Abstract
Purpose
Describe and analyze the trends of thyroid cancer incidence and mortality in Guangzhou, explore the potential influencing factors, and provide evidence for the government to formulate prevention and treatment measures.
Methods
Incident and death cases of thyroid cancer were retrieved from the Guangzhou cancer registry. The joinpoint regression models were used to estimate the incidence and mortality trends. Age-period-cohort models were used to estimate the age, period, and cohort effects on the time trends. Grey correlation analysis was performed to explore possible connections between thyroid cancer and social factors.
Results
A total of 15,955 new cases of thyroid cancer were registered in Guangzhou during 2004–2018, the age-standardized incidence rate (ASIR) of thyroid cancer increased from 4.29/105 in 2004 to 22.36/105 in 2018, with the average annual percentage change (AAPC) of 13.40%. The overall increase can be attributed to the increase in the incidence of papillary thyroid carcinoma (PTC), which was dominated by tumors <2 cm. The ASIR was higher in women (16.12/105) compared to men (5.46/105), and young and middle-aged individuals had higher incidence rates than older people. The number of thyroid cancer deaths registered between 2010 and 2018 was 356, and the age-standardized mortality rates (ASMRs) were stable (approximately 0.42/105). Men’s ASMR (0.34/105) and women’s (0.49/105) were similar, and those 60 and older had greater mortality. The period and cohort relative risks showed an overall increasing trend. Furthermore, there was a strong positive correlation between the ASIRs and social determinants.
Conclusions
During the study period, the incidence rate of thyroid cancer among young and middle-aged people in Guangzhou showed a rapidly increasing trend, and the mortality was relatively stable. In the future, more effective preventive measures should be taken for this age group to reduce the burden of disease and avoid overdiagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is one of the most common malignant tumors of human endocrine system and head and neck, which originates from thyroid follicular epithelium or parafollicular epithelial cells [1]. Over the past few decades, the thyroid cancer incidence rates have apparently risen rapidly in many countries throughout the world (such as, the United States, South Korea, China, etc.) [2]. According to the International Agency for Research on Cancer’s GLOBOCAN 2020 [3], 586,000 thyroid cancer cases were diagnosed worldwide, leading to thyroid cancer ranking the ninth among all cancers. The age-standardized incidence rate (ASIR) was 6.6/105, and the rate of women (10.1/105) was higher than that of men (3.1/105). Compared with the large number of cases, the deaths of the thyroid cancer were only 44,000. The age standardized mortality rate (ASMR) was 0.43/105, which was significantly lower than the incidence rate. And there was no difference between men (0.34/105) and women (0.49/105). Thyroid cancer, the fastest growing tumor in China, is growing at a rate of 20% per year. The 2016 annual report of the Chinese Cancer Registry [4] showed that the ASIR of thyroid cancer was 10.37/105, and the rate in women (15.81/105) was three times higher than that in men (5.11/105) and ranked the third in women malignant tumors. Furthermore, thyroid cancer is more prevalent in regions with strong socioeconomic development in China, such as Tianjin, Beijing, Shanghai, Zhejiang Province, and Guangdong Province, where thyroid cancer currently ranks among the top five malignant tumors [5]. A study found that after a thyroid cancer diagnosis, the cost of subsequent therapy increased by about 4% annually and was expected to exceed the cost of colon cancer treatment by 2039 [6]. This rapid growth will inevitably increase the financial burden on society as well as individual patients.
The underlying causes of this growth trend in thyroid cancer remain unknown. Previously recognized risk factors related to thyroid cancer include exposure to ionizing radiation (including radiation pollution caused by nuclear facilities [7] and medical radiation exposure [8], family history of thyroid disease [9], iodine supplement or deficiency [10], etc). The contributing elements are continually evolving along with the growth of the social economy and the acceleration of urbanization. The increase in the use of healthcare systems (such as increased exposure to medical X-rays, head and neck CT scans, dental X-rays, etc.), personal risk factors (such as gender, age, unhealthy lifestyle [11] and psychological factors [12], etc.), and the interaction of many risk variables, including the environment factors (such as air pollution [13,14,15], endocrine disruptors [16] and carcinogens [17, 18], may lead to an increase in the incidence rate of thyroid cancer. However, these factors cannot fully explain the rapid increase in incidence rate of thyroid cancer. In some high-income countries such as the United States and South Korea, excessive screening and high diagnostic rates were considered to be the main reasons for the high incidence rate [19]. Additionally, more sophisticated medical procedures are frequently used in regions that have higher socioeconomic development, such as fine needle aspiration (FNA) of the thyroid gland and high-resolution ultrasound, which increases the possibility of over diagnosis.
Guangzhou, the capital of Guangdong Province and the central area of the Pearl River Delta, is known as the “South Gate” of China and a crucial entry point and center for the opening of the nation to the outside world. Its total GDP and economic growth rate are among the top in the nation, and it has a relatively complete system of public service guarantees and relatively balanced resources for education and healthcare. In recent years, the incidence rate of thyroid cancer in Guangzhou has continued to grow rapidly, which has aroused widespread public concern. However, there is no comprehensive and systematic epidemiological trend analysis on thyroid cancer in Guangzhou. This study investigated the temporal trends of thyroid cancer incidence and mortality in Guangzhou, China, based on the research methods and materials. Using age-period-cohort models to assess the impact of age, period and birth cohort on the temporal trends of incidence rate by gender. In addition, the potential association between the incidence rate of thyroid cancer and social factors was examined using grey correlation analysis. It is convenient to timely understand the variations in the incidence and mortality of thyroid cancer and potential risk factors in Guangzhou, and it can also offer a scientific basis for thyroid cancer prevention and treatment.
Materials and methods
Data collection
Incident and death cases data
The incident cases data from 2004 to 2018 and the deaths data from 2010 to 2018 of thyroid cancer in Guangzhou were both from the Guangzhou cancer registry (Established in 1998) of the Guangzhou Center for Disease Control and prevention, and was obtained from the Guangzhou malignant tumor case registration and report management information system. All cancer cases were reported through the hospital’s network direct reporting system [20]. The data of new cases included demographic information (such as name, sex, date of birth, nationality, household address, etc.) and tumor characteristic information (such as the year of disease diagnosis, ICD 10th edition code (ICD-10), Third Edition (ICD-O-3) code, diagnosis location, clinical diagnosis, pathological diagnosis and the underlying cause of death, etc.). The ICD-10 code had been verified based on the clinical diagnosis and pathological diagnosis of the hospital, and tumor patients with the ICD-10 code of C73 were chosen as thyroid cancer cases. The pathological types were classified according to ICD-O-3: papillary thyroid carcinoma (PTC, 8050, 8052, 8260, 8340–8343, 8450), follicular thyroid carcinoma (FTC, 8290, 8330–8331, 8333, 8335), medullary thyroid carcinoma (MTC, 8345–8346, 8510) and anaplastic thyroid carcinoma (ATC, 8020, 8021). The other pathological types correspond to others. Verified and merged the duplicate reported cases one by one to ensure that all included cases were new cases, and verified the supplementary reports after finding the missing reports.
Demographic data and social factors
This study collected relevant data from census data and the Guangzhou Statistical Yearbook by the website of Guangzhou Municipal Bureau of Statistics (http://tjj.gz.gov.cn), including population census data from 2000, 2010 and 2020, registered population data from 2004 to 2018 in Guangzhou, social-economic development and medical and health resources related data. Based on 3-year population census data, the age structure distributions of the population from 2004 to 2018 were calculated using interpolation method [21]. The data related to socio-economic development and medical and health resources mainly include: Gross Domestic Product, Per Capita Gross Domestic Product, Per Capita Annual Disposable Income of Urban and Rural Residents, Permanent Population Density, Life Expectancy, Health Care Institutions (Hospitals), Medical Professionals (Doctors), Hospital Beds, Government healthcare expenditure, Proportion of Expenditure for Medical and Health to Total Fiscal Expenditure, Health Care and Medical Services Expenditure of Urban and Rural Residents (Table S1).
Statistical analysis
Data preprocessing
In this study, Microsoft Excel 2016 and SPSS 26.0 statistical analysis software were used for data preprocessing and statistical analysis. The crude incidence rates (CIRs), crude mortality rates (CMRs), ASIRs and ASMRs of thyroid cancer were calculated based on the annual average population of Guangzhou and the world Segi’s population [22]. According to the age of cancer diagnosis, the number of cases was stratified by sex and age (0–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79 and >=80), and the sex-age-specific incidence and mortality rates were calculated. Age was presented as median and inter quartile (IQ), and count data was expressed as frequency (%).
Joinpoint regression model
We used the joinpoint software (version 4.9.1.0) provided by the National Cancer Institute Surveillance and research program to build a connection point regression model (log linear model) to reflect the long-term trends of thyroid cancer incidence and mortality rates [23]. The grid search method (GSM) was used to obtain the regression function with unknown connection points. The Monte Carlo permutation test was used to test whether the obvious changes of the trend were statistically significant. Annual percentage change (APC), average annual percentage change (AAPC) and 95% CI (Confidence Interval) were used as outcome indicators to reflect the trends of thyroid cancer incidence and mortality rates over time.
Age-period-cohort model
The age-period-cohort model was used to study the effects of age, period and cohort on ASIRs of thyroid cancer by using a free network tool (http://analysistools.nci.nih.gov/apc/) provided by the National Cancer Institute of the United States [24]. In the age-period-cohort model, the age range was limited to 20–84 years and divided into 11 groups based on 5 years old (20–24 years old to 80–84 years old), the diagnosis period was divided into 3 groups (2004–2008, 2009–2013, 2014–2018), and the birth cohort was divided into 15 groups (from 1924–1928 to 1994–1998). The central age group, the period group and the cohort group were selected as the reference. The APCs for each age group, knowing as the local drifts in the analysis, and annual percentage changes of the expected age adjusted rates over time (net drift) were also estimated. The effects of periods and cohorts were expressed as rate ratios relative to the reference period and the reference cohort, respectively. Wald’s test was used to determine significance, and a two-sided P value less than 0.05 was considered statistically significant.
Grey correlation analysis
Grey correlation analysis is a statistical analysis method for multiple factors based on grey system theory [25]. The major goal of the method is to identify the key influencing variables by evaluating the degree of correlation between the geometry of the compared sequence and the reference sequence. The main advantage of this approach is the absence of rigorous constraints for the number and regularity of samples [26]. The steps of grey correlation analysis are as follows:
Step1: Set up the comparative sequence and reference sequence:
The reference sequence (Yj) is the ASIRs of thyroid cancer, including men, women, and total. The compared sequence (Xi) refers to social determinants, such as Social-Economic Development and Medical and Health Resources.
Step2: Standardize the original data:
Data normalization is necessary before variables with different units may be analyzed and contrasted. The min-max normalization approach was employed in this study to normalize the data. All Yj values and Xi values were normalized to values between 0 and 1 after normalization. The formula is as follows:
Step3: Calculate the grey correlation coefficient. This correlation coefficient is expressed as:
Step4: Calculate the grey correlation degrees as:
The value of γ (yj, xi) ranges from 0 to 1. Generally, if 0 < γ (yj, xi) ≤ 0.30, the correlation is considered to be low; if 0.30 < γ (yj, xi) ≤ 0.60, the correlation is moderate; if 0.60 < γ (yj, xi) ≤ 1.0, the correlation is strong.
Results
General demographic characteristics
With the extension of per capita life expectancy, the proportion of elderly population in Guangzhou has significantly increased in the past 15 years. From 2004 to 2018, the proportion of the population aged 60 and above reached 10.04%, with 9.04% of men and 11.15% of women. According to the World Health Organization’s definition of an aging society (with over 10% of the population over 60 years old), Guangzhou has entered an aging society (Fig. 1).
Basic information of incident and death cases
During the period of 2004–2018, a total of 15955 new thyroid cancer cases were registered in Guangzhou (Table S2). The number of women patients (11914, 74.67%) was more than that of men patients (4041, 25.33%). The median age of diagnosis of thyroid cancer was 44 years old. In men, women and the total population, the median age of diagnosis showed an early trend with the extension of time. Overall, the analysis results showed that thyroid cancer in Guangzhou was more common among people aged 20–59 years (13,184, 82.63%). The number of registered thyroid cancer deaths from 2010 to 2018 was 356 (128 (35.96%) men and 228 (64.04%) women). The median age of death of thyroid cancer was 66 years old. Notably, in contrast to the distribution of thyroid cancer cases, the proportion of thyroid cancer-related deaths among the elderly population over 60 was relatively large (222, 62.36%), and the age of death increased with an extension of time. (Table S3).
Incidence and mortality
The total CIR of thyroid cancer was 13.11/105, and the ASIR was 10.78/105. The ASIR of women (16.12/105) was about three times that of men (5.46/105). In addition, the ASIRs of thyroid cancer showed an upward trend from 2004–2018, and the ASIR in 2018 (22.36/105) was about 5 times that in 2004 (4.29/105) (Table 1). The total CMR of thyroid cancer from 2010 to 2018 was 0.29/105 (0.21/105 in men and 0.38/105 in women). The overall ASMR was 0.42/105, and the ASMR was roughly similar among men (0.34/105) and women (0.49/105). Year-by-year CMRs and ASMRs were detailed in Table 2, with relatively stable changes.
Age-specific incidence and mortality rates
From the age of onset, there was a large gender difference in the incidence of thyroid cancer. The incidence rates of thyroid cancer were similar in men and women before the age of 15. The women incidence rates increased in the 15–19 age group, peaked in the 50–54 age group, and then sharply decreased. However, men incidence peaked later than women incidence, in the 60–64 age group, and then slowly decreased as age increased. The incidence rates of women in all ages were significantly higher than that of men (Fig. 2a). Compared to the age-specific incidences, before 55–59 years old, the age-specific mortality rates were extremely low. The mortality rate started increasing quickly from the age group of 60–64 years, peaked at the age group of 80–84 years (Fig. 2b).
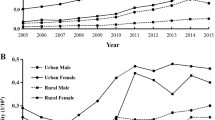
Temporal trends of incidence and mortality rates by gender
During the study period, the ASIR of thyroid cancer increased from 4.29/105 in 2004 to 22.36/105 in 2018, and the AAPC was 13.40% (95% CI: 12.17% ~ 14.64%, P < 0.001). When gender-specific trends were explored (Table 3 and Fig. 3a), men’s and women’s ASIRs both showed significant increase tendencies over time, with men (AAPC = 13.14%, 95% CI: 8.94% ~ 17.50%, P < 0.001) rising slightly faster than women (AAPC = 12.48%, 95% CI: 11.28% ~ 13.70%, P < 0.001). In addition, the joinpoint regression of men thyroid cancer incidence rate identified two significant inflection points in 2009 and 2012 (Fig. 3a and Table 3). The ASIRs changed steadily from 2004 to 2009 (APC = 2.78%, 95% CI: −2.79% ~ 8.66%, P = 0.283), while beginning in 2009, the ASIRs started to rise quickly. APCs was 26.95% (95% CI: 5.21% ~ 53.18%, P = 0.020) in the period 2009–2012 and 15.71% (95% CI: 13.59% ~ 17.89%, P < 0.001) in the period 2012–2018, respectively. In terms of mortality, the ASMR of thyroid cancer changed from 0.17/105 in 2010 to 0.45/105 in 2018. According to joinpoint regression analysis, the AAPC was 4.55% (95% CI: −4.86% ~ 14.89%, P = 0.301) in the period 2010–2018, demonstrating that the mortality rates were relatively stable without discovering significant changes over time. Similar patterns of mortality trend were found in men and women (Table 4 and Fig. 4a).
Temporal trends of incidence and mortality rates by age
When considering the age-specific incidence trends (Table 3 and Fig. 3b), the age-specific incidence rates in other age groups exhibited obvious upward trends over time, with the exception of the 0–19 years old (AAPC = 3.53%, 95% CI: −7.57% ~ 15.96%, P = 0.549) and above 80 years old age groups (AAPC = −0.22%, 95% CI: −4.23% ~ 3.96%, P = 0.910), which did not display any significant changes. Especially among young and middle-aged people aged 20–49, the increasing trends of thyroid cancer incidence rate were particularly significant. In addition, among all subgroups, the age-specific mortality rates in the 60–69 age groups (AAPC = 22.88%, 95% CI: 3.53% ~ 45.83%, P = 0.018) and the 70–79 age groups (AAPC = 7.81%, 95% CI: 0.90% ~ 15.18%, P = 0.031) showed an upward trend, whereas the age-specific mortality rates in the other subgroups were relatively stable and did not show a significant trend of change (Table 4 and Fig. 4b).
Trends of incidence by pathological type
Due to inadequate case registration data from 2004 to 2009 and data related to tumor characteristics (such as pathological type, staging, and size) were missing, we only conducted tumor pathological analysis on the data of thyroid cancer cases from 2010 to 2018. In Guangzhou, 13242 thyroid cancer cases were diagnosed between 2010 and 2018. Based on the pathological types, these cases were categorized into five groups: PTC, FTC, MTC, ATC and other. The PTC accounted for the majority of the cases (92.30%), followed by FTC (2.20%), MTC (0.80%), ATC (0.20%) and others (4.60%). The trends in the ASIRs of the different pathological types of thyroid cancer in 2010–2018 can be seen in Table S4 and Fig. S1. The results demonstrated that PTC predominated the incidence of thyroid cancer throughout the study period, and that the ASIR showed a rapidly increase over time, whereas the ASIRs of other pathological types were low and the trends were steady. Considering 87.52% of the tumor size data was absent, we only assessed the tumor sizes of 1525 patients with PTC (Table S5). Our results revealed that PTC with a tumor size of less than 2 cm accounted for a larger proportion compared to PTC with tumor sizes greater than 2 cm and that the number of cases grew rapidly over time (Fig. S2). In addition, with the pathological types of thyroid cancer, we analyzed the basic situation of new thyroid cancer cases in different age groups (Table S6). According to the findings, the less malignant PTC accounted for more than 90% in the 20–59 age group, and the proportion gradually decreased with the increase of age. In contrast, FTC, MTC, and ATC with moderate and high malignancy were more prevalent in people aged 60 years and older.
Age-period-cohort analysis
The results of age-period-cohort analysis of men and women were shown in Fig. 5. In men, the age-at-onset curve that was adjusted for period and cohort effects showed a trend of first rising and then falling with age, reaching the peak in the 75–79 age group. Whereas, in women, the incidence rate increased with age throughout. The period effects showed an increase in both sexes, and increased significantly in the most recent period, 2014–2018. The rate ratios of period effects for 2014–2018 vs 2004–2008 were 4.25 for men and 3.25 for women. In general, the risk of thyroid cancer increased with birth cohort in both sexes. The cohort effects remained stable for the first several birth cohorts, followed by upwards inflection for men and women born after mid-1960s.
Age-period-cohort model of the ASIRs of thyroid cancer in men and women in Guangzhou, 2004–2018. a Men; b Women. Longitudinal age curve: Expected age-specific rates (per 100000) in reference cohort adjusted for period effects; Period RR period effects on incidence; Cohort RR cohort effects on incidence; Local drift values: annual percentage change of age-specific groups for incidence; The shaded bands indicate 95% CIs; The dashed lines indicate the reference period (2009–2013 as reference) and cohort (1959–1963 birth cohort group as reference)
Grey correlation analysis
Table 5 showed the indicators for Socio-Economic development and Medical and Health Resources. There were 13 indicators in total, including 6 for socioeconomic development and 7 for Medical and Health Resources. The ASIRs of total, men and women thyroid cancer were used as the reference sequences, and all thirteen indicators were used as the comparative sequences for grey correlation analysis. The results of the analysis were listed in Table 6. From the grey correlation analysis, whether total, men, or women, the grey correlation values between the ASIRs of thyroid cancer and social determinants were larger at a strong level. It means that Socio-Economic development and Medical and Health Resources had a great impact on thyroid cancer incidence rate.
Based on the grey correlation values between the ASIRs of total and the 13 indicators, the top grey correlation was X10, which corresponded to government healthcare expenditures, with a grey correlation value of 0.8862. Followed by X8, which was the number of Medical Professionals (Doctors), with a grey correlation value of 0.7827. It implied that government healthcare spending and the number of medical professionals (doctors) were the primary factor indicators for connection with the incidence rate of thyroid cancer. Among the indicators of Social-Economic Development, the indicators with high correlation were X1, X3, X4 and X5, corresponding to GDP, Per Capita Annual Disposable Income of Urban and Rural Residents, Permanent Population Density, respectively, and the grey correlation values were 0.7040, 0.7417, 0.7710, and 0.7034, respectively. These indicators reflected the changes of Guangzhou’s economic development level and people’s living standards to some extent. This implied that changes in the level of economic development and people’s living standards were also closely related to the incidence of thyroid cancer.
Discussion
Our study used data from a population-based cancer registry that included 9.13 million Guangzhou residents to describe the temporal trends in thyroid cancer incidence and mortality rates. The ASIRs of thyroid cancer in Guangzhou increased almost fivefold from 4.29/105 in 2004 to 22.36/105 in 2018, with an AAPC of 13.40%, and there were obvious gender and age disparities. In contrast to the ASIRs, the thyroid cancer ASMRs was low and stable, and increased from 0.17/105 in 2010 to 0.45/105 in 2018. Thyroid cancer incidence rising significantly and mortality rates exhibiting a stable trend in Guangzhou were similar with those in the majority of other nations [27, 28]. In China, the ASIRs of thyroid cancer increased from 3.21/105 in 2005 to 9.61/105 in 2015, and the mortality rate increased from 0.28/105 in 2010 to 0.35/105 in 2015 [29]. In contrast, we found that the ASIR of thyroid cancer in Guangzhou was 4.42/105 in 2005, which was similar to the incidence level in China, and it was 14.94/105 in 2015, which was significantly higher than the China’s average. The ASMR in 2015 was 0.59/105, which was slightly higher than the national average for China. From the data above, it was apparent that the ASIRs in Guangzhou were increasing more quickly than the national average, but the ASMRs were not much different from that in China, they were all at a low level. What factors caused the rapid rise of incidence in Guangzhou was worth exploring.
The research revealed that, women had a higher incidence of thyroid cancer than men (women to men ratio: 3:1), but their mortality rates (0.49/105) were similar to the men’s (0.34/105). Women sex hormones and reproductive processes are thought to have a significant role in the development of thyroid cancer [30,31,32]. And the curves of gender-age-specific incidences revealed that the incidence of thyroid cancer in women began to rise rapidly at the age of 20 and peaked between the ages of 50–54, coinciding with menopause in women, implying that estrogen levels may be involved in the development of thyroid cancer. Women’s estrogen levels are naturally higher than men’s, and women in their 20 s to 40 s are at the height of their reproductive potential and have the highest hormone levels of their lives. As a result, thyroid cancer in women is more likely to occur at this time. In addition, women are more likely than men to use healthcare services (since of perimenopausal and reproductive factors), which may make thyroid screening and diagnosis more easily accessible and timely for women [33, 34].
In the study period, the overall trend of incidence was not significantly different between men (13.14%) and women (12.48%). However, men showed two inflection points in 2009 and 2012. The ASIRs of thyroid cancer in men changed steadily between 2004 and 2009. It could be that thyroid cancer was previously thought to be more common in women and they were usually more conscious of their health, which made women more likely to be detected than men [35]. Between 2009 and 2012, the ASIRs in men began to increase at a rate of 26.95%, indicating a “explosive” growth trend. The possible reasons were as follows: in 2009, the American Thyroid Association revised the guidelines for the diagnosis and treatment of thyroid cancer [36], and China also released the first Guidelines for the Diagnosis and Treatment of Differentiated Thyroid Cancer [37], defining the diagnostic criteria for thyroid cancer. During this period, the Ministry of Health of China released the Interim Provisions on Health Examination Management [38] and gradually implemented the New Medical Revolution (the coverage percentage of social medical insurance increased from 29.7% to 95.7% between 2003 and 2011) [39]. The implementation of thyroid cancer diagnosis and treatment guidelines and some policies further increased people’s medical needs and health examination consciousness, leading to the diagnosis of previously undetected male patients. As a results, a huge number of men cases were found in a short period, indicating an “explosive” growth. After the “explosive” growth, the men incidence rate began to moderate at a rate of 15.71%, slightly higher than that of women, during 2012 to 2018. In addition, exposure to occupational risk factors may be a contributing factor to the increase in men incidence rates. During the period from 2000 to 2010, with the development of the economy and the acceleration of industrialization, the exposure to occupational risk factors got more and more apparent, and the number of cases of occupational disorders increased dramatically [40], which lead to the increased incidence rate of thyroid cancer in men [16].
The results showed that the proportion of thyroid cancer cases in 20–59 years old reached 82.63% (13184/15955). The incidence rates of thyroid cancer were higher and increased faster in this age range compared to other age groups, but the mortality rates were very low. It’s possible reason maybe that this age group belongs to occupational population and receives yearly health examination, which lead to more hidden patients be identified and raise the chance of exposing to medical radiation. Previous studies have also shown that the increase in medical radiation exposure [41, 42] and health screening rates [43,44,45] may lead to a rapid increase in the incidence of thyroid cancer. Furthermore, they are more likely to use computers, mobile phones, and other electronic devices for extended periods of time due to work-related reasons. Researches had indicated that radio frequency radiation from electronic devices such as mobile phones will affect thyroid hormones and cells [46, 47]. And prolonged or frequent usage of mobile phones can especially increase the risk of thyroid cancer in those with susceptible single nucleotide polymorphism mutations (SNPs, a type of genetic mutation) [48]. As a key entryway and hub for China’s opening-up, Guangzhou has a remarkable economic growth. Due to intense social competition and fast-paced way of life, people in this age group are frequently more likely to experience long-term strain from life, job, and psychology. What’s more, they also frequently live irregular lifestyles and eat erratically (such as eating takeout and staying up late, etc.). Long periods of intense stimulation will cause abnormal autoimmune regulation, disrupt the normal operation of the endocrine system, and result in thyroid illness [11, 12]. Moreover, the vast majority of thyroid cancers were low malignant PTC in this age group (over 90%), which may be associated with lower mortality and better prognosis.
Conversely, in the age group of 60 years and older, the proportion of cases of thyroid cancer was only 14.81% (2525/15955), but the proportion of deaths was as high as 62.36% (222/356). And the incidence rates of thyroid cancer in this age group were relatively lower compared to the 20–59 age group, but the mortality rates were higher. It may be related to the proportion decline of low malignancy PTC and the proportion increase of high malignancy of other pathological types, resulting in the higher mortality rate and poor prognosis in this age group compared to those aged 20 to 59. Elderly people often suffer from degenerative changes in tissue cells, decreased physiological function, and a steady decrease in their immunity and defense against tumors, making it difficult to recognize and eliminate mutated cells, which results in a higher malignancy of thyroid cancer in the elderly [49]. Considering that young and middle-aged people were more likely to develop thyroid cancer and less to die from thyroid cancer, it was essential for them to improve lifestyles and reduce environmental risk factors to decrease the occurrence of thyroid cancer, especially the PTC. With the population aging [50], the issue of thyroid cancer prevention and treatment will get much worse in Guangzhou. In the future, the screening of thyroid cancer for the elderly should get adequate attention to promote them early diagnosis and aggressive therapy.
The outcomes of the age-period-cohort models revealed that the incidence rate of thyroid cancer appeared to be influenced by both period and birth cohort effects. The development of social economy, the improvement of diagnostic methods, and the increase of medical detection of thyroid nodules may lead to an abnormal increase in the incidence rate of men and women over the past decade. Consistent with previous study findings [51], our results also indicated that the ASIRs of thyroid cancer were much more closely related to medical and health resources, such as the government healthcare expenditure, the number of Medical Professionals (Doctors) and people’s access to and affordability of medical care resources. In other words, with the Guangzhou government’s increased investment in healthcare costs and medical resources, people have access to more and better healthcare services and easier undergo thyroid ultrasound examinations, so as to, increase the rate of thyroid cancer being identified. Moreover, the results of our grey correlation analysis also showed that the change of economic development level and people’s living standard in Guangzhou were also closely related to the incidence of thyroid cancer. Guangzhou, an international metropolis, with intense social competitiveness, a quick pace of life and strong job pressure, all of which frequently cause people to suffer from psychological and spiritual issues (such as long-term anxiety, depression and stress). And people’s lifestyles have changed significantly along with the growth in income and the improvement in living standards. The negative emotions and unhealthy eating and living habits may cause the thyroid cancer [11, 12]. Many developed arears, such as the United States, Denmark, and Shanghai, China, all have the same thyroid cancer incidence rate pattern [52,53,54].
To sum up, we were more inclined to consider that the overdiagnosis related to the increase of Medical and Health Resources was the primary cause of the sharp increase of thyroid cancer incidence rate in Guangzhou. The reasons were as follows: first of all, even though the ASIRs of thyroid cancer increased in Guangzhou, the ASMRs continued to be low and stable. The phenomenon may be attributed to the widespread use of modern diagnostic techniques, such as ultrasound and fine needle aspiration, which increased PTC (especially papillary thyroid microcarcinoma (PTMC), tumor size <1 cm) detection. And our resulted showed that the increase in the incidence of thyroid cancer was virtually entirely due to an increase in PTC in the 20–59 age group and was dominated by tumors smaller than 2 cm. PTC is regarded as an inert cancer, because the majority of patients show no apparent symbols, have low aggressiveness, progress slowly, and have a favorable prognosis [55]. Some epidemiological studies have also confirmed this notion, showing that PTMC was the primary cause of the rise in PTC diagnoses [28, 56, 57]. Secondly, the development and implementation of some relevant policies not only increase people’s (particularly 20–59 age group) attention to their own health, but also increase their opportunity of health examination and medical consumption, which further leads to the discovery of occult thyroid cancer and increasing the detection rate. In addition, our results showed that the level of social and economic development in Guangzhou and the level of government investment in medical and health resources were closely related to the incidence of thyroid cancer. Previous study demonstrated that people who live in economically developed areas were more aware of health management, had access to more medical resources and were more likely to undergo thyroid-related examinations [58]. These results in the increase of detecting small, clinically insignificant cases of thyroid cancer, which increased the number of thyroid cancer cases but not the life span.
Thyroid cancer overdiagnosis is a problem because it might be difficult to identify which people require therapy. According to our data, thyroid surgery was carried out on a majority of patients (93.11%) with thyroid cancer. The situation was similar even in patients with PTC (95.31%), but the PTC is considered low-risk and the patient prognosis is good, with a 5-year disease-specific survival rate of >98% [59]. The risk of consequences from thyroid surgery is low but significant, and it includes hypoparathyroidism and nerve injury that may lead to hoarseness and even voice loss. Furthermore, thyroid replacement treatment is required for follow-up patients. These not only lower their quality of life but also increase the economic strain on patients and the healthcare system. In the future, further studies are needed to establish more cautious diagnostic methods, and should pay attention to the strategies of screening and control thyroid cancer.
We acknowledge that there are certain limitations to our study. Firstly, the study suggested that a crucial factor in a sharp increase in the incidence rate of thyroid cancer was overdiagnosis, but did not make further screening recommendations. In the future, we will further improve the data information on tumor size, stage, prognosis and treatment of thyroid cancer patients to assess the degree of thyroid cancer overdiagnosis in Guangzhou, on the basis of prospective cohort studies or disease monitoring in natural population. Secondly, in common with other analyses of cancer registry data, we were unable to assess the exposure of key risk factors in the underlying population and in cancer cases, such as social factors (education level, income level, medical resources, etc.), lifestyle and dietary patterns, and environmental exposure. Additionally, there are geographic variations in the distribution of risk factors for thyroid cancer, such as economic level, medical resources and environment factors (air, industrial and agricultural pollution). Exploring the regional clustering of thyroid cancer incidence in Guangzhou will help identify the association between thyroid cancer and other risk factors, and then implement targeted prevention. Thus, it is necessary to apply spatial analysis to explore the precise reasons in the future.
Conclusion
In conclusion, during the study period, the incidence rate of thyroid cancer in Guangzhou increased significantly, while the mortality was relatively steady. The majority of the new cases were low-risk PTC subtype with beneficial prognoses. Women were more likely to get thyroid cancer than men, however since 2009, men’s upward trend have exceeded women’s, and the gender gap has gradually closed. The 20–59 age group has a higher incidence rate and a lower mortality rate of thyroid cancer than that group of 60 years and older. Effective measures and tailored projects targeting the target population, especially those aged 20–59, can greatly reduce the burden caused by thyroid cancer. Additionally, our results implied that there may be an overdiagnosis of thyroid cancer in Guangzhou. Therefore, more studies on the cause, prevention, and treatment of thyroid cancer are required to improve diagnostic criteria or establish more practical diagnostic methods to detect thyroid cancer patients with clinical significance.
Data availability
Data are available from the corresponding authors upon reasonable request and with permission of Guangzhou Center for Disease Control and Prevention.
References
National Health Commission, Guidelines for diagnosis and treatment of thyroid cancer (2018 edition). Chin. Arch. Gen. Surg. (Electron. Ed.) 13, 1–15 (2019)
W.Q. Bao, H. Zi, Q.Q. Yuan et al. Global burden of thyroid cancer and its attributable risk factors in 204 countries and territories from 1990 to 2019. Thorac. Cancer 12(18), 2494–2503 (2021). https://doi.org/10.1111/1759-7714.14099
H. Sung, J. Ferlay, R.L. Siegel et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021). https://doi.org/10.3322/caac.21660
R. Zheng, S. Zhang, H. Zeng et al. Cancer incidence and mortality in China, 2016. J. Natl Cancer Cent. 2(1), 1–9 (2022)
R.S. Zheng, S.W. Zhang, K.X. Sun et al. Cancer statistics in China, 2016. Chin. J. Oncol. 45(3), 212–220 (2023). https://doi.org/10.3760/cma.j.cn112152-20220922-00647
B.H. Lang, C.K. Wong, C.T. Chan, Initial attributable cost and economic burden of clinically-relevant differentiated thyroid cancer: A health care service provider perspective. Eur. J. Surg. Oncol. 41(6), 758–765 (2015). https://doi.org/10.1016/j.ejso.2015.01.019
M.D. Tronko, G.R. Howe, T.I. Bogdanova et al. A cohort study of thyroid cancer and other thyroid diseases after the Chornobyl accident: thyroid cancer in Ukraine detected during first screening. J. Natl Cancer Inst. 98(13), 897–903 (2006). https://doi.org/10.1093/jnci/djj244
S.J. Schonfeld, C. Lee, A. Berrington de González, Medical exposure to radiation and thyroid cancer. Clin. Oncol. (R. Coll. Radio.) 23(4), 244–250 (2011). https://doi.org/10.1016/j.clon.2011.01.159
B. D’Avanzo, C. La Vecchia, S. Franceschi et al. History of thyroid diseases and subsequent thyroid cancer risk. Cancer Epidemiol. Biomark. Prev. 4(3), 193–199 (1995)
Y. Wang, W. Wang, Increasing incidence of thyroid cancer in Shanghai, China, 1983–2007. Asia Pac. J. Public Health 27(2), 223–229 (2015). https://doi.org/10.1177/1010539512436874
S. Afrashteh, M. Fararouei, M.T. Parad et al. Sleep quality, stress and thyroid cancer: a case-control study. J. Endocrinol. Invest 45(6), 1219–1226 (2022). https://doi.org/10.1007/s40618-022-01751-4
T. Bogović Crnčić, M. Ilić Tomaš, N. Girotto et al. Risk factors for thyroid cancer: what do we know so far? Acta Clin. Croat. 59(Suppl 1), 66–72 (2020). https://doi.org/10.20471/acc.2020.59.s1.08
X. Cong, Air pollution from industrial waste gas emissions is associated with cancer incidences in Shanghai, China. Environ. Sci. Pollut. Res 25(13), 13067–13078 (2018). https://doi.org/10.1007/s11356-018-1538-9
Q. He, M. Wu, Q. Shi et al. Association of Ozone Exposures with the risk of thyroid nodules in Hunan Province: a population-based cohort study. Environ. Health 21(1), 65 (2022). https://doi.org/10.1186/s12940-022-00874-8
S. Karzai, Z. Zhang, W. Sutton et al. Ambient particulate matter air pollution is associated with increased risk of papillary thyroid cancer. Surgery 171(1), 212–219 (2022). https://doi.org/10.1016/j.surg.2021.05.002
E. Kruger, E.A. Toraih, M.H. Hussein et al. Thyroid carcinoma: a review for 25 years of environmental risk factors studies. Cancers (Basel) 14(24), 6172 (2022). https://doi.org/10.3390/cancers14246172
P. Malandrino, C. Scollo, I. Marturano et al. Descriptive epidemiology of human thyroid cancer: experience from a regional registry and the “volcanic factor”. Front Endocrinol. (Lausanne) 4, 65 (2013). https://doi.org/10.3389/fendo.2013.00065
A. Buha, V. Matovic, B. Antonijevic et al. Overview of cadmium thyroid disrupting effects and mechanisms. Int J. Mol. Sci. 19(5), 1501 (2018). https://doi.org/10.3390/ijms19051501
M. Li, L. Dal Maso, S. Vaccarella, Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 8(6), 468–470 (2020). https://doi.org/10.1016/S2213-8587(20)30115-7
H. Liu, G. Lin, K. Li et al. Evolution of cancer registration combining online reporting with follow-up in the community: practices in Guangzhou, China. Asian Pac. J. Cancer Prev. 18(3), 639–646 (2017). https://doi.org/10.22034/APJCP.2017.18.3.639
National Cancer Center. Chinese guideline for cancer registration 2016. (People’s Medical Publishing House, Beijing, 2016)
R. Doll, P. Cook, Summarizing indices for comparison of cancer incidence data. Int J. Cancer 2(3), 269–279 (1967). https://doi.org/10.1002/ijc.2910020310
H.J. Kim, M.P. Fay, E.J. Feuer et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med 19(3), 335–351 (2000). https://doi.org/10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z
P.S. Rosenberg, D.P. Check, W.F. Anderson, A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomark. Prev. 23(11), 2296–2302 (2014). https://doi.org/10.1158/1055-9965.EPI-14-0300
D. Julong, Introduction to grey system theory. J. grey Syst. 1(1), 1–24 (1989)
T. Xuerui. Medical Grey Relational Theory and its Application. (Science Press, Beijing, 2019).
J. Huang, C.H. Ngai, Y. Deng et al. Incidence and mortality of thyroid cancer in 50 countries: a joinpoint regression analysis of global trends. Endocrine 80(2), 355–365 (2023). https://doi.org/10.1007/s12020-022-03274-7
L. Du, Y. Wang, X. Sun et al. Thyroid cancer: trends in incidence, mortality and clinical-pathological patterns in Zhejiang Province, Southeast China. BMC Cancer 18(1), 291 (2018). https://doi.org/10.1186/s12885-018-4081-7
J. Wang, F. Yu, Y. Shang et al. Thyroid cancer: incidence and mortality trends in China, 2005-2015. Endocrine 68(1), 163–173 (2020). https://doi.org/10.1007/s12020-020-02207-6
W.J. Mack, S. Preston-Martin, L. Bernstein et al. Reproductive and hormonal risk factors for thyroid cancer in Los Angeles County females. Cancer Epidemiol. Biomark. Prev. 8(11), 991–997 (1999)
G.E. Krassas, Thyroid disease and female reproduction. Fertil. Steril. 74(6), 1063–1070 (2000). https://doi.org/10.1016/s0015-0282(00)01589-2
M. Derwahl, D. Nicula, Estrogen and its role in thyroid cancer. Endocr. Relat. Cancer 21(5), 273–283 (2014). https://doi.org/10.1530/ERC-14-0053
Y. Wang, K. Hunt, I. Nazareth et al. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open 3(8), e003320 (2013). https://doi.org/10.1136/bmjopen-2013-003320
K.D. Bertakis, R. Azari, L.J. Helms et al. Gender differences in the utilization of health care services. J. Fam. Pr. 49(2), 147–152 (2000)
K. LeClair, K.J.L. Bell, L. Furuya-Kanamori et al. Evaluation of gender inequity in thyroid cancer diagnosis: differences by sex in US thyroid cancer incidence compared with a meta-analysis of subclinical thyroid cancer rates at autopsy. JAMA Intern Med 181(10), 1351–1358 (2021). https://doi.org/10.1001/jamainternmed.2021.4804
Z. Guo, Q. Li, H. Li, Interpretation of the diagnostic and treatment guidelines for thyroid nodules and differentiated thyroid cancer by the American Thyroid Society in 2009. Chinese. J. Pract. Surg. 30(10), 859–862 (2010)
J. Chen, C. Li, S. Wang, Diagnosis and treatment guidelines for differentiated thyroid cancer (preliminary draft). Cancer Prev. Treat. 24(01), 55–68 (2011)
Gazette of the National Health Commission of the People’s Republic of China. Notice of the Ministry of Health on the Issuance of the Interim Provisions on the Management of Health Checkups. (General Office of the National Health Commission, Beijing, 2009)
Q. Meng, L. Xu, Y. Zhang et al. Trends in access to health services and financial protectio-n in China between 2003 and 2011: a cross-sectional study. Lancet 379(9818), 805–814 (2012). https://doi.org/10.1016/S0140-6736(12)60278-5
Q. Ding, L. Schenk, S.O. Hansson, Occupational diseases in the People’s Republic of China between 2000 and 2010. Am. J. Ind. Med. 56(12), 1423–1432 (2013). https://doi.org/10.1002/ajim.22245
M.A. Han, J.H. Kim, Diagnostic X-ray exposure and thyroid cancer risk: systematic review and meta-analysis. Thyroid 28(2), 220–228 (2018). https://doi.org/10.1089/thy.2017.0159
A. Memon, I. Rogers, P. Paudyal et al. Dental X-rays and the risk of thyroid cancer and meningioma: a systematic review and meta-analysis of current epidemiological evidence. Thyroid 29(11), 1572–1593 (2019). https://doi.org/10.1089/thy.2019.0105
Y. Liu, F. Lai, J. Long et al. Screening and the epidemic of thyroid cancer in China: an analysis of national representative inpatient and commercial insurance databases. Int J. Cancer 148(5), 1106–1114 (2021). https://doi.org/10.1002/ijc.33298
H.S. Ahn, H.J. Kim, K.H. Kim et al. Thyroid cancer screening in South Korea increases detection of papillary cancers with no impact on other subtypes or thyroid cancer mortality. Thyroid 26(11), 1535–1540 (2016). https://doi.org/10.1089/thy.2016.0075
S. Seo, S. Park, D.N. Lee et al. Increased incidence of thyroid cancer in occupational radiation epidemiology: attribution to screening among radiation workers. Radiat. Res 195(4), 397–400 (2021). https://doi.org/10.1667/RADE-20-00193.1
J.F. Asl, B. Larijani, M. Zakerkish et al. The possible global hazard of cell phone radiation on thyroid cells and hormones: a systematic review of evidences. Environ. Sci. Pollut. Res Int 26(18), 18017–18031 (2019). https://doi.org/10.1007/s11356-019-05096-z
T. Alkayyali, O. Ochuba, K. Srivastava et al. An exploration of the effects of radiofrequency radiation emitted by mobile phones and extremely low frequency radiation on thyroid hormones and thyroid gland histopathology. Cureus 13(8), e17329 (2021). https://doi.org/10.7759/cureus.17329
J. Luo, H. Li, N.C. Deziel et al. Genetic susceptibility may modify the association between cell phone use and thyroid cancer: a population-based case-control study in Connecticut. Environ. Res 182, 109013 (2020). https://doi.org/10.1016/j.envres.2019.109013
G. Pawelec, Immunosenescence and cancer. Biogerontology 18(4), 717–721 (2017). https://doi.org/10.1007/s10522-017-9682-z
W. Lutz, W. Sanderson, S. Scherbov, The coming acceleration of global population ageing. Nature 451(7179), 716–719 (2008). https://doi.org/10.1038/nature06516
M. Soheylizad, S. Khazaei, E. Jenabi et al. The relationship between human development index and its components with thyroid cancer incidence and mortality: using the decomposition approach. Int J. Endocrinol. Metab. 16(4), e65078 (2018). https://doi.org/10.5812/ijem.65078
C. Zhu, T. Zheng, B.A. Kilfoy et al. A birth cohort analysis of the incidence of papillary thyroid cancer in the United States, 1973-2004. Thyroid 19(10), 1061–1066 (2009). https://doi.org/10.1089/thy.2008.0342
M. Blomberg, U. Feldt-Rasmussen, K.K. Andersen et al. Thyroid cancer in Denmark 1943-2008, before and after iodine supplementation. Int J. Cancer 131(10), 2360–2366 (2012). https://doi.org/10.1002/ijc.27497
P.P. Bao, Y. Zheng, C.X. Wu et al. Cancer incidence in urban Shanghai, 1973-2010: an updated trend and age-period-cohort effects. BMC Cancer 16, 284 (2016). https://doi.org/10.1186/s12885-016-2313-2
H. Katoh, K. Yamashita, T. Enomoto et al. Classification and general considerations of thyroid cancer. Ann. Clin. Pathol. 3(1), 1045 (2015)
L. Davies, H.G. Welch, Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 295(18), 2164–2167 (2006). https://doi.org/10.1001/jama.295.18.2164
A. Miranda-Filho, J. Lortet-Tieulent, F. Bray et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 9(4), 225–234 (2021). https://doi.org/10.1016/S2213-8587(21)00027-9
M. Li, R. Zheng, L. Dal Maso et al. Mapping overdiagnosis of thyroid cancer in China. Lancet Diabetes Endocrinol. 9(6), 330–332 (2021). https://doi.org/10.1016/S2213-8587(21)00083-8
T.S. Wang, J.A. Sosa, Thyroid surgery for differentiated thyroid cancer—recent advances and future directions. Nat. Rev. Endocrinol. 14(11), 670–683 (2018). https://doi.org/10.1038/s41574-018-0080-7
Acknowledgements
We thank all the participants in the study and the healthcare workers of the Community Health Centers and the Center for Disease Control and Prevention.
Funding
The study was supported by the National Natural Science Foundation of China (No: 81803326), Guangzhou Key Research and Development Project (No: 202206080008), The Key Project of Medicine Discipline of Guangzhou (No: 2021-2023-12), Applied Basic Research Program of Shanxi (No: 201801D221265), Research Project of Postgraduate Education Reform in Shanxi Province (No: 2020YJJG134), Teaching Reform and Innovation Project of higher education in Shanxi Province (No: J20220372), Medical Education Research Project of Medical Education Branch of Chinese Medical Association and Medical Education Professional Committee of Chinese Higher Education Association (No: 2020A-N02036), and Teaching Reform and Innovation Project of Shanxi Medical University (No: GXJ202011).
Author information
Authors and Affiliations
Contributions
B.L., P.Q., and X.H. conceived and designed the project. B.L., S.W., H.X., and K.L. collected the data. J.Zhou, Y.L., H.L., Z.S., Y.W., and J.Zhang analysed and interpreted the data. The first draft of the manuscript was written by J.Zhou and the revision was completed by X.H., J.Zhou, and Y.L. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, J., Liang, B., Liu, Y. et al. Exploring temporal trends and influencing factors for thyroid cancer in Guangzhou, China: 2004–2018. Endocrine 84, 509–523 (2024). https://doi.org/10.1007/s12020-023-03578-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03578-2