Abstract
Background
Activated prothrombin complex concentrates factor eight inhibitor bypassing activity (FEIBA) has been recommended for reversing novel oral anticoagulants (NOAC) in the context of intracerebral hemorrhage (ICH), though few clinical studies report its use.
Methods
A prospective study of patients with spontaneous ICH was conducted from May 2013 to May 2015. Hospital complications including hemorrhage (gastrointestinal bleeding, anemia requiring transfusion, and surgical site bleeding) and thrombosis (pulmonary embolus, deep vein thrombosis, ischemic stroke, and myocardial infarction) were recorded. All ICH patients underwent baseline head CT and a follow-up stability scan in 6 h. NOAC taken within 48 h of presentation was reversed with FEIBA (50 u/kg) per protocol. Three-month outcomes were assessed using the modified rankin score (mRS).
Results
Of 127 ICH patients enrolled, 6 (5 %) had NOAC-related ICH including: oral factor XA inhibitor N = 5 (4 %; N = 4 rivaroxaban, N = 1 apixaban] and direct thrombin inhibitor N = 1 (0.8 %; dabigatran). The indication for NOAC was atrial fibrillation in all patients and the median CHADS2–VASC score was 4 (range 2–5). The median admission NIHSS was 2 (range 0–14) and the median ICH volume was 8 mL (range 1–20). Five patients (3 rivaroxaban, 1 apixaban, 1 dabigatran) presented within 48 h and received FEIBA within a median of 13 h (range 10–29 h) from their last NOAC dose and 8 h (range 4.5–20) from the time last known well. None of the patients had ICH expansion, hemorrhagic, or thrombotic complications. Three-month median mRS was 1 (range 0–6).
Conclusion
In this small case series, reversal of NOAC with FEIBA was not associated with ICH expansion or any thrombotic or hemorrhagic complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
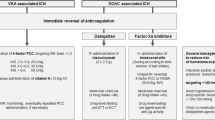
Atrial fibrillation is a major risk factor for ischemic strokes. Its prevalence is on the rise due to an aging population [1]. Vitamin K antagonists such as warfarin have been the mainstay of drug therapy to prevent embolic events related to atrial fibrillation [2]. However, limitations of warfarin include its narrow therapeutic window, requirement of frequent blood testing, drug and food interactions, and hemorrhagic adverse events. The most feared complication of warfarin therapy is intracerebral hemorrhage (ICH), which carries a high morbidity and mortality rate (65 %) [3]. Novel oral anticoagulants (NOACs) such as direct thrombin inhibitors (dabigatran) and oral factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban) have been FDA approved in recent years for prevention of cardioembolic strokes in patients with non-valvular atrial fibrillation among other indications for their use [4–6]. NOACs are proven at least as effective as warfarin in preventing strokes, with less risk of hemorrhage, wider therapeutic range, shorter half-lives, and no required blood testing [7]. Although the risk of ICH is significantly less with some NOACs than with warfarin, no reversal agents or effective antidotes are available to date. The recent American Heart Association guidelines on management of spontaneous ICH in setting of NOACs suggest the use of factor eight inhibitor bypassing activity (FEIBA) as a potential reversal agent (Class IIb, level C) [8]. FEIBA is an activated prothrombin complex concentrate, which contains activated factors II, VII, IX, and X [9]. The evidence for the use of FEIBA in counteracting coagulopathy in NOAC-related ICH is mainly based on animal and healthy volunteer studies assessing laboratory endpoints, rather than radiographic or clinical outcomes. We report five cases of NOAC-related ICH treated with FEIBA in our tertiary care center along with a review of the existing literature.
Methods
Study Population
We retrospectively reviewed prospectively collected data on patients admitted with spontaneous ICH to the Cleveland Clinic Neurocritical care unit between May 2013 and May 2015. Inclusion criteria for the study database were: age ≥ 18 years, ICH diagnosed by brain computed tomography (CT), and admission to the neurological ICU within 14 days of initial intracranial hemorrhage. Exclusion criteria were: traumatic or postoperative ICH. The local institutional review board approved the study. All patients or their surrogate decision makers were consented for participation in this study.
Patient Assessments
The following data were prospectively collected: demographics including age, gender, medical history, pre-morbid functional status, admission glasgow coma scale, national institute of health stroke scale (NIHSS), ICH score, and baseline medications. Admission laboratory findings were recorded including: the PT, INR, aPTT, creatinine, platelet count, and chromogenic factor Xa assay (as available). NOAC taken within 48 h of presentation with ICH was reversed with FEIBA (50 u/kg). This dose was selected based on studies in healthy volunteers, which have shown partial or complete reversal of rivaroxaban-induced coagulation abnormalities using FEIBA doses ranging from 25 to 80 u/kg [10, 11]. Additionally, case reports of FEIBA to reverse dabigatran-associated life-threatening bleeding have used doses ranging from 26 to 100 u/kg [12–14]. However, when only 26 u/kg was administered, an additional 16 u/kg was required due to the concern for ongoing bleeding [15]. The European Heart Rhythm Association and others have suggested a dose of 50 u/kg of FEIBA for dabigatran-associated bleeding. Because the risk of thrombotic events and DIC increases with higher doses, 50 u/kg of FEIBA were selected [16]. Adjustments for renal or hepatic insufficiency are not required. Hospital complications including hemorrhage (gastrointestinal bleeding, anemia requiring transfusion, and surgical site bleeding) and thrombosis (deep vein thrombosis, pulmonary embolus, ischemic stroke, and myocardial infarction) were recorded. Hemorrhagic complications were recorded because FEIBA is not a specific antidote to oral direct factor Xa inhibitors or direct thrombin inhibitors. It is conceivable that incomplete coagulopathy reversal could occur, leading to hemorrhagic complications. At ICU admission, all patients received a screening EKG and three sets of cardiac enzyme measurements 8 h apart. If cardiac enzyme levels were elevated, additional levels were measured serially every 8 h. Screening venous compression ultrasound was not performed in accordance with published guidelines [17, 18]. In patients who developed symptoms of venous thromboembolism (hypoxia, chest pain, lower extremity swelling, or unexplained fever) venous ultrasound and/or chest angiography were performed.
All ICH patients underwent admission brain CT and a follow-up stability scans in 6 h to assess for hematoma expansion. ICH volumes were calculated using the ABC/2 method. The final etiology of the ICH was adjudicated by the Neuro ICU attendings caring for the patient after review of the clinical and radiographic data. Three-month outcomes were assessed using the modified rankin score (mRS) by telephone interview following hospital discharge.
Results
A total of 127 ICH patients were identified and met our inclusion criteria including: 92 non-coagulopathic patients (72 %), 29 warfarin-related ICH patients (23 %), and six NOAC-related ICH patients (5 %). The NOAC-related ICH group was further categorized based on the specific NOAC used and included five patients on oral factor Xa inhibitors (four patients on rivaroxaban, one patient on apixaban) and one patient with dabigatran-related ICH. The median pre-morbid mRS was similar across groups: 0 (range 0–3) for the non-coagulopathic group, 0 (range 0–5) for the warfarin group, and 0 (range 0–3) for the NOAC group. Admission NIHSS was lower in the NOAC group (2, range 0–14) compared to the warfarin (8, range 0–32) and non-coagulopathic (8, range 0–33) groups. The median ICH volume was also smaller in the NOAC group (8 mL, range 1–20) compared to the warfarin (9 mL, range 1–123 mL) and non-coagulopathic (14 mL, range 1–112 mL) groups.
Five patients (3 rivaroxaban, 1 apixaban, and 1 dabigatran) presented within 48 h of the last NOAC dose and received FEIBA within a median of 13 h (range 10–29 h) from the last NOAC dose, and 8 h (range 4.5–20) from the last known well time. No patient had renal or liver insufficiency that would prolong NOAC clearance. The indication for NOAC use in all patients was atrial fibrillation, and the median CHADS2–Vasc score was four (range 2–5). The median time from last known well to the first head CT was 8 h (range 1–19 h). Pertinent demographics, medications, laboratory findings, ICH location and etiology, hospital and discharge outcomes are listed in Table 1.
Case 1 is a 49-year-old man with a past medical history of coronary artery disease, diabetes mellitus, hypertension, refractory atrial fibrillation (CHADS2–Vasc score 2), and cardiac ablation complicated by pulmonary vein stenosis. He presented initially for cardiac catheterization and dilation of a pulmonary vein. He was taking rivaroxaban 20 mg daily and aspirin 81 mg daily prior to admission. Post procedure, the patient complained of a mild headache and right homonymous hemianopia. His pre-morbid mRS was 0, initial NIHSS was 2, ICH score was 0, INR 1.2, and platelet count was 235 × 103/µL. The time from last known well to the first CT brain was 8 h. A CT scan of the brain without contrast revealed a 6 mL left occipital ICH without intraventricular hemorrhage (Fig. 1(1a)). He received FEIBA 50 u/kg (3210 units) 13 h from his last dose of rivaroxaban, and 10 h from his last known well time. His follow-up head CT without contrast showed no expansion of the ICH (Fig. 1(1b)). His hospital course was uneventful and he was discharged home with a follow-up 3-month mRS of 0.
Case 2 is an 81-year-old woman with hypertension, a remote history of non-Hodgkin’s lymphoma for which she received chemotherapy and radiation, and atrial fibrillation (CHADS2–Vasc score of 4). She presented with confusion and headache and was taking rivaroxaban 20 mg once a day. Her pre-morbid mRS was 0, initial NIHSS was 2, ICH score was 1, INR 1.1, and platelet count 225 × 103/µL. The time from last known well to the first CT brain was 19 h. CT scan of the brain without contrast showed a 10 mL left parietal ICH (Fig. 1(2a)). She received FEIBA 50 u/kg (4355 units) 29 h from her last dose of rivaroxaban, 20 h from her last known well time. Follow-up head CT scan without contrast showed no expansion of the ICH (Fig. 1(2b)). Her hospital course was uneventful and she was discharged to a skilled nursing facility for physical therapy. Her 3-month mRS was 1.
Case 3 is an 81-year-old man with hypertension, Parkinson’s disease, previous stroke, renal cell carcinoma status post nephrectomy, prostate cancer status post prostatectomy, and atrial fibrillation (CHADS2–Vasc score of 5). He presented with right hemiparesis and confusion on rivaroxaban (20 mg daily) and aspirin (81 mg daily). His pre-morbid mRS was three, initial NIHSS was 14, ICH score was 1, INR 1.3, and platelet count 209 × 103/µL. The time from last known well to the first CT brain was 1 h CT scan of the brain without contrast showed an 8 mL left basal ganglia ICH without intraventricular extension (Fig. 1(3a)). The time from last known well to the first CT brain was 1 h He received FEIBA 50 u/kg (4245 units) ,10 h from his last dose of rivaroxaban, and 4.5 h from his last known well time and 1 pool of platelets. The initial rivaroxaban assay was elevated at 3.03 (normal < 0.10 IU/mL) 2 h after the FEIBA infusion. Due to risk of rebleed and after consultation with the hematology team, an additional 25 u/kg dose (2064 units) was given 6 h later. The follow-up rivaroxaban assay was 0.21 IU/mL 3 h after the second infusion. Repeat CT scan of the brain without contrast showed no expansion of the ICH (Fig. 1(3b)). There were no hemorrhagic or thrombotic complications during his hospitalization, and the patient was discharged to a skilled nursing facility. His 3-month mRS was six.
Case 4 is an 81-year-old woman with hypertension and atrial fibrillation (CHADS2–Vasc score of 4). She presented with sudden onset of dizziness and gait instability on apixaban 2.5 mg twice a day and aspirin 81 mg once a day. Her pre-morbid mRS was 0, initial NIHSS was 0, ICH score was 2, INR 1.0, and platelet count 255 × 103/µL. The time from last known well to the first CT brain was 2 h. CT of the brain without contrast showed a 1.5 mL right cerebellar hemorrhage (Fig. 1(4a)). She received FEIBA 50 u/kg (3174 units) 13 h from her last dose of apixaban, 6 h from her last known well time. Her follow-up CT scan of the brain without contrast showed no expansion of the ICH (Fig. 1(4b)), and her hospital course was uneventful. She was discharged home and her 3-month mRS was 1.
Case 5 is a 69-year-old man with hypertension, hyperlipidemia, coronary artery disease status post coronary artery bypass grafting, ventricular fibrillation arrest with an implantable cardioverter defibrillator, and paroxysmal atrial fibrillation status post prior ablation (CHADS2–Vasc score of 3). He presented with sudden onset headache and right homonymous hemianopia on dabigatran 150 mg twice a day and aspirin 81 mg daily. His pre-morbid mRS was 0, initial NIHSS was 2, ICH score was 0, INR 1.2, and platelet count 198 × 103/µL. His CT scan of the brain without contrast showed a 20 mL left occipital hemorrhage (Fig. 1(5a)) The time from last known well to the first CT brain was 8 h. He received FEIBA 50 u/kg (4500 units) 12 h from his last dabigatran dose, 8 h from his last known well time. Follow-up CT scan of the brain without contrast showed no expansion of the ICH (Fig. 1(5b)). He was discharged home and his 3-month mRS was 1.
None of the patients who received FEIBA had ICH expansion on follow-up head CT, hemorrhagic, or thrombotic complications. At 3-month follow-up, the median mRS was 1 (range 0–6) in FEIBA-treated NOAC patients, versus mRS 4 (range 0–6) in non-coagulopathic patients, and mRS 4 (range 0–6) in warfarin-associated ICH patients.
Discussion
To our knowledge, this is one of the first case series of patients with NOAC-related ICH who were treated with FEIBA to reverse drug-induced coagulopathy. Overall, 5 % of our cohort had NOAC-associated ICH. It should be noted, however, that four of five patients were taking aspirin in addition to a NOAC, which may increase the risk of ICH. We found no radiographic ICH expansion following FEIBA, and no thrombotic or hemorrhagic complications. NOAC-associated ICH tended to be less severe (as measured by admission NIHSS and ICH volume) than VKA-associated or non-coagulopathic ICH. This is likely by chance, given the small number of NOAC-associated hemorrhages in this series, but merits further evaluation in larger multicentered studies. The evidence to date on FEIBA reversal for NOAC-associated ICH is based on case reports (involving a variety of types of hemorrhages), healthy volunteers, and animal studies.
A case series of four patients on dabigatran treated with FEIBA included patients with life-threatening subdural hematoma, iatrogenic pericardial effusion, upper gastrointestinal bleeding, and basal ganglia ICH. In the ICH case, FEIBA was given 17 h after the last dose of dabigatran and hematoma size was noted to increase by 11.4 mL on follow-up head CT three days after onset [12]. The Northwestern Emergency Medicine Residency group [19] also reported the use of FEIBA in two cases of NOAC-related life-threatening hemorrhage. One patient with atrial fibrillation and a subdural hematoma received FEIBA to reverse dabigatran and had no interval progression of the subdural hematoma on repeat CT scan. The second patient with atrial fibrillation on rivaroxaban was found to have a retroperitoneal hemorrhage with a ruptured iliac artery aneurysm. This patient received FEIBA prior to open repair surgery along with multiple units of platelets and cryoprecipitate. The patient had no complications and resumed rivaroxaban on hospital day 10. An additional case report describes a patient with traumatic subdural hematoma on rivaroxaban, for which FEIBA was used prior to drainage. The surgery was uncomplicated, with no reported bleeding events [20]. Other case reports describe the successful use of FEIBA in reversing coagulopathy associated with dabigatran and include cases of iatrogenic pericardial effusion following ablation [15], urgent percutaneous trans-hepatic drainage of a gallbladder empyema [13], and emergent surgery for an incarcerated femoral hernia [14].
Apart from case reports, other studies have examined the ability of FEIBA to reverse laboratory markers of NOAC-induced coagulopathy. An ex vivo study [10] randomized ten healthy, white, male subjects to receive either rivaroxaban or dabigatran and then receive the other anticoagulant after a 15-day washout period. Prothrombin complex concentrate (PCC), Recombinant activated Factor VII (rfVIIa), or FEIBA were used for reversal of anticoagulation. Endogenous thrombin potential, maximum concentration of thrombin, thrombin lag time, and time to reach the maximum concentration of thrombin were measured. The authors found that low doses FEIBA appeared to correct coagulation abnormalities associated with both dabigatran and rivaroxaban, while PCC and rfVIIa led to incomplete correction. Higher doses of FEIBA and PCC led to overcorrection, which could place patients at risk of thrombosis. An in vitro study of the effects of FEIBA, PCC, and rVIIa on healthy volunteer blood spiked with dabigatran found that FEIBA considerably shortened the clotting time compared to rFVIIa or PCC [21]. Similarly, FEIBA has been shown to reverse thrombin generation parameters in the plasma of eight healthy volunteers exposed to dabigatran [22]. Another in vitro study examined changes in the PT, thrombin generation assay and clotting time (CT) in rivaroxaban-exposed healthy subjects treated with FEIBA, PCC, or rFVIIa [11]. All three agents were at least partially effective in reversing laboratory parameters of coagulopathy. Recombinant fVIIa and FEIBA were more effective in reversing the PT, clotting time and lag time of thrombin generation compared to PCC. Both FEIBA and PCC reversed endogenous thrombin potential abnormalties in a concentration-dependent fashion, while rFVIIa led to only partial correction. Overall, this study suggests that FEIBA may more effectively reverse rivaroxaban-induced laboratory abnormalities compared to PCC or rFVIIa.
While FEIBA may ameliorate the anticoagulant effects of NOAC, it does not directly inhibit the drug. Although one of our cases received a repeated dose of FEIBA following an elevated rivaroxaban assay, it should be noted that FEIBA is not expected to change assay levels, though hemostasis may be improved. Rather, chromogenic Xa assay levels decline as the drug is metabolized and cleared. Depending on the half-life of the drug, or in the context of renal failure where drug clearance may be prolonged, FEIBA redosing may be required since the half-life of some components of FEIBA is short (i.e., Factor VII has a half-life of 4–6 h) and rebound coagulopathy could occur. However, FEIBA can cause dose-dependent complications such as thrombotic events (myocardial infarction, pulmonary embolus, disseminated intravascular coagulopathy/consumption; 4–8 events per 100,000 infusions) [23]. Although the thrombotic risks of FEIBA appear to be low, it should be noted that most of the safety data for FEIBA were conducted in young hemophiliac patients, who may not have the same vascular risk factors as an ICH population. Therefore, the thrombotic risks may be higher than reported. There are other uncommon side effects of FEIBA that bear mentioning. First, because FEIBA contains residual FVIII antigen, it can provoke an immunological response leading to increased factor VIII inhibitor titers in some patients (anamnesis) [23, 24]. However, these increases in inhibitor titers do not seem to impact hemostasis achieved with FEIBA [23]. Additionally, as with any plasma derived transfusion product, FEIBA administration carries a small risk of infection. However, the two step vapor heating viral inactivation process mitigates this risk without affecting FEIBA’s efficacy. There have been no reports of HIV or hepatitis transmission definitively linked to FEIBA since the introduction of vapor-heated viral inactivation in 1985 [23]. Because FEIBA is a plasma derived product, it may not be acceptable for use by Jehovah’s witnesses. Rare allergic reactions to FEIBA have been reported [23].
In October 2015 the FDA approved the first specific antidote for dabigatran. Idarucizumab (Praxbind®) is a monoclonal antibody that binds with very high affinity to dabigatran and thrombin-bound dabigatran, neutralizing its activity. It has been shown to produce immediate and complete reversal of the anticoagulant effects of dabigatran without thrombotic complications in healthy volunteers with mild to moderate renal impairment [25, 26]. In a study [27] of dabigatran-treated patients with either serious life-threatening bleeding or the requirement for an urgent procedure, Idarucizumab administration led to near complete normalization of the dilute thrombin time and ecarin clotting time in 89 % of patients within 4 h of dosing and lowered dabigatran drug levels for up to 24 h. Thirty-three out of thirty-six (92 %) patients requiring urgent procedures on dabigatran achieved normal intraoperative hemostasis. Five of ninety patients developed thrombotic complications including deep vein thrombosis, pulmonary embolus, left atrial thrombus, myocardial infarction, and ischemic stroke.
Andexanet alfa (Annexa/PRT064445) is another specific antidote under development. It is an inactive recombinant protein that is similar in structure to Factor Xa and binds with high affinity to Factor Xa inhibitors and heparin activated antithrombin. Previous studies have demonstrated its ability to reduce bleeding in animal models [28] and reverse coagulopathy (anti-Xa activity level) in phases I and II human volunteer studies [29]. It is currently being evaluated as part of a phase III study in bleeding patients and patients requiring urgent procedures treated with Factor Xa inhibitors (NCT02329327) [30].
Another promising agent, PER977 (Aripazine/Ciraparantag), is a small synthetic molecule designed originally to reverse heparin and fondaparinux effects. It also has activity against oral direct factor Xa inhibitors. Studies have shown reversal of anti-Xa effect in human blood and rat plasma spiked with dabigatran, rivaroxaban, and apixaban, along with reduction of bleeding to baseline parameters [31]. Other studies demonstrated improved coagulation parameters (PT and aPTT) and thromboelastography measures of coagulation in a rat model exposed to rivaroxaban, edoxaban, dabigatran, or apixaban [32]. Complete reversal of edoxaban-induced prolongation of whole blood clotting time was achieved after a single dose of aripazine in an in vivo human study [33].
Our case series has the limitation of being small and observational, largely because NOAC-related ICH is rare. Further multicenter studies are needed to verify the efficacy of FEIBA in preventing hematoma expansion and improving functional outcome. It is likely, however, that specific antidotes to NOAC will be favored over FEIBA when they become available. Until then, FEIBA appears to be a reasonable reversal agent for patients with NOAC-related ICH.
References
Magnani JW, Rienstra M, Lin H, Sinner MF, Lubitz SA, McManus DD, et al. Atrial fibrillation: current knowledge and future directions in epidemiology and genomics. Circulation. 2011;124:1982–93.
Van Walraven C, Hart RG, Singer DE, et al. Oral anticoagulants vs. aspirin in nonvalvular atrial fibrillation: an individual patient metaanalysis. JAMA. 2003;288:2441–8.
Hart RG, Boop BS, Anderson DC. Oral anticoagulants and intracranial hemorrhage facts and hypotheses. Stroke. 1995;26:1471–7.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51. doi:10.1056/NEJMoa0905561 published correction appears in N Engl J Med. 2010;363:1877.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91. doi:10.1056/NEJMoa1009638.
Connolly SJ, Eikelboom J, Joyner C, Diener HC, Hart R, Golitsyn S, Flaker G, Avezum A, Hohnloser SH, Diaz R, Talajic M, Zhu J, Pais P, Budaj A, Parkhomenko A, Jansky P, Commerford P, Tan RS, Sim KH, Lewis BS, Van Mieghem W, Lip GY, Kim JH, Lanas-Zanetti F, GonzalezHermosillo A, Dans AL, Munawar M, O’Donnell M, Lawrence J, Lewis G, Afzal R, Yusuf S, AVERROES Steering Committee and Investigators. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364:806–17. doi:10.1056/NEJMoa1007432.
Chatterjee S, Sardar P, Biondi-Zoccai G, Kumbhani DJ. New oral anticoagulants and the risk of intracranial hemorrhage: traditional and Bayesian meta-analysis and mixed treatment comparison of randomized trials of new oral anticoagulants in atrial fibrillation. JAMA Neurol. 2013;70:1486–90. doi:10.1001/jamaneurol.2013.4021.
Hemphill JC III, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung G, Goldstein J, Macdonald L, Mitchell P, Scott P. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032.
Turecek PL, Váradi K, Gritsch H, Schwarz HP. FEIBA: mode of action. Haemophilia. 2004;10(Suppl 2):3–9.
Marlu R, Hodaj E, Paris A, Albaladejo P, Cracowski JL, Pernod G. Effect of non-specific reversal agents on anticoagulant activity of dabigatran and rivaroxaban: a randomised crossover ex vivo study in healthy volunteers. Thromb Haemost. 2012;108(2):217–24.
Perzborn E, Heitmeier S, Laux V, Buchmuller A. Reversal of rivaroxaban-induced anticoagulation with prothrombin complex concentrate, activated prothrombin complex concentrate and recombinant activated factor VII in vitro. Thromb Res. 2014;133(4):671–81.
Schulman S, Ritchie B, Goy JK, Nahirniak S, Almutawa M, Ghanny S. Activated prothrombin complex concentrate for dabigatran-associated bleeding. Br J Haematol. 2013;164:296–310.
Wong H, Keeling D. Activated prothrombin complex concentrate for the prevention of dabigatran-associated bleeding. Br J Haematol. 2014;166:140–53.
Puttick T, Bahl R, Mohamedbhai H. Emergency reversal of dabigatran for emergency surgery. BMJ Case Rep. 2015. doi:10.1136/bcr-2014-209057.
Dager W, Roberts A. Reversing dabigatran with FEIBA in a patient with a transseptal perforation during cardiac ablation. Crit Care Med. 2011;39(12):243.
Heidbuchel H, Verhamme P, Alings M, et al. European heart rhythm association practical guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15:625–51.
Meyer CS, Blebea J, Davis K Jr, Fowl RJ, Kempczinski RF. Surveillance venous scans for deep venous thrombosis in multiple trauma patients. Ann Vasc Surg. 1995;9(1):109–14.
Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, Samama CM. Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e227S–77S. doi:10.1378/chest.11-2297.
Kiraly A, Lyden A, Periyanayagam U, Chan J, Pang P. Management of hemorrhage complicated by novel oral anticoagulants in the emergency department: case report from the northwestern emergency medicine residency. Am J Ther. 2013;20:300–6.
Maurice-Szamburski A, Graillon T, Bruder N. Favorable outcome after subdural hematoma treated with FEIBA in a 77-year-old patient treated by rivaroxaban. J Neurosurg Anesthesiol. 2014;26:2.
Lindahl TL, Wallstedt M, Gustafsson KM, Persson E, Hillarp A. More efficient reversal of dabigatran inhibition of coagulation by activated prothrombin complex concentrate or recombinant factor VIIa than by four-factor prothrombin complex concentrate. Thromb Res. 2015;135(3):544–7.
Khoo TL, Weatherburn C, Kershaw G, Reddel CJ, Curnow J, Dunkley S. The use of FEIBA(R) in the correction of coagulation abnormalities induced by dabigatran. Int J Lab Hematol. 2013;35(2):222–4.
Aledort LM. Factor VIII inhibitor bypassing activity (FEIBA)-addressing safety issues. Haemophilia. 2008;14:39–43.
Dimichele D. Inhibitors: resolving diagnostic and therapeutic dilemmas. Haemophilia. 2002;8(3):280–7.
Glund S, Stangier J, Schmohl M, De Smet M, Gansser D, Lang B, Moschetti V, Ramael S, Reilly P. A specific antidote for dabigatran: immediate, complete and sustained reversal of dabigatran induced anticoagulation in healthy male volunteers. Circulation. 2013;128:A17765.
Glund S, Stangier J, Schmohl M, Moschetti V, Haazen W, Gansser M, Norris S, Lang B, Reilly P. Idarucizumab, a specific antidote for dabigatran: immediate, complete and sustained reversal of dabigatran induced anticoagulation in elderly and renally impaired subjects. Blood. 2014;124:A344.
Pollack CV Jr, Reilly PA, Eikelboom J, et al. Idarucizumab for dabigatran reversal. N Engl J Med. 2015. doi:10.1056/NEJMoa1502000.
Lu G, DeGuzman FR, Hollenbach SJ, Karbarz MJ, Abe K, Lee G, Luan P, Hutchaleelaha A, Inagaki M, Conley PB, et al. A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nat Med. 2013;19(4):446–51.
Crowther M, Vandana M, Michael K, et al. A Phase 2 randomized, double-blind, placebo-controlled trial demonstrating reversal of rivaroxaban-induced anticoagulation in healthy subjects by andexanet alfa (PRT064445), an antidote for Fxa inhibitors. 55th ASH annual meeting, New Orleans 2013.
Crowther M, Levy G, Lu G, Leeds J, Barron L, Conley P, Castillo J, Curnutte J, Connolly S. ANNEXA-A: a phase 3 randomized, double-blind, placebo-controlled trial, demonstrating reversal of apixaban-induced anticoagulation in older subjects by andexanet alpha (PRT064445), a universal antidote for factor Xa (fXa) Inhibitors. Circulation. 2014;130:2105.
Laulicht B, Bakhru S, Jiang X, et al. Antidote for new oral anticoagulants: mechanism of action and binding specificity of PER977. Presented at the 24th Congress of the International Society on Thrombosis and Haematosis, Amsterdam, June 29–July 4, 2013.
Bakhru S, Laulicht B, Jiang X, Chen L, Pan D, Grosso M, Morishima Y, Brown K, Masumoto H, Costin J, Steiner S. PER977: a synthetic small molecule which reverses over-dosage and bleeding by the new oral anticoagulants. Circulation. 2014;128:A18809.
Ansell JE, Bakhru SH, Laulicht BE, Steiner SS, Grosso M, Brown K, Dishy V, Noveck RJ, Costin JC. Use of PER977 to reverse the anticoagulant effect of edoxaban. N Engl J Med. 2014;371:2141–2. doi:10.1056/NEJMc1411800.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Dibu, J.R., Weimer, J.M., Ahrens, C. et al. The Role of FEIBA in Reversing Novel Oral Anticoagulants in Intracerebral Hemorrhage. Neurocrit Care 24, 413–419 (2016). https://doi.org/10.1007/s12028-015-0213-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-015-0213-y