via N-methyl-D-aspartate receptors. Proc Natl Acad Sci U S A 97:11551–11556.
Behl C, Davis JB, Lesley R, Schubert D (1994) Hydrogen peroxide mediates amyloid beta protein toxicity. Cell 77:817–827.
Berger P, Kozlov SV, Cinelli P, Kruger SR, Vogt L, Sonderegger P (1999) Neuronal depolarization enhances the transcription of the neuronal serine protease inhibitor neuroserpin. Mol Cell Neurosci 14:455–467.
Borges VM, Lee TW, Christie DL, Birch NP (2010) Neuroserpin regulates the density of dendritic protrusions and dendritic spine shape in cultured hippocampal neurons. J Neurosci Res 88:2610–2617.
Butterfield DA, Boyd-Kimball D (2004) Amyloid beta-peptide(1-42) contributes to the oxidative stress and neurodegeneration found in Alzheimer disease brain. Brain Pathol 14:426–432.
Cheng Y, Cawley NX, Loh YP (2013) Carboxypeptidase E/NFalpha1: a new neurotrophic factor against oxidative stress-induced apoptotic cell death mediated by ERK and PI3-K/AKT pathways. PLoS One 8:e71578.
Cheng Y, Rodriguiz RM, Murthy SR, Senatorov V, Thouennon E, Cawley NX, Aryal DK, Ahn S, Lecka-Czernik B, Wetsel WC, Loh YP (2015) Neurotrophic factor-alpha1 prevents stress-induced depression through enhancement of neurogenesis and is activated by rosiglitazone. Mol Psychiatry 20:744–754
Choi H, Park HH, Koh SH, Choi NY, Yu HJ, Park J, Lee YJ, Lee KY (2012) Coenzyme Q10 protects against amyloid beta-induced neuronal cell death by inhibiting oxidative stress and activating the P13K pathway. Neurotoxicology 33:85–90.
Cinelli P, Madani R, Tsuzuki N, Vallet P, Arras M, Zhao CN, Osterwalder T, Rulicke T, Sonderegger P (2001) Neuroserpin, a neuroprotective factor in focal ischemic stroke. Mol Cell Neurosci 18:443–457
de la Monte SM, Wands JR (2006) Molecular indices of oxidative stress and mitochondrial dysfunction occur early and often progress with severity of Alzheimer’s disease. J Alzheimers Dis 9:167–181.
Duarte AI, Santos P, Oliveira CR, Santos MS, Rego AC (2008) Insulin neuroprotection against oxidative stress is mediated by Akt and GSK-3beta signaling pathways and changes in protein expression. Biochim Biophys Acta 1783:994–1002.
Fabbro S, Schaller K, Seeds NW (2011) Amyloid-beta levels are significantly reduced and spatial memory defects are rescued in a novel neuroserpin-deficient Alzheimer’s disease transgenic mouse model. J Neurochem 118:928–938.
Fabbro S, Seeds NW (2009) Plasminogen activator activity is inhibited while neuroserpin is up-regulated in the Alzheimer disease brain. J Neurochem 109:303–315.
Gandhi, S., Abramov, A.Y., 2012. Mechanism of oxidative stress in neurodegeneration. Oxidative Medicine and Cellular Longevity, Article ID 428010.
Garrido C, Galluzzi L, Brunet M, Puig PE, Didelot C, Kroemer G (2006) Mechanisms of cytochrome c release from mitochondria. Cell Death Differ 13:1423–1433.
Gharbi SI, Zvelebil MJ, Shuttleworth SJ, Hancox T, Saghir N, Timms JF, Waterfield MD (2007) Exploring the specificity of the PI3K family inhibitor LY294002. The Biochemical Journal 404:15–21.
Hastings GA, Coleman TA, Haudenschild CC, Stefansson S, Smith EP, Barthlow R, Cherry S, Sandkvist M, Lawrence DA (1997) Neuroserpin, a brain-associated inhibitor of tissue plasminogen activator is localized primarily in neurons. Implications for the regulation of motor learning and neuronal survival The Journal of Biological Chemistry 272:33062–33067.
Hayashi H, Campenot RB, Vance DE, Vance JE (2007) Apolipoprotein E-containing lipoproteins protect neurons from apoptosis via a signaling pathway involving low-density lipoprotein receptor-related protein-1. J Neurosci 27:1933–1941.
Herz J, Strickland DK (2001) LRP: a multifunctional scavenger and signaling receptor. J Clin Invest 108:779–784.
Hill RM, Parmar PK, Coates LC, Mezey E, Pearson JF, Birch NP (2000) Neuroserpin is expressed in the pituitary and adrenal glands and induces the extension of neurite-like processes in AtT-20 cells. The Biochemical Journal 345:595–601.
Hu K, Yang J, Tanaka S, Gonias SL, Mars WM, Liu Y (2006) Tissue-type plasminogen activator acts as a cytokine that triggers intracellular signal transduction and induces matrix metalloproteinase-9 gene expression. J Biol Chem 281:2120–2127.
Joseph JA, Shukitt-Hale B, Casadesus G, Fisher D (2005) Oxidative stress and inflammation in brain aging: nutritional considerations. Neurochem Res 30:927–935.
Kinghorn KJ, Crowther DC, Sharp LK, Nerelius C, Davis RL, Chang HT, Green C, Gubb DC, Johansson J, Lomas DA (2006) Neuroserpin binds Abeta and is a neuroprotective component of amyloid plaques in Alzheimer disease. J Biol Chem 281:29268–29277.
Krueger SR, Ghisu GP, Cinelli P, Gschwend TP, Osterwalder T, Wolfer DP, Sonderegger P (1997) Expression of neuroserpin, an inhibitor of tissue plasminogen activator, in the developing and adult nervous system of the mouse. J Neurosci 17:8984–8996.
Lebeurrier N, Liot G, Lopez-Atalaya JP, Orset C, Fernandez-Monreal M, Sonderegger P, Ali C, Vivien D (2005) The brain-specific tissue-type plasminogen activator inhibitor, neuroserpin, protects neurons against excitotoxicity both in vitro and in vivo. Mol Cell Neurosci 30:552–558.
Lee TW, Coates LC, Birch NP (2008) Neuroserpin regulates N-cadherin-mediated cell adhesion independently of its activity as an inhibitor of tissue plasminogen activator. J Neurosci Res 86:1243–1253.
Lee TW, Tsang VW, Birch NP (2015) Physiological and pathological roles of tissue plasminogen activator and its inhibitor neuroserpin in the nervous system. Front Cell Neurosci 9:396.
Lee YJ, Park KH, Park HH, Kim YJ, Lee KY, Kim SH, Koh SH (2009) Cilnidipine mediates a neuroprotective effect by scavenging free radicals and activating the phosphatidylinositol 3-kinase pathway. J Neurochem 111:90–100.
Li J, O W, Li W, Jiang ZG, Ghanbari HA (2013) Oxidative stress and neurodegenerative disorders. Int J Mol Sci 14:24438–24475.
Ma J, Tong Y, Yu D, Mao M (2012) Tissue plasminogen activator-independent roles of neuroserpin in the central nervous system. Neural Regeneration Research 7:146–151.
Madani R, Kozlov S, Akhmedov A, Cinelli P, Kinter J, Lipp HP, Sonderegger P, Wolfer DP (2003) Impaired explorative behavior and neophobia in genetically modified mice lacking or overexpressing the extracellular serine protease inhibitor neuroserpin. Mol Cell Neurosci 23:473–494.
Makarova A, Mikhailenko I, Bugge TH, List K, Lawrence DA, Strickland DK (2003) The low density lipoprotein receptor-related protein modulates protease activity in the brain by mediating the cellular internalization of both neuroserpin and neuroserpin-tissue-type plasminogen activator complexes. J Biol Chem 278:50250–50258.
Mancuso C, Scapagini G, Curro D, Giuffrida Stella AM, De Marco C, Butterfield DA, Calabrese V (2007) Mitochondrial dysfunction, free radical generation and cellular stress response in neurodegenerative disorders. Front Biosci 12:1107–1123.
Mantuano E, Inoue G, Li X, Takahashi K, Gaultier A, Gonias SL, Campana WM (2008a) The hemopexin domain of matrix metalloproteinase-9 activates cell signaling and promotes migration of Schwann cells by binding to low-density lipoprotein receptor-related protein. J Neurosci 28:11571–11582.
Mantuano E, Mukandala G, Li X, Campana WM, Gonias SL (2008b) Molecular dissection of the human alpha2-macroglobulin subunit reveals domains with antagonistic activities in cell signaling. J Biol Chem 283:19904–19911.
Melo A, Monteiro L, Lima RM, Oliveira DM, Cerqueira MD, El-Bacha RS (2011) Oxidative stress in neurodegenerative diseases: mechanisms and therapeutic perspectives. Oxidative Med Cell Longev 2011:467180.
Miranda E, Lomas DA (2006) Neuroserpin: a serpin to think about. Cell Mol Life Sci 63:709–722.
Mohsenifar A, Lotfi AS, Ranjbar B, Allameh A, Zaker F, Hasani L, Kia BE, Hasannia S (2007) A study of the oxidation-induced conformational and functional changes in neuroserpin. Iran Biomed J 11:41–46.
Navarro-Yubero C, Cuadrado A, Sonderegger P, Munoz A (2004) Neuroserpin is post-transcriptionally regulated by thyroid hormone. Brain research. Mol Brain Res 123:56–65.
Nielsen HM, Minthon L, Londos E, Blennow K, Miranda E, Perez J, Crowther DC, Lomas DA, Janciauskiene SM (2007) Plasma and CSF serpins in Alzheimer disease and dementia with Lewy bodies. Neurology 69:1569–1579.
Osterwalder T, Cinelli P, Baici A, Pennella A, Krueger SR, Schrimpf SP, Meins M, Sonderegger P (1998) The axonally secreted serine proteinase inhibitor, neuroserpin, inhibits plasminogen activators and plasmin but not thrombin. J Biol Chem 273:2312–2321.
Osterwalder T, Contartese J, Stoeckli ET, Kuhn TB, Sonderegger P (1996) Neuroserpin, an axonally secreted serine protease inhibitor. EMBO J 15:2944–2953.
Parmar PK, Coates LC, Pearson JF, Hill RM, Birch NP (2002) Neuroserpin regulates neurite outgrowth in nerve growth factor-treated PC12 cells. J Neurochem 82:1406–1415.
Qin XY, Cheng Y, Murthy SR, Selvaraj P, Loh YP (2014) Carboxypeptidase E-DeltaN, a neuroprotein transiently expressed during development protects embryonic neurons against glutamate neurotoxicity. PLoS One 9:e112996.
Radi E, Formichi P, Battisti C, Federico A (2014) Apoptosis and oxidative stress in neurodegenerative diseases. J Alzheimers Dis 42(Suppl 3):S125–S152.
Robinson SD, Lee TW, Christie DL, Birch NP (2015) Tissue plasminogen activator inhibits NMDA-receptor-mediated increases in calcium levels in cultured hippocampal neurons. Front Cell Neurosci 9:404.
Shi Q, Gibson GE (2007) Oxidative stress and transcriptional regulation in Alzheimer disease. Alzheimer Dis Assoc Disord 21:276–291.
Shi, Y., Mantuano, E., Inoue, G., Campana, W.M., Gonias, S.L., 2009. Ligand binding to LRP1 transactivates Trk receptors by a Src family kinase-dependent pathway. Science Signaling 2, ra18.
Stoeckli ET, Lemkin PF, Kuhn TB, Ruegg MA, Heller M, Sonderegger P (1989) Identification of proteins secreted from axons of embryonic dorsal-root-ganglia neurons. Eur J Biochem 180:249–258.
Thomas T, Thomas G, McLendon C, Sutton T, Mullan M (1996) Beta-amyloid-mediated vasoactivity and vascular endothelial damage. Nature 380:168–171.
Uranga RM, Katz S, Salvador GA (2013) Enhanced phosphatidylinositol 3-kinase (PI3K)/Akt signaling has pleiotropic targets in hippocampal neurons exposed to iron-induced oxidative stress. J Biol Chem 288:19773–19784.
Wang L, Zhang Y, Asakawa T, Ll W, Han S, Ll Q, Xiao B, Namba H, Lu C, Dong Q (2015) Neuroprotective effect of neuroserpin in oxygen-glucose deprivation- and reoxygenation-treated rat astrocytes in vitro. PLoS One 10:1–16
Wang S, Chong ZZ, Shang YC, Maiese K (2012) Wnt1 inducible signaling pathway protein 1 (WISP1) blocks neurodegeneration through phosphoinositide 3 kinase/Akt1 and apoptotic mitochondrial signaling involving Bad, Bax, Bim, and Bcl-xL. Curr Neurovasc Res 9:20–31.
Wannier-Morino P, Rager G, Sonderegger P, Grabs D (2003) Expression of neuroserpin in the visual cortex of the mouse during the developmental critical period. Eur J Neurosci 17:1853–1860.
Wu J, Echeverry R, Guzman J, Yepes M (2010) Neuroserpin protects neurons from ischemia-induced plasmin-mediated cell death independently of tissue-type plasminogen activator inhibition. Am J Pathol 177:2576–2584.
Yang J, Liu X, Bhalla K, Kim CN, Ibrado AM, Cai J, Peng TI, Jones DP, Wang X (1997) Prevention of apoptosis by Bcl-2: release of cytochrome c from mitochondria blocked. Science 275:1129–1132
Yepes M, Sandkvist M, Wong MK, Coleman TA, Smith E, Cohan SL, Lawrence DA (2000) Neuroserpin reduces cerebral infarct volume and protects neurons from ischemia-induced apoptosis. Blood 96:569–576.
Zhang Y, Moheban DB, Conway BR, Bhattacharyya A, Segal RA (2000) Cell surface Trk receptors mediate NGF-induced survival while internalized receptors regulate NGF-induced differentiation. J Neurosci 20:5671–5678.
Zhang Y, Zhao J, Wang J, Jiao X (2010) Brain-derived neurotrophic factor inhibits phenylalanine-induced neuronal apoptosis by preventing RhoA pathway activation. Neurochem Res 35:480–486
Acknowledgments
This research was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Health and Human Development, National Institutes of Health, USA, and grants from the Auckland Medical Research Foundation and the University of Auckland to NPB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animal procedures were approved by the Animal Care and Use Committee, NICHD, NIH.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cheng, Y., Loh, Y.P. & Birch, N.P. Neuroserpin Attenuates H2O2-Induced Oxidative Stress in Hippocampal Neurons via AKT and BCL-2 Signaling Pathways. J Mol Neurosci 61, 123–131 (2017). https://doi.org/10.1007/s12031-016-0807-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-016-0807-7