Abstract
Background
Factors associated with discharge disposition and mortality following aneurysmal subarachnoid hemorrhage (aSAH) are not well-characterized. We used a national all-payer database to identify factors associated with home discharge and in-hospital mortality.
Methods
The National Inpatient Sample was queried for patients with aSAH within a 4-year range. Weighted multivariable logistic regression models were constructed and adjusted for age, sex, race, household income, insurance status, comorbidity burden, National Inpatient Sample SAH Severity Score, disease severity, treatment modality, in-hospital complications, and hospital characteristics (size, teaching status, and region).
Results
Our sample included 37,965 patients: 33,605 were discharged alive and 14,350 were discharged home. Black patients had lower odds of in-hospital mortality compared with White patients (adjusted odds ratio [aOR] = 0.67, 95% confidence interval [CI] 0.52–0.86, p = 0.002). Compared with patients with private insurance, those with Medicare were less likely to have a home discharge (aOR = 0.58, 95% CI 0.46–0.74, p < 0.001), whereas those with self-pay (aOR = 2.97, 95% CI 2.29–3.86, p < 0.001) and no charge (aOR = 3.21, 95% CI 1.57–6.55, p = 0.001) were more likely to have a home discharge. Household income percentile was not associated with discharge disposition or in-hospital mortality. Paradoxically, increased number of Elixhauser comorbidities was associated with significantly lower odds of in-hospital mortality.
Conclusions
We demonstrate independent associations with hospital characteristics, patient characteristics, and treatment characteristics as related to discharge disposition and in-hospital mortality following aSAH, adjusted for disease severity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aneurysmal subarachnoid hemorrhage (aSAH) has had historically high in-hospital mortality rates when compared with other causes of stroke [1, 2]. Mortality and discharge disposition can be affected by a wide range of patient-level and hospital-level factors, including age, comorbidities, treatment modality, and in-hospital complications [3,4,5]. Several studies have used the Nationwide Inpatient Sample (NIS) database to explore predictors of patient outcomes after SAH but have been limited by the use of nonspecific measures of SAH severity and the unvalidated reliance on discharge disposition as a measure of patient outcome [1, 6,7,8].
Until recently, there was no rapid measure of SAH severity available within the NIS database. However, the NIS-SAH Severity Score (NIS-SSS) was developed in 2014 on the basis of information available within the database and validated against existing aSAH severity and general disability scores (Hunt-Hess grade and Modified Rankin Scale) [9]. Consequently, more clinically relevant conclusions can be drawn regarding predictors of discharge disposition after hospitalization for aSAH using these measures.
The goal of this study is to identify patient-level and hospital-level factors that predict home discharge disposition and in-hospital mortality for patients with aSAH after adjusting for NIS-SSS and variables that may potentially influence discharge disposition and/or mortality. Findings may inform treatment planning for inpatient and after-care settings.
Methods
Data Source and Patient Population
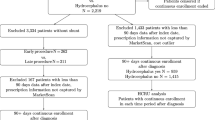
This study was a retrospective analysis of approximately 4 years of data (1 January 2012 to 30 September 2015) from the Healthcare Cost and Utilization Project NIS. The NIS is a national all-payer database maintained by the United States Agency for Healthcare Research and Quality that contains information from more than 7 million hospitalizations annually across a 20% stratified sample of all discharges from nonfederal, short-term hospitals in the United States. The NIS represents approximately 35 million annual hospitalizations once sampling weights are applied. Up to 30 diagnoses and 15 procedure codes associated with each discharge record are captured by using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) system. Sampling weights were used for all estimates reported in this study. Because all data reported in the NIS are deidentified, this study was exempt from approval by the Institutional Review Board.
Patients were included if they had a primary ICD-9-CM diagnosis code of SAH (diagnosis code 430). To ensure that our sample contained patients with aSAH, we excluded patients with ICD-9-CM codes consistent with head trauma (ICD-9-CM diagnosis codes 800.0–801.9, 803.0–804.9, 850.0–854.1, and 873.0–879.9), arteriovenous malformation and/or fistula (ICD-9-CM diagnosis code 747.81; ICD-9-CM procedure codes 39.53, 92.30). Patients were excluded if their All Patient Refined Diagnosis Related Group (APRDRG) Severity Subclass was missing. Furthermore, our analysis was restricted to patients who underwent treatment with either surgical clipping (ICD-9-CM procedure code 39.51) or endovascular coiling (ICD-9-CM procedure codes 39.72, 39.75, 39.76, 39.79, 39.52) during their hospitalization to exclude patients transferred out of facilities that were unable to provide treatment.
Data Collection
The primary objective of this study was to identify factors associated with discharge to home and in-hospital mortality following aSAH, after controlling for disease severity and other baseline variables. Disease severity was measured by using the NIS-SSS, which has been validated as a proxy for the Hunt-Hess grade [9]. NIS-SSS was grouped for scores < 7 and those ≥ 7; an NIS-SSS score of 7 is equivalent to a Hunt-Hess grade of 4. Patient variables collected included age (< 50, 50–64, 65–79, and ≥ 80 years), sex, race (White, Black, Hispanic, Asian or Pacific Islander, Native American, Other), household income (0–25th percentile, 26th–50th percentile, 51st–75th percentile, 76th–100th percentile), insurance status (Medicare, Medicaid, Private, Self-Pay, No charge, Other), APRDRG disease severity (no, minor/moderate, major, or extreme loss of function), treatment modality (surgical clipping or endovascular coiling), and number of in-hospital complications. In-hospital complications analyzed included Terson’s syndrome (ICD-9-CM code 379.23), vasospasm (435.9), Takotsubo’s cardiomyopathy (429.83), seizure (780.31, 780.39), iatrogenic cerebrovascular infarction or hemorrhage (997.02), deep venous thrombosis (453.2, 453.40–453.42, 453.81–453.89, 453.9), pulmonary embolism (415.1, 415.10, 415.11, 415.19), myocardial infarction/other cardiac complication (410.00–410.92, 997.1), acute renal failure (584.5–584.9), and acute respiratory failure (518.4, 518.51–518.53, 518.81). Hospital characteristics collected included hospital bed size (small, medium, large), hospital type (rural, urban teaching, urban nonteaching), and hospital region (Northeast, Midwest, South, West). Comorbidity status was assessed by using the Elixhauser comorbidity measure, which has been validated for use in administrative datasets [10]. Patients were assigned one point per Elixhauser comorbidity to compute an Elixhauser comorbidity score, which was analyzed as a categorical variable (0–2, 3–5, and ≥ 6). Outcome measures included discharge disposition and in-hospital mortality. Discharge disposition was classified as home or nonhome (short-term hospital, home health care, or other facility). Patients who died in the hospital were not included in the discharge disposition analysis.
To note, the NIS database does not distinguish between acute rehabilitation, subacute rehabilitation, and skilled nursing facilities. Thus, the reported outcome of nonhome discharge does not always represent a negative outcome, as acute rehabilitation often precedes home discharge. Despite this limitation, home discharge is still generally the most favorable outcome, and thus understanding predictors of home discharge yields important insights. We chose to use the NIS database because of its robust sample size and breadth of characteristics.
Statistical Analysis
All statistical analyses and data processing steps were conducted in SAS Version 9.4 (SAS Institute, Cary, NC) using proc survey procedures to account for NIS strata, clusters, and weighting. Patients were stratified on the basis of discharge disposition or in-hospital mortality. Weighted descriptive statistics summarizing sociodemographic characteristics, comorbidities, and hospital characteristics for patients were generated. Weighted frequencies of sociodemographic characteristics, comorbidities, and hospital characteristics were compared among groups by using the Rao-Scott χ2 test. Multivariable logistic regression models were constructed to identify factors independently associated with discharge home and in-hospital mortality, after adjusting for covariates (age, sex, race, household income, insurance status, Elixhauser comorbidity score, NIS-SSS, APRDRG disease severity, treatment modality, number of complications, hospital bed size, hospital type, and hospital region). Statistical significance was defined at the p < 0.05 level.
Results
We present survey-weighted national estimates for home and nonhome discharge and for discharged alive and in-hospital mortality in Tables 1 and 2, respectively. We present adjusted odds ratios (aOR) from our multivariable logistic regression analysis for home discharge and for in-hospital mortality in Tables 3 and 4, respectively. Our mortality analysis included 37,965 patients, of whom 33,605 (88.5%) were discharged alive. A total of 33,595 patients were included in our discharge disposition analysis (patients with missing discharge data were excluded) and 14,350 (42.7%) were discharged home. We present a multicollinearity analysis; there is low concern for multicollinearity in our model (Supplemental Table 1).
System/Care Setting
Hospital bed size (small, medium, or large) and hospital type (rural, urban nonteaching, or urban teaching) were not associated with discharge disposition or in-hospital mortality. Compared with patients in hospitals in the Northeast, patients in hospitals in the Midwest (aOR 1.31, 95% confidence interval [CI] 1.05–1.63, p = 0.016), South (aOR 1.73, 95% CI: 1.39–2.15, p < 0.001), and West (aOR 2.21, 95% CI: 1.74–2.81, p < 0.001) had increased odds of home discharge. There were no differences in in-hospital mortality among hospital regions.
Socioeconomic Factors
Insurance status was associated with discharge disposition. Compared with patients with private insurance, those with Medicare were less likely to have a home discharge (aOR 0.58, 95% CI 0.46–0.74, p < 0.001). Those with self-pay (aOR 2.97, 95% CI 2.29–3.86, p < 0.001) and no charge (aOR 3.21, 95% CI 1.57–6.55, p = 0.001) were more likely to have a home discharge. There was no significant difference in likelihood for home discharge between private and Medicaid insurances. Compared with privately insured patients, those with self-pay also had a higher likelihood of in-hospital mortality (aOR 1.69, 95% CI 1.26–2.27, p < 0.001). Household income percentile was not associated with discharge disposition or in-hospital mortality.
Demographic Factors
Increased age was associated with decreased likelihood of home discharge and increased likelihood of in-hospital mortality. Compared with patients aged under 50 years, those aged 50–64 years (aOR 0.55, 95% CI 0.47–0.64, p < 0.001), 65–79 years (aOR 0.28, 0.22–0.37, p < 0.001), and more than 80 years (aOR 0.10, 95% CI 0.06–0.18, p < 0.001) were less likely to be discharged home. Compared with patients aged under 50 years, those aged 65–79 years (aOR 1.78, CI 1.29–2.45, p < 0.001), and more than 80 years (aOR 3.55, 95% CI 2.29–5.51, p < 0.001) were more likely to die in-hospital. Women made up a higher proportion of the cohort of patients with aSAH and, on unadjusted analysis, were less likely to have home discharge (p < 0.001). However, when adjusted for covariates, this association was no longer significant (aOR 0.88, 95% CI 0.77–1.00, p = 0.057). There was no difference in mortality between sexes. Although there were no significant differences in discharge dispositions between races, Black patients had lower odds of in-hospital mortality compared with White patients (aOR 0.67, 95% CI 0.52–0.86, p = 0.002).
Severity of Illness
Greater NIS-SSS and increased APRDRG disease severity were associated with lower odds of home discharge and greater odds of in-hospital mortality. Compared with patients with an NIS-SSS less than 7, those with a score greater or equal to 7 demonstrated lower odds of home discharge (aOR 0.46, CI 0.38–0.56, p < 0.001) and higher odds of in-hospital mortality (aOR 1.23, CI 1.02–1.48, p < 0.034). Compared with patients with none to moderate loss of function (i.e., APRDRG score of 1 or 2), patients with major loss of function had a decreased odds of home discharge (aOR 0.38, 95% CI 0.31–0.46, p < 0.001) and increased odds of in-hospital mortality (aOR 6.95, 95% CI 2.83–17.09, p < 0.001). This was similarly seen in patients with extreme loss of function (aOR 0.10, 95% CI 0.08–0.13, p < 0.001 for home discharge: aOR 33.39, 95% CI 12.20–83.80, p < 0.001 for in-hospital mortality).
A higher number of Elixhauser comorbidities was associated with lower odds of home discharge and paradoxically lower odds of in-hospital mortality. Compared with patients with zero to two comorbidities, those with three to five comorbidities (aOR 0.70, 95% CI 0.61–0.80, p < 0.001) and greater than six comorbidities (aOR 0.43, 95% CI 0.32–0.57, p < 0.001) had a lower odds of home discharge. Compared with patients with zero to two comorbidities, those with three to five comorbidities (aOR 0.58, 95% CI 0.48–0.69, p < 0.001) and greater than six comorbidities (aOR 0.43, 95% CI 0.34–0.62, p < 0.001) had lower odds of in-hospital mortality. When comparing characteristics of patients with zero to two Elixhauser comorbidities with those with greater than six comorbidities on univariate analysis, groups differed with respect to age, sex, race, insurance status, disease severity, treatment modality, number of complications, and discharge disposition (Supplemental Table 2). There was no difference in in-hospital mortality.
Treatment
Clipping, as compared with coiling, was associated with a decreased likelihood of home discharge (aOR 0.69, 95% CI 0.59–0.80, p < 0.001) but no difference in in-hospital mortality. Increased numbers of complications were associated with a decreasing likelihood of home discharge and increasing likelihood of in-hospital mortality. Compared with patients with no complications, those with one, two, and three or more complications had significantly (p < 0.001) lower rates of home discharge and higher rates in-hospital mortality, respectively (home discharge: one complication, aOR 0.68, 95% CI 0.58–0.81; two complications, aOR 0.55, 95% CI 0.43–0.70; ≥ 3 complications aOR 0.49, 95% CI 0.34–0.72. In-hospital mortality: one complication, aOR 2.24, 95% CI 1.69–2.97; two complications, aOR 2.52, 95% CI 1.86–3.42, ≥ 3 complications aOR 2.13, 95% CI 1.45–3.10).
Discussion
This work represents the first analysis, adjusted for multiple measures of aSAH disease severity, of patient-level and hospital-level factors for home discharge in the population of patients with aSAH. With respect to facility characteristics, although hospitals in the Northeast were associated with lower odds of home discharge, there were no regional differences in mortality rates. With respect to patient variables, Medicare insurance, older age, and poorer health status were associated with lower rates of home discharge. Older age, self-pay insurance status, greater NIS-SSS, lower Elixhauser comorbidities, and White race (compared with Black race) were associated with greater odds of in-hospital mortality. Regarding treatment variables, clipping (compared with coiling) and greater number of complications were associated with lower odds of home discharge. We show metavariables (care setting), patient variables, and treatment variables all influence disposition and mortality outcomes, and this work highlights the disparities that may exist in the population of patients with aSAH.
Although our study cannot identify causal mechanisms for the associations seen, it informs future analyses of data sets that have more granularity. Longitudinal studies examining health outcomes prior to aneurysm rupture and post discharge beyond the inpatient setting, qualitative studies examining health-related quality of life and patient preferences, and institutional studies examining time to care and specific interventions will all help identify reasons for why the health disparities seen exist. Our work generates multiple hypotheses regarding hospital system characteristics, patient characteristics, and treatment characteristics. It informs us of patient groups, such as regarding insurance status and comorbidity score, that may have suboptimal outcomes and need more support.
Hospital System Characteristics
Hospital-level factors, including location, were associated with home discharge, although hospital bed size and type (rurality and teaching status) were not. Although it is difficult to ascertain exactly why hospitals in the Northeast are associated with decreased home discharge, several hospital-level cultural factors can influence outcomes, including regional implementation of initiatives, such as nurse-driven patient mobilization (e.g., physical therapy) and neurointensivist-led care teams, which have been shown to significantly improve discharge disposition outcomes in patients with aSAH [11, 12]. Furthermore, higher hospital aSAH volume has been shown to be associated with increased home discharge and lower in-hospital mortality, suggesting hospitals with higher aSAH volumes may provide better outcomes, perhaps owing to more experienced surgeons or better equipped teams [13, 14]. Illustratively, a study comparing aSAH treated at an institution’s tertiary referral university hospital and safety net county hospital found that the university hospital had significantly more discharges to home or rehabilitation centers than the county hospital did. Even after adjusting for disease severity, length of hospital stays, and insurance status, county hospital patients were more than three times more likely to be discharged with a poor Modified Rankin Scale score and Glasgow Outcome Scale score [15]. Interestingly, an NIS database study on heart failure also found that the Northeast region was associated with the least risk-adjusted rate of routine home discharge [16].
Patient Characteristics
Older age was associated with worsened outcomes, which aligns with past aSAH analyses. Two separate single-institution retrospective studies found that age and Hunt-Hess grade were associated with discharge disposition and mortality, whereas race, sex, frailty, Fisher score, body mass index, multiple aneurysms, and aneurysm size and location were not [17, 18]. A prospective study found that age and clinical grade at presentation affected 6-month postdischarge outcomes as measured by Glasgow Coma Outcome scale, although time to surgery post aSAH bleed did not [19]. A study of patients more than 70 years old found that increasing age significantly affects discharge disposition and mortality: patients who died in-hospital and who were discharged to rehabilitation were significantly older than those discharged home [20].
Black patients have a decreased in-hospital mortality compared with White patients. In contrast, a study analyzing all patients with SAH discharged in New York City in a 1-year time span found that non-White race was associated with poorer Modified Rankin Scale score, even when controlling for payer status [21]. A national study on patients with traumatic brain injury found that, compared with White patients, Black patients were less likely to opt for withdrawal of life support or engage in palliative measures, such as going to hospice, possibly due to distrust of the hospital system [22]. There is currently a dearth of work done on racial associations with outcomes in patients with aSAH, and additional work should be done to further explore these findings.
Compared with privately insured patients, Medicare patients had lower odds of home discharge, whereas self-paying patients had higher odds of home discharge. This finding has been previously shown in both SAH and intracerebral hemorrhage populations, suggesting that for self-pay patients, home discharge may indicate limited access to rehabilitation and skilled care facilities and a lack of readily accessible discharge options, and in reality, may not be an optimal health outcome [23, 24].
Severity of Condition and Treatment Characteristics
We found more severe disease, as measured by number of Elixhauser comorbidities, NIS-SSS, APRDRG severity, and number of complications, was, unsurprisingly, associated with lower odds of home discharge. Patients with a high Elixhauser comorbidity burden did not differ from those with a low comorbidity burden on univariate analysis. However, paradoxically, a greater number of Elixhauser comorbidities was associated with lower odds of mortality, although this index has previously been shown to be a predictor of mortality [25, 26]. The reason why lower comorbidity burden is associated with in-hospital mortality after adjustment for all other variables on multivariate analysis is unclear. As shown in our supplemental analysis, multicollinearity would not the culprit. Rather, it can be hypothesized that withdrawal of life-sustaining support is less likely to be pursued in individuals with a baseline higher morbidity because they already lived with a significant number of burdens. Hence, it is possible that such patients may survive but are discharged to a higher level of care. Indeed, families of patients with more comorbidities may be more familiar with the hospital system and more likely to opt for discharge to a higher level of care, such as a skilled nursing facility or long-term acute care hospital, rather than withdrawing care. There is also a chance that patients with a higher comorbidity burden had early withdrawal of life-sustaining support, which was not counted as in-hospital mortality. However, given the lack of data on code status of patients, this hypothesis cannot be thoroughly tested. A limitation of the NIS and many databases is the inability to capture qualitative data such as cultural tendencies, patients’ goals of care, family dynamics, and physician–patient decision making.
Finally, treatment modality can influence discharge disposition; we found that coiling was associated with a greater odds of home discharge than clipping. This is likely because patients who undergo clipping need additional care in the acute period, as demonstrated in a previous NIS analysis finding that clipping is associated with increased length of hospital stay compared with coiling [4]. The data set unfortunately does not delineate the nuances decision making required when deciding between endovascular or open surgeon for complex aneurysms including aneurysmal architecture or potential need for dual antiplatelet therapy (DAPT).
Limitations
Several limitations are present in our work. First, errors are likely present when coding patients in the NIS, particularly for patients who died in the hospital and are coded retroactively [27], which may bias our mortality results, as the total number of comorbidities in deceased patients may not be fully coded. However, audits are routinely conducted on billing claims, which incentivizes accurate reporting [28]. Second, although the NIS data set allows for robust analysis of population-level data, it did not provide detailed treatment-specific factors that may influence clinical decision making, such as aneurysm size and morphology, the presence of multiple aneurysms requiring treatment, or clinical versus radiographic vasospasm. Crucial treatment variables, such as time to aneurysm clipping or blood pressure control, could not be analyzed. To help overcome this limitation, our analysis adjusted for broad treatment patterns (securement method and number of complications) and hospital factors, which often influence treatment protocols. Third, with respect to our primary outcome of discharge disposition, the NIS does not distinguish between acute rehabilitation, subacute rehabilitation, and skilled nursing facilities, although discharge to acute rehabilitation may be considered a positive outcome in the setting of ruptured aSAH. Additionally, patient code status (which we did not have data on) may have influenced outcomes, as patients with do-not-resuscitate status or do-not-intervene status may not have received interventions or may have been discharged home despite a poor condition. Finally, because ICD-9-CM codes do not specify aSAH, there is a possibility that non-aSAH was included. However, we minimized the risk of capturing non-aSAH by excluding all trauma-related and arteriovenous malformation/fistula-related diagnoses, as well as limiting the sample to patients who were clipped or coiled.
Conclusions
This study demonstrates substantial independent associations with hospital characteristics, patient characteristics, and treatment characteristics as related to discharge disposition and in-hospital mortality following aSAH, adjusted for disease severity. Future studies are needed to identify drivers of these differences and elucidate avenues by which to mitigate them.
References
Jaja BNR, Saposnik G, Nisenbaum R, et al. Racial/ethnic differences in inpatient mortality and use of institutional postacute care following subarachnoid hemorrhage. J Neurosurg. 2013;119:1627–32. https://doi.org/10.3171/2013.7.JNS13544.
Ovbiagele B. Nationwide trends in in-hospital mortality among patients with stroke. Stroke. 2010;41:1748–54. https://doi.org/10.1161/STROKEAHA.110.585455.
Lagares A, Gómez PA, Alen JF, et al. A comparison of different grading scales for predicting outcome after subarachnoid haemorrhage. Acta Neurochir (Wien). 2005;147:5–16. https://doi.org/10.1007/s00701-004-0417-y.
Hammer A, Ranaie G, Erbguth F, et al. Impact of complications and comorbidities on the intensive care length of stay after aneurysmal subarachnoid haemorrhage. Sci Rep. 2020;10:6228. https://doi.org/10.1038/s41598-020-63298-9.
Khatri R, Tariq N, Vazquez G, Suri MFK, Ezzeddine MA, Qureshi AI. Outcomes after nontraumatic subarachnoid hemorrhage at hospitals offering angioplasty for cerebral vasospasm: a national level analysis in the United States. Neurocrit Care. 2011;15:34–41. https://doi.org/10.1007/s12028-010-9423-5.
Bateman BT, Olbrecht VA, Berman MF, Minehart RD, Schwamm LH, Leffert LR. Peripartum subarachnoid hemorrhage: nationwide data and institutional experience. Anesthesiology. 2012;116:324–33. https://doi.org/10.1097/ALN.0b013e3182410b22.
Brinjikji W, Lanzino G, Rabinstein AA, Kallmes DF, Cloft HJ. Age-related trends in the treatment and outcomes of ruptured cerebral aneurysms: a study of the nationwide inpatient sample 2001–2009. AJNR Am J Neuroradiol. 2013;34:1022–7. https://doi.org/10.3174/ajnr.A3321.
Hoh BL, Chi Y-Y, Waters MF, Mocco J, Barker FG. Effect of weekend compared with weekday stroke admission on thrombolytic use, in-hospital mortality, discharge disposition, hospital charges, and length of stay in the Nationwide Inpatient Sample Database, 2002 to 2007. Stroke. 2010;41:2323–8. https://doi.org/10.1161/STROKEAHA.110.591081.
Washington CW, Derdeyn CP, Dacey RG, Dhar R, Zipfel GJ. Analysis of subarachnoid hemorrhage using the Nationwide Inpatient Sample: the NIS-SAH Severity Score and Outcome Measure. J Neurosurg. 2014;121:482–9. https://doi.org/10.3171/2014.4.JNS131100.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. https://doi.org/10.1097/00005650-199801000-00004.
Young B, Moyer M, Pino W, Kung D, Zager E, Kumar MA. Safety and feasibility of early mobilization in patients with subarachnoid hemorrhage and external ventricular drain. Neurocrit Care. 2019;31:88–96. https://doi.org/10.1007/s12028-019-00670-2.
Samuels O, Webb A, Culler S, Martin K, Barrow D. Impact of a dedicated neurocritical care team in treating patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2011;14:334–40. https://doi.org/10.1007/s12028-011-9505-z.
Pandey AS, Gemmete JJ, Wilson TJ, et al. High subarachnoid hemorrhage patient volume associated with lower mortality and better outcomes. Neurosurgery. 2015;77:462–70. https://doi.org/10.1227/NEU.0000000000000850.
Prabhakaran S, Fonarow GC, Smith EE, et al. Hospital case volume is associated with mortality in patients hospitalized with subarachnoid hemorrhage. Neurosurgery. 2014;75:500–8. https://doi.org/10.1227/NEU.0000000000000475.
Strickland BA, Mert M, Ravina K, et al. Discrepancy in neurologic outcomes following aneurysmal subarachnoid hemorrhage as a function of socioeconomic class. World Neurosurg. 2020;138:e787–94. https://doi.org/10.1016/j.wneu.2020.03.087.
Akintoye E, Briasoulis A, Egbe A, et al. Regional variation in mortality, length of stay, cost, and discharge disposition among patients admitted for heart failure in the United States. Am J Cardiol. 2017;120:817–24. https://doi.org/10.1016/j.amjcard.2017.05.058.
Larrew T, Pryor W, Weinberg J, et al. Aneurysmal subarachnoid hemorrhage: a statewide assessment of outcome based on risk factors, aneurysm characteristics, and geo-demography. J Neurointerv Surg. 2015;7:855–60. https://doi.org/10.1136/neurintsurg-2014-011359.
McIntyre MK, Gandhi C, Long A, et al. Age predicts outcomes better than frailty following aneurysmal subarachnoid hemorrhage: a retrospective cohort analysis. Clin Neurol Neurosurg. 2019;187:105558. https://doi.org/10.1016/j.clineuro.2019.105558.
Ross N, Hutchinson PJ, Seeley H, Kirkpatrick PJ. Timing of surgery for supratentorial aneurysmal subarachnoid haemorrhage: report of a prospective study. J Neurol Neurosurg Psychiatry. 2002;72:480–4. https://doi.org/10.1136/jnnp.72.4.480.
Awe OO, Gonzalez LF, Hasan D, Maltenfort M, Rossenwasser R, Jabbour P. Treatment outcome of aneurysmal subarachnoid hemorrhage in patients aged 70 years and older. Neurosurgery. 2011;68(3):753–8. https://doi.org/10.1227/NEU.0b013e318207a9fb.
Zacharia BE, Grobelny BT, Komotar RJ, Sander Connolly E, Mocco J. The influence of race on outcome following subarachnoid hemorrhage. J Clin Neurosci. 2010;17:34–7. https://doi.org/10.1016/j.jocn.2009.05.015.
Williamson T, Ryser MD, Ubel PA, et al. Withdrawal of life-supporting treatment in severe traumatic brain injury. JAMA Surg. 2020;155(8):723–31. https://doi.org/10.1001/jamasurg.2020.1790.
James ML, Grau-Sepulveda MV, Olson DM, et al. Insurance status and outcome after intracerebral hemorrhage: findings from Get With The Guidelines-stroke. J Stroke Cerebrovasc Dis. 2014;23:283–92. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.02.016.
Lai PMR, Dasenbrock H, Lin N, Du R. The impact of insurance status on the outcomes after aneurysmal subarachnoid hemorrhage. PLoS ONE. 2013;8:e78047. https://doi.org/10.1371/journal.pone.0078047.
Thompson NR, Fan Y, Dalton JE, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015;53:374–9. https://doi.org/10.1097/MLR.0000000000000326.
Simard M, Sirois C, Candas B. Validation of the combined comorbidity index of Charlson and Elixhauser to predict 30-day mortality across ICD-9 and ICD-10. Med Care. 2018;56:441–7. https://doi.org/10.1097/MLR.0000000000000905.
Gologorsky Y, Knightly JJ, Lu Y, Chi JH, Groff MW. Improving discharge data fidelity for use in large administrative databases. Neurosurg Focus. 2014;36:E2. https://doi.org/10.3171/2014.3.FOCUS1459.
Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5:143–51.
Funding
There are no funding sources to report.
Author information
Authors and Affiliations
Contributions
UVM BS: conception, data interpretation, article drafting, article revisions. HAK MD: conception, data analysis, data interpretation, article drafting. XZ MD: conception, data interpretation, article revisions, supervision. SS BA: data interpretation, article drafting. CHW MD: conception, data interpretation, article revisions, supervision. AHB MD: article revisions. MS MD: data interpretation, article revisions. NCB MD: article revisions, supervision. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts to report.
Ethical approval/informed consent
We have adhered to ethical guidelines. Institution review board approvals and use of informed consent does not apply.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mahajan, U.V., Khan, H.A., Zhou, X. et al. Predictors of In-Hospital Mortality and Home Discharge in Patients with Aneurysmal Subarachnoid Hemorrhage: A 4-Year Retrospective Analysis. Neurocrit Care 38, 85–95 (2023). https://doi.org/10.1007/s12028-022-01596-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01596-y