Abstract
The aim of this autopsy study was to investigate chest-compression associated injuries to the trunk in out-of-hospital and in-hospital non-traumatic cardiac arrest patients treated with automated external chest compression devices (ACCD; all with LUCAS II devices) versus exclusive manual chest compressions (mCC). In this retrospective single-center study, all forensic autopsies between 2011 and 2017 were included. Injuries following cardiopulmonary resuscitation (CPR) in patients treated with mCC or ACCD were investigated and statistically compared using a bivariate logistic regression. In the seven-year period with 4433 autopsies, 614 were analyzed following CPR (mCC vs. ACCD: n = 501 vs. n = 113). The presence of any type of trunk injury was correlated with longer resuscitation intervals (30 ± 15 vs. 44 ± 25 min, p < 0.05). In comparison with mCC, treatment with ACCD led to more frequent skin emphysema (5 vs 0%, p = 0.012), pneumothorax (6 vs. 1%, p = 0.008), lung lesions (19 vs. 4%, p = 0.008), hemopericardium (3 vs 1%, p = 0.025) and liver lesions (10 vs. 1%, p = 0.001), all irrespective of confounding aspects. Higher age and longer CPR durations statistically influenced frequency of sternal and rib fractures (p < 0.001). The mean number of fractured ribs did not vary significantly between the groups (6 ± 3 vs. 7 ± 2, p = 0.09). In this cohort with unsuccessful CPR, chest compression-related injuries were more frequent following ACCD application than in the mCC group, but with only minutely increased odds ratios. The severity of injuries did not differ between the groups, and no iatrogenic injury was declared by the forensic pathologist as being fatal. In the clinical routine after successful return of spontaneous circulation a computed tomography scan for CPR-associated injuries is recommended as soon as possible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients suffering from out-of-hospital and in-hospital cardiac arrest, external chest compressions and ventilation are part of standard care to regain spontaneous circulation and potentially save patients’ lives. Over the years, the technique of chest compression in cardiac arrest has been optimized steadily to achieve higher efficiency, an increased survival rate and an improved outcome [1, 2].
Various automatic chest compression devices (ACCD) guarantee chest compressions of consistent quality [3]. One example of an ACCD is the Lund University Cardiopulmonary Assist System (LUCAS), a piston device conducting chest compression and active decompression by a suction cup (Fig. 1). The ACCD needs to be placed precisely on the central region of the chest, well above the lower sternum.
The LUCAS II device is battery-powered and performs uninterrupted chest compressions at a frequency of 100 min−1 and a compression depth of 5 cm [4].
ACCDs appear to be a relief for medical teams facilitating cardiopulmonary resuscitation (CPR), however, according to the European Resuscitation Council (ERC) guidelines, their routine use is explicitly not recommended [5, 6]. There is a high adherence to these guidelines in our region for the use of ACCDs [7]. However, studies so far have failed proving better outcomes regarding the neurological status for ACCD compared to manual chest compression (mCC) [8, 9]. Instead, some studies have even demonstrated worse outcomes [10, 11]. An ‘absolute’ contraindication of ACCD use is only known for already-dead patients. ‘Relative’ contraindications are listed for pregnant women, instable thoraces or other deformations of the thoracic cavity as well as when living wills are existent contradicting CPR [7].
Furthermore, the mechanical forces occurring during ACCD usage seem to be higher and more intense compared to mCC, whereby the probability of serious injuries may arise. The range of traumatic injuries caused by ACCD comprises cutaneous abrasions, rib and sternal fractures, and solid organ lesions [12, 13]. Concerning this issue, recent studies show contradicting results in comparison of common mCC to ACCD [14,15,16,17]. Overall, the mentioned outcomes of ACCD show great variation and lack in reproducibility [16]. However, all of the existing studies cited [14,15,16,17] used basic statistical evaluation to compare mCC- and ACCD-associated injuries in unadjusted analyses but failed to investigate relevant CPR-associated confounders, such as age and sex of the patients or duration of CPR, using multivariate analyses. Even though none of the former studies report any life-threatening events, single alarming case reports emphasize the potential danger of traumatic injury in ACCD and warrant further investigation [18,19,20].
The aim of this forensic study was to investigate whether out-of-hospital and in-hospital cardiac arrest patients treated with ACCD suffer more frequently and more intensively from chest compression-associated injuries to the trunk, compared to mCC treatment, and to investigate the influence of relevant confounders of the existence of CPR-associated injury.
Methods
Study design
A retrospective design was set up, including an autopsy collective with priority on forensic considerations given the inconsistent knowledge on ACCD-associated injury. Therefore, a retrospective single-center autopsy-based study was carried out for all forensic autopsies performed at the Institute of Legal Medicine, University of Leipzig, Germany between 2011 and 2017. The study was approved by the ethics committee of the Medical Faculty of the University of Leipzig, Germany (code: 104/17-ek).
Out of all autopsies, only cases suffering from out-of-hospital and/or in-hospital cardiac arrest in which CPR were performed were included. All CPR cases in non-natural deaths involving injuries to the trunk (between shoulder level and pelvis line), of non-adolescents, with return of spontaneous circulation (ROSC) and associated survival periods longer than 12 h were excluded. This limit of time exclusion was set as all patients with initial survival were treated intensively after ROSC and we wished to exclude the influence of further medical measures entirely. Subsequently, we divided the resulting cohort into cases with only manual (mCC group) or mCC with additional extended mechanical chest compressions by ACCD (for all cases: LUCAS II device, battery device; Physio Control, Redmond, USA; ACCD group).
Data collection
All autopsy reports (including autopsy findings, emergency medical services’ logbooks, emergency department charts, physicians’ reports and police statements, if available) were evaluated considering demographics, causes and places of death and with special focus on relevant CPR-related variables (e.g. associated injuries, existence of bystander CPR, CPR duration, airway management). The data were collected according to the ‘Utstein style’ [3]. Any chest compression-related injury was diagnosed whenever the resuscitation attempts were plausible and likely to cause the finding without other necessary explanations as described elsewhere [21]. All airway management-associated injuries were excluded from further investigation of this study in order to focus on chest compression-derived injuries.
All autopsies in our institute were done according to the S1 guideline ‘Forensic autopsy’ by the German Society of Legal Medicine [22] and the local autopsy procedures have been fully accredited by the German Accreditation Body (DAkkS) since 2010.
Analysis
All variables were coded into anonymous data using Microsoft Excel (2010; Bellevue, WA, USA). Statistical tests were conducted using R (version 3.14.0, 2017) and SPSS 23.0 (IBM, IL, USA). After verifying normal distribution by Shapiro-Wilk test, descriptive statistics included numbers and percentages with mean ± standard deviation (SD). In the first step data were compared between the two treatment groups with Pearson correlations, Chi-square tests for categorical variables and Student’s t test for continuous variables.
Second, the patient cases with complete datasets were included in a bivariate logistic regression analysis to compare the frequency of injuries between the two CPR methods to all relevant CPR-associated confounders.
P values were adjusted for multiple comparisons and were considered as statistically significant at a level of p < 0.05 and as highly statistically significant at p < 0.001.
Results
In the 7-year period, out-of-hospital and/or in-hospital cardiac arrest CPR were performed in 1338 cases (30.2%) from a total of 4433 forensic autopsies (Fig. 2). Out of these, the study cohort (n = 614) reflects 45.9% of all cases of unsuccessful CPR (Supplemental Fig. 1).
PRISMA chart of group selection. Excluded cases marked ‘others’ describe fatalities of a pregnant woman, one case after pathologic pre-autopsy and one after CPR by a different automated chest compression device other than LUCAS II (AutoPulse). CPR; cardiopulmonary resuscitation; n, numbers; h, hours; mCC, manual chest compression; ACCD, automated chest compression device
The frequency of ACCD-treated cases rose significantly over the period of study (2011, n = 8 vs. 2017, n = 45, p = 0.004). According to the results of forensic autopsy, most of the investigated individuals of both treatment groups died from cardiac disease (mCC vs. ACCD: 57.7% (n = 289) vs. 59.3% (n = 67)). Table 1 presents demographic and treatment data of both groups.
There were a number of cases without any detectable CPR-associated injury, predominating in a significantly higher number for mCC cases. The existence of any type of injury was associated with longer CPR duration efforts for both methods, if the duration time was available (without vs. with injury: 30 ± 16 vs. 44 ± 25 min, p < 0.0001 for mCC and 43 ± 13 vs. 74 ± 33 min, p = 0.04 for ACCD). ACCD cases were more often initially resuscitated by medical laymen than mCC cases. A detailed documentation of the CPR duration was missing in 206 cases. Another interesting aspect that was seen was that with increasing age, CPR duration was limited moderately (mCC vs. ACCD: r = −0.15, p = 0.06 vs. r = −0.25, p = 0.01).
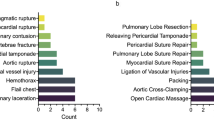
There was a wide range of CPR-associated injuries for both treatment groups consisting of different cutaneous, organ and osseous lesions (see Fig. 3 as illustration).
Representative autopsy pictures of chest compression-related injuries. Typical skin injuries following chest compression with LUCAS II-device showing imprints only (a), typical round-shaped lesions (b) and mostly avital heavy dermal abrasions (c). Circumscribed tissue bleeding above the sternum (d) and dislocated sternal fracture with interruption of the osseous continuity (e). Extensive pericardial hemorrhage (f) and ruptured pericardium (g; photographed under tension). Intensive subendocardial bleeding in the left ventricle (h). Multiple superficial injuries of the liver (i)
The injuries registered in both treatment groups are presented in Fig. 4 and further details regarding the number, localization and mean volume of special injury categories are in Table 2. Nominally, the ACCD group seemed to be associated with higher percentages in skin injuries, especially at the sternal chest, ranging from superficial to heavy skin abrasions and subcutaneous bleedings.
Bivariate logistic regression tests were subsequently performed to check for association between the injury category listed in Fig. 4 and the CPR method, as well as other interfering factors (age, sex, body mass index and CPR duration; n = 364). Sex, body mass index and existence of bystander CPR did not influence any of the injury categories from a statistical perspective. Most of the registered injuries were more frequent in the ACCD group, but generally with an odds ratio only slightly above 1 (see Table 3). The age of the deceased influenced thoracic injuries, especially the existence of sternal (p = 0.002) and rib (p < 0.001) fractures. Further, sternal and rib fractures were more frequent the longer the CPR duration was (both p < 0.001). The existence of rib fractures did not show significant alterations to the applied CPR method.
The absolute numbers of rib fractures in total were n = 1936 for mCC and n = 497 for ACCD.
Figure 5 illustrates the distribution of all registered rib fractures. The frontal lines (parasternal, midclavicular) were significantly more often injured than lateral or posterior lines. The mean number of fractured ribs did not differ between both groups (mCC vs. ACCD: 6.5 ± 2.3 vs. 5.9 ± 2.5) and the right to left distribution was almost equally, but slightly more left-sided in both treatments (Table 2). Most commonly injured were the 3rd to 6th ribs at the front of the thoracic aperture, but there were also cases with other levels of fractured ribs (from 1st to 12th).
Most of the recorded solid organ lesions were small, located superficially and the differentiation of the injury location remained insignificant between both treatment groups (Table 2). No relevant injury to the spleen or other abdominal organs after CPR was registered.
Great vessel injuries were detected solely at the thoracic cavity nearby the pericardium. Injury to the thoracic aorta (adventitial bleedings, no rupture), internal thoracic artery (total ruptures), right coronary artery (laceration) and the inferior vena cava (straining) were registered in both groups.
Although many different minor to severe injuries were detected it can clearly be stated that no chest compression associated injury in both groups was determined as ultimate cause of death.
Discussion
This retrospective single-center autopsy-based study over a 7-year period found nominally more ACCD-than mCC-associated injuries but the age of the patients and the CPR duration were confounding factors that especially influenced the existence of osseous injuries. However, the severity of all injuries did not differ statistically between the ACCD and the mCC group. No injury registered was fatal for the individual.
Since the introduction of chest compression by Kouwenhoven et al. [1], mCC has been a standard of treatment for many years. External chest compression by mCC and increasingly by ACCD are performed in order to produce a minimal cardiac output and are recommended life-saving procedures by the ERC guidelines on CPR [5]. ACCD use, however, is only recommended under specific circumstances (e.g. persistent ventricular tachycardia, prolonged CPR duration and transportation, CPR efforts in high altitude or with high stress levels for the rescue team, and CPR in air rescue services) [5]. Thereby, a meta-analysis of existing studies did not suggest that ACCD are inferior to mCC regarding outcomes [23].
External chest compression represents an iatrogenic chest trauma as compressions to a depth of ideally 5 cm but no more than 6 cm in adult patients are recommended [5]. It is well known that CPR can be a cause of injury in general [24]. For this reason, detailed forensic autopsy investigations are needed to define realistic frequencies of relevant CPR-associated injuries to optimize the clinical strategies in cases of initial survival [25], but should also be evaluated under consideration of relevant statistical confounders, which was missing in comparable studies so far. Further, from a forensic point of view, detailed knowledge is needed when judging other injuries caused by external trauma such as accidents or violence by other persons in legal cases.
Previous forensic autopsy results with up to 180 cases following mCC [26] showed similar distributions of mCC-related injuries in comparison to our given mCC group including more than 500 cases. The most frequent mCC related injuries next to dermal abrasions are fractures of ribs and sternum.
Studies comparing the incidence of chest compression-associated injury between ACCD and mCC cases are summarized in Table 4. One study using the data from the LUCAS in Cardiac arrest (LINC) trial discovered no difference in injury frequency in both groups [14]. In line with our investigation, another study using extended data from the LINC trail found a higher incidence of injuries in the LUCAS group [15]. However, the percentage of cases without any CPR-related injury is nominally smaller for ACCD than for mCC in all studies [14,15,16, 27]. Interestingly, only one study contradicts the research and daily routine experience with more than 80.0% uninjured patients treated with mCC as well as with ACCD [17]. The findings of both groups for skin injuries on the spine and chest by Lardi et al. [16] were in line with our investigation, whereas most other studies did not report such dermal findings at all, most plausibly because these injuries are mainly without clinical relevance. However, the consequence of dermal injuries for surviving patients has not been investigated thoroughly until now. Lardi et al. [16] presented the sole forensic study relating to ACCD-associated injuries to date, and most of the results compare similarly to ours.
The results for sternal fractures are in line with Lardi et al. [16] and Smekal et al. [14, 15] (mCC vs. ACCD: 21.3–54.2% vs. 29.0–58.3%), but disagree with Koster et al. (mCC vs. ACCD: 4.0% vs. 6.5%) [17]. Koster et al. [17] used computed tomography imaging (CT) or clinical follow-up for detecting injuries in most of their cases, methods known to be less sensitive compared to necropsy. Other investigations used CT for postmortem analysis of CPR-related injury [28] or a combination of autopsy, postmortem CT and clinical investigation [17]. Forensic autopsy is the remaining gold standard in detection and evaluation of injuries, optionally with the use of post-mortem CT. Obviously, the level of detail in descripting (minor) injuries associated to CPR may fluctuate between single examiners or institutes. Several specialists in forensic pathology were responsible for the autopsies described here. Although we cannot ensure full consistency in the injury documentation between all colleagues retrospectively, the used guidelines and local regulations in this single-center comparison should have kept differences to a minimum.
The frequency of rib fractures was equal to other investigations rising from 58.7–64.6% in the mCC and 48.1–81.0% in the ACCD group [15,16,17] confirming the overall knowledge that rib fractures are common CPR-associated injuries. But yet, the occurrence of rib fractures seemed to correlate more with the patients’ ages and CPR duration than with the two CPR methods investigated. Spine fractures were rare in all studies [14, 15] and vertebral body bleedings were described separately in single cases [29].
However, our investigation could demonstrate that treatment with ACCD leads more often to hemothorax (additionally also influenced by the age of the deceased), pneumothorax and lung lesions compared to mCC alone. These findings were not reported with comparable differences in percentage numbers by other investigations [15,16,17, 30]. One explanation for these different findings might be the different sample sizes of available studies. Another might be that post-mortem diagnosis of pneumothorax requires special autopsy techniques, which were possibly not conducted by other investigators in every single case. Interestingly, the severity of organ damages or total bleeding volumes was not at all different for both methods.
We did wonder if chest compression-related pericardial ruptures were not detected, or rather were just not reported by other studies, as we recognized such injuries more than once in our investigations, and it was also presented in case reports [20, 31, 32].
The results for more frequent liver lesions after ACCD usage were comparable to published data [13, 15, 17], though other authors failed to report on volumes of associated hemoperitoneum.
From an emergency physician point of view, the findings in our investigation justify a standard work-up for CPR-associated injuries following mCC as well as ACCD in the clinical routine during CPR and after ROSC as all injuries described here must also be expected in survivors. This should include a computed tomography scan of the chest and abdomen right after admission of patients with out-of-hospital ROSC and also after successful ROSC in-hospital as soon as possible. In line with other investigations [33, 34], our study showed that longer duration of resuscitation efforts was associated with a higher incidence of CPR-related injuries. This should be kept in mind, especially in the ACCD cases, since ACCDs are recommended for transportation over a longer time interval. There are other groups assuming that traumatic lesions may occur during the first minutes of chest compression [35]. This may also explain why cases with shorter CPR durations showed different injury patterns in both groups (e.g. one case presented heart and lung lesions after 25 min of CPR by mCC, and pericardial rupture and hemothorax after 20 min of CPR using ACCD). In line with previously-published data [14,15,16, 26], in our study no major injury that could be identified as the ultimate cause of death for the cases investigated was detected. However, it was easy to imagine that some of the injuries detected could be associated with high morbidity in cases of survival [36]. Moreover, based on this investigation, clinicians have to expect CPR-associated injuries in each case and should be familiar with frequent and rare complications of CPR attempts [37].
This study has several limitations. First, the study design was retrospective, meaning that age-dependent diseases (such as osteoporosis) could not be assessed as an additional interfering factor. To our knowledge, only Smekal et al. [15] report percentages of osteoporosis in their charts. Additionally, the application of anticoagulants or established rescue lysis therapy could not be considered thoroughly as we were lacking toxicological laboratory parameters which could be tested reliably post-mortem and since their use was reported inconsequently in the autopsy records. Vice versa, the influence of anticoagulants or lysis therapy should only affect bleeding volumes and not the existence of soft tissue or osseous injury.
Overall, the main confounders of CPR-related injuries are CPR duration and age at death, as shown in our results. Our report is the first one to use bivariate logistic regression to look for diverse statistical influences besides the method of CPR used, on injury in cases where CPR has been carried out. Further prospective studies should therefore try to use statistical multivariable analyses by composite endpoints of major injuries consequently.
Moreover, not all cardiac arrest deaths were admitted to the Institute of Legal Medicine due to local autopsy policy of the state and law enforcement institutions indicating that there is an unalterable selection bias in forensic autopsy databases. However, the study sample size of 614 patients is larger than those of other comparable investigations (Table 4). Thirdly, we observed a forensic section cohort with the exclusive use of LUCAS devices as example of all existing ACCD. Consequently, the frequency of injuries could be different among surviving patients and/or other ACCD used since forensic autopsy cohorts may show special and different demographic and epidemiological data compared to all patients suffering from cardiac arrest. In addition, provider expertise with the ACCD also appeared to be a potential confounder, as misapplication of the device may increase the risk of injury in general [38]. Given the retrospective nature of the study we were not able to determine how much this potential bias influenced our results.
In comparison to all existing literature, we listed the most detailed variety of injuries and the largest cohort compared to other research studies [14,15,16,17, 27, 30, 39, 40].
Considering all facts, it should be kept in mind that all ACCD cases immediately underwent mCC after confirming cardiac arrest in daily routine before ACCD started, which might be one reason for the longer CPR durations in ACCD group compared to the mCC cohort. Consequently, it is difficult to distinguish sole mCC from combined mCC and ACCD complications. An additional inconsistency for our findings might be the existence or duration of bystander CPR until the arrival of professionals who then took over the role of CPR, but this does not seem to influence the frequency of the injuries in our study. Nevertheless, the systematic ‘higher’ injury frequencies of ACCD raise the suspicion to be associated to their use instead of sole mCC at least for all categories, which were shown to be independent from confounders (skin emphysema, pneumothorax, lung lesion, hemopericardium and liver lesion). Hypothetically, younger persons might get more forceful CPR attempts and were more often resuscitated by ACCD as geriatric patients. Therefore, the only investigation reporting of sole ACCD use [17] should be evaluated separately because this does not correspond to the circumstances of reality in emergency and forensic medicine and CPR efforts cannot be delayed for scientific purposes for evident ethical reasons as stated previously [16]. Unfortunately, we were not able to collect the time to application of ACCD in most of the cases due to the retrospective study design. If the time was available in some single cases, the interval was mostly limited to 20 min but never passed 45 min. Other studies also showed very fast application of ACCD after primary mCC in most cases [41]. However, it has to be kept in mind, that this potential bias may significantly impact the results if aggressive and prolonged mCC preceding placement of the ACCD were associated with more frequent injuries compared to patients who only had very brief manual compressions prior to ACCD initiation.
In summary, in patients with unsuccessful CPR, chest compression-related injuries were more frequent in the ACCD than in the mCC group in our autopsy cohort. Further relevant confounders were age and CPR duration, especially for osseous injuries. The severity of injuries did not differ between both groups, and no iatrogenic injury was declared by the forensic pathologist as being fatal.
Key points
-
1.
This is to date the most detailed variety of injuries and the largest cohort comparing ACCD and mCC groups.
-
2.
The severity of all CPR-associated injuries did not differ between both treatments.
-
3.
Higher age and longer CPR durations influenced the frequency of sternal and rib fractures.
-
4.
No registered chest compression-associated injury was fatal for the individual.
-
5.
The findings justify a standard work-up in the clinical routine after ROSC, including a computed tomography scan of the chest and abdomen, for CPR-associated injuries.
References
Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960;173:1064–7.
Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40:1192–8.
Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Bossaert LL, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132:1286–300.
Gates S, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, et al. Prehospital randomised assessment of a mechanical compression device in out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised trial and economic evaluation. Health Technol Assess. 2017;21:1–176.
Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, et al. European resuscitation council guidelines for resuscitation 2015: section 3. Adult advanced life support. Resuscitation. 2015;95:100–47.
Truhlar A, Deakin CD, Soar J, Khalifa GE, Alfonzo A, Bierens JJ, et al. European resuscitation council guidelines for resuscitation 2015: section 4. Cardiac arrest in special circumstances. Resuscitation. 2015;95:148–201.
Ondruschka B, Baier C, Hartwig T, Gräwert S, Böhm L, Dreßler J, et al. Guideline adherence of frustrating cardiopulmonary resuscitation by automated external chest compression devices. Notarzt. 2018. https://doi.org/10.1055/a-0669-9207.
Marti J, Hulme C, Ferreira Z, Nikolova S, Lall R, Kaye C, et al. The cost-effectiveness of a mechanical compression device in out-of-hospital cardiac arrest. Resuscitation. 2017;117:1–7.
Newberry R, Redman T, Ross E, Ely R, Saidler C, Arana A. No benefit in neurologic outcomes of survivors of out-of-hospital cardiac arrest with mechanical compression device. Prehosp Emerg Care. 2018;22:338–44.
Buckler DG, Burke RV, Naim MY, MacPherson A, Bradley RN, Abella BS, et al. Association of mechanical cardiopulmonary resuscitation device use with cardiac arrest outcomes: a population-based study using the CARES registry (Cardiac Arrest Registry to Enhance Survival). Circulation. 2016;134:2131–3.
Ji C, Lall R, Quinn T, Kaye C, Haywood K, Horton J, et al. Post-admission outcomes of participants in the PARAMEDIC trial: a cluster randomised trial of mechanical or manual chest compressions. Resuscitation. 2017;118:82–8.
Pinto DC, Haden-Pinneri K, Love JC. Manual and automated cardiopulmonary resuscitation (CPR): a comparison of associated injury patterns. J Forensic Sci. 2013;58:904–9.
Olds K, Byard RW, Langlois NE. Injuries associated with resuscitation – an overview. J Forensic Legal Med. 2015;33:39–43.
Smekal D, Johansson J, Huzevka T, Rubertsson S. No difference in autopsy detected injuries in cardiac arrest patients treated with manual chest compressions compared with mechanical compressions with the LUCAS device – a pilot study. Resuscitation. 2009;80:1104–7.
Smekal D, Lindgren E, Sanderl H, Johansson J, Rubertsson S. CPR-related injuries after manual or mechanical chest compressions with the LUCAS™ device: a multicenter study of victims after unsuccessful resuscitation. Resuscitation. 2014;85:1708–12.
Lardi C, Egger C, Larribau R, Niquille M, Mangin P, Fracasso T. Traumatic injuries after mechanical cardiopulmonary resuscitation (LUCAS™2): a forensic autopsy study. Int J Legal Med. 2015;129:1035–42.
Koster RW, Beenen LF, van der Boom EB, Spijkerboer AM, Tepaske R, van der Wal AC, et al. Safety of mechanical chest compression devices AutoPulse and LUCAS in cardiac arrest: a randomized clinical trial for non-inferiority. Eur Heart J. 2017;38:4006–13.
Kolopp M, Franchi A, Grafiadis P, Martrille L. Cardiothoracic injuries after CardioPump CPR: a report of two cases and review of the literature. Int J Legal Med. 2018;132:771–4.
Milling L, Leth PM, Astrup BS. Life-threatening and suspicious lesions caused by mechanical cardiopulmonary resuscitation. Am J Forensic Med Pathol. 2017;38:219–22.
Ondruschka B, Hartwig T, Gries A, Hädrich C, Dreßler J, Bernhard M. Pericardial laceration after using an automated mechanical chest compression device. Notfall Rettungsmed. 2017;20:424–9.
Ondruschka B, Baier C, Siekmeyer M, Buschmann C, Dreßler J, Bernhard M. Cardiopulmonary-resuscitation-associated injuries in still−/newborns, infants and toddlers in a German forensic collective. Forensic Sci Int. 2017;279:235–40.
German Society of Legal Medicine. S1 guideline ‘Forensic autopsy’. 2017. http://www.awmf.org/uploads/tx_szleitlinien/054-001l_S1_Die-rechtsmedizinische_Leichenoeffnung_2018-02.pdf. Accessed 09 July 2018.
Gates S, Quinn T, Deakin CD, Blair L, Couper K, Perkins GD. Mechanical chest compression for out of hospital cardiac arrest: systematic review and meta-analysis. Resuscitation. 2015;94:91–7.
Buschmann C, Schulz T, Toskos M, Kleber C. Emergency medicine techniques and the forensic autopsy. Forensic Sci Med Pathol. 2013;9:48–67.
Fanton L, David JS, Gueugniaud PY, Malicier D. Forensic aspects of automated chest compression. Resuscitation. 2008;77:273–4.
Yamaguchi R, Makino Y, Chiba F, Torimitsu S, Yajima D, Inokuchi G, et al. Frequency and influencing factors of cardiopulmonary resuscitation-related injuries during implementation of the American Heart Association 2010 Guidelines: a retrospective study based on autopsy and postmortem computed tomography. Int J Legal Med. 2017;131:1655–63.
Truhlar A, Hejna P, Zabka L, Zatopkova L, Cerny V. Injuries caused by the autopulse and LUCAS II resuscitation systems compared to manual chest compressions. Resuscitation. 2010;81:S62.
Koga Y, Fujita M, Yagi T, Nakahara T, Miyauchi T, Kaneda K. Effects of mechanical chest compression device with a load-distributing band on post-resuscitation injuries identified by post-mortem computed tomography. Resuscitation. 2015;96:226–31.
Rößler L, Dümpelmann D, Tsokos M. “Simon’s bleedings“ without a hanging situation. Rechtsmedizin. 2018;28:298–300.
Rubertsson S, Smekal D, Huzevka T, Johansson J. Mechanical chest compressions with the LUCAS device does not increase the incidence of injuries in cardiac arrest victims. Circulation. 2007;116:II_930.
Agdal N, Jorgensen TG. Penetrating laceration of the pericardium and myocardium and myocardial rupture following closed-chest cardiac massage. Acta Med Scand. 1973;194:477–9.
Klintschar M, Darok M, Radner H. Massive injury to the heart after attempted active compression-decompression cardiopulmonary resuscitation. Int J Legal Med. 1998;111:93–6.
Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest. 1987;92:287–91.
Boland LL, Satterlee PA, Hokanson JS, Strauss CE, Yost D. Chest compression injuries detected via routine post-arrest care in patients who survive to admission after out-of-hospital cardiac arrest. Prehosp Emerg Care. 2015;19:23–30.
Baubin M, Rabl W, Pfeiffer KF, Benzer A, Gilly H. Chest injuries after active compression-decompression cardiopulmonary resuscitation (ACD-CPR) in cadavers. Resuscitation. 1999;43:9–15.
Buschmann C, Schulz F. Delayed pericardial tamponade after successful resuscitation. Resuscitation. 2009;80:1328–9.
Buschmann C, Tsokos M. Frequent and rare complications of resuscitation attempts. Intensive Care Med. 2009;35:397–404.
Treffer D, Monschau S, Helm M, Weißleder A. Mechanische thoraxkompressions-geräte. Notfallmedizin Up2date. 2018;13:125–30.
Englund E, Silfverstolpe J, Halvarsson B, Löfberg H, Walther C. Injuries after cardiopulmonary resuscitation: a comparison between LUCAS mechanical CPR and standard CPR. Resuscitation. 2008;77:S13–4.
Menzies D, Barton D, Darcy C, Nolan N. Does the LUCAS device increase trauma during CPR? Resuscitation. 2008;77:S13.
Tranberg T, Lassen JF, Kaltoft AK, Hansen TM, Stengaard C, Knudsen L, et al. Quality of cardiopulmonary resusciation in out-of-hospital cardiac arrest before and after introduction of a mechanical chest compression device, LUCAS-2; a prospective, observational study. Scand J Trauma Resusc Emerg Med. 2015;23:37.
Acknowledgments
The authors would like to thank Miss Lina Woydt for providing the anatomic sketch and Miss Aqeeda Singh for proofreading the paper as a native speaker.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethics committee of the Medical Faculty of the University of Leipzig, Germany (code: 104/17-ek).
Informed consent
Informed consent was waived due to the retrospective nature of the study.
Electronic supplementary material
Supplemental Fig. 1
Overview of the annual distribution of forensic autopsy cases at the Institute of Legal Medicine (University of Leipzig, Germany) with unsuccessful cardiopulmonary resuscitation (CPR) subdivided in annual numbers of manual chest compression (mCC) and automated chest compression device (ACCD) recorded in this study. All ACCD cases used a LUCAS II device. (JPEG 35 kb)
Rights and permissions
About this article
Cite this article
Ondruschka, B., Baier, C., Bayer, R. et al. Chest compression-associated injuries in cardiac arrest patients treated with manual chest compressions versus automated chest compression devices (LUCAS II) – a forensic autopsy-based comparison. Forensic Sci Med Pathol 14, 515–525 (2018). https://doi.org/10.1007/s12024-018-0024-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-018-0024-5