Abstract
Background
Although small series have suggested that younger age is associated with less favorable outcome after severe traumatic brain injury (TBI), confounders and biases have limited our understanding of this relationship. We hypothesized that there would be an association between age and mortality in children within an ongoing observational, cohort study.
Methods
The first 200 subjects from the Approaches and Decisions for Acute Pediatric TBI trial were eligible for this analysis (inclusion criteria: severe TBI (Glasgow Coma Scale [GCS] score ≤ 8], age 18 years, and intracranial pressure (ICP) monitor placed; exclusion: pregnancy). Children with suspected abusive head trauma (AHT) were excluded to avoid bias related to the association between AHT and mortality. Demographics, and prehospital and resuscitation events were collected/analyzed, and children were stratified based on age at time of injury (< 5, 5–< 11, 11–18 years) and presented as mean ± standard error of the mean (SEM). Analyses of variance were used to test the equality of the means across the group for continuous variable, and Chi-square tests were used to compare percentages for discrete variables (post hoc comparisons were made using t test and Bonferroni corrections, as needed). Kaplan–Meier curves were generated for each age subgroup describing the time of death, and log-rank was used to compare the curves. Cox proportional hazards regression models were used to assess the effect of age on time to death while controlling for covariates.
Results
In the final cohort (n = 155, 45 excluded for AHT), overall age was 9.2 years ± 0.4 and GCS was 5.3 ± 0.1. Mortality was similar between strata (14.0, 20.0, 20.9%, respectively, p = 0.58). Motor vehicle accidents were the most common mechanism across all strata, while falls tended to be more common in the youngest stratum (p = 0.08). The youngest stratum demonstrated increased incidence of spontaneous hypothermia at presentation and decreased hemoglobin concentrations and coagulopathies, while the oldest demonstrated lower platelet counts.
Conclusions
In contrast to previous reports, we failed to detect mortality differences across age strata in children with severe TBI. We have discerned novel associations between age and various markers of injury—unrelated to AHT—that may lead to testable hypotheses in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is the leading cause of trauma-related death and permanent disability. According to the Centers for Disease Control, an estimated 1.7 million TBIs occur in the USA annually with a tri-modal distribution of incidence—children 0–4 years, adolescents 15–19 years, and adults > 65 years—at highest risk [1]. Over the past decade, TBI-related emergency department visits increased by 70% [2]. Among children in the USA, TBI was responsible for 7440 deaths, 60,000 hospitalizations, and 600,000 emergency visits [3]. The economic burden of pediatric TBI is estimated to exceed $50 billion annually [3]. The Brain Trauma Foundation released guidelines for the management of severe pediatric TBI [4, 5], yet there is considerable management variability among practitioners of pediatric TBI [6]. In 2011, an international collaboration recommended a comparative effectiveness research approach with the overarching goal of improving and standardizing TBI management [7]. Fundamental to achieving this goal is to understand how TBI affects children across the age spectrum.
The association between age and outcome after TBI in children is poorly understood. It has been theorized that the plasticity of the immature brain could allow adaptations to the initial insults—leading to improved overall outcomes or even survival from severe injuries. This has not been borne out by the existing literature [8] as younger age has often been associated with worse outcome [9,10,11]. An analysis of 103 children with severe TBI revealed lower post-resuscitation GCS, more frequent hypotension, and higher mortality among children < 4 years [12]. However, a single-center series of children with severe TBI showed children < 5 years had better outcomes [13], while another spanning the entire injury range also found better outcomes in infants [14].
An important consideration in the assessment of age on outcomes in children with severe TBI is the confounding factor of abusive head trauma (AHT). Children with AHT likely have delay in seeking medical care, have less reliable medical historians, and may have chronic injuries. AHT has been shown to carry a worse prognosis than accidental TBI [15,16,17,18]. Similarly, previous studies of young children that showed a worse outcome for the youngest age group included both accidental injuries and AHT [12, 19]. To study the effect of age alone on mortality—as well the association with other clinical events—we chose to exclude children with AHT from our analysis.
We hypothesized that there was a relationship between age and mortality in children with severe TBI. To test this hypothesis, we analyzed data from the first 200 children of the approaches and decisions for acute pediatric TBI (ADAPT) trial. Secondarily, we assessed the association of injury characteristics and prehospital/resuscitation events and age.
Methods
The ADAPT trial is a comparative effectiveness study of children with severe TBI funded by a cooperative agreement with National Institute of Neurological Disorders and Stroke (U01 NS 081041). The overall goal of the study is to compare the effectiveness of strategies related to intracranial hypertension, secondary injuries, and metabolic support in 1000 children from multiple centers within the USA and abroad.
All sites obtained institutional review/ethics board approval, and the University of Pittsburgh received Institutional Review Board approval to coordinate the study. The design of the ADAPT trial is observational—sites care for children based on their local standards without any study-based interventions. Because of this study design and the scientific need to avoid without selection bias, all clinical sites were granted permission to collect data regarding the acute hospitalization on all children meeting inclusion/exclusion criteria (inclusion: age < 18 years, diagnosis of severe TBI [GCS score ≤ 8], and placement of intracranial pressure [ICP] monitor at study site; exclusion: pregnancy). Informed consent was obtained for follow-up activities. Therefore, the subjects within the overall study and this report represent consecutive eligible subjects admitted to study sites. Mortality was defined as death within the study period.
The first 200 subjects enrolled in the ADAPT trial (February 22, 2014–December 22, 2014) were studied. The analysis was intended to determine the factors associated with mortality in children with different mechanisms of injury—with a focus on the age of the subjects. Demographic characteristics, injury details/scores (Abbreviated Injury Scores [AIS], Injury Severity Scores, Pediatric Risk of Mortality [PRISM] III scores), prehospital events, and resuscitation events were analyzed. Definitions of these variables are provided in Supplementary table. Mortality and the cause of death as indicated by the medical records were identified. Prehospital events were defined as events that occurred from the time of the injury until presentation to the study hospital. Resuscitation phase of care was defined as from the time of admission to the clinical site until the ICP monitor was placed.
Data Stratification and Data Analysis
The age of subjects was defined at the time of ICP monitor placement. Children were stratified by age: < 5, 5–< 11, and 11–< 18 years. Children with any likelihood of child abuse were excluded. Briefly, clinical sites were asked to stratify children of any age based on the likelihood of abuse, as we have previously published. For this analysis, children with “Definite,” “Probable,” and “Possible” child abuse were excluded from this analysis (“Definite” indicates that medical record review demonstrates that the medical diagnosis of child abuse was made by a healthcare professional at the clinical site; “Probable” indicates that the diagnosis of child abuse was a part of the differential diagnosis of the clinical team, but a final diagnosis had not been made; and “Possible” indicates that there is documentation within the medical record that child abuse was being considered). The clinical characteristics are reported by age subgroup as means and standard errors for continuous variables and percentages for discrete variables. Analyses of variance were used to test the equality of the means across the group for continuous variable, and Chi-square tests were used to compare percentages for discrete variables. If significant differences were identified (p < 0.05), pairwise post hoc comparisons were made (t test for continuous variables, Chi-square for discrete variables), with a Bonferroni correction for multiple comparisons (p < 0.05/3). Kaplan–Meier curves were generated for each age subgroup describing the time of death of study participants. A log-rank was used to compare the curves. Cox proportional hazards regression models were used to assess the effect of age on time to death while controlling for covariates. Data in all tables are presented as mean (± SEM) unless otherwise noted.
Results
Of the first 200 subjects enrolled in the ADAPT trial, the 45 subjects (22.5%) with concern for abuse were excluded from this analysis. Of the remaining 155 subjects, 43 children were < 5 years, 45 children were 5–< 11 years, and 67 children were 11–< 18 years (Table 1). There was no difference in proportion of females in the 3 groups (34.9 vs. 40.0 vs. 31.3%, p = 0.641). With respect to race, 106 children were white, 31 were black, and 18 were classified as “other,” and there was an increased representation of white children in the two oldest cohorts when compared to the youngest cohort (48.8 vs. 73.3 vs. 76.1%, p = 0.02 overall; p = 0.042 for < 5 vs. 5–< 11 years, p = 0.082 for < 5 years vs. 11–< 18 years). As expected, the 3 groups differed significantly by weight (14.9 kg ± 0.5 vs. 29.4 kg ± 1.4 vs. 58.5 kg ± 2.1, p < 0.001 overall and across all groups). With respect to the cause of injury, 101 subjects were in motor vehicle collisions, 26 had falls, 4 had homicide/assault, and 24 were classified as “other.” There were trends in causes of injury among the different age groups, as the middle group tended to be more likely to be involved in a motor vehicle accident than to sustain a fall, but the trends did not reach statistical significance (p = 0.094). There were no differences in type of injury among the 3 groups but the oldest group was more likely to be under the influence of drugs (0 vs. 0 vs. 8.5%, p = 0.013). There were no differences between the three age groups with respect to transportation to the hospital, and there was no difference in GCS scores at the time of ICP monitor placement among the age groups (5.2 ± 0.3 vs. 5.6 ± 0.3 vs. 5.2 ± 0.2, p = 0.64).
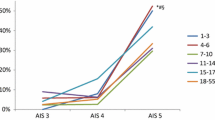
The relationship between age, injury characteristics, and prehospital events is shown in Table 2. The oldest group had increased Head AIS scores compared to the other two groups (4.0 ± 0.2 vs. 4.1 ± 0.1 vs. 4.4 ± 0.1, p = 0.040 overall; p = 0.049 for < 5 years vs. 11–< 18 years and p = 0.023 for 5–< 11 years vs. 11–< 18 years). The youngest group tended to have more apnea events (20.9 vs. 15.6 vs. 4.5%, p = 0.086), and there were no other differences among age groups with other prehospital events assessed.
The impact of age on measures during the resuscitation phase is shown in Table 3. Overall, there was a difference in the incidence of hypothermia between the groups (35.7 vs. 26.7 vs. 12.1%, p = 0.014 overall; p = 0.004 for < 5 years vs. 5–< 11 years and p = 0.05 for < 5 years vs. 11–< 18 years). Fluids administered (ml/kg/h) prior to ICP monitor placement was greater in the youngest group compared to the oldest (12.0 ± 1.3 vs. 8.5 ± 1.0), while fluid output was not different. There were several associations between the groups with respect to laboratory values. Compared to the oldest cohort, the youngest cohort had (i) lower hemoglobin concentrations (10.7 g/dl ± 0.3 vs. 11.8 g/dl ± 0.2, p = 0.003), (ii) greater incidence of abnormal partial thromboplastin time (PTT) (39.5 vs. 19.4%, p = 0.004), and (iii) greater incidence of abnormal international normalized ratio (INR) (27.9 vs. 17.9%, p = 0.005). The older cohort demonstrated lower platelet counts compared to the middle cohort (248 × 103 ± 10.9 vs. 297 × 103 ± 12.0, p = 0.006). Lastly, there were no differences in other events during the resuscitation phase among the age groups.
The association between age and PRISM III variables is shown in Table 4. While age-related differences in heart rate and blood pressures were observed, the highest recorded pH differed across the age strata and was lower in the youngest cohort compared to the oldest cohort (7.40 ± 0.01 vs. 7.44 ± 0.01, p = 0.011). Moreover, the highest blood urea nitrogen (BUN) and creatinine (Cr) varied among the 3 age strata (BUN: 12.6 mg/dl ± 0.6 vs. 14.4 mg/dl ± 0.6 vs. 14.3 mg/dl ± 1.4, p = 0.036 overall, p = 0.03 for < 5 vs. 5–< 11 years and p = 0.019 for < 5 vs. 11–< 18 years; Cr: 0.4 mg/dl ± 0.01 vs. 0.6 mg/dl ± 0.01 vs. 0.8 mg/dl ± 0.01, p < 0.0001 overall and between all groups). The neurological examination at the time the child qualified for the study is shown in Table 5. Of note, many aspects of the entire examination were not tested for a large proportion of the overall population.
Uncorrected mortality rates of the 3 age groups were not different (14.0 vs. 20.0 vs. 20.9%). Cox proportional hazard ratio [HR, referenced to < 5 years] for the middle cohort = 1.469; HR for oldest cohort = 1.544, p = 0.660. After adjusting for potential confounders, the HR for cohorts was not significantly different (HR = 1.407 and 1.192, respectively, p = 0.906).
Discussion
The current evidence-based guidelines for management of severe TBI in children were developed to make recommendations for children across the entire age spectrum, and the overall goals of the ADAPT trial are to expand these guidelines for clinicians and researchers. With the exception of cerebral perfusion pressure thresholds, none of the guidelines attempt to account for differences in ages of the children who were injured despite the widely held belief that treatment recommendations for infants and teenagers may need to differ [5]. However, the existing literature that informs the guidelines are simply insufficient to describe how age affects outcomes after severe TBI in children. We undertook the current study to describe the association between age and mortality and included a number of other variables to try to define characteristics of the various age groups. In this relatively large cohort of 155 children with severe TBI who underwent intracranial monitoring, we did not find a difference in mortality between subjects across 3 age strata that have been previously observed.
The relationship between young age and outcome after neurological insults has a long history in developmental neuroscience. Some suggest that since dendritization, myelination, and synaptogenesis occur early during development, early insults may be better tolerated because these developmental processes can adapt [20,21,22,23]. This “early plasticity theory” would suggest younger animals may have improved outcomes after an injury. On the contrary, others argue that an injury during this developmental stage may lead to a more vulnerable brain as these developmental processes are disrupted [24,25,26,27,28,29]. As these developmental processes continue over many years, we chose to study mortality in our large cohort study to start to identify factors that might have an impact on this more immediate outcome.
To date, our study represents one of the larger cohorts to interrogate the relationship between age and mortality in children with severe TBI. Levin studied 103 children with severe TBI and found that children < 4 years had the highest mortality (almost 80% at 1 year after injury) and children 5–10 years had the lowest (~ 20%) [12]. However, they did not control for covariates and likely included children with abusive head trauma, in contrast to our work. Their high mortality rates in the youngest cohort could be explained because this cohort (i) had lower GCS scores, (ii) worse pupillary examination, (iii) more surgically evacuated lesions, (iv) increased shock, and (v) higher ICPs. Similarly, Michaud reported that mortality was highest in children < 2 years (50%) compared to older children (35% for 3–14 years; 14% for > 14 years) [19]. In regression analysis, they found injury severity scores and pupillary examination were the most significant predictors of mortality. In contrast to these studies, we found no differences in mortality across similar age strata, with the youngest cohort exhibiting a nonsignificant trend toward lower mortality. In a very large cohort, Morrison and colleagues analyzed 16,000 children in the National Pediatric Trauma Registry and showed a higher mortality in the prepubertal group (0–7 years) while controlling for other contributing factors [30]. However, this study included mild/moderate/severe TBI children with a concomitantly low mortality rate (5%). Most consistent with our findings, Berger and colleagues found a nonsignificant trend of decreased mortality in children < 5 years compared to those 6–10 and 11–17 years (25 vs. 42.8 vs. 35.7%) in 37 children [13].
Of interest, two large, French studies have addressed the relationship between age and other characteristics with outcomes. In the first report, Ducrocq and colleagues interrogated a trauma registry to determine early predictive factors associated with outcome in children with TBI [10]. The investigators state that the children (n = 585) all had severe TBI—yet the median GCS was 6 with an interquartile ratio from 3 to 8—indicating that at least some of the subjects might have had a post-resuscitation GCS > 8. Nevertheless, analysis of this large cohort indicated that age < 2 years was associated with increased mortality independent of other risk factors. Similarly, Tude Melo and colleagues studied 315 children from the same Parisian trauma center over a 6-year period [11]. In this series, mortality rate was quite high (30%), and the investigators found that age < 2 and other factors (initial GCS score ≤ 5, accidental hypothermia, hyperglycemia, and coagulation disorders) were independent risk factors for mortality. However, they found that children < 2 years of age had a very high mortality rate (47%) despite resuscitation and transportation to the hospital by highly trained personnel. Neither report indicated whether child abuse was suspected in this young cohort—thereby making direct comparison with our data difficult.
To put our association between age and mortality into context with these other studies, the differences between studies are likely due to differences in inclusion/exclusion criteria (the requirement for placement of an ICP monitor and the exclusion of AHT children), clinical practice differences over different time epochs as neurotrauma care has improved, and the ability of studies to use statistical adjustments for measured covariates. An important consideration in comparing our work to previous studies is the decision to include or exclude children with abusive head trauma. Results from several studies show worse outcome in abusive head trauma (AHT), although many were limited by the same factors of other papers related to age: limited sample size (implying limited statistical power to detect differences) and other study design flaws such as selection bias related to patient recruitment [16,17,18, 31]. Since AHT are undoubtedly part of the youngest cohort in any analysis, this would obviously lead to worse outcomes in this youngest group [32]. To avoid these pitfalls and to more fully explore the epidemiology age in children with severe TBI without being overwhelmed by the effect of AHT, we did not include abuse in this analysis. Interestingly, even after excluding children with AHT—a condition whereby caregivers often refuse to seek medical care in a timely manner—we still detected differences in hospital transport across the age strata.
Within our comprehensive assessments of this cohort, we found associations between age and the various factors that could be potential hypotheses for the field to explore. Some of these associations are quite expected—weight, heart rates, blood pressure, and measures of renal function differ by age—but still emphasize that clinicians caring for children across the entire age range will need to account for these factors. Other associations were quite novel and could impact care and outcomes. For example, the youngest children were more likely to have presented with hypothermia during the resuscitation phase compared to older children. This may be due to developmental differences in temperature regulation during resuscitation, differences in injury severity, or a result of exposure in infants with increased surface area/volume. The impact of spontaneous hypothermia early after injury is uncertain, despite several randomized control trials attempting to study its effects [33,34,35]. We detected associations between hematopoietic system and age, with younger subjects demonstrating alterations in hemoglobin, PTT, and INR and the oldest children demonstrating lower platelet counts. These findings need to be explored to establish why these associations manifest in the different age groups.
There are limitations to our study. The most important is the possibility of a type 2 error, concluding that age and mortality are unrelated when an association actually exists. Because this analysis represents one of the larger cohorts to date, this concern is somewhat mitigated and we expect that an analysis of the full cohort of 1000 children may be more illustrative. It is also possible that medical decisions, such as those related to withdrawal of life support, could also be influenced by the age of the child. Our completed study will assess outcomes based on Glasgow Outcome Scale-Extended for Pediatrics, which may assist us in understanding the extent of this limitation. Our study is necessarily biased toward children who meet our inclusion criteria—with ICP monitoring being required to be a part of this study. It is possible that there is an inherent bias within the sites where ICP monitoring is more or less likely to occur. Unfortunately, there is no way for us to know how this bias influences our results. As a corollary to this limitation, children who were deemed too severely injured benefit from ICP monitoring—thereby underestimating the mortality of overall TBI in the broader population at the clinical sites. Because our overall study design of ADAPT was to determine the effectiveness of ICP-derived therapies (among others), we believe that our choice for inclusion/exclusion was warranted despite this potential bias for this study. Lastly, we did not account for premorbid conditions for this analysis as has been done by others [36, 37]. We do anticipate performing this type of analysis on the larger cohort when all outcome information is available to us.
In conclusion, we failed to detect differences in mortality in children of differing ages with severe TBI as others have done in the past. We have also found several provocative associations that will need to be confirmed in larger cohorts and other populations of children. We feel that the work of understanding how age affects outcomes—including secondary injury characteristics, mortality, and eventually functional outcomes—is essential to understand the natural history of the disease. It is only with analyses such as ours that we can advance toward a more patient-centered approach to care for children across the entire age range.
References
CDC. Traumatic Brain Injury in the United States, emergency department visits, hospitalizations, and deaths. [cited January 7, 2016] http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf.
CDC. Traumatic brain injury in the United States: Fact Sheet.
Stanley RM, Bonsu BK, Zhao W, et al. US estimates of hospitalized children with severe traumatic brain injury: implications for clinical trials. Pediatrics. 2012;129(1):e24–30.
Carney NA, Chesnut R, Kochanek PM. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med. 2003;4(3 Suppl):S1.
Kochanek PM, Carney N, Adelson PD, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents–second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1–82.
Dean NP, Boslaugh S, Adelson PD, et al. Physician agreement with evidence-based recommendations for the treatment of severe traumatic brain injury in children. J Neurosurg. 2007;107(5 Suppl):387–91.
Tosetti P, Hicks RR, Theriault E, et al. Toward an international initiative for traumatic brain injury research. J Neurotrauma. 2013;30(14):1211–22.
Taylor HG, Alden J. Age-related differences in outcomes following childhood brain insults: an introduction and overview. J Int Neuropsychol Soc. 1997;3(6):555–67.
Anderson V, Catroppa C, Morse S, et al. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116(6):1374–82.
Ducrocq SC, Meyer PG, Orliaguet GA, et al. Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med. 2006;7:461–7.
Tude Melo JR, DiRocco F, Blanot S, et al. Mortality in children with severe head trauma: predictive factors and proposal for a new predictive scale. Neurosurgery. 2010;67:1542–7.
Levin HS, Aldrich EF, Saydjari C, et al. Severe head injury in children: experience of the Traumatic Coma Data Bank. Neurosurgery. 1992;31(3):435–43 (discussion 443–434).
Berger MS, Pitts LH, Lovely M, et al. Outcome from severe head injury in children and adolescents. J Neurosurg. 1985;62(2):194–9.
Crowe LM, Catroppa C, Babl FE, et al. Timing of traumatic brain injury in childhood and intellectual outcome. J Pediatr Psychol. 2012;37(7):745–54.
Keenan HT, Runyan DK, Marshall SW, et al. A population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury. Pediatrics. 2004;114(3):633–9.
Prasad MR, Ewing-Cobbs L, Swank PR, et al. Predictors of outcome following traumatic brain injury in young children. Pediatr Neurosurg. 2002;36(2):64–74.
Ewing-Cobbs L, Kramer L, Prasad M, et al. Neuroimaging, physical, and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics. 1998;102(2 Pt 1):300–7.
Hymel KP, Makoroff KL, Laskey AL, et al. Mechanisms, clinical presentations, injuries, and outcomes from inflicted versus noninflicted head trauma during infancy: results of a prospective, multicentered, comparative study. Pediatrics. 2007;119(5):922–9.
Michaud LJ, Rivara FP, Grady MS, et al. Predictors of survival and severity of disability after severe brain injury in children. Neurosurgery. 1992;31(2):254–64.
Goldman PS, Galkin TW. Prenatal removal of frontal association cortex in the fetal rhesus monkey: anatomical and functional consequences in postnatal life. Brain Res. 1978;152(3):451–85.
Kennard MA. Age and other factors in motor recovery from precentral lesions in monkeys. Am J Physiol. 1936;115(1):138–46.
Kolb B, Gibb R. Possible anatomical basis of recovery of function after neonatal frontal lesions in rats. Behav Neurosci. 1993;107(5):799–811.
Villablanca JR, Carlson-Kuhta P, Schmanke TD, et al. A critical maturational period of reduced brain vulnerability to developmental injury. I. Behavioral studies in cats. Brain Res Dev Brain Res. 1998;105(2):309–24.
Anderson V, Spencer-Smith M, Wood A. Do children really recover better? Neurobehavioural plasticity after early brain insult. Brain. 2011;134(Pt 8):2197–221.
Bittigau P, Sifringer M, Pohl D, et al. Apoptotic neurodegeneration following trauma is markedly enhanced in the immature brain. Ann Neurol. 1999;45(6):724–35.
Giza CC, Prins ML. Is being plastic fantastic? Mechanisms of altered plasticity after developmental traumatic brain injury. Dev Neurosci. 2006;28(4–5):364–79.
Kolb B, Cioe J, Whishaw IQ. Is there an optimal age for recovery from motor cortex lesions? I. Behavioral and anatomical sequelae of bilateral motor cortex lesions in rats on postnatal days 1, 10, and in adulthood. Brain Res. 2000;882(1–2):62–74.
Kolb B, Gibb R, van der Kooy D. Neonatal frontal cortical lesions in rats alter cortical structure and connectivity. Brain Res. 1994;645(1–2):85–97.
Sifringer M, Stefovska V, Zentner I, et al. The role of matrix metalloproteinases in infant traumatic brain injury. Neurobiol Dis. 2007;25(3):526–35.
Morrison WE, Arbelaez JJ, Fackler JC, et al. Gender and age effects on outcome after pediatric traumatic brain injury. Pediatr Crit Care Med. 2004;5(2):145–51.
Ewing-Cobbs L, Prasad M, Kramer L, et al. Acute neuroradiologic findings in young children with inflicted or noninflicted traumatic brain injury. Childs Nerv Syst. 2000;16(1):25–33 (discussion 34).
Davies FC, Coats TJ, Fisher R, et al. A profile of suspected child abuse as a subgroup of major trauma patients. Emerg Med J. 2015;32(12):921–5.
Adelson PD, Wisniewski SR, Beca J, et al. Comparison of hypothermia and normothermia after severe traumatic brain injury in children (Cool Kids): a phase 3, randomised controlled trial. Lancet Neurol. 2013;12(6):546–53.
Hutchison JS, Ward RE, Lacroix J, et al. Hypothermia therapy after traumatic brain injury in children. New Engl J Med. 2008;358(23):2447–56.
Adelson PD, Ragheb J, Kanev P, et al. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery. 2005;56(4):740–54 (discussion 740–754).
Moran LM, Babikian T, Del Piero L, et al. The UCLA study of predictors of cognitive functioning following moderate/severe pediatric traumatic brain injury. J Int Neuropsychol Soc. 2016;22(5):512–9.
Treble-Barna A, Zang H, Zhang N, et al. Observed parent behaviors as time-varying moderators of problem behaviors following traumatic brain injury in young children. Dev Psychol. 2016;52(11):1777–92.
Acknowledgments
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number U01 NS081041. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Investigators for the ADAPT trial are Shruti Agrawal, Addenbrookes Hospital, Cambridge, UK; Sarah Mahoney, Alder Hey Children’s NHS Foundation Trust, Liverpool, UK; Deepak Gupta, All India Institute of Medical Sciences, New Delhi, India; John Beca, Auckland DHB Charitable Trust, Starship Children’s Hospital, Auckland, NZ; Laura Loftis, Baylor College of Medicine, Houston, TX; Kevin Morris, Birmingham Children’s Hospital NHS Foundation Trust, Birmingham, UK; Lauren Piper, Levine Children’s Hospital, Charlotte, NC; Anthony Slater, Children’s Health Queensland Hospital and Health Service, Brisbane, Australia; Karen Walson, Children’s Healthcare of Atlanta, Atlanta, GA; Tellen Bennett, Children’s Hospital Colorado, Aurora, CO; Todd Kilbaugh, Children’s Hospital of Philadelphia, Philadelphia, PA; AM Iqbal O’Meara, Children’s Hospital of Richmond, Richmond, VA; Nathan Dean, Children’s National Medical Center, Washington, DC; Ranjit S. Chima, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH; Katherine Biagas, Columbia University, New York, NY; Enno Wildschut, Erasmus Medical Center, Rotterdam, Netherlands; Mark Peters, Great Ormond St Hospital NHS Foundation Trust, London, UK; Kerri LaRovere, Boston Children’s Hospital, Boston, MA; Joan Balcells, Hospital Vall d’Hebron, Barcelona, Spain; Courtney Robertson, John Hopkins University, Baltimore, MD; Shira Gertz, Joseph M. Sanzari Children’s Hospital at Hackensack University Medical Center, Hackensack, NJ; Akash Deep, King’s College Hospital NHS Foundation Trust, London, UK; Sian Cooper, Leeds Teaching Hospitals NHS Trust, Leeds, UK; Mark Wainwright, Lurie Children’s Hospital, Chicago IL; Sarah Murphy, Massachusetts General Hospital, Boston, MA; John Kuluz, Miami Children’s Hospital, Miami, FL; Warwick Butt, Murdoch Children’s Research Institute, Royal Children’s Hospital, Melbourne, Australia; Nicole O’Brien, Nationwide Children’s Hospital, Columbus, OH; Neal Thomas, Pennsylvania State University, Hershey, PA; Sandra Buttram, Phoenix Children’s Hospital, Phoenix, AZ; Simon Erickson, Princess Margaret Hospital, Perth, Australia; J. Mahil Samuel, Royal Manchester Children’s Hospital NHS Foundation Trust, Manchester, UK; Rachel Agbeko, The Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK; Richard Edwards, University Hospital Bristol NHS Foundation Trust, Bristol, UK; Kesava Ananth Ramakrishnan, University Hospital Southampton NHS Foundation Trust, Southampton, UK; Margaret Winkler and Santiago Borasino, University of Alabama at Birmingham, Birmingham, AL; Joanne Natale, University of California, Davis, Sacramento, CA; Christopher Giza, University of California, Los Angeles, Los Angeles, CA; Mary Hilfiker and David Shellington, University of California, San Diego, San Diego, CA; Anthony Figaji, Red Cross War Memorial Children’s Hospital, Cape Town, South Africa; Elizabeth Newell, University of Iowa Children’s Hospital, Iowa City, IA; Edward Truemper, University of Nebraska Medical Center and Nebraska Medical Center, Omaha, NE; Robert Clark, University of Pittsburgh, Pittsburgh, PA; Kit Newth, Children’s Hospital of Los Angeles, Los Angeles, CA; Nadeem Shafi, LeBonheur Children’s Hospital, Memphis, TN; Darryl Miles, University of Texas Southwestern Medical Center, Dallas, TX; Michelle Schober, University of Utah, Jerry Zimmerman, University of Washington, Seattle, WA; Peter Ferrazzano, University of Wisconsin, Madison, WI; Jose Pineda, Washington University–St. Louis, St. Louis, MO; and Ajit Sarnaik, Wayne State University, Detroit, MI.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sarnaik, A., Ferguson, N.M., O’Meara, A.I. et al. Age and Mortality in Pediatric Severe Traumatic Brain Injury: Results from an International Study. Neurocrit Care 28, 302–313 (2018). https://doi.org/10.1007/s12028-017-0480-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0480-x