Abstract
Anti-HMGCR antibodies represent a characteristic serological feature of statin-exposed and statin-unexposed patients with immune-mediated necrotizing myopathy (IMNM). We assessed anti-HMGCR antibodies in patients with suspected IMNM following statin exposure and patients with other autoimmune rheumatic diseases. We evaluated the presence of anti-HMGCR autoantibodies in sera samples from 13 statin-exposed patients who were suspected of having IMNM, 38 patients with different inflammatory and autoimmune rheumatic diseases and 29 healthy subjects. The autoantibodies were evaluated by two assays: a new chemiluminescence QUANTA Flash HMGCR kit utilizing BIO-FLASH system and QUANTA Lite® HMGCR ELISA kit. Twelve samples from patients with suspicion for IMNM were found positive for anti-HMGCR antibodies by both assays. Only one of the 13 samples that were found positive by ELISA was negative by CIA. A very good qualitative correlation (κ = 0.95; 95 % CI 0.85–1.0) and quantitative agreement (Spearman’s rho 0.87; P value < 0.0001; 95 % CI 0.62–0.96) were found between these two assays. All samples from healthy subjects and from the disease-controlled patient cohort were negative for anti-HMGCR antibodies. In comparison with ELISA results, the CIA exhibited high sensitivity and specificity values of 92.3 and 100 %, respectively. Receiver operating characteristic analysis for CIA and ELISA yielded area under the curve values of 0.99. The presence of anti-HMGCR antibodies may be a useful biomarker of IMNM in statin-exposed patients. There is a good correlation between the two anti-HMGCR antibody assays evaluated in the present study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic inflammatory myopathies (IIMs) represent a heterogeneous group of systemic autoimmune rheumatic diseases with high mortality and morbidity rates [1, 2]. The frequency of autoantibodies directed against nuclear or cytoplasmic constituents ranges from 50 to 80 % in patients with dermatomyositis (DM) or polymyositis (PM). A wide spectrum of myositis-specific autoantibodies (MSAs) and myositis-associated autoantibodies (MAAs) has been recently identified and contributed to better clinical classification of IIMs at diagnosis [3].
In recent years, immune-mediated necrotizing myopathy (IMNM) was also recognized as a distinct form of autoimmune muscle disease [4]. Unlike IIM where lymphocytic infiltrates are predominantly found within muscle tissue, IMNM is characterized by prominent myofiber necrosis with abundant macrophages and minimal lymphocytic infiltration [5]. Current evidence suggests that IMNM may be associated with the presence of distinct autoantibodies recognizing either the signal recognition particle (SRP), a cytoplasmic protein that binds the signal sequences of newly synthesized proteins and facilitates their translocation into the endoplasmic reticulum [2, 6], or 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR), the rate-controlling enzyme of the mevalonate pathway involved in cholesterol synthesis [7–13].
Historically, anti-HMGCR was firstly reported by Christopher-Stine and colleagues as “anti-200/100” [7]. Due to the strong association of these novel autoantibodies with statin use in 63 % of the patients with necrotizing myopathy, Mammen and colleagues in the same group searched for an autoantigenic target in the cholesterol synthesis cascade.
This “anti-200/100” autoantibody was later identified as directed against HMGCR [8].
Anti-HMGCR antibodies have been identified in patients with IMNM associated with statin exposure as well as in statin-unexposed patients [7–14]. The discovery of these antibodies created a new subset of IMNM that may be sometimes clinically distinguishable from other forms of IIM and other muscle diseases associated with muscle necrosis, including toxic myopathies, endocrinopathies and muscular dystrophies. In stain-exposed patients, the presence of anti-HMGCR antibodies may point to the autoimmune nature of the myopathy, in contrast to other forms of statin-induced myotoxicity [9].
Different technologies may be used to detect anti-HMGCR antibodies including immunoprecipitation, quantitative addressable laser bead immunoassay (ALBIA), enzyme-linked immunosorbent assay (ELISA) and chemiluminescence immunoassay (CIA) [7–14]. Immunoprecipitation was an early assay that was time-consuming and expensive [7]. In 2012, ELISA was validated as consistent, efficient test for the identification of anti-HMGCR autoantibodies with sensitivity and specificity of 94.4 and 99.3 %, respectively [8]. During the last few years, the CIA technology has been applied for autoantibody testing [15]. CIA technology offers rapid detection of antibodies, high reproducibility and broader dynamic range than ELISA that enables a more accurate quantification of the results.
The main aim of the present study was to compare between two different techniques for the detection of anti-HMGCR antibodies: ELISA and CIA using BIO-FLASH system. For this purpose, we evaluated the presence of anti-HMGCR antibodies in statin-exposed patients with suspected IMNM, in patients with other autoimmune inflammatory diseases and in healthy subjects.
Materials and methods
Sera samples
We evaluated the presence of anti-HMGCR autoantibodies in sera samples from 13 patients who were suspected of having IMNM. All patients fulfilled the Bohan and Peter criteria for PM and were previously exposed to statins [16, 17].
The control group consisted of 29 healthy subjects and 38 patients with different inflammatory and autoimmune rheumatic diseases including systemic lupus erythematous (SLE; n = 12 patients), rheumatoid arthritis (RA; n = 10), ankylosing spondylitis (AS; n = 8), systemic sclerosis (SS; n = 2), polymyositis (PM; n = 2) and antiphospholipid syndrome (APS; n = 4).
The study fulfilled the ethical guidelines of the most recent Declaration of Helsinki and received approval by the local ethical committees (Edinburgh, 2000; Registration number: 1895-15-SMC).
Diagnostic assays
QUANTA Lite® HMGCR ELISA kit
ELISA plates coated with recombinant HMGCR were incubated with diluted patient samples. The evaluation was done according to the standard protocol of QUANTA Lite HMGCR ELISA (Inova Diagnostics Inc., San Diego, CA, USA). The principles of this assay have recently been summarized elsewhere [14]. The cutoff was defined as 20 units (U/mL).
QUANTA Flash HMGCR kit
Chemiluminescence QUANTA Flash HMGCR assay utilizing recombinant human HMGCR antigen coupled to paramagnetic beads (Inova Diagnostics Inc., San Diego, CA, USA) was performed on the BIO-FLASH® system (Biokit S.A., Barcelona, Spain). The BIO-FLASH® instrument is a fully automated chemiluminescent immuno-analyzer, and the principles of this system have recently been described elsewhere [15]. The cutoff was defined as 20 chemiluminescence units (CU). MSA was evaluated by Sclero-Poly-Synthetase Profile 8 Ag Dot (Alphadia S.A/N.V. Diagnostic Products, Belgium), and MAA was assessed by ANA Immunofluorescence (Hep-2 Cell line, Bio-Rad Laboratories, Inc., USA) and EIA (Quanta Lite, Inova Diagnostics, Inc., USA).
Statistics
The data were statistically evaluated using the MedCalc Software (version 16.4.3; MedCalc Software bvba, Ostend, Belgium). Cohen’s kappa agreement tests and Spearman’s correlation were carried out to analyze the agreement between ELISA and CIA, and P value > 0.05 was considered significant. Receiver operating characteristics (ROC) analysis was used to analyze the discriminatory ability of these assays.
Results
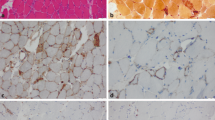
All patients with suspicion for IMNM presented with proximal weakness following statin therapy which persisted at least 8–10 weeks after statin cessation. Serum creatine kinase (CK) levels ranged from 2700 to 12,200 IU/L. EMG was consistent with a myopathic picture. In 12 patients, the diagnosis of necrotizing myopathy was proven by muscle biopsy: 10 patients underwent biopsy before the detection of anti-HMGCR antibodies; in the remaining the biopsy was performed after the detection of these antibodies. In one patient, the biopsy result was inconclusive. Results of screening for MSAs and MAAs were available only in three patients, and they were all negative.
Twelve samples from patients with suspicion for IMNM were found positive for anti-HMGCR antibodies by both assays. Only one of the 13 samples that were found positive by ELISA was negative by CIA. All samples from healthy subjects and from the disease-controlled patient cohort were negative for anti-HMGCR antibodies (Figs. 1, 2). In comparison with ELISA results, the CIA exhibited high sensitivity and specificity values of 92.3 and 100 %, respectively.
A very good qualitative agreement was found between these two assays (κ = 0.95; 95 % CI 0.85–1.0) (Table 1). A quantitative comparison between CIA and ELISA based on the levels of anti-HMGCR antibodies also revealed a strong correlation (Spearman’s coefficient 0.87; P value < 0.0001; 95 % CI 0.62–0.96) (Fig. 3).
Receiver operating characteristic (ROC) analysis for CIA and ELISA yielded area under the curve values of 0.99 (Fig. 4).
Discussion
IMNM is a complex heterogeneous group of muscle disorders with a similar histopathological pattern on muscle biopsy, including muscle cell necrosis and degeneration without significant inflammatory infiltrates. However, the clinical spectrum of IMNM is very broad and the analysis of all of the underlying causes may prove to be difficult. IMNM may be associated with viral infections such as hepatitis C [18] and HIV [19, 20], malignancy [20, 21] or connective tissue diseases such as scleroderma [22, 23] or antisynthetase syndrome [24]. Additional subsets of IMNM are characterized by the presence of autoantibodies directed against SRP [2, 6] and HMGCR [7–12]. The classification and diagnostic criteria for IMNM are currently investigated, and the verification of distinct subsets of IMNM based on autoantibodies, environmental triggers and more specific muscle biopsy features is often needed.
In the present study, we evaluated the presence of anti-HMGCR antibodies in statin-exposed patients with suspicion for IMNM and two control groups: healthy subjects and patients with different autoimmune rheumatic diseases. Our cohorts were tested by two different assays: ELISA and CIA. Similarly to previous reports, our results confirmed that anti-HMGCR antibodies were strongly associated with IMNM following statin exposure in comparison with control groups. With regard to statin-exposed patients with suspicion for IMNM, a very good qualitative agreement (κ = 0.95) and strong quantitative correlation based on anti-HMGCR antibodies levels (Spearman’s rho 0.87) were found between these two techniques. Both assays were able to discriminate between IMNM patients and controls in a similar manner, as shown by ROC analysis (Fig. 4). In comparison with ELISA results, The CIA showed good performance characteristics with specificity of 92.3 % and sensitivity of 100 %. Our data confirmed the previous results that anti-HMGCR antibodies may be detected using different assays including CIA technology and ELISA with good inter-method agreement [14]. A fully automated measurement process makes CIA an attractive alternative to the more traditional ELISA. An additional method, ALBIA might also be a reliable screening test for anti-HMGCR antibodies that displays good agreement with the methods discussed above [14].
In our study, we mainly focused on patients suspected of having IMNM according to clinical manifestations that included muscle weakness and prolonged CPK elevation (more than 8–10 weeks) following statin withdrawal. Remarkably, the initial clinical presentations of autoimmune and self-limited forms of statin-related muscle disease may be similar and differential diagnosis may be difficult. However, anti-HMGCR autoantibodies have not been detected in patients with statin intolerance or rhabdomyolysis [9, 25]. Thus, negative results may exclude IMNM and distinguish between those who require treatment and those who may recover following statin withdrawal only. However, commercial anti-HMGCR ELISA has a false positive rate of approximately 0.7 %, and some statin-exposed patients with self-limited myotoxicity may be misclassified as autoimmune disease patients by this method [9]. In this regard, testing for anti-HMGCR antibodies should only be performed in patients with a high clinical probability of IMNM mostly associated with statins.
It has been found that statin exposure in different populations of anti-HMGCR-positive patients with IIM/IMNM ranges from 15 to 94 % [8, 10, 26–28]. Thus, only 15 % of anti-HMGCR-positive patients with IIM in the China study had previous statin exposure [26]. Similarly, the majority of anti-HMGCR-positive patients from an European cohort who were suspected of having IMNM were not exposed to statins [27]. In contrast, a more early study from the USA revealed that the prevalence of statin use reached 72.7 % in a cohort of IIM patients [10]. Moreover, an Australian report showed that 94 % of HMGCR antibody-positive patients with IMNM had been previously exposed to statins [28]. This difference in the prevalence of statin exposure may be explained by different genetic backgrounds as well as by the fact that different studies analyzed different patient cohorts suffering from either IIM or IMNM. In this context, it is important to emphasize that many food products contain increased levels of natural statins which might or might not explain the existence of anti-HMGCR antibodies in so-called statin-naïve patients [29]. Another interesting aspect is that not all forms of statins seem to have an equivalent effect on the initiation of IMNM [30]. Although an additional recent report showed that anti-HMGCR antibodies were found in both IIM and IMNM and were associated strongly with statin use [31], further studies with separate analysis of these conditions are required.
As discussed above, the proportion of statin-naïve HMGCR antibody-positive patients varies between different studies. Although both statin-exposed and statin-unexposed anti-HMGCR positive myopathy patients have similar clinical manifestations and genetic risk factor associated with the class II HLA allele DRB1*11:01, significant differences were found between the two groups [32]. In comparison with statin-exposed patients, statin-unexposed patients were more likely to be younger, African-American and have higher CK levels and a low response to immunosuppressive therapy [8].
It should be noted that necrotizing myopathy may be associated with various malignancies [20, 21] In addition, necrotizing myopathy is more common in older people who are more likely to be exposed to statins. Therefore, the presence of anti-HMGCR antibodies in IMNM patients may suggest autoimmune etiology of the disease, but this condition may also be associated with coexisting malignancy. For instance, one earlier study noted that 13 % of anti-HMGCR-positive IMNM patients had a malignancy, although the status of statin exposure in this subpopulation was unknown [7]. For this reason, a full malignancy workup at the time of diagnosis of IMNM may be recommended, similar to the one that would be undertaken at the time of diagnosis of PM or DM. To date, according to age appropriate malignancy screening, none of our IMNM patients had malignancies.
In the current study, anti-HMGCR antibodies were not detected in patients with different systemic autoimmune rheumatic diseases. In this regard, previous reports have shown that these antibodies are rarely found in patients with autoimmune diseases other than IMNM. For example, an early basic study revealed that among 45 anti-HMGCR-positive patients, one patient had ILD associated with anti-Jo 1-positive antisynthetase syndrome, and another patient had ILD related to anti-Pm/Scl-positive scleroderma [8]. However, anti-HMGCR-positive IMNM is usually characterized by a typical phenotype that includes progressive muscle weakness and sometimes arthralgia, myalgia, dysphagia and Raynaud’s phenomenon, while multisystem manifestations, especially ILD, appear to be uncommon. The clinical significance of anti-HMGCR positivity in the two patients described above is unknown, but the possibility of an overlap syndrome as well as false positive results was not excluded. In addition, low titers of anti-HMGCR antibodies were previously detected in three patients with Sicca syndrome [14] and also in one patient with pSS without symptoms of myopathy [26]. In our study, one IMNM patient had low titer of anti-HMGCR antibodies as detected by ELISA, while CIA did not find anti-HMGCR reactivity. A repeat test for anti-HMGCR antibodies was not performed in this patient who completely recovered following treatment with corticosteroids. It is possible that patients with statin-associated IMNM may sometimes have a low titer of anti-HMGCR antibodies, and recurrent assessment of these antibodies is required. Therefore, anti-HMGCR antibodies detected in moderate and high titers are highly specific for IMNM, but low titers do not exclude this disease in certain clinical situations. Therefore, a novel strategy regarding patients with low titers of anti-HMGCR antibodies should be proposed.
The current study has several limitations: First of all, the study involves a relatively small cohort of patients with IMNM, due to the rarity of this disease. Secondly, our initial visit data do not reflect true patients’ status before treatment because some patients started steroids treatment before the anti-HMGCR antibodies were evaluated. Thirdly, the results of screening for MSA and MAA were available only in three patients.
Conclusion
In summary, this study demonstrates that anti-HMGCR antibodies are a promising highly specific biomarker that may aid in the diagnosis of IMNM in statin-exposed patients.
The presence of anti-HMGCR antibodies may be detected by different techniques, such as CIA and ELISA, with a good inter-method agreement.
References
Dalakas MC. Polymyositis, dermatomyositis and inclusion-body myositis. N Engl J Med. 1991;325:1487–98.
Mahler M, Miller FW, Fritzler MJ. Idiopathic inflammatory myopathies and the anti-synthetase syndrome: a comprehensive review. Autoimmun Rev. 2014;13:367–71.
Betteridge Z, McHugh N. Myositis-specific autoantibodies: an important tool to support diagnosis of myositis. J Intern Med. 2016;280:8–23.
Basharat P, Christopher-Stine L. Immune-mediated necrotizing Myopathy: update on diagnosis and management. Curr Rheumatol Rep. 2015;17:72.
Amato AA, Greenberg SA. Inflammatory myopathies. Continuum (Minneap Minn) 2013;19(6):1615–33.
Miller T, Al-Lozi MT, Lopate G, Pestronk A. Myopathy with antibodies to the signal recognition particle: clinical and pathological features. J Neurol Neurosurg Psychiatry. 2002;73:420–8.
Christopher-Stine L, Casciola-Rosen LA, Hong G, Chung T, Corse AM, Mammen AL. A novel autoantibody recognizing 200-kd and 100-kd proteins is associated with an immune-mediated necrotizing myopathy. Arthritis Rheum. 2010;62:2757–66.
Mammen AL, Chung T, Christopher-Stine L, Rosen P, Rosen A, Doering KR, et al. Autoantibodies against 3-hydroxy-3-methylglutaryl-coenzyme A reductase in patients with statin-associated autoimmune myopathy. Arthritis Rheum. 2011;63:713–21.
Mammen AL, Pak K, Williams EK, Brisson D, Coresh J, Selvin E, et al. Rarity of anti-3-hydroxy-3-methylglutaryl-coenzyme A reductase antibodies in statin users, including those with self-limited musculoskeletal side effects. Arthritis Care Res (Hoboken). 2012;64:269–72.
Werner JL, Christopher-Stine L, Ghazarian SR, Pak KS, Kus JE, Daya NR, et al. Antibody levels correlate with creatine kinase levels and strength in anti-3-hydroxy-3-methylglutaryl-coenzyme A reductase-associated autoimmune myopathy. Arthritis Rheum. 2012;64:4087–93.
Mohassel P, Mammen AL. The spectrum of statin myopathy. Curr Opin Rheumatol. 2013;25:747–52.
Mohassel P, Mammen AL. Statin-associated autoimmune myopathy and anti-HMGCR autoantibodies. Muscle Nerve. 2013;48:477–83.
Watad A, Soriano A, Vaknine H, Shoenfeld Y, Amital H. Immune mediated myopathy following long-term statin therapy. Isr Med Assoc J. 2015;17:128–9.
Musset L, Miyara M, Benveniste O, Charuel JL, Shikhman A, Boyer O, et al. Analysis of autoantibodies to 3-hydroxy-3-methylglutaryl-coenzyme A reductase using different technologies. J Immunol Res. 2014;2014:405956.
Bentow C, Swart A, Wu J, Seaman A, Manfredi M, Infantino M, et al. Clinical performance evaluation of a novel rapid response chemiluminescent immunoassay for the detection of autoantibodies to extractable nuclear antigens. Clin Chim Acta. 2013;424:141–7.
Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975;292:344–7.
Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med. 1975;292:403–7.
Satoh J, Eguchi Y, Narukiyo T, Mizuta T, Kobayashi O, Kawai M, et al. Necrotizing myopathy in a patient with chronic hepatitis C virus infection: a case report and a review of the literature. Intern Med. 2000;39:176–81.
Snider WD, Simpson DM, Nielsen S, Gold JW, Metroka CE, Posner JB. Neurological complications of acquired immune deficiency syndrome: analysis of 50 patients. Ann Neurol. 1983;14:403–18.
Lazarou IN, Guerne PA. Classification, diagnosis, and management of idiopathic inflammatory myopathies. J Rheumatol. 2013;40:550–64.
Dalakas MC. Review: an update on inflammatory and autoimmune myopathies. Neuropathol Appl Neurobiol. 2011;37:226–42.
Ellis E, Ann Tan J, Lester S, Tucker G, Blumbergs P, Roberts-Thomson P, et al. Necrotizing myopathy: clinicoserologic associations. Muscle Nerve. 2012;45:189–94.
Bhansing KJ, Lammens M, Knaapen HK, van Riel PL, van Engelen BG, Vonk MC. Scleroderma-polymyositis overlap syndrome versus idiopathic polymyositis and systemic sclerosis: a descriptive study on clinical features and myopathology. Arthritis Res Ther. 2014;16:R111.
Mehndiratta P, Mehta S, Manjila SV, Kammer GM, Cohen ML, Preston DC. Isolated necrotizing myopathy associated with ANTI-PL12 antibody. Muscle Nerve. 2012;46:282–6.
Floyd JS, Brody JA, Tiniakou E, Psaty BM, Mammen A. Absence of anti-HMG-CoA reductase autoantibodies in severe self-limited statin-related myopathy. Muscle Nerve. 2016;54:142–4.
Ge Y, Lu X, Peng Q, Shu X, Wang G. Clinical characteristics of anti-3-hydroxy-3-methylglutaryl coenzyme A reductase antibodies in Chinese patients with idiopathic inflammatory myopathies. PLoS One. 2015;10:e0141616.
Allenbach Y, Drouot L, Rigolet A, Charuel JL, Jouen F, Romero NB, et al. Anti-HMGCR autoantibodies in European patients with autoimmune necrotizing myopathies: inconstant exposure to statin. Medicine (Baltimore). 2014;93:150–7.
Ramanathan S, Langguth D, Hardy TA, Garg N, Bundell C, Rojana-Udomsart A, et al. Clinical course and treatment of anti-HMGCR antibody-associated necrotizing autoimmune myopathy. Neurol Neuroimmunol Neuroinflamm. 2015;2:e96.
Musset L, Allenbach Y, Benveniste O, Boyer O, Bossuyt X, Bentow C, et al. Anti-HMGCR antibodies as a biomarker for immune-mediated necrotizing myopathies: a history of statins and experience from a large international multi-center study. Autoimmun Rev. 2016. doi:10.1016/j.autrev.2016.07.023.
Klein M, Mann H, Pleštilová L, Zámečník J, Betteridge Z, McHugh N, et al. Increasing incidence of immune-mediated necrotizing myopathy: single-centre experience. Rheumatology (Oxford). 2015;54:2010–4.
Limaye V, Bundell C, Hollingsworth P, Rojana-Udomsart A, Mastaglia F, Blumbergs P, et al. Clinical and genetic associations of autoantibodies to 3-hydroxy-3-methyl-glutaryl-coenzyme a reductase in patients with immune-mediated myositis and necrotizing myopathy. Muscle Nerve. 2015;52:196–203.
Mammen AL, Gaudet D, Brisson D, Christopher-Stine L, Lloyd TE, Leffell MS, et al. Increased frequency of DRB1*11:01 in anti-hydroxymethylglutaryl-coenzyme A reductase-associated autoimmune myopathy. Arthritis Care Res (Hoboken). 2012;64:1233–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shovman, O., Gilburd, B., Chayat, C. et al. Anti-HMGCR antibodies demonstrate high diagnostic value in the diagnosis of immune-mediated necrotizing myopathy following statin exposure. Immunol Res 65, 276–281 (2017). https://doi.org/10.1007/s12026-016-8867-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-016-8867-x